Dania’s Stage 4 Colon Cancer with Liver and Peritoneal Carcinomatosis Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

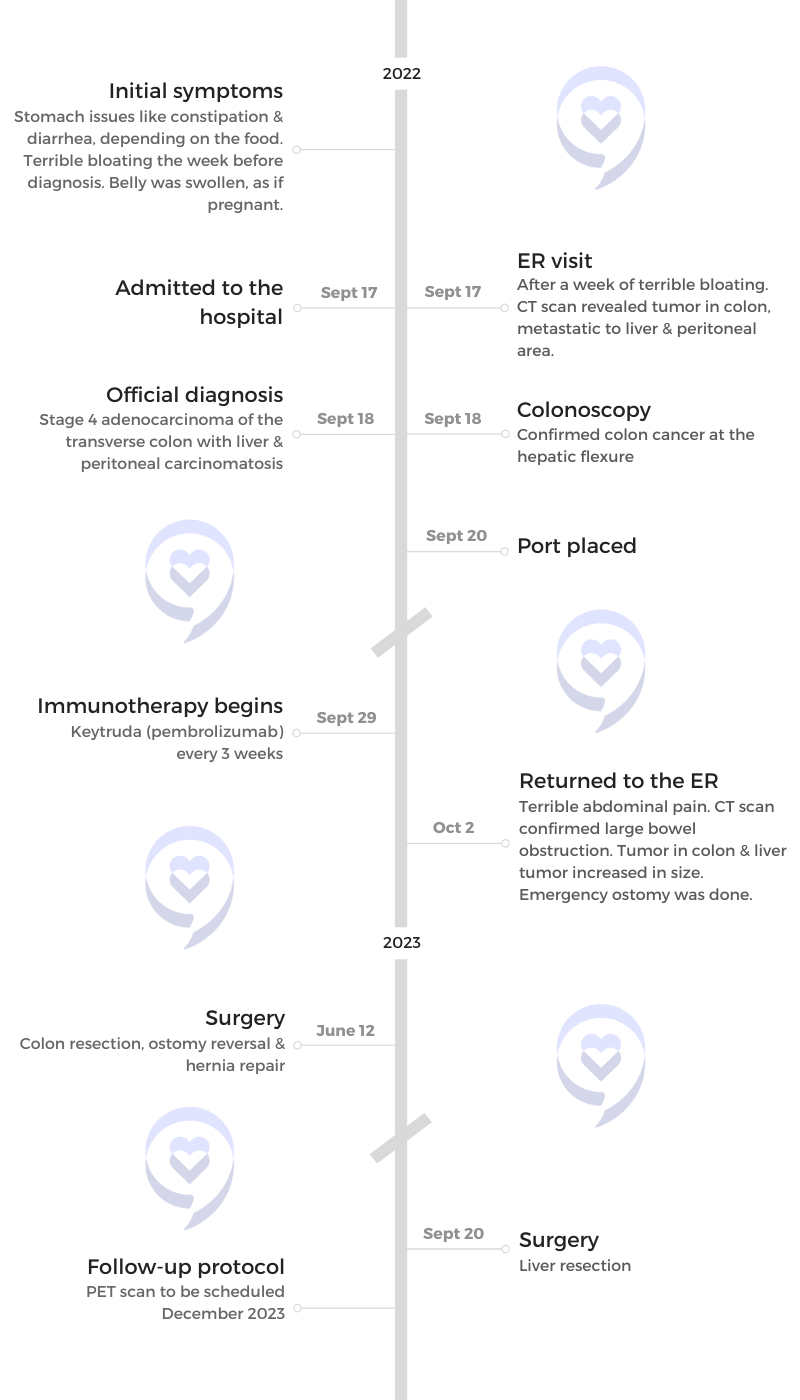
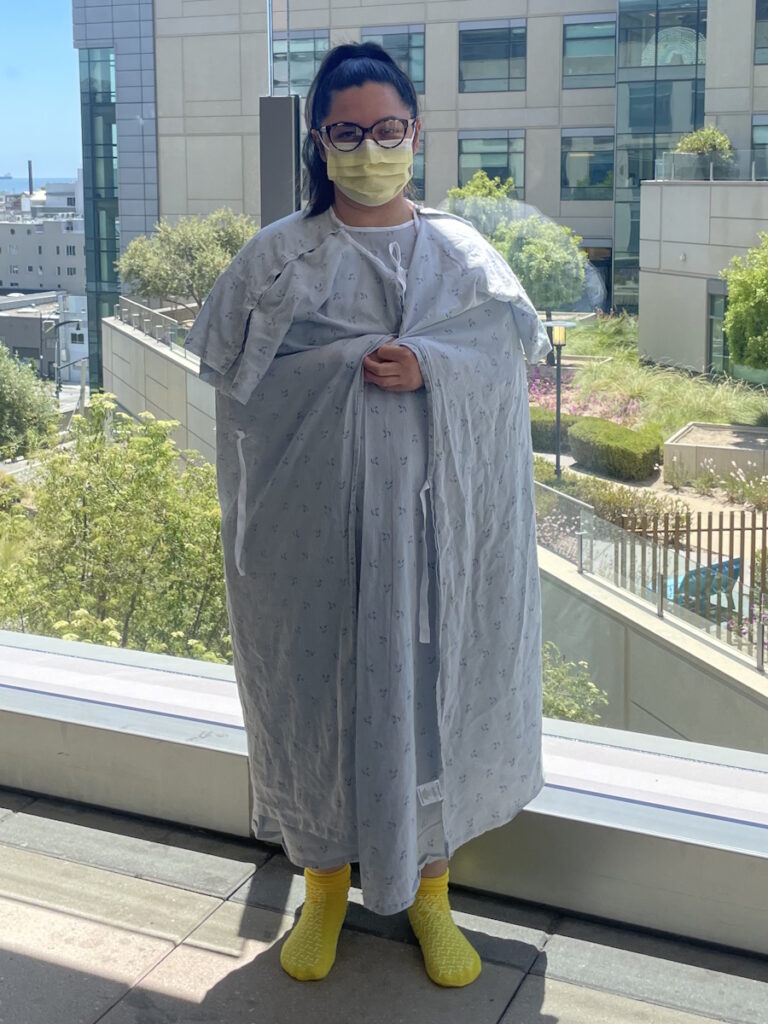
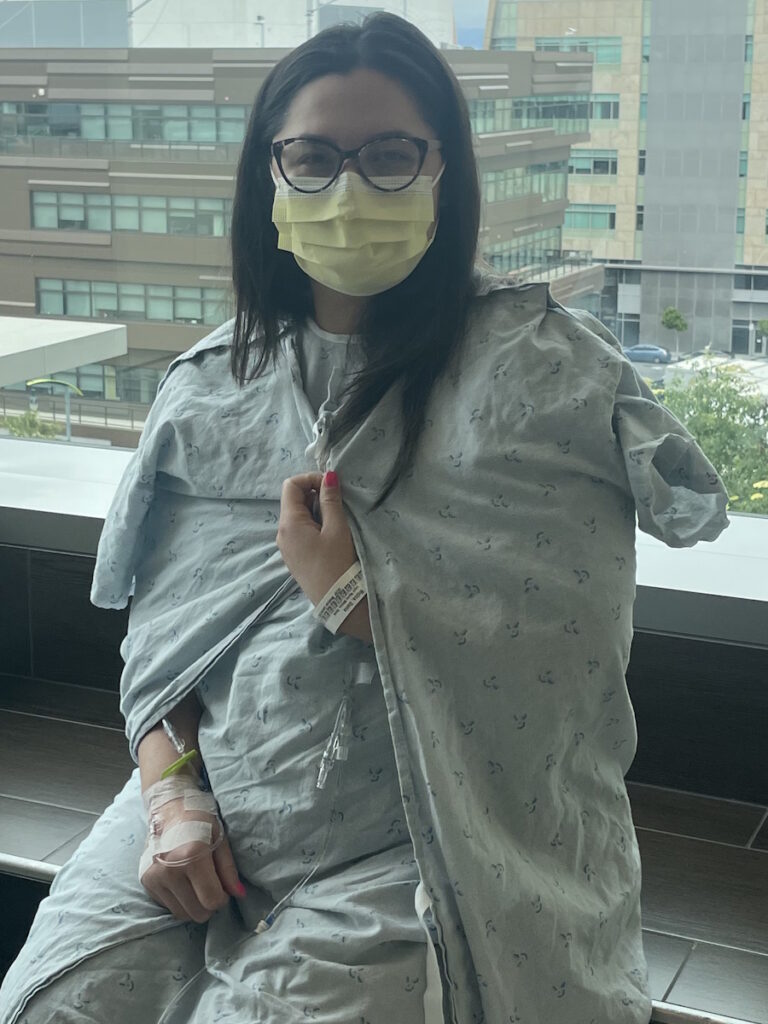
Dania, a 35-year-old mother of three, shares her journey of being diagnosed with stage 4 colon cancer that spread to her liver and peritoneum.
She experienced stomach issues since childhood but didn’t seek medical attention until her symptoms intensified. A visit to the emergency room revealed the shocking diagnosis of colon cancer. The news was initially overwhelming, but her faith and acceptance helped her face the challenging road ahead.
She began immunotherapy with Keytruda, responding well and experiencing minimal side effects. However, she faced complications, including a blockage that required an emergency ostomy.
During this time, Dania and her family made significant life changes, moving closer to her husband’s family for additional support. Her husband played a crucial role as her advocate, utilizing his medical knowledge to navigate the complexities of cancer care.
She emphasizes the importance of not taking health for granted, urging others to be proactive about their well-being. She advocates for increased accessibility to colonoscopies and encourages individuals to speak up and be persistent in seeking medical attention if something feels wrong.
In addition to Dania’s narrative, The Patient Story offers a diverse collection of colorectal cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Dania M.
- Diagnosis:
- Colon cancer
- Staging:
- 4
- Initial Symptoms:
- Stomach issues like constipation & diarrhea, depending on the food
- Terrible bloating the week before diagnosis
- Belly was swollen, as if pregnant
- Treatment:
- Surgeries: colon resection, stoma, hernia repair, liver resection
- Immunotherapy: KEYTRUDA (pembrolizumab)
Introduction
I’m 35 years old. I have three kids, ages 17, 12, and three.
I’m married. My husband works in the medical field. He used to be an oncology nurse, but he’s a case manager now so he’s still in the medical field but in a different branch.
I was in school prior to being diagnosed. Now I’m volunteering. I love volunteering at my church. I teach catechism and found that I really love working with children, especially adolescents.

I didn’t have alarming symptoms that made me think of cancer.

Pre-diagnosis
Initial Symptoms
I have always had stomach issues since I was little. Food wouldn’t sit right. I would eat carbs or bread and it would hit me hard in my belly then it would take days for my belly to go back. I’ve dealt with it for years and learned to live with it.
I learned what food would hurt me. If I ate it, I knew I was going to suffer later. I never thought to have it checked out or think that wasn’t normal. I didn’t have alarming symptoms that made me think of cancer, not until September.
Symptoms Intensified
We went to a wedding where I ate a lot of carbs and drank wine. At the end of the night, I felt a strange pain in my stomach, but I thought, It’s the food. I ate a lot today. Not the best, not the healthiest. I knew the process. It would take a few days of cutting out foods that hurt me and sticking to a clean diet so my stomach would get back to normal.
Only this time, it didn’t. The following day, I woke up feeling very bloated and uncomfortable so I thought, Maybe one more day, but it went that way the whole week. My husband, being a nurse, said, “This is strange. You shouldn’t be feeling this way. Not after a week.” He kept telling me to go to the ER, but I was hesitant because my idea was that the ER is for life or death and I didn’t feel like this was such a situation.
Scheduling a PCP Appointment
I made an appointment with my regular doctor. This was September. They didn’t schedule it until October. My husband said, “No, you need CT scans. You need additional testing.”
Finally, Saturday came and this was a week from the prior Saturday when I felt that sharp stomach pain. I woke up and was still feeling really uncomfortable. By then, my tummy looked a couple of months pregnant. It was so bloated and uncomfortable.

‘Everything looks good. Your blood work looks good. The real way to find out what’s going on is through a CT scan.’

Emergency Room Visit
I turned to my husband and said, “You know what? I should probably go to the ER.” He asked if I wanted him to come with me and I said, “No, it’s fine. I’m sure I’ll be back by noon.” We were having this conversation at around 8 or 9 o’clock. I even said, “Be ready. Maybe we can go out for breakfast or late brunch after.” I was thinking they were going to diagnose me with gastritis or some type of stomach issue.
I went to the ER and checked in. I even felt bad because there are other people who are sicker and here I don’t even have pain. I was bloated. Luckily, it wasn’t busy so they admitted me quite quickly. They did all the regular testing and blood work. Everything came out fine.
The doctor comes in, starts examining me, touches my belly, and we start talking. He was feeling the bottom portion of my belly and he said, “You know why I’m feeling there, right?” I said, “Yeah, in case my appendix is doing something.”
He said, “Yeah. Everything looks good. Your blood work looks good. The real way to find out what’s going on is through a CT scan. The only thing is that you’ll be exposed to radiation.” I said, “That’s fine. Let’s do it.”
Getting a CT Scan
He does the CT scan. I was still waiting by myself. I have the app for that particular medical group so I can get my results before the doctor can come in and tell me.
I had been looking at my blood test results, taking screenshots, and sending them to my husband who was home with my two girls. My 17-year-old son was out of town at the time. I thought, Maybe my CT scan results are in, so I check and they were.
Getting the Results
Everything was broken down. I didn’t understand the medical terms so I scrolled to the bottom because I knew it would have a conclusion where they give you the bigger picture.
I felt like a bucket of water had been thrown my way. I felt my heart skip a beat and drop. I don’t remember the exact words, but all I remember are the words “cancer” and “tumor.”
All I remember is him saying, ‘This is going to be a long road. There are so many things being done for cancer now.’
Diagnosis
Reaction to the Diagnosis
I froze. I took a screenshot and sent it to my husband. He immediately called me and I could hear the panic in his voice. He said, “Calm down. Everything will be okay.” I remember shaking. I was in shock.
At that moment, the doctor comes in. Poor guy. I’m sure that the last thing he wanted to do at that moment was tell a 33-year-old that she had colon cancer. I actually felt sorry for him. I’m sure it was hard.
I had my husband on speaker and I remember the doctor showing me my file. He asked, “Is this you?” I nodded. My eyes were glassy. I wasn’t crying yet, but I was about to.
He pulled up a chair and sat next to me. I honestly don’t even remember what he told me. All I remember is him saying, “This is going to be a long road. There are so many things being done for cancer now.”
Processing the Diagnosis
I was trying to process what I read. At that moment, my husband raced over to the hospital. He started calling my mom, my dad, and my siblings, and they all arrived and were very supportive.
Looking back, I don’t know if this was a symptom, but my stomach was so irregular. If I ate something like carbs, I would get constipated. If I did have blood in my stool, I thought it was constipation because it was so hard to go to the bathroom. It wasn’t something that would scare me or be a red flag.
Cancer never went through my mind. Nobody in my family has had cancer, any type of cancer. I’m the first one so it was a shock to everybody in my family.
I remember having a conversation with God and saying, ‘I give this all to you. I don’t know what my journey will be like, but I hand it all over to You. Whatever happens, let me have peace. Let my family have peace. You’re completely in control.’

Looking Back
Around that time, I remember being frustrated with everything and being uncomfortable with my stomach. I remember saying, “I’m going to make an appointment and get to the bottom of this. Maybe it’s a food allergy. Maybe I have something. Food isn’t sitting right. It’s hurting me. I shouldn’t be having this much pain or struggles with food. I should be able to eat normally and not have a bloated tummy immediately after eating.”
I remember saying, “I’m going to schedule an appointment. Maybe a nutritionist. Maybe I’ll see my doctor and she can run some tests or refer me to a specialist to see what it is that I have.”
They say that it’s such a silent killer. It doesn’t get diagnosed until it’s causing damage. At this point, it was already causing issues with my colon.
Admitted to the Hospital
After that, I was hospitalized for three days where they did a colonoscopy, a biopsy, and everything. I remember being on cruise control. I never really broke down and cried. I feel like I accepted it.
Leaning on Faith
I’m a practicing Catholic so my faith is a big part of my life. I don’t remember what procedure it was. It might have been my colonoscopy because I was going to be put to sleep.
I remember the countdown and having a conversation with God and saying, “I give this all to you. I don’t know what my journey will be like, but I hand it all over to You. Whatever happens, let me have peace. Let my family have peace. You’re completely in control.”
As I fell asleep, I felt so much peace. It helped me stay calm. At that time, I didn’t know what the stage was and where I was with the diagnosis. All I knew was I had a tumor and I had colon cancer, but I had a lot of peace after that.
I decided that I wasn’t going to be angry because being angry was going to feed this monster. I wanted to do what I needed to do. I gave it all up to God and I felt a freedom after that.

My children were going to see me at my sickest and that’s the only thing that tore me, but I was at peace.

Treatment
Discussing the Treatment Plan
At the ER, when the doctor came in to talk to me, he asked if I had any questions. At the time, I only had one. I asked, “Is it going to hurt?” I wanted to be prepared. I’m the type of person where I like to know.
I don’t remember exactly what he said, but he said, “That’s a very interesting question you’re asking. I usually get that a lot from older patients.” I don’t know what he meant by that.
I wanted to know what I was about to go through to prepare myself. I kept thinking my children were going to see me at my sickest and that’s the only thing that tore me, but I was at peace. I said, “Let’s go with it and see where I’m heading.”
Pathology Report
I was diagnosed on September 17th when I went to the ER. The next day, I received the pathology report, which confirmed the cancer. My tumor was at the top of my colon.
I don’t even remember them telling me. I remember briefly hearing conversations that it was stage 3 or 4. Finally, in one of my appointments and through seeing in my app, I saw stage 4 colon cancer with liver and peritoneal carcinomatosis.
Realizing the Gravity of the Situation
My husband was an oncology nurse and worked years in that department so he has been my biggest advocate. I understood that that was pretty late, but I didn’t understand the gravity of it.
I try not to Google because online, they will tell you the worst-case scenario and I didn’t want to know so much. I don’t think I understood what that meant until I had a conversation with my oncologist a few months down the road.
I was under the understanding that I would have surgery to remove the tumor and start treatment and all that. I asked the doctor when we would start thinking about surgery. She wouldn’t straightforwardly say we’re not looking at surgery, but the conversation led to that. Surgery was not on the table because my cancer had spread.
That’s when it hit me. My heart dropped. My husband was right next to me during the video call. After we hung up, I looked at him and asked him for clarification to see if I understood right and that’s when I broke down. I understood then that it was a lot more serious than I thought.

The CT scan confirmed that my tumor was blocking 98% of the colon. He said I would need an emergency ostomy.
Keytruda Immunotherapy Treatment
When I was diagnosed and while they were doing all those tests, they wanted to give me a first dose of chemo before leaving the hospital so they put in my port. My husband started talking to the doctors to see if I would be a good candidate for immunotherapy. The oncologist decided that they would wait for the pathology report to come back to see if I was indeed a good candidate and, thank God, I was.
I went home with the goal to start immunotherapy as soon as possible. I had my first immunotherapy on September 29th and that has been the only treatment I’ve been receiving.
I’ve been doing Keytruda. I haven’t had any side effects at all. I do feel a little tired, but compared to what chemo does to you, I’ve been so blessed. I am so thankful.
New Stomach Pains
I ended up going to the emergency room again at the beginning of October. It started with horrible stomach pain. It felt like contractions. I could not eat anything. The smallest thing I would vomit back up. My husband made me a smoothie, begging me to eat something.
I spent the whole Saturday in bed, in pain and extremely nauseous. We thought it was a reaction to the immunotherapy because I just had my first dose. But it was horrible. The pain was so excruciating.
On Sunday morning, my husband turned to me and asked how I was feeling. I said, “I don’t feel good. What do we do?” He said, “ER.” We headed to the ER. The same doctor that diagnosed me was there. As soon as he saw my name, he rushed into my room. After reading my symptoms, he had an idea of what the issue was.
He looked at me and said, “Remember that first day when I told you this would be a long journey and there would be some bumps in the road? This is just a bump.”
He thought it was a blockage. The tumor was already blocking the passage so I was eating, but nothing was coming out. The only way to confirm this was to have another CT scan and it confirmed that my tumor was blocking 98% of the colon. He said I would need an emergency ostomy.

My quality of life wasn’t good. I couldn’t do much. I couldn’t do basic tasks because I felt so tired. It hurt. I couldn’t lift.

Emergency Stoma Surgery
Having an emergency ostomy was harder than my cancer diagnosis because all of a sudden, I was pooping through a bag.
I had to learn how to clean it and how to take care of it. I’m a very squeamish person so this was a challenge for me. It was painful. To see part of my organ outside of my body was an adjustment.
But I have so much support. I would see my ostomy nurse two days a week. She would come to my house, help me change it, and educate me more on it. She was the sweetest lady. Love her. She was amazing.
She gave me my space. She understood that it was hard for me and let me drive this situation. She knew that I was struggling. She gave me time and, eventually, after baby steps, I was able to clean it. By the time we were done, I was doing it on my own and I learned to take care of it.
Prolapsed Stoma
Immediately after, I started having issues with my ostomy. It prolapsed so it was starting to come out. Mine started protruding. Eventually, it would get really big and would hang out. It was very painful. I started developing a pretty good-sized hernia right behind it. Once I lay down, it went back into my body.
It’s a blessing because, without this, I could have lost my life so I was very, very thankful for it. But it was very uncomfortable. I had to use a waistband to keep everything in place.
My quality of life wasn’t good. I couldn’t do much. I couldn’t do basic tasks because I felt so tired. It hurt. I couldn’t lift.
I said to my oncologist, “We have to fix this because this is not a good way to live. My future is so unknown. I want to be able to go to the park. I want to be able to do stuff with my kids. I want to make memories.” The conversation started happening about referring me to another oncologist for a second opinion to see what we could do.

We were heading in the right direction. This is from surgery being off the table to removing this tumor. It was such a blessing.

Getting a Second Opinion
The goal was to see if I could have surgery to replace the ostomy. I was referred to UCSF and I spoke to a doctor there via video chat. He saw my chart and said, “I don’t see why we couldn’t have surgery for this.” He said that we could pause immunotherapy and then have surgery, but he said that he would refer me to a surgeon there because they would know best.
I was referred to a surgeon and she was amazing. She gave me the worst-case scenario and the best-case scenario. After seeing everything, she said that she would try to see where the tumor was, and if everything wasn’t in my favor, she would remove the tumor or do a colon redirection and repair my hernia.
But if she goes in there and everything looks worse than what the CT scans have shown, then she would close up the stoma and place it somewhere else where it wasn’t likely to prolapse or cause another hernia. She said that as long as I had the tumor, the ostomy had to stay in.
I have been responding really well to treatment. Everything had shrunken significantly. But because of scar tissue and not knowing, we didn’t want to risk reversing the ostomy, having to go to the emergency room again with the same problem, and then having emergency surgery.
We scheduled surgery for June 12th. She came in, took a last look, and made markings. She was so amazing and so thorough. She wanted to cover her bases before going into surgery. She decided on a new stoma placement should we have the worst-case scenario.
Surgery
Colon Resection, Ostomy Reversal & Hernia Repair
Thank the Lord, everything came out great.
The first night was horrible. I had so much pain because it was a pretty big opening. She took out the main tumor and a big chunk of my colon, and she repaired my hernia.
I went back for my follow-up appointment to remove the drainage. She told me that the doctor had taken out everything. She focused on the colon. She gave me the great news that from stage 4, it had gone to stage 1. If the cancer hadn’t spread, that would have been the end of my cancer journey. We still had the liver and the peritoneal area.
The amazing news was that we were heading in the right direction. This is from surgery being off the table to removing this tumor. It was such a blessing. She also took out my appendix because it was connected somehow. She said that they went through it and they studied it and had no cancer, which is amazing news. The cancer stopped spreading.
I still needed to have PET and CT scans to confirm. But he said that everything looked great and that the immunotherapy and surgery were successful.

Seeing a New Oncologist
Another blessing of my husband working in the medical field was that he knew people and started asking for an oncologist referral. I got a new oncologist where we moved and he is amazing.
At my first appointment, he was very proactive. He said, “Let’s see what we can do with your liver,” because that was the next step. Immediately, he referred me to a surgeon at USC.
He explained that I was responding perfectly to immunotherapy. Everything was shrinking. The cancer could shrink a lot with immunotherapy, but there are still cancer cells there and the risk of it coming back is greater. He said that the best thing to do was to have surgery and remove that part of the liver so that’s what we did.
Partial Hepatectomy (Liver Resection)
We scheduled surgery again for September 20th. I mentioned to him about the lining of the stomach and he said he would look into it. He would check that out, too. The surgery date came, I had surgery, and it was successful. Thank God.
He said that everything looked great based on what he saw, but I still needed to have PET and CT scans to confirm. But he said that everything looked great and that the immunotherapy and surgery were successful.
Follow-up Appointment
I saw my oncologist recently, who scheduled me for a PET scan to see where we’re at, but he said that I look good and that everything looks great.

We decided to move, which was scary because I had to look for new doctors and everything.

Getting Support from Family
Moving Closer to Family
Around that time, we made a life-changing decision. We lived in Northern California and decided to move to Southern California to be closer to my husband’s side of the family.
My family had been great, but we needed a little more support with appointments. My in-laws are retired and they’ve been amazing. We decided to move, which was scary because I had to look for new doctors and everything.
Husband as Biggest Advocate
I knew nothing about cancer, just little things that my husband would tell me when he would come home. He would get close to patients that he cared for and when they would pass away, he’d come home sad and we’d talk about it.
Things would be different if my husband didn’t have the knowledge that he did. He’s been my biggest advocate. He understands so he can have conversations with the doctors and surgeons. I don’t know what my situation would have been like otherwise.
I saw a palliative care doctor and she would ask me how he was doing. She said that knowing works like a double-edged sword because he knows too much. He knew stage 4 was serious. He knows that this can go south fast so I can’t imagine what he feels being my husband and knowing all this information.
In a way, sometimes I feel like ignorance is bliss. I didn’t know much, which helped me because I didn’t realize the extent of my illness until I had that conversation with my doctor that one day. But having somebody who knows is big.

Things would be different if my husband didn’t have the knowledge that he did. He’s been my biggest advocate.

Words of Advice
Don’t take your health for granted. If you feel that something is wrong, have it checked out. I never thought in a million years I would be on this journey.
Be proactive and push. The day I went into the ER, the doctor didn’t want to do the CT scan because I looked fine, but I said, “It’s okay if I’m exposed to radiation. Let’s do this. I want to know what’s going on.”
Colon cancer is happening to a lot of younger people. This is not an old person’s disease anymore. I’ve read about people as young as in their 20s being diagnosed with colon cancer.
For some reason, it is so hard to schedule a colonoscopy. Whatever the reason is, that needs to change. It should be more accessible.
So many people are dying because they’re being diagnosed at such a late stage. It’s so silent at the beginning and you don’t know that there’s something wrong until it starts creating havoc in your body and that needs to change.
We need to have a colonoscopy or whatever testing is available at a younger age. My siblings were able to schedule a colonoscopy immediately because I have cancer. They became high risk. My sister had such a hard time scheduling an appointment because of insurance. That should change.
You have to advocate. Speak up and be firm. If something is wrong, don’t stop because the more you wait, the more this monster can mess with your health.

Don’t take your health for granted. If you feel that something is wrong, have it checked out.

Inspired by Dania's story?
Share your story, too!
More Colon Cancer Stories
Shannon M., Colon Cancer, Stage 1
Cancer Details: Found the cancer as a result of her Lynch Syndrome
1st Symptoms: Routine colonoscopy found polyp
Treatment: Partial colectomy
Hugo T., Colon Cancer, Stage 1
Cancer Details: Diagnosed 2 weeks after 5 years remission from testicular cancer
1st Symptoms: Inflamed bowel
Treatment: Subtotal colectomy, immunotherapy
Rachel B., Sigmoid Colon Cancer, Stage 1
Cancer Details: The sigmoid colon (or pelvic colon) is the part of the large intestine that is closest to the rectum
1st Symptoms: Stomach discomfort, nausea, bloating, blood in stool
Treatment: Colectomy
Chris T., Colon Cancer, Stage 2
Cancer Details: Discovered Lynch Syndrome after genetic testing
1st Symptoms: Found the cancer as a result of family history, early colonoscopy
Treatment: Partial colectomy
Shannon C., Colon Cancer, Stage 2A
Cancer Details: Diagnosed at 29, tested positive for Lynch Syndrome
1st Symptoms: Severe pains after eating
Treatment: Partial colectomy
Barbara M., Colon Cancer, Stage 3
Cancer Details: Family history wasn’t flagged, should have had colonoscopy earlier
1st Symptoms: Stomach discomfort, difficult to process food
Treatment: Colectomy, Chemo (FOLFOX, CAPOX)
Shelley B., Colon Cancer, Stage 3B
Cancer Details: Had no usual first symptoms, found as a result of routine colonoscopy and endoscopy
1st Symptoms: None
Treatment:Partial colectomy, chemotherapy (FOLFOX)
Lindsay D., Colon Cancer, Stage 4
Cancer Details: Diagnosed at 32, cancer spread to ovary and lung
1st Symptoms: Lump in pelvic area, funny-smelling food, weight loss
Treatment: Chemotherapy, colectomy (surgery)
Lee J., Colon Cancer, Stage 4, Recurrence
Cancer Details: Recurrence then remission
1st Symptoms: Discovered stage 4 cancer from unrelated CT scan
Treatment: Neoadjuvant chemo (FOLFOX), hemicolectomy (partial colon surgery), adjuvant chemo (FOLFOX), chemo post-recurrence (FOLFIRI), liver surgery
JJ S., Colorectal Cancer, Stage 4
Age at Diagnosis: 27l
1st Symptoms: Abdominal pain, blood in stool
Treatment: Surgery to remove tumor, chemotherapy, clinical trial of Keytruda (pembrolizumab)
Haley P., Colon Cancer, Stage 3C
Symptoms: Constipation, fatigue, shortness of breath
Treatment: Surgery, chemotherapy
Amanda G., Colon Cancer, Stage 2A
Symptoms: Gurgly stomach, blood in stool, chronic constipation
Treatment: Surgery (hemicolectomy), chemotherapy (CAPOX), Zarxio
Symptoms: Fatigue, anemia, irregular bowel movements, loss of appetite, heavy periods Treatment: Laparoscopy, chemotherapy, partial hysterectomy
Dania M., Colon Cancer, Stage 4, with Liver and Peritoneal Carcinomatosis
Symptoms: Constipation, diarrhea, terrible bloating, swollen belly, as if pregnant
Treatment: Surgery, immunotherapy (KEYTRUDA)
Stephanie K., Colon Cancer, Stage 3
Symptoms: Very bad cramps, bloating, indigestion, burping
Treatment: Surgery, chemotherapy (CAPOX)
Jason A., Colon Cancer, Stage 3B
Symptoms: Abdominal pressure, fatigue, small amounts of blood in stool
Treatment: Surgery (colon resection), chemotherapy (FOLFOX: folinic acid, fluorouracil, and oxaliplatin)