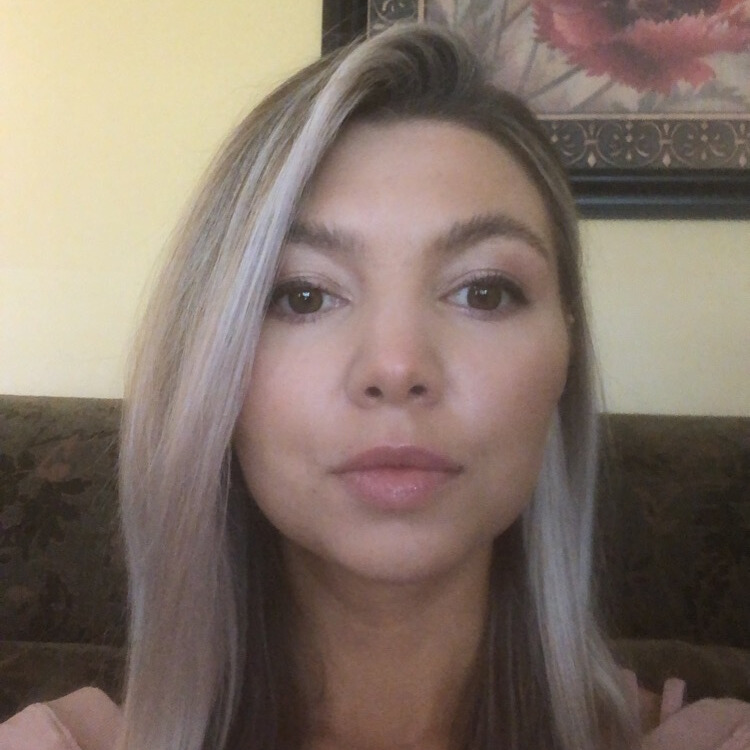
Jenn’s Recurrent Melanoma Story
Jenn, a recent college graduate, scored her dream job working for the Chicago Cubs. Years earlier, she had taken a health class that led her to learn the ABCDEs and warning signs of skin cancer. Then in 2014, she noticed an abnormal mole that matched 3 out of 5 of the ABCDEs of skin cancer. She visited a dermatologist that confirmed she had stage 1B melanoma.
Living by herself in Chicago hours away from family made recovering from her diagnosis difficult, so Jenn made the tough decision to leave her dream job, move back to her small town, and live with her parents. It was here that she discovered the burden her cancer diagnosis and recent life transitions had on her mental health which led her to seek help from a therapist.
After being cancer-free for 5 years, Jenn’s mental health was again negatively impacted by the effects of the pandemic. About a year after lockdowns began, Jenn had her second melanoma diagnosis which would be the first of 3 recurrences in 11 months.
Now a year cancer-free, Jenn shares her recurrent melanoma story with us, including how she worked on her mental health, what her experience with scanxiety has been like, making life-changing decisions after a cancer diagnosis, and her advice for those on their own cancer journeys.

Try to change that perspective of, I’m lost and I don’t know who I am anymore, into this idea that you get to find out who you are now. Have fun exploring and trying new things and seeing what you love. You’re getting to know yourself all over again.
Jenn S.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms
Tell us about yourself
My name is Jenn and I am originally from a smallish town in western Wisconsin, but I currently live in Saint Paul, Minnesota.
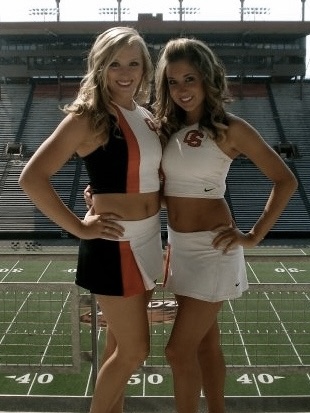
I grew up in a family that absolutely loves sports, so I ended up going to college for sports. I didn’t play, but I got my degree in sports communication and then went on and got my master’s in sports management. When my first job outside of college was with the Chicago Cubs, it was a pinch-me moment. I’ve worked for 4 professional sports teams, including winning a WNBA championship with the Minnesota Lynx.
It was this random general education class that I took when I was in college that may have ended up saving my life.

Today I am the director of marketing at a small financial planning firm here in the Twin Cities. I also teach part-time in our communications department at my alma mater, Concordia University Saint Paul.
I am a huge advocate of animal rescue, including having my own rescue, Xena The Warrior Kitty. I used to love doing fun runs and 5Ks and I just started getting back into it between my first and second melanoma diagnosis, but it got really hard to keep up with during the ongoing surgeries. That’s something I’ve been feeling really called to try to get back into, so hopefully soon.
Lastly, I really love to read and write. I have for as long as I can remember. I wrote my first book when I was in second grade, one of those fill-in-the-blank hardcover books that they give you. Writing has really become a big part of my healing process and processing everything I’ve gone through with cancer.
How did you know the warning signs of skin cancer?

It was this random general education class that I took when I was in college that may have ended up saving my life. As part of our general education requirements, we had to choose a physical education class and I ended up taking a general health class. As part of that curriculum, we were each assigned to do a research project and report on a different illness or disease. Mine ended up being skin cancer, something that I knew nothing about.
I learned the different types of skin cancer and the warning signs. What really stuck with me were the ABCDEs of melanoma. That really came full circle.
What were your first symptoms?
It was a dark, chocolatey brown on one half and even darker brown on the other half. Right in the middle, there was a black dot, so the color was very unique.
A few years later, I was living in Chicago, I was working for the Cubs, and it was late 2014. At some point, I started to notice that there was a mole on my right shoulder that just didn’t sit right with me. I didn’t know how long it had been there. I knew it hadn’t always been there, otherwise, I wouldn’t all of a sudden be noticing it. I can’t trace back to when it first appeared. The first picture I remember seeing it in was around July of that year when I went back later and looked.

As far as the ABCDEs go, it was the color that really stood out, and it was asymmetrical and the diameter. It was a dark, chocolatey brown on one half and even darker brown on the other half. Right in the middle, there was a black dot, so the color was very unique. If you drew a line down the center, it didn’t match, and it was larger than the size of a pencil eraser, which is 3 of the 5 things that you look for when it comes to melanoma. That was in late 2014.
I went home for the holidays and I showed it to my mom. Of course, she was trying to be reassuring, and she said, “I’m sure it’s nothing, but you should definitely make an appointment with a dermatologist. If nothing else, you’ll get peace of mind.”
Making an appointment with the dermatologist
When I got back to Chicago, I got an appointment very fast. Maybe it was because of the holidays, because these days the dermatology wait is probably 6 months to get in and see somebody. But I was able to get in within a week. It was the first Tuesday of January. I went in and met with the dermatologist. He looked at the mole, put his hand on my shoulder, and said, “Thank you for coming in and showing me this.” My heart just sank. His reaction was very sobering. In a way, I think it helped to prepare me.
You’re never prepared to hear the words “You have cancer” but I knew that it was serious and it was a good thing I had come in when I did. I would tell anyone if you see something, if you have any doubts, trust your gut and make the appointment. Worst case scenario, it’s nothing, and that’s what you would hope for.

Getting a biopsy and awaiting the results
When I left the appointment that day, they did a shave biopsy and sent it down to pathology, and told me I would probably hear from them in the middle of the following week. If I didn’t hear from them by that following Friday, give them a call.

Less than a week later, on Monday, I was at work, sitting at my cubicle in our office, and got a phone call and didn’t recognize the number. I let it go to voicemail and then saw that it was from my doctor and I was not expecting to hear from them that soon. I excused myself to the hallway to give them a callback. The specific clinic that I went to in Chicago has a screening process. When you call, you tell them who they are, who you are, and who you’re calling to speak to, and they’ll put you on hold while they pull up your records and look to see if they need to get somebody right away. It was also the end of the day, 4:30 in the afternoon, so nurses and doctors were probably getting ready to leave, finishing up their last appointment.
Diagnosis
The doctor came back on and he’s like, “I’m sorry to tell you this. It’s cancer.” I remember nothing else from the phone call after that.

What did the doctors say?
She put me on hold and she came back and said, “Jennifer, they want to speak to you right away. I’m going to put you through to the doctor.” It was another one of those moments where my heart just sank. I remember so vividly, I was outside the elevator bank, and one of my co-workers was coming off the elevator. I smiled at him like everything was fine, and inside I’m just like, this is going to change everything. The doctor came back on and he’s like, “I’m sorry to tell you this. It’s cancer.” I remember nothing else from the phone call after that.
»MORE: Reacting to a Cancer Diagnosis

I texted my boss. He was aware of the situation, so knew I would be hearing something new, that I’d had the appointment the week before. I texted him and let him know I’m going to be leaving a little bit early. Once a week, we work late and it was my day to work late. He’s like, “Don’t worry, we’ll cover it.” Immediately after texting him, I called my mom and it was calling her and having to say those words out loud that really made it real for the first time.
Being alone through a cancer diagnosis
That was one of the hardest things going through that alone. It did lead to me deciding to move back home for a little bit with the longer-term goal of moving close to home, but still in a big city. I love my small town, but I’m a big-city girl at heart.
In the coming days, I made an appointment on that phone call to have a consultation with an oncologist that Wednesday. My family was 5-hours away by car, and I knew they would want to come down for the surgery and treatment and all of that.

The oncologist was great. We called my mom on speakerphone. She was able to be on speakerphone through the entire conversation which was really helpful because I just found out that I had cancer. My mind is spinning. The questions I have are definitely not the questions she has and the odds of me remembering anything, I definitely didn’t take notes. We were giggling at my mom and all the questions she would ask. In the end, I was really grateful because those were things that, as we got closer to my surgery, I would wonder about and she had the answers and it hadn’t occurred to me.
What was your staging?

They were able to give me a couple of different dates for options for my surgery. Based on the shave biopsy that they had done, their initial estimate of staging was that I was stage 1B, but the only way to be sure of that was to also do a sentinel node biopsy and make sure that the cancer hadn’t spread to my lymph nodes.
Describe what a sentinel node biopsy is
A sentinel node biopsy is a procedure typically done on the day of your surgery. You go in a little bit earlier before your operation. They will inject a dye into the area where your cancer is, then you have to sit and wait for that dye to travel through your bloodstream so they’re able to see if the cancer had spread. The dye is very painful. The closest thing I can compare it to is a Lidocaine injection times 50. It burns, you can feel it traveling through you.

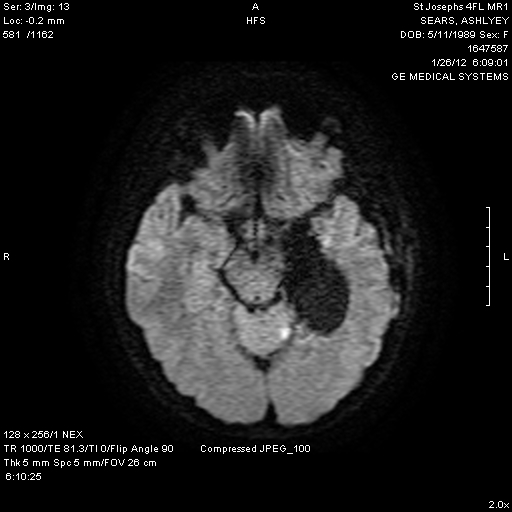
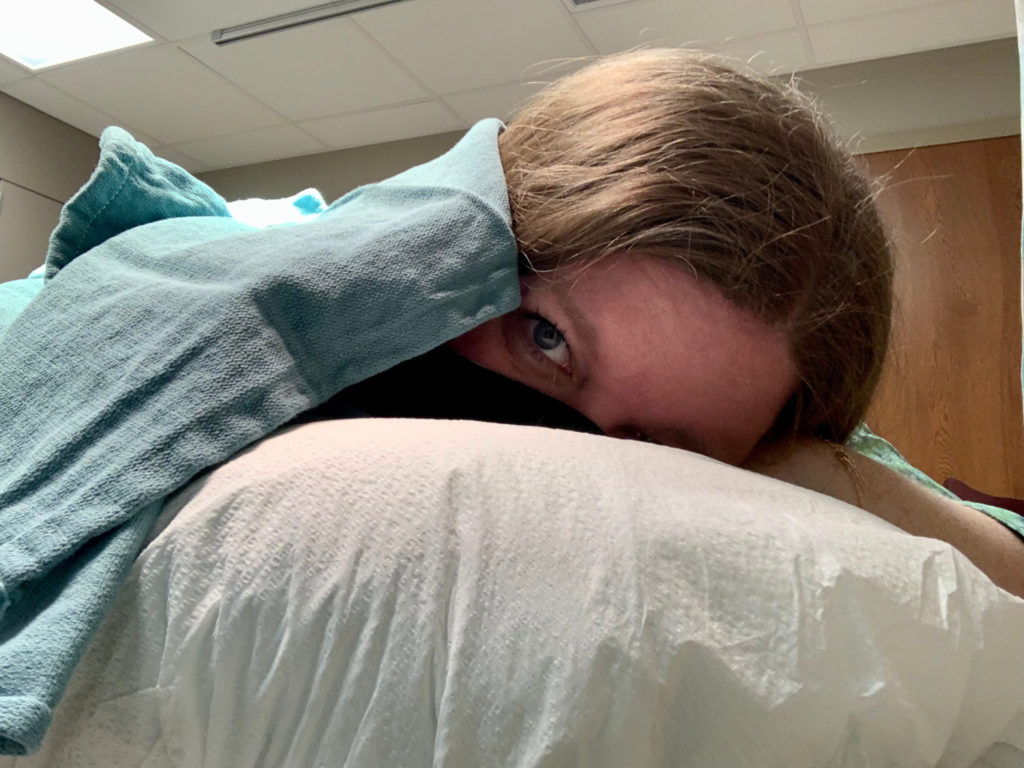
After it’s had time to travel, they take a bunch of photos, so you have to stay really still. It’s about a 15 to 20-minute process. You’re slid into a tube, very similar to an MRI, and they scan and take pictures. Any of the lymph nodes that light up are the ones that they end up removing during surgery. I actually had lymph nodes in 2 different areas that lit up. I had to have 2 removed from under my right arm and one removed from the right side of my neck.
Surgery
How long did your procedure take that day?
Because I had to be there early for the sentinel node biopsy – I had to be at the hospital at 8 a.m. – it was actually so early that my family wasn’t able to be there yet. I traveled to the hospital alone, on the Red Line train in Chicago with my little backpack, and I brought a stuffed animal with me. I felt like a little kid traveling to see their family, but I needed something to comfort me, especially going in alone.
I went in at about 8:00 for the lymph node tracing, and from start to finish, I want to say it took about 2 hours. I didn’t have a watch on me because I wasn’t allowed to wear any jewelry that day so I just left it behind. I didn’t have an exact amount of time, but it was between 10 and 10:30 when I was brought back out to the waiting room in that area where then my sister and my mom were both waiting for me and were able to be with me until my operation. From that point, they brought me down to get checked into the operating room for the surgery. My surgery was scheduled for one with anesthesia and surgery prep around noon.
»MORE: Cancer Surgery Treatments
There was a little bit of a gap in between so my mom, sister, and I were brought down to the operating room. They got me set up in the operating room area and in a gown. So many people came in to talk to me. I had a plastic surgeon come in and talk to me because, on the top of your shoulder, there’s not a lot of extra skin. The oncologist was doing the surgery to remove cancer and the lymph nodes and the plastic surgeon was coming in to then stitch it back up so that there would be less of a scar and to maintain the skin that was there as best as they could.
Being prepped for surgery

The anesthesiologist was coming in and talking to me about complications and risks and waivers, the plastic surgeon coming in and covering all of that, and then the oncologist coming in and covering all of that too. That was when I really started to get scared. I was talking to my mom and my sister and I was joking like, Mom, if anything happens, you get my cat. Jill If anything happens, you get my shoes. Laughing was my coping mechanism for it to help keep the fears down.
I’d never had surgery before this. Luckily, after they gave me the anesthesia, my mom and my sister were able to walk beside my bed while they started wheeling me down to the O.R. The last thing I remember is my sister being on one side and my mom being on the other. I was out cold before I even got to the operating room.
How long did the surgery take?

I believe the surgery took about 2.5 to 3 hours, and the next thing I remember is waking up in the operating room, and I was incredibly nauseous. That’s a common side effect of anesthesia, but because I hadn’t had surgery before, we didn’t know that I was going to have that. I was in the recovery room for a pretty long time because I wasn’t able to leave until I was able to at least keep crackers and some water down through an IV. They were able to give me anti-nausea meds, but it was at least half an hour before I could even sit up without feeling nauseous.
I believe we left around 4:30. From the time I got there at 8 a.m. until the time I left, it was 8 to 4:30. About 9.5 hours.
Describe your recovery process

That was the first time that I realized that if I had to continue doing this on my own, I didn’t think it was realistic to do so far away from my family with that extra support.
After the surgery, I had to be off of work for at least a week and a half, and then I was going to be able to return for 2.5 days with restricted mobility. Because I lived in Chicago and didn’t have a car, it was extra challenging because I took the red line to work every day. On the train, especially during rush hour, you’re lucky if you get a seat. There was no realistic way for me to stand and hang on to a bar for balance having just had major surgery on my shoulder.
My mom and my sister were able to stay through the weekend and they helped me get up, set up with groceries, get things close by me in my apartment, and set me up as best as they could.
I ended up having, not a reaction to Vicodin, but I’d never had it before and the Vicodin ended up making me very nauseous as well. There were days when I’d be laying on my side trying to eat something before taking Vicodin to manage it because it made me so sick to my stomach.
The doctor prescribed a new medication that would help with the pain, but would hopefully not have the same side effects. We were in the middle of a snowstorm and I didn’t have a car. A friend of mine had to dig the car out of a snow bank to go get it for me. That was the first time that I realized that if I had to continue doing this on my own, I didn’t think it was realistic to do so far away from my family with that extra support.
What was the result of your surgery?
It took about a week and a half to get the results from my surgery pathology. My lymph nodes, all 3, were confirmed clear. There had been no spread so that confirmed a stage 1 diagnosis. Then the plan was skin checks every 3 months for 5 years to be reassessed in 3 years, depending on if we found further spots, if I had other recurrences or anything like that.

How did you process your cancer diagnosis?
I had no idea what was to come but didn’t really process it because everything happened so fast. My immediate reaction was just to put it behind me.
My very next skin check just happened to be the day before my lease was up on my apartment. Knowing that my skin check was the day before my lease was up left this feeling of my life being really uncertain. A lot of that was probably cancer too, but at the time, I hadn’t even processed the actual diagnosis. Everything happened so fast. From the time of my appointment with the dermatologist where they did a biopsy until the surgery where they actually removed the melanoma was less than 3 weeks.

I remember after the surgery when we got the pathology that everything was clear, I was like, that was it? There was a lot of guilt surrounding that because so many people have more challenging cancer diagnoses and go through a lot more treatment. I had no idea what was to come but didn’t really process it because everything happened so fast. My immediate reaction was just to put it behind me.
Mental Health
Making big decisions due to a cancer diagnosis
When I had that skin check, I was like, Well, what if this comes back? I can’t do this on my own. It’s really hard. I had amazing friends in Chicago but had not even been there for 2 years, so I didn’t have the same strength of relationships that I had back home. I also had my foot in the door at an incredible organization. I was halfway through getting my master’s degree in sports management at that point, so I felt like I was having to choose between 2 futures.
Do I choose my career knowing that health-wise, that may be more difficult or do I choose having my family close by in case my health does take a turn? But this may have a huge impact on my career. I went back and forth no less than 10 to 15 times a day. I drove my mom crazy. I was calling her multiple times a day. I would call her when I woke up in the morning, when I was walking to the train to go to work, and on my lunch break. She’s like, “Jenn, you just have to pick one. There’s no right or wrong answer. It’s whatever you think is right for you.” I was like, well, what do you think? She’s like, “I can’t make that decision for you. You have to make it for yourself.”

Ultimately I did end up deciding to go home, but that was really hard too, because that meant I wasn’t going to have a job. I hadn’t lived at home for years, and it felt like a huge step backward. Going from a big city like Chicago to my small hometown where I wasn’t close with a lot of my classmates from high school, it didn’t feel like I had a lot there. It was a really difficult transition.
»MORE: Read More About Cancer Support
Struggling to transition to life changes post-cancer
I’ve now developed a healthy relationship with the sun, but for a while, if it was between 10 and 2, I was terrified to be outside.
When I was back home, I first leaned into running, taking care of myself, and getting outside. A lot of anxieties crept in. I had melanoma, which is skin cancer, so I want to go for a run. Typically I was a middle-of-the-day runner. I’m not going to run outside in the middle of the day because now, to a degree, I’m afraid of the sun. I can’t have this cancer come back. I’ve now developed a healthy relationship with the sun, but for a while, if it was between 10 and 2, I was terrified to be outside. I was afraid that something I had done had caused this and I didn’t want to cause it to happen again.

I also wasn’t working, so I had a lot of free time. I felt somewhat worthless. I was actually finishing my master’s at that time, but I placed so much worth in this career that I was working towards that all of a sudden, feeling stagnant was really difficult. I was applying for a ton of jobs up in Saint Paul, Minneapolis, which is a pretty big sports community as well, and just wasn’t hearing a lot back. That really took a hit on my self-esteem.
All of my friends were either in the Twin Cities, which is an hour’s car ride away, or back in Chicago, which was a 5.5-hour car ride away. My parents were essentially my entire social life.
What was the state of your mental health after cancer?
I had struggled with depression in the past, so when that thought crossed my mind, I immediately was aware of it and caught it and was like, this is not okay. I don’t want to feel this way.

I went to coffee one day and it was a really eye-opening moment. After I left the coffee shop, I was sitting at the stoplight and I was just waiting for it to turn green so that I could go. I remember thinking, I don’t want to be here anymore. I don’t want to be alive anymore. I felt like such a huge burden to my parents at this point. I had more skin checks and they all came back with needing more biopsies. Luckily, none of them were melanoma at that point, but they were coming back atypical and I couldn’t see a future that didn’t involve my family having to take care of me and me being terrified of cancer and having more biopsies and more surgeries. It felt hopeless like there was no way out.
I had struggled with depression in the past, so when that thought crossed my mind, I immediately was aware of it and caught it and was like, this is not okay. I don’t want to feel this way. Because of my history of depression, I was able to talk to my mom about it. We have a pretty open relationship about that stuff and I’ve been able to go to her for support when it happened before.
I started seeing a therapist close to my hometown and it was helpful at the time. She wasn’t really the right fit for me, but there weren’t a ton of options, so it was helping. My sister, the company that she worked for, needed some help. I was able to start working there part-time. She knew that it was temporary, but for me, it at least gave me a feeling of doing something worthwhile. I was making money. If I wanted to go visit my friends in the cities, I could pay for my own gas. It gave me a little bit more sense of independence back. A few months later, I ended up getting a job offer for an internship at Target Field with the Minnesota Twins.
How did you manage your mental health?

For me, it’s been finding things that bring me purpose. Cancer has really changed my perspective on that.
With mental health and depression, having good things happen doesn’t fix it. It doesn’t cure it. I still go to therapy at least once a month, sometimes more often, depending on what’s happening with my health and what stage we’re at with skin checks and biopsies and things like that.
»MORE: Cancer and Mental Health
I think it’s choosing to do the smallest thing that you can do and go from there. Some days, if you can get up and take a shower and brush your teeth and that’s all you can do, you did it. Every day, keep going and finding things.
For me, it’s been finding things that bring me purpose. Cancer has really changed my perspective on that. It’s changed how I see my career and how I spend my time. Finding what really drives you to want to get out of bed in the morning and doing the smallest thing every day that you can do, eventually, you find yourself being able to do more and more.
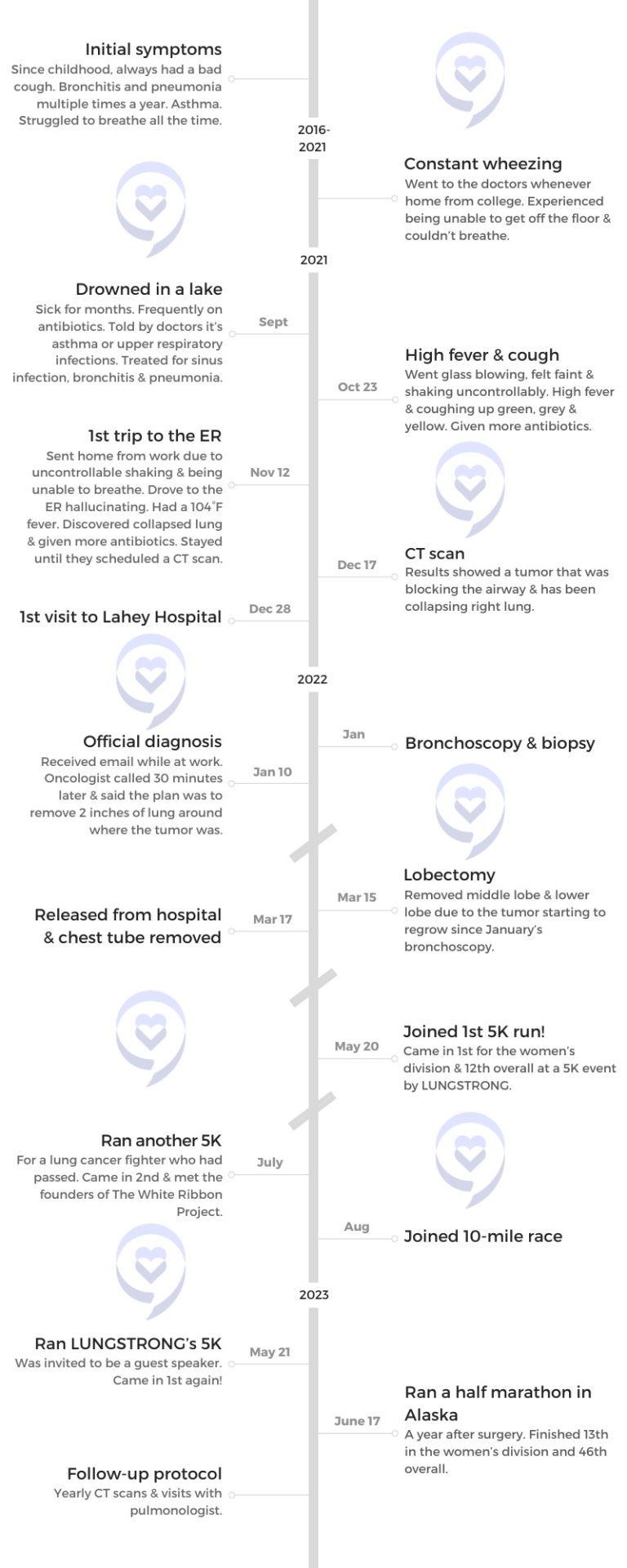
Celebrating a cancer-free milestone
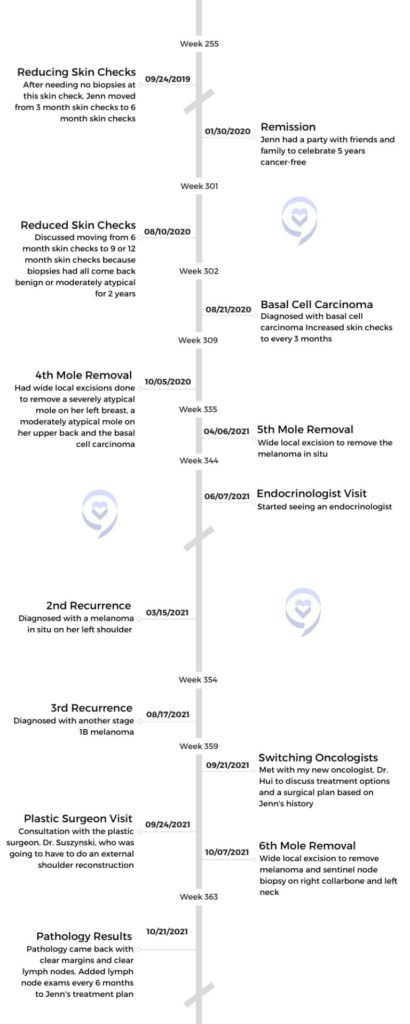
There was a pretty significant time frame between my first diagnosis in January 2015 and my second diagnosis in January 2020. In January 2020, I celebrated being 5 years cancer-free. I had a big celebration with friends and family at a local brewery nearby. We reserved a little space and set it up for drop-in for 2 hours. It was really special to have people from all different aspects of my life come and celebrate.
It felt like a huge accomplishment and I really needed to celebrate it because even though your melanoma hasn’t come back, it doesn’t mean that you’re not having biopsies and surgeries at that point. I had already had a number of surgeries in between because of moderately and severely atypical moles where they needed to go in and get more to make sure it didn’t become cancer again, so that felt like a huge accomplishment.
Then 2 months later, things really shut down due to the pandemic. That was very challenging in a lot of ways at first from a mental health perspective. I live alone with my rescue cat and my sister was pregnant at the time, so I was limited access to her. My mom has an autoimmune disease, so our family had to be extra cautious. We really weren’t socializing at all. My entire social life disintegrated. We FaceTime and things like that, but it’s not the same as being in person.
Recurrence
Describe your experience with recurrence
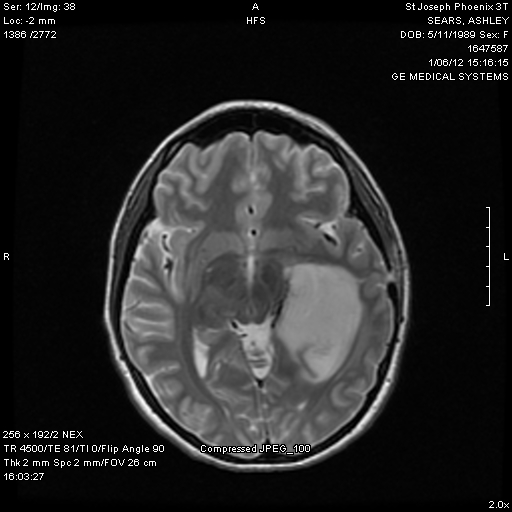
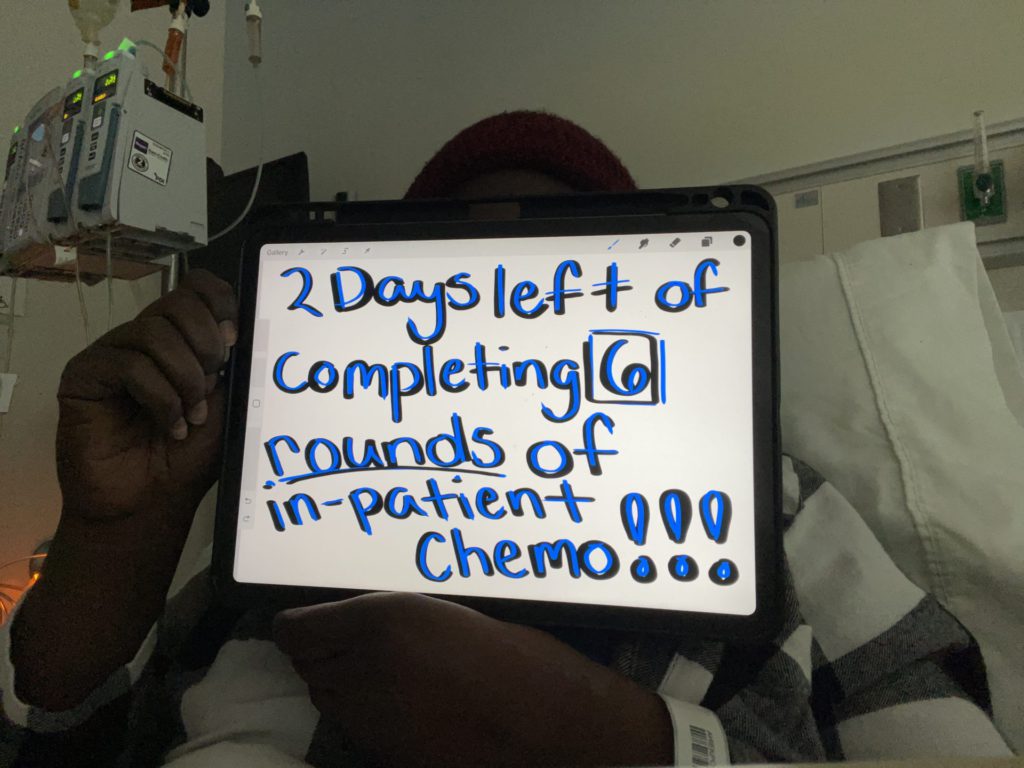
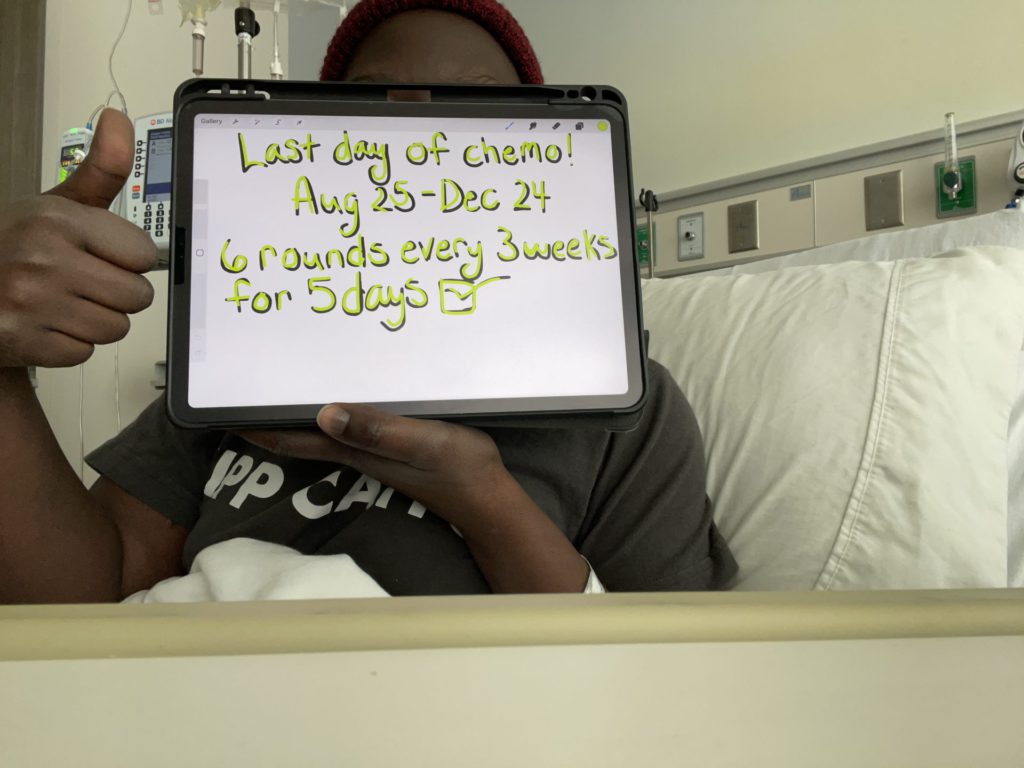
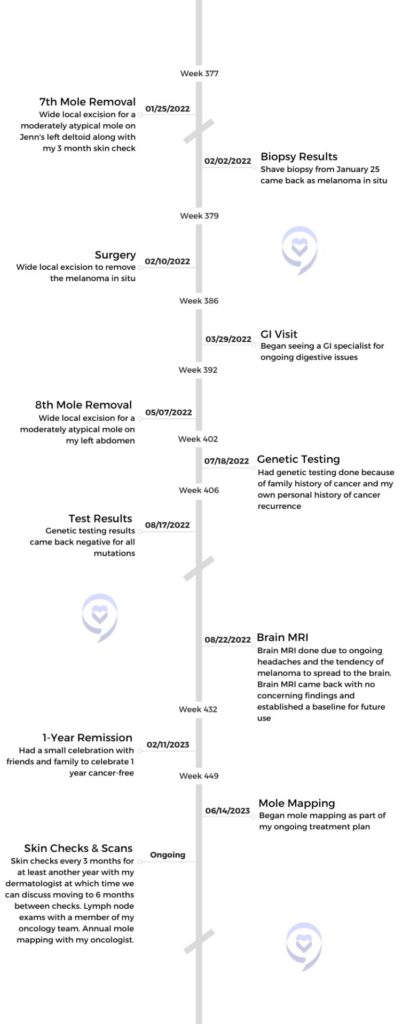
About a year later, while we were still very much in the effects of the pandemic in March of 2021, I received my second melanoma diagnosis. Because of my skin checks, which at that point we were up to 6 months skin checks because I’d been doing pretty well, we found a stage 0. They still do what’s called a WLE or wide local excision, which is a surgery. The difference with stage 0, I’m actually awake for it instead of under anesthesia because they don’t have to go in as deep or as wide. They don’t have to take quite as much skin.
That was the first of a very tough year for me. I had my third diagnosis a few months later in October of 2021. That one ended up being another stage 1B, so I did have to go under anesthesia with that one.
Because I’d had a stage 0 melanoma in that area, as well as 2 severely atypical moles removed, I had a lot of scar tissue and they can’t use scar tissue to help close up the wound. A plastic surgeon had to come in and I ended up having almost an entire external shoulder reconstruction where they had to, take the skin and shift everything in order to close it and take more skin than they normally would because they were cutting out some of that scar tissue. I actually have 1 scar that used to go up and down that actually now goes horizontally, which is the biggest thing that I can see now that really shows how much they had to do at that time.
About a year later, while we were still very much in the effects of the pandemic in March of 2021, I received my second melanoma diagnosis.
A few months later, I ended up having my fourth melanoma diagnosis, which was another stage 0 melanoma. So in 11 months, I had 3 recurrences. That was after 5 years, and with melanoma and a lot of cancers, I believe 5 years is a milestone. After you hit the 5-year mark, your chance of recurrence goes down. That was why I decided to have a party that year because it felt like I’d been holding my breath waiting to hit that 5-year mark, especially with all of the atypical moles and surgeries in between. It was like, okay, maybe we’re out of the woods. It was a weight lifted off my shoulders but I didn’t have long before that weight was right back.
How did you process your cancer recurrence?
I don’t know if I ever mentally processed it. I was very much in survival mode. Not as much after the first one because it was stage 0, so it felt like our plan is working. This isn’t ideal, I don’t want more melanomas, but we caught it very early. Stage 0 cancer is borderline precancerous so where it’s right on the edge of being a severely atypical mole and a melanoma. It felt like a setback but wasn’t as devastating as getting that next one in October.

I had just started my new job as the director of marketing in July of 2021. Then in October, just a few months later, having to tell them my cancer is back, I’m going to need some time off, I was facing a lot of uncertainty. This is my second one now in 6 months. That was a really difficult conversation to have. They were incredibly supportive, and they still are.
I continued to go to therapy but feel like I met with my therapist and cried on every visit. We talked a lot about how to live in those small moments because I couldn’t see a future past my next skin check. I was starting to ask, is this really going to be the rest of my life? Skin check melanoma, skin check melanoma. It wasn’t until the first skin check after that stage 0, the most recent one that I was able to let out a little bit of a breath. Everything came back benign in that one so we didn’t have to do any further excisions. Since then, I’ve had 2 skin checks where we didn’t do any biopsies.
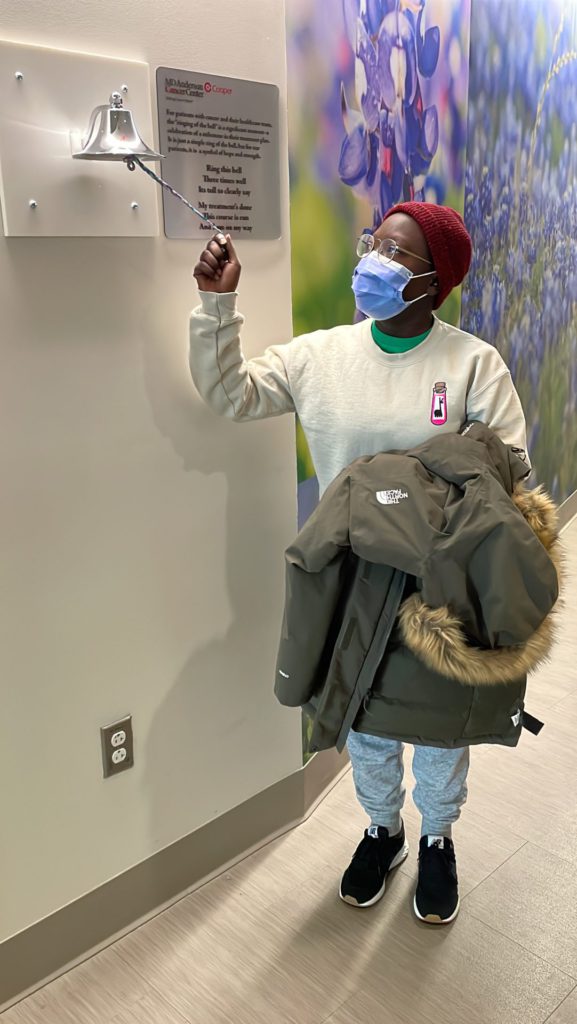
Being cancer-free for a year after 3 recurrences
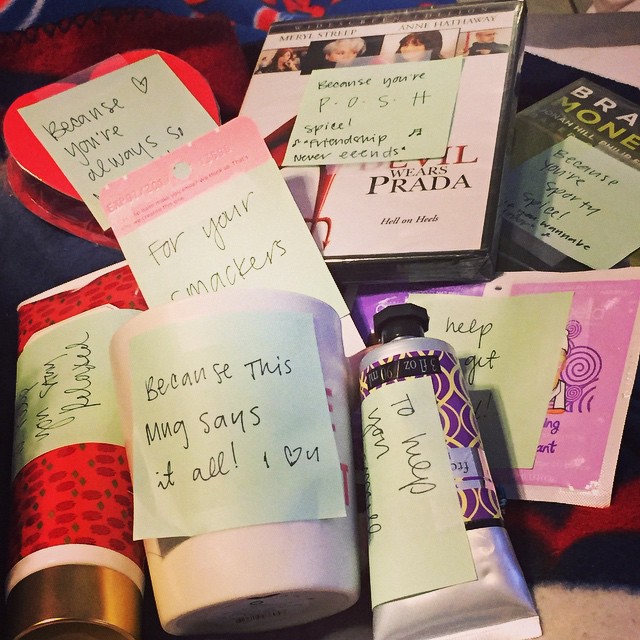
In February, on Valentine’s Day of this year, I celebrated 1-year of being cancer-free again and had a skin check the week before that anniversary date. It felt like there was so much pressure on that skin check. I did have one biopsy done at that one. The day before we had my celebration planned, I got the results back that everything was clear I was really able to celebrate with friends and family and had a smaller party.

In February, on Valentine’s Day of this year, I celebrated 1-year of being cancer-free again.
It was a smaller group, but it was really the people that had supported me. If my parents or my sister couldn’t be at an appointment, I have a group of friends that have a group text that I’m not in because they knew that I would never ask for help. When they knew I had an appointment that somebody couldn’t go to with me, they would coordinate among themselves and decide who was going to go and made sure I never went to an appointment alone. Things like that. Those are the people that I had there on that day.

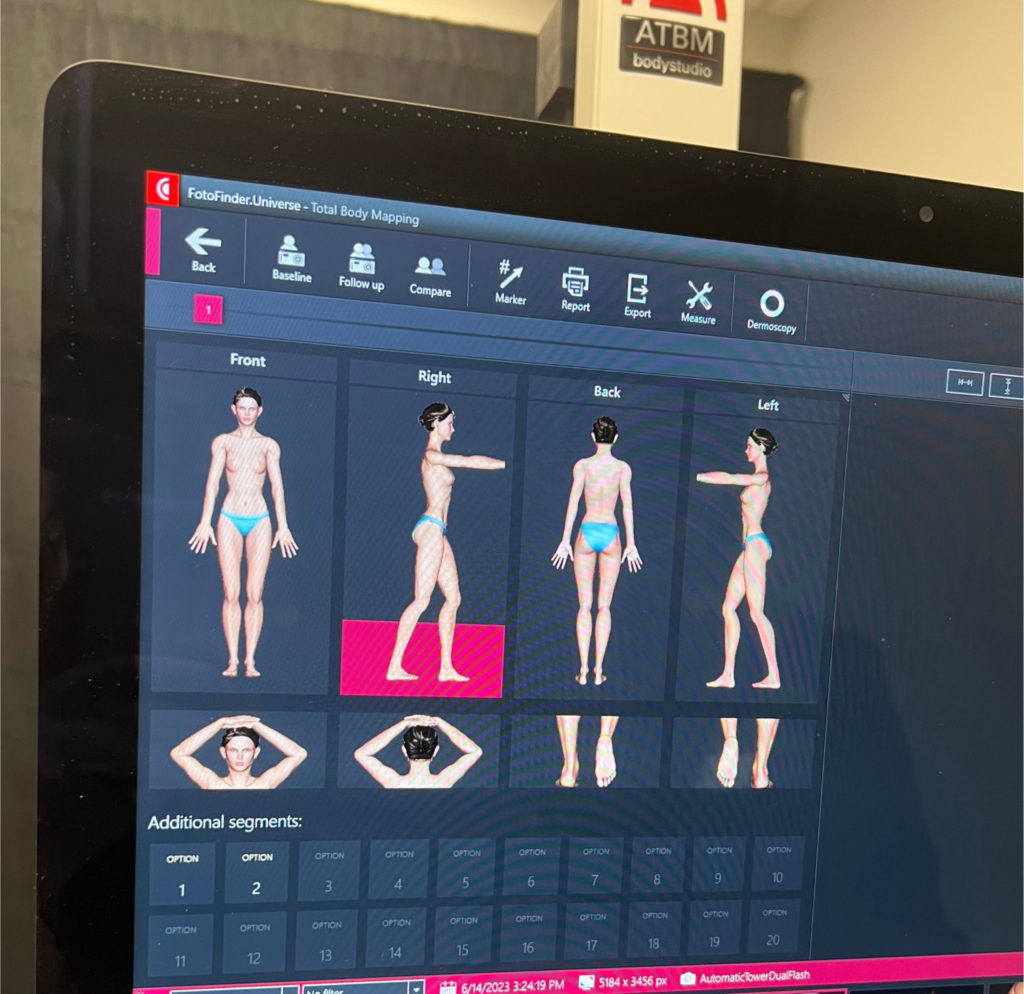
How often do you have skin checks now?
After my most recent stage 1B, we got more aggressive with my treatment plan. I’m still very fortunate that I’m not on medication for it or having to do immunotherapy, which is generally the common treatment with melanoma. In addition to my 3-month skin checks, which I’m currently on, the goal is to hit annual skin checks. It’s funny to feel like that’s such a huge achievement because that’s what everybody should be doing but I haven’t made it there since January 2015. The closest I’ve gotten is a discussion about going to 9 months.

The importance of having support on your cancer journey
Leading up to the skin checks, I always make sure I plan my therapy around those. That really helps. When I know I have a skin check, I will schedule a therapy appointment for the same week. Or if the skin check is at the beginning of the week, my therapy appointment will be at the end of the week so it’s less than a week away from the skin check leading up to it. That’s when I increase how often I’m going to therapy. Usually, about 2 weeks after my skin check, I’ll schedule another therapy appointment because that’s when we can expect that my results would have come in. It’s so helpful to know that I have this person to talk to and process all of those feelings and no matter what happens, I have that extra support system behind me.


Talking to family, knowing that that group of friends is there to make sure that I’m not going alone…It’s partly for the emotional support, but also it’s helpful to have somebody after if they biopsy something on my back and I have to get dressed after. I’m extra grateful because, after COVID, they would go with me but they would have to sit in the car. I had to go in by myself for a really long period of time.
Dealing with scanxiety
In a weird way, that year has made me more comfortable in survival mode than not. That’s something that I’ve really been working through in the last year and a half, figuring out how to live for the future and not for the next melanoma.

It’s interesting too, because I find that a majority of my scanxiety comes leading up to the skin check. No matter how many biopsies they do, there’s still that sense of relief, because that’s the part that unfortunately, I’ve become most comfortable with. I’m like, okay, so now from here I know what happens. They’ll either come back moderately typical, we’ll do this or it’ll be severely atypical and we’ll do this. I know how to handle what happens after. I don’t know how to handle the uncertainty.
Going into the skin check is actually harder than waiting for the result. It’s almost a relief even if they do a biopsy and I don’t usually feel nervous until I get to the point where I know the results could be coming any day. I just want to know so that I know what we’re going to do and implement a plan. In a weird way, that year has made me more comfortable in survival mode than not. That’s something that I’ve really been working through in the last year and a half, figuring out how to live for the future and not for the next melanoma.
Reflections
What were your feelings about being outside post-melanoma diagnosis?



Shortly after my first melanoma, about a month after I moved back home, my family went to Disney World on vacation in Orlando, Florida. It was April or May, but Orlando, Florida in early summer or late spring, you think of sun, being outdoors, and beaches. That was really difficult because I was like, how do I go on this trip and enjoy the trip and not hang out by the pool with my family? I bought 100+ SPF and was putting it on every 5 minutes. I was terrified to be outside at the theme parks. I would find a patch of shade and run to it while my family waited in line. There was a lot of fear initially.
The importance of sun protection
SPF or UPF clothing has been incredibly helpful because reapplying sunscreen throughout the day is so important but that’s a lot easier if you’re at home or even at a cabin versus in a theme park where you’re getting in lines. You can only bring so much in. UPF clothing is really helpful. Sunglasses are so important and you want to make sure that they have 100% UV protection. You can even get cheap sunglasses with that.



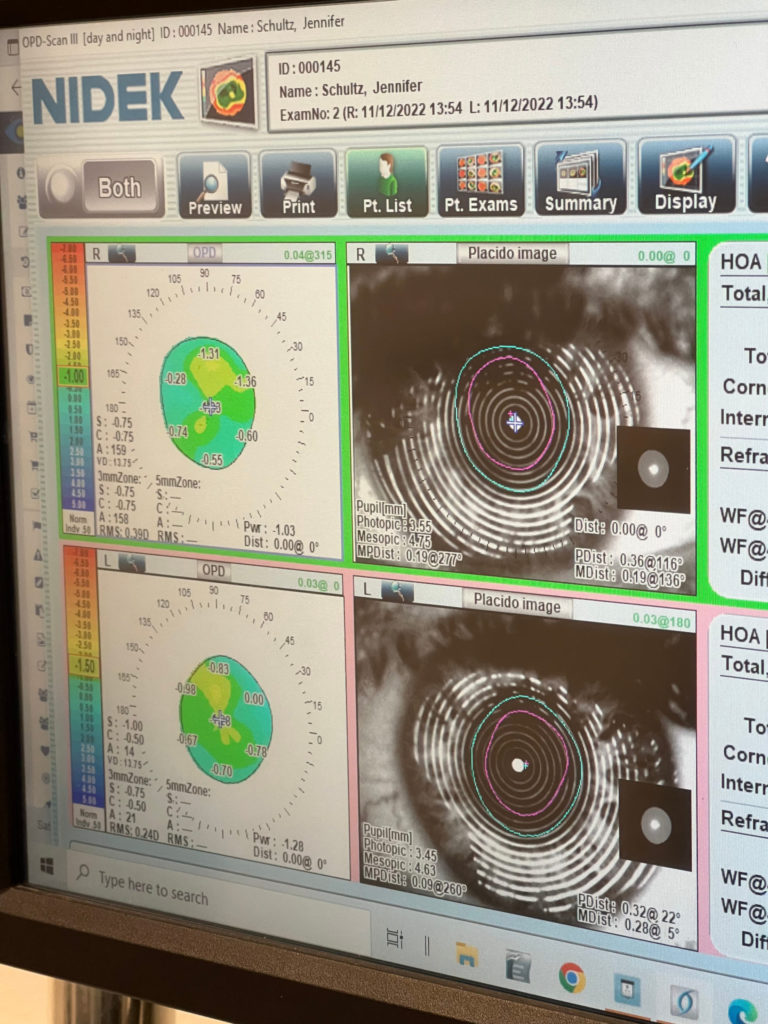
One thing that I didn’t know until after I was diagnosed is that you can get melanoma in your eyes, so even my annual eye exams are extra important. They do the 3D imaging now instead of dilating my eyes at every appointment, so my eye exams have changed.
Also, wear a hat any time you’re outside because even if you put sunscreen on your scalp, the sun is beating down on the top of your head and the tops of your ears, the back of your neck. Wearing a hat, especially a wide-brimmed hat, is so important if you’re going to be outside.
If you can, avoid peak sunlight hours. Typically that’s between 10 a.m. and 2 p.m. when the sun is hottest. I’ve learned a lot about the UV index, which ranges from 0 to about 12. You’ll very rarely see it get that high, but at a 0, it’s very safe. It’s usually right away in the morning or at dusk where the intensity isn’t as high. The higher it gets, the more often you have to apply sunscreen, and the more you should seek shade wearing those extra layers of clothing, sunglasses, hats, and stuff like that.
It’s actually really cool. I didn’t even know it was on there. But on almost any weather app, if you scroll down, it’ll actually tell you the UV index at any time of the day, so that’s been really helpful. Sometimes if I’m outside and I’m like, do I need to put on more sunscreen? I’ll check the UV index. It’s a helpful tool to base that on.
How previous sunburns can be a precursor to melanoma

A lot of people think if they use tanning beds, it’s safer, and it’s actually not because there are UVA and UVB rays and tanning beds have the type of UV rays that are less likely to make you burn, but more likely to give you skin cancer.
It was very frustrating for a while knowing that I was doing all of these things and the melanoma was still coming back. It also stresses the importance that no sun damage is reversible. I think there are a lot of times where my tan faded or I got sunburned, but I put on my lotion and my aloe vera and it’s healed but our skin remembers every bit of sun damage that we’ve ever had. So my melanoma isn’t coming back because I haven’t been doing enough, and maybe it wouldn’t have happened had I taken better protection from the sun earlier, but it’s really leaning into everything that I can do now to lower my risk from what it already is.
There’s a stat that I want to say is, 2 blistering sunburns before the age of 18 can increase your risk of skin cancer by over 50%. A lot of people think if they use tanning beds, it’s safer, and it’s actually not because there are UVA and UVB rays and tanning beds have the type of UV rays that are less likely to make you burn, but more likely to give you skin cancer. There’s a lot of misinformation surrounding that right now, which is also really important. There’s so much information and misinformation around tanning that’s really hard to hear. Especially at the beginning of the year when gyms are using unlimited tanning to sell gym memberships.
What advice do you have for someone on their cancer journey?



There are 2 pieces of information that I would give to somebody going through a diagnosis. The first one, and I hear it a lot from others who have experienced cancer as well, believe in yourself and advocate for yourself. If a doctor tells you that you’re wrong, never be afraid of getting a second opinion. Nobody knows your body better than you do. If something doesn’t feel right, and maybe it’s not, have a care team that you trust. That is so important. If you have any hesitations about your doctor, seek out a second one. The worst thing that happens is it’s nothing, but you would never want to not do it. It ends up changing the course of your treatment or you end up missing something or catching something later when it could really change the outcome.
»MORE: How To Be A Cancer Patient Advocate
The other thing is it’s so common to feel lost after a cancer diagnosis. We go through so much that it really changes us. It changes how you see yourself. It changes how you see your career, time with your family, and time in general. Try to change that perspective of, I’m lost and I don’t know who I am anymore, into this idea that you get to find out who you are now. Have fun exploring and trying new things and seeing what you love. You’re getting to know yourself all over again.



I felt a huge lack of control after my diagnosis, and something I never in a million years would have dreamed of doing was speaking to lawmakers in Congress. Advocacy work has given me so much purpose, and that’s not going to be the same for everybody, but that’s something I never even would have considered before my diagnosis. I get so much joy and purpose out of it and being able to take that frustration and lack of control and channel that into something that’s creating change for others facing similar experiences.
More Melanoma Stories
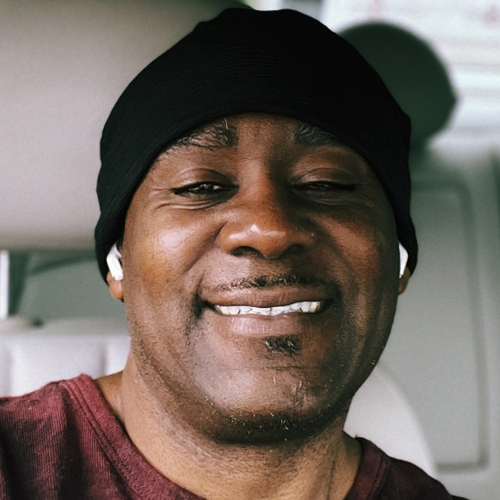
Ellis E., 3A
1st Symptoms: Changing mole on arm
Treatment: Lymph node resection, immunotherapy (Opdivo), targeted therapy (BRAF inhibitor)
...
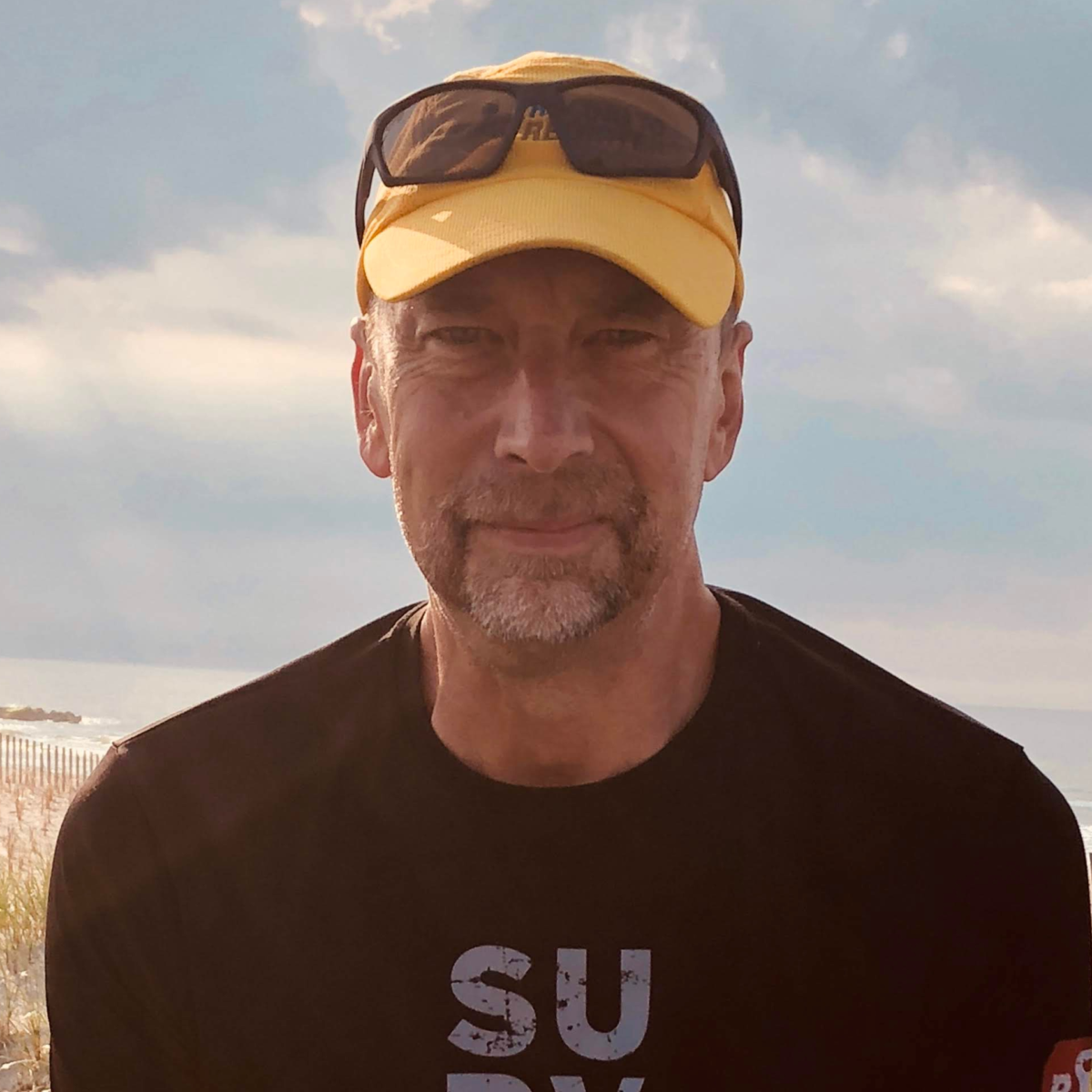
Rich B., 3B
Diagnosis: Melanoma
1st Symptoms:Suspicious, dark spots
Treatment: Immunotherapy (Nivolumab/Opdivo)
...
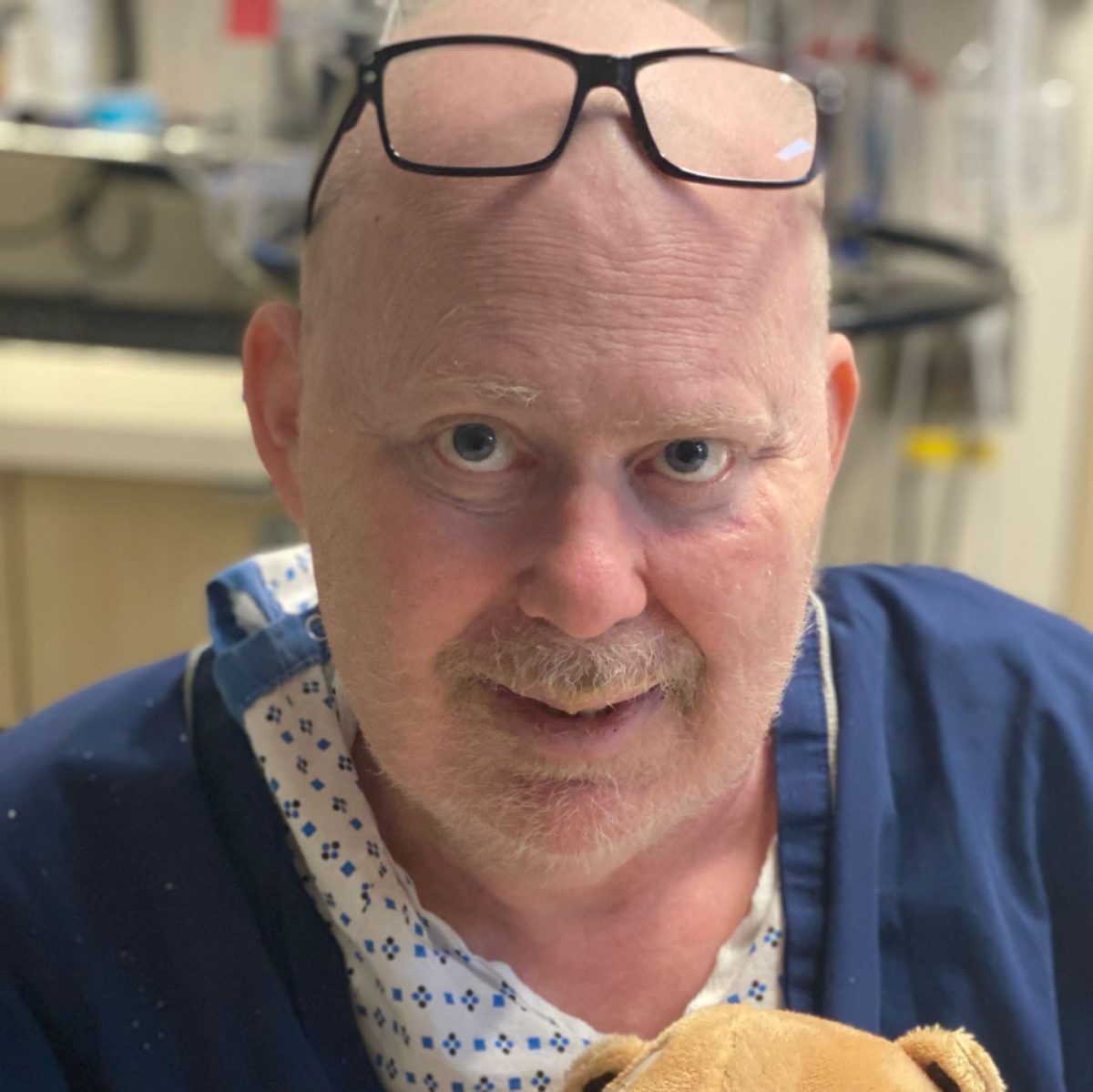
Amy H.
Diagnosis: Melanoma (4 bouts), Cervical cancer
Stage: Various stages (1-2)
Initial Symptom: Melanoma: Bad sunburn leading to scarring, Cervical: painful intercourse, cramps, pain during Pap smear
Treatment: Melanoma: Excision and Mohs surgeries, Cervical: partial hysterectomy
...