Hugo’s Stage 1 Colon Cancer Story
Hugo shares his stage 1 colon cancer experience. Hugo details his treatment path of surgery, steroids, and immunotherapy. He also dives into how his diagnoses (also diagnosed with testicular cancer) fueled his new passion in cancer advocacy.

- Name: Hugo T.
- Diagnosis: Colon cancer
- Staging: 1
- 1st Symptoms:
- Inflammation of bowel (worse than usual for someone with ulcerative colitis)
- Colonoscopy found polyp
- Treatment:
- Surgery
- Subtotal colectomy
- Emergency bowel surgery
- Steroid treatment
- Immunotherapy
- Vedolizumab
- Surgery
- First Cancer: Testicular cancer, stage 2B
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
It took me a while to realize how powerful it can be to share your story. I urge anyone out there, if you’re going through this yourself, I’ve found that it is really mentally healing to share.
The people you can connect with make you realize you’re not alone.
Hugo T.

Diagnosis
How did you find out about your cancer?
I had 5 years of clear CT scans from testicular cancer I had had. It was June of 2018, and I was probably the fittest, happiest, and healthiest I’d been in a long time. I was living in Brisbane with my lovely partner Amber. We celebrated this momentous milestone of the last 5 years and opened up a bottle of champagne.
It was one of the best moments of my life. It was very short lived. Two months later, I was scheduled for a routine colonoscopy. I got some unwanted all too familiar words.
He told me I had colorectal cancer. To find out 2 months after I had been 5 years in remission after testicular cancer was a punch to the gut.
Did you have any symptoms before the diagnosis?
When I say it was a routine colonoscopy, I’ve always had a history of bowel disease, but it’s been really mild. I’ve always had a bit of mild ulcerative colitis. Nothing that’s really affected me much, but enough to say I need 3 yearly colonoscopies just to stay on top of it and treat it.
This just happened to be one of those routine colonoscopies, but I had asked to push it up because my bowels were flaring up a little bit. I told my gastroenterologist, and he agreed to see me sooner.
When you go in, you’re in for a day, get a camera up the bum, and you have a look at what’s going on. Usually, you get the results back and happy dance. This was one different.
This colonoscopy happened to be a blessing in disguise because coincidentally it came back positive for bowel cancer. I don’t know what you call that — gut intuition or what — but I definitely listened to my body and thought that what was going on wasn’t normal for me.
How did the doctor diagnose the cancer?
The camera went up and saw a bit of inflammation, and there was also this big polyp. They’re usually benign, but sometimes they can be cancerous. It’s not common for a young guy, so my doctor sent it off for a biopsy.
After the colonoscopy, he said, “There was a suspicious polyp. It’s probably nothing, but I’ll see you in 2 weeks to go over the results.” At that point, bowel cancer did not cross my mind. I went to work the next day, and it just did not cross my mind.
It wasn’t until I got a call that afternoon from the doctor’s receptionist that said, ‘Hugo, the doctor needs to see you.’
I told her I wasn’t due for 2 weeks, and she said he wanted to see me that afternoon. As soon as I heard that, my stomach dropped. I got that really sick feeling, and I tried to stay positive.
I went to the appointment with my partner, and that’s when we got the news. The feeling of hearing that with her sitting next to me there at the doctor was a bit of a shock to the system.
How did you react to this diagnosis?
It’s interesting. It’s still pretty fresh and raw. The doctor was amazing and answered all the questions I needed to ask. I held it together pretty well, but I think mainly for my partner, I felt like I had to brave.
He told me the only course of treatment I needed to have then was to have my bowel removed. We spoke about the different options and how much of the bowel to remove.
Ultimately, I processed everything, but it wasn’t until I walked out of the doctor’s office that I completely broke down.
I reached a tipping point. I thought, ‘How can I go through this again?’
I had just beaten testicular cancer, and now I was about to go through this whole new cancer I knew nothing about.
One of the hardest things I’ve done was calling my family — my parents, my sister, and my twin brother. Having to say, “I have bowel cancer,” to my family while fighting back tears and hearing pain in their voice, you realize that cancer affects far more than just the individual.
I felt like I was causing my family so much more pain because of what I was about to go through. I felt like it wasn’t fair for them, just like it wasn’t fair me. It was a difficult moment, and it made it more real.
»MORE: Patients share how they processed a cancer diagnosis
Surgery & Recovery
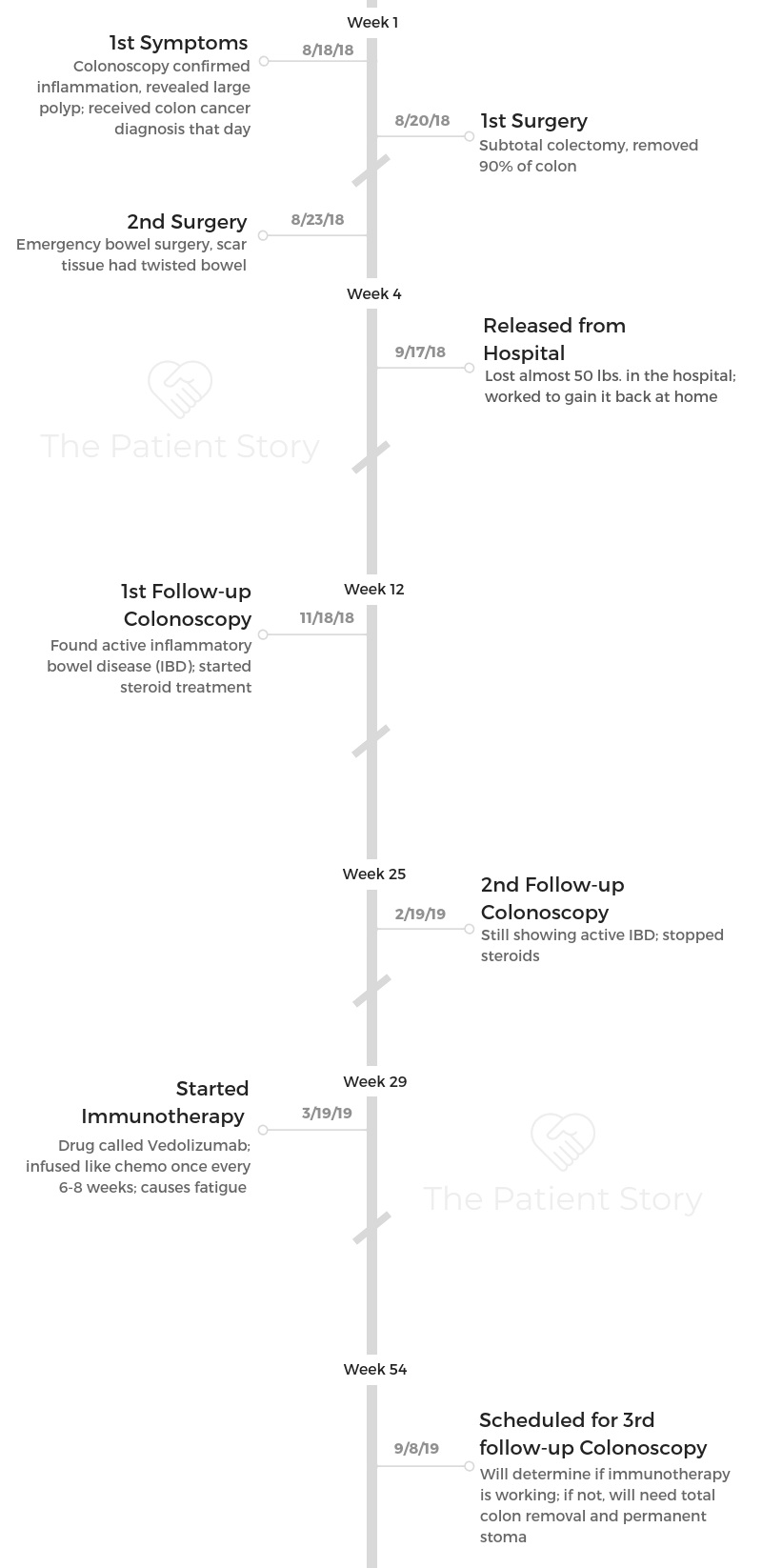
What were the next steps after diagnosis?
They moved pretty quickly. Bowel cancer kills more young Australians aged 24-29 than any other cancer. It is Australia’s second biggest cancer killer behind lung cancer. It does kill a lot of people.
That’s why they moved very quickly. They said it seemed to be contained to the bowel, which was fantastic, but they had to operate very quickly.
Within 2 days, I had what’s called a subtotal colectomy, which is basically surgery to remove most of my colon. They removed about 90% of my large bowel — my colon, which is connected to the rectum. That’s where the cancer was.
What was the subtotal colectomy recovery like?
I had the first surgery where they took the bowel out, and I recovered pretty well. I had a catheter, the poo bag, the gastral tube, and pain relief, and I was recovering well. Then I started going downhill quickly, just as I was getting ready to be discharged from the hospital.

Immunotherapy
Why did your doctor start you on immunotherapy?
I had a follow-up colonoscopy after the surgery that confirmed that there was no active cancer. Because I didn’t have my whole bowel removed, I didn’t require a stoma or a colostomy bag.

Since I’ve still got a bit of inflammation, and they said that’s likely what caused my bowel cancer in the first place, the doctor said I’m at such a high risk of getting colon cancer again. He basically said, “It’s more so when you get cancer again, not if, if you don’t treat this inflammation.”
What’s the immunotherapy like?
It’s relatively new on the scene. It’s an extremely expensive drug. It hasn’t had a lot of evidence-based studies done about it, but the evidence it has had is very successful. I’m in that situation where I’ll try anything to avoid a bag and avoid getting cancer again. If this doesn’t work, I’ll take the next step.
Essentially, I go to the hospital for a few hours once every 6 weeks. It’s not toxic like chemo, but it’s still a heavy drug. Every 6 to 8 weeks, it’s an infusion where they hook you up like chemo. One hour, you’re getting infused, and the others you’re getting some fluids.
Where chemo targets all your cells, including healthy cells, this targets only the inflamed cells in my stomach. It doesn’t suppress your immune system. It actually boosts it, so it’s quite interesting. It is a common treatment that they have for people who have Crohn’s or ulcerative colitis. I know they can use it to treat melanoma as well.
Hopefully, it does its job, and I won’t require another surgery, but I will have a follow-up colonoscopy in a couple of months. That’s the important one.
That will show whether it’s been working or if I will need a stoma or a colostomy bag for the rest of my life. It’s a lot to take in for a 27-year-old, but I’ll do what I have to do.
»MORE: Read more patient experiences with immunotherapy
What hoops did you have to jump through to get on it?
The big one is if they try to put you on immunosuppressants, which is the opposite of immunotherapy. That’s what they want you to go on before you get on this drug, because this is really expensive.
However, I skipped that hoop because it’s been proven that being on immunosuppressants can increase your risks of getting blood cancers. Because of my medical history, I said that it seemed ridiculous to go on immunosuppressants. You have to go to the board who says whether or not you meet the requirements for this drug, and they did agree in my case.
Since I still have active bowel disease, I fall into that category that is very suitable for this treatment. The concern is that my bowel disease, in what remains of it, is going to be the cause if I get cancer again. That’s the reason why I took the drastic approach to go on something like this.
A lot of people on this medication have severe bowel disease. I don’t, but I’ve got such a significant risk for colon cancer that I fall in the category of qualifying for this drug.
My doctor signed off on it, it got approved, and the Army signed off on it. I’m very fortunate they’ve been supporting me this whole journey. I’ve been on it for 3 cycles now, and I’ve got a couple more to go.
Do you have any side effects from it?
Mainly it’s just the fatigue. I’ve been through chemo, surgeries, and recoveries, and so this could be a lot worse. It does knock me around a bit with the fatigue, but apart from that, it’s 10 times better than what I experienced with chemo and surgeries.
Next Steps
What’s your next course of action?
If this medication proves to be suppressing the inflammation and it’s working, then I’ll stay on this for the foreseeable future. If there’s still inflammation and it hasn’t suppressed it at all, I’m at such a high risk for colon cancer that I’m essentially gambling with my life.
We’re not talking about colostomy bags or further treatment; we’re talking about life or death. That’s the brutal fact of it, so if it doesn’t work, my doctor recommended removing the rest of the bowel.
If that happens, I’ll just have to take the recommendation and live the rest of my life with a stoma and colostomy bag.

Do I want that at 27 years old, and would it ruin my Army career? No, I don’t, and yeah, it probably would. But when you’re talking about your life, it’s a pretty small compromise.
What would the colostomy bag be like?
Picture you’re eating. The food goes down, and it processes through your small bowel. Once it goes through there, it goes through your large bowel.
Your large bowel does a lot of the heavy digesting for those heavy foods. It then goes to your rectum, and that’s when it comes out and you have a bowel movement.
If I had the large bowel removed, I wouldn’t have anywhere for food to go after the small bowel, and I’d have to have the colostomy bag. Once it processed through my small bowel, there would have to be an external opening, where the small bowel literally comes out of my body, and they attach it to the bag. When I eat, it would come out into the bag.
It doesn’t sound ideal, but believe it or not, advancements have come a long way, and people can live pretty normal lives with it.
Do you have any advice for people reading this?
From me, being proactive, we caught it early. That was paramount. Learn to know what your normal is, because my normal was different than someone else’s normal. When something’s outside of my normal, I go get it checked.
The difference with early detection is that it can quite literally save your life. It saved mine.

How has your cancer experience fueled your work?
It took me a while to realize how powerful it can be to share your story. I urge anyone out there, if you’re going through this yourself, I’ve found that it is really mentally healing to share. The people you can connect with make you realize you’re not alone.
There’s so much campaigning and support for older people living with cancer — which is fantastic — but I don’t feel like there’s enough awareness for young adults for living with cancer. That’s what prompted me to start an initiative, a movement, and maybe one day a foundation.
It’s called 25 Stay Alive. Rather than waiting until we’re 50 to be proactive with our health, I think it should be in our 20s. That’s when we should start being aware of changes to our bodies, because I’ve had 2 types of cancer in my 20s.
I know so many other people who have had cancer in their 20s. If they had waited until they were 50, life would be very different.
I’m all about knowing your body, knowing yourself, and being proactive. There’s no shame in seeking help. That’s pretty much what 25 Stay Alive encompasses, and I’m really passionate about continuing that awareness.
If, for nothing else, to change people’s perspective. You might not be going through cancer, but you might hear my story, and it might change your perspective and help you see, “I’m pretty healthy. I’ve got my health. Let’s keep it that way.”

25StayAlive’s Instagram
25StayAlive’s Facebook Page
Inspired by Hugo's story?
Share your story, too!
Colon Cancer Stories
Jackson A., Colon Cancer, Stage 3
Symptom: Sharp abdominal pain
Treatment: Surgery (emergency transverse colectomy)
Jay W., Colon Cancer, Stage 4
Symptom: Occasional presence of blood in stool
Treatments: Chemotherapy, surgery (installation of port and liver infusion pump, colectomy, hepatectomy, liver ablation, removal of liver infusion pump)
Kelly C., Colon Cancer, Stage 4
Symptoms: Constipation, bloating, severe abdominal pain
Treatments: Surgeries (colectomy, colostomy, hepatectomy), chemotherapy
Marc Anthony S., Lynch Syndrome and Colon Cancer, Stage 2A
Symptoms: Blood in stool, severe constipation, persistent exhaustion, constantly feeling cold
Treatment: Surgeries (sigmoid colectomy, lymphadenectomy)
Crystal W., Colon Cancer
Symptoms: Blood in stool, intermittent severe lower abdominal pain, urinary tract infection (UTI) with strong odor, fistula
Treatments: Surgeries (cystectomy, oophorectomy, and hysterectomy), chemotherapy
Albita G., Colon Cancer, Stage 4
Symptoms: Blood in stool, pain during defecation, constant constipation, steady weight gain in the midsection despite exercising
Treatments: Surgeries (colectomy, hepatectomy, hysterectomy), chemotherapy, radiation