David’s Stage 4 Follicular Lymphoma Story
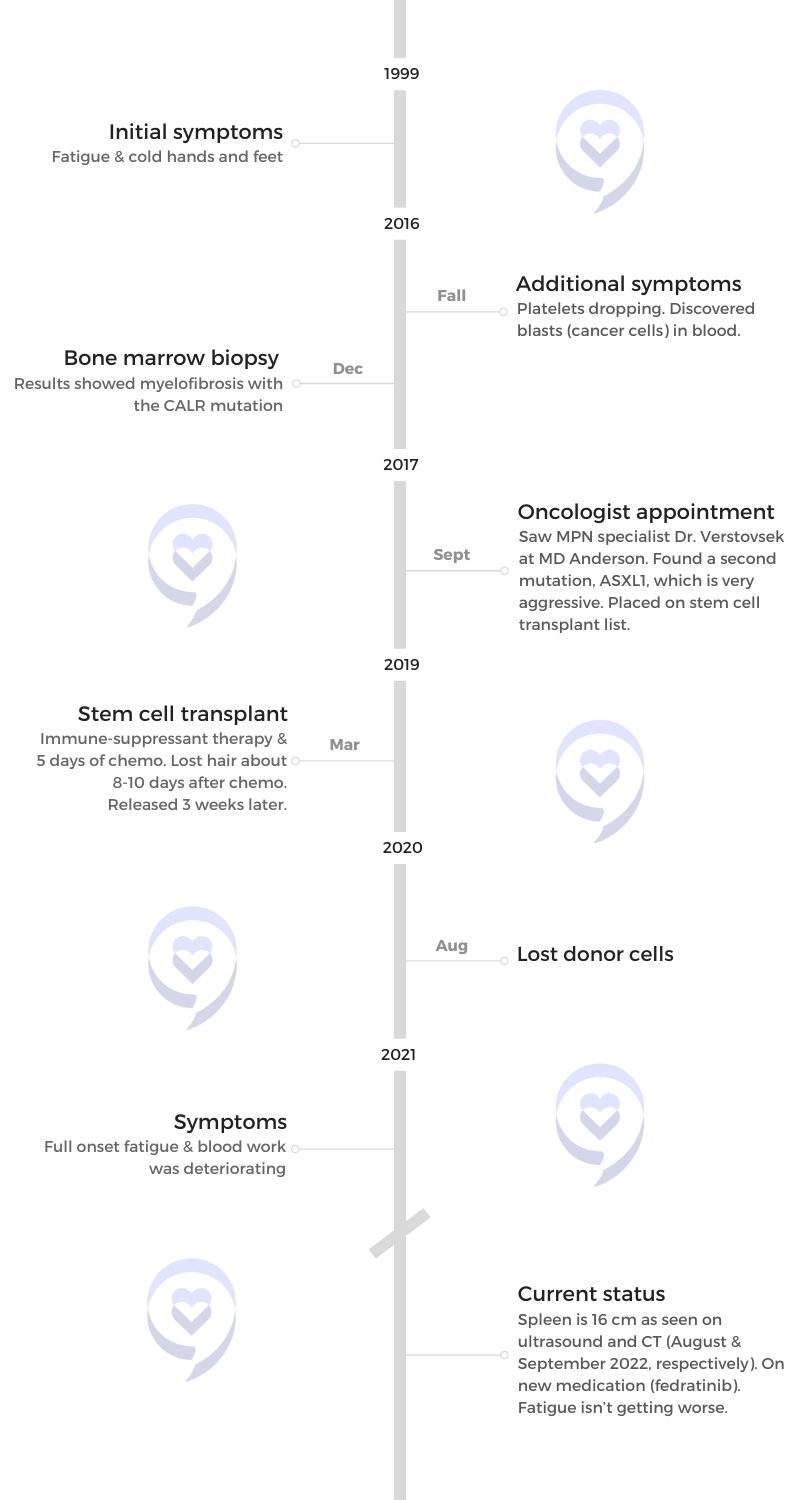
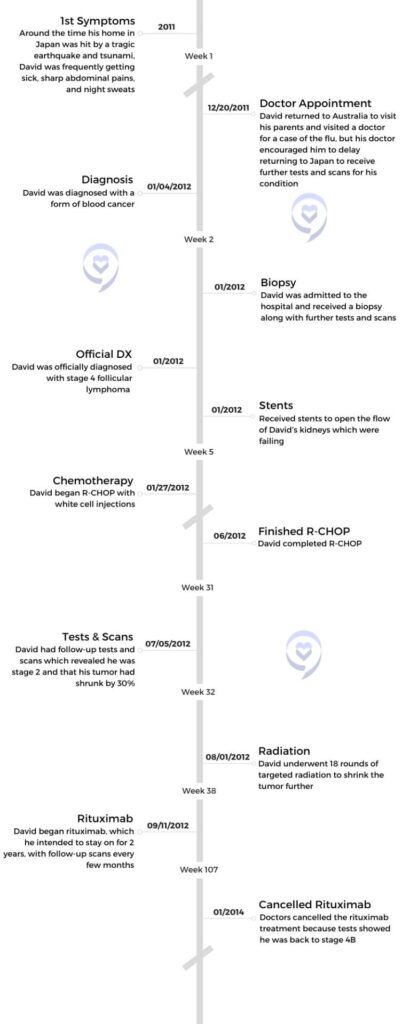
David, a stage 4 follicular lymphoma survivor, began his journey with cancer in 2011 when he experienced sharp abdomen pains and persistent sickness while living in Japan. Initially dismissed as the flu, he faced a delayed diagnosis due to the aftermath of a devastating earthquake and tsunami. The loss of his home and business added complexity to his struggle as he sought treatment for his blood cancer.
After enduring grueling chemotherapy and a clinical trial, David faced severe side effects and a slow tumor response. Despite temporary relief, the cancer returned, leading to a stem cell transplant that came with complications. Battling infections, respiratory issues, and a grim prognosis, David emerged from the transplant determined to focus on diet, exercise, and a positive mindset. Now, 9.5 years into remission, he attributes his recovery to disciplined lifestyle choices, offering a beacon of hope to others facing the challenges of stage 4 follicular lymphoma.

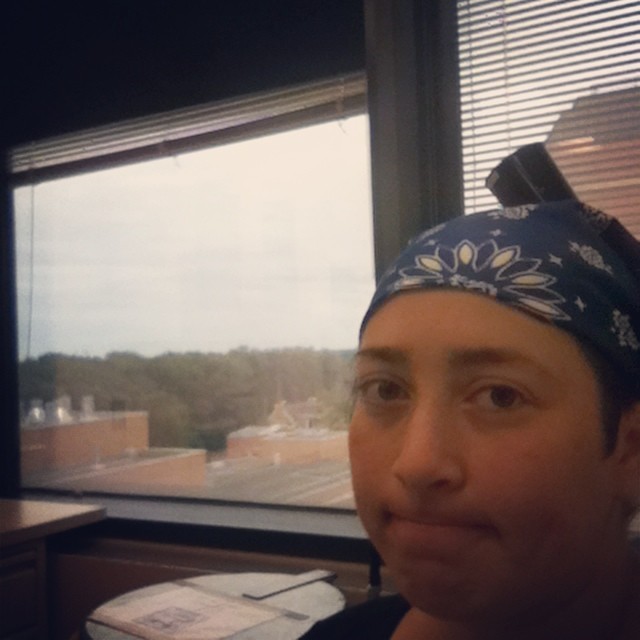
- Name: David K.
- Diagnosis (DX):
- Follicular lymphoma
- Staging:
- 4
- Symptoms:
- Sharp abdomen pains
- Frequently sick
- Night sweats
- Less stamina
- Age at DX: 38
- Treatments:
- Chemotherapy
- Immunotherapy
- Radiation
- 18 rounds
- Clinical trial
- Stem cell transplant
- Autologous
If you feel like you’ve got a mountain to climb in front of you, don’t look at the mountain. Just focus on the next step.
David K.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms
Tell us about yourself

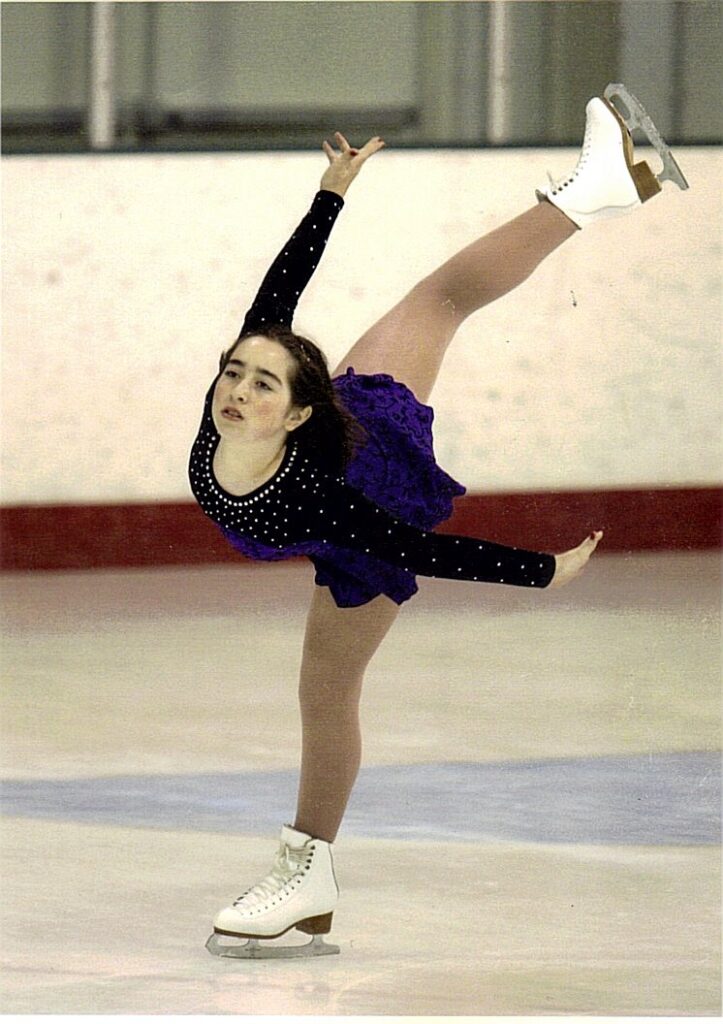
I am David. I have a YouTube channel trying to help people and some Facebook groups. At the moment, my hobbies are mostly to do with sport, healthy eating, healthy lifestyle and that sort of thing. Grounding and getting outdoors as much as possible.
What were your initial symptoms?
My story with cancer started back in 2011. I didn’t take a lot of notice at the time. Of course, many of us don’t. We sort of pass different health issues off as just part of life.
I was having very sharp abdomen pains off and on throughout the day, but it wouldn’t last. It would only be for a few seconds at a time. They gradually got worse and worse. I was sick all the time. I had a cold all the time. Like all year I was fighting colds and flu.
What was happening in your life around this time?
At the time, we were living in Japan and in March of 2011, we were hit by a 9 magnitude earthquake that lasted over 6 minutes. That resulted in the large tsunami that hit us afterward. We spent a few months without power, water, gas, or anything like that for a while. We’re riding around on bicycles, trying to find places that have some food and water for us to buy. Things did settle down and supplies started coming in so we could get fuel and things like that again. We were trying to rebuild.
I’m a strength and conditioning coach and I was coaching athletes at the time. I was trying to build that business back up and my wife had to go back to work. In between that, we were helping other people trying to clean up after the tsunami. We cleaned out houses that did survive, visited shelters, and tried to bring food, clothing, and things like that to people who didn’t have any. It’s kind of difficult. You’re trying to rebuild yourself as well.

Did you see a doctor to address your symptoms?
I was getting sick all the time, as I said. I did see a doctor once and he just said it was a flu. He did an x-ray and didn’t say much about it. He was confused by my blood results, and he said he would check me again early next year.
But in December, I decided to visit my family here in Australia. As soon as I got off the plane again, I was sick with the flu. I decided to go see their local doctor to get something for the flu and just have a general checkup. He decided to do a blood test. That next day he called me back in to have a look at the results. I wasn’t expecting it to be that soon. He was confused by the blood results as well because I was quite fit. I thought I was healthy, I was doing everything right.
He felt around my abdomen and he didn’t tell me what it was, because he didn’t know. But he said, “Look, I think you should stay here and get this checked out.” I was by myself. My wife was still in Japan working. I had to go home, tell my parents, call my wife, and tell her, “Look, I don’t think I’ll be able to come home in January,” when I was due to go home. “Because I might be a little bit worse off than I thought.”
Diagnosis
Travel plans were delayed due to the doctor’s recommendation
I just thought it was a bit of the flu, and while I was doing that, my doctor organized an ultrasound and x-rays to be done in the town near my parent’s place because they lived in the countryside about a 4-hour drive from the main city, Brisbane. Over the Christmas holidays, not a lot happens, so it took a few days for this to happen. On the 3rd of January, my wife decided to join me. She arrived here in Australia, and that same day, the hospital in the city called me just a couple of hours after she arrived. They called me and asked me to go into that hospital that night. Of course, we didn’t do it that night. We went the next day and they didn’t speculate on any reason why. They just told me that it was rather urgent.
My parents and my wife all made the trip and we went into the emergency room and we’re thinking, okay, we might be here for a few hours just waiting. But surprisingly, they had me in a bed within about 10 or, 15 minutes and I was surrounded by all these doctors, nurses, council workers, and counselors. People that are getting ready to tell me something is really bad.
Receiving a cancer diagnosis
Eventually, the test came back and they diagnosed me as stage 4 follicular lymphoma. With follicular lymphoma, there’s no chance of a cure. There’s only hope for a remission period.
They said that they didn’t know what type of cancer it was, but they knew that I had a large tumor and that I had a form of blood cancer that they needed to do tests for. It was a bit of a head spin. I wasn’t prepared for anything like that. I knew I wasn’t well because I kept getting the flu and things like that, but I wasn’t expecting that. I wasn’t expecting them to say, “Look, you’ve got cancer.”
I was only 38, 2 months away from my 39th birthday. The year before was a pretty tough year. Going through running, my usual training, and things like that, I started slowing down a lot. I was thinking I was just getting old, that’s what I put it down to. Then the tests started, and that took a little over a week because there’s quite a numerous amount of tests. We did all sorts of scans, a biopsy of the main tumor, and my kidney function. The kidney function was important because the size of the tumor was that big that it had sort of crushed all the other organs around it. It was wrapped around my aorta is where it originated from.
It killed my left kidney and my right kidney was just down to 12% capacity. The cancer was already pretty much going to kill me. I probably wouldn’t have lasted long enough for the cancer to come there because the kidney was going to fail before then. That was the priority before they could start treatment. I had to have stents put in. They put them in both kidneys to try and get the left one going, but it had shrunk too much to recover. The stent operations were done every 3 months for a couple of years after that.
»MORE: Reacting to a Cancer Diagnosis
What stage were you?
Eventually, the test came back and they diagnosed me as stage 4 follicular lymphoma. With follicular lymphoma, there’s no chance of a cure. There’s only hope for a remission period. The more you treat it or the heavier you treat it, usually the shorter the remission period and the more aggressive it comes back.
Adjusting to life with cancer
I wasn’t too worried about that at the time. I was more concerned about our life in Japan. I’d been there for 10 years. Everything that we had was in Japan, and our whole life was there. Our home, business, car – just everything that you build up over the years career-wise. We lost all that because of the cancer.
All I wanted them to do was just cut out the tumor, dose me up with some drugs, and then just let me go. That was pretty much how I was thinking about it right up to treatment. I didn’t take on board that I was going to be there all the time, for the rest of my life, or that it might come back. That took some time to get around. I didn’t delve too much into it at the time. I just wanted to take it step by step.
Before my first treatment, my wife had to go back to Japan. This was a difficult stage for us because this might have been the last time we ever saw each other. They told me my kidney function, because of the way it was, I might have less than 3 months to live. She had to go back to Japan to sort out our lives and get rid of everything that we couldn’t keep, and that would take some time. We didn’t expect to be able to see each other again. That was difficult.
While she was gone. I then had to try and organize a visa for her to come to Australia because she’s Japanese. I had to try and set up a home, find a place to live, and start again while I was going through treatment. So when I started treatment and went through treatment, I was pretty much homeless. I was living on couches and spare rooms of friends and family that were close enough to the hospital or within an hour’s drive. There was just a lot going on, having to move internationally and then going through treatment and getting the diagnosis. It was a real head spin, just so much going on at once.

This was a difficult stage for us because this might have been the last time we ever saw each other. They told me my kidney function, because of the way it was, I might have less than 3 months to live.
Chemotherapy
What cancer treatment were you on?
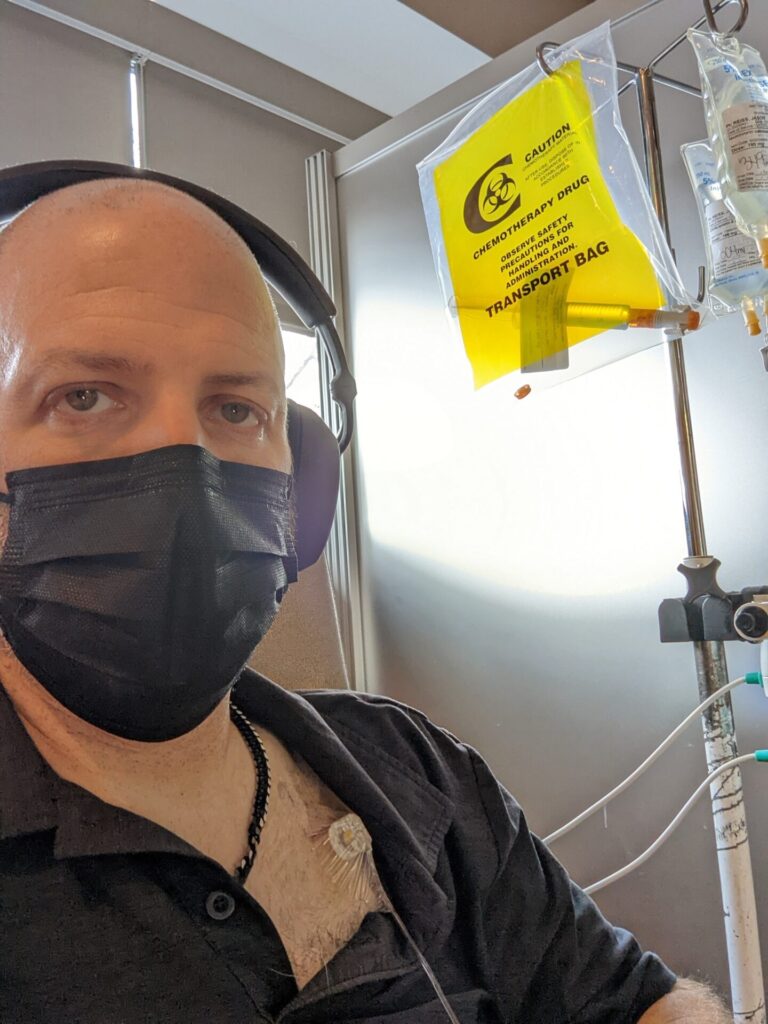
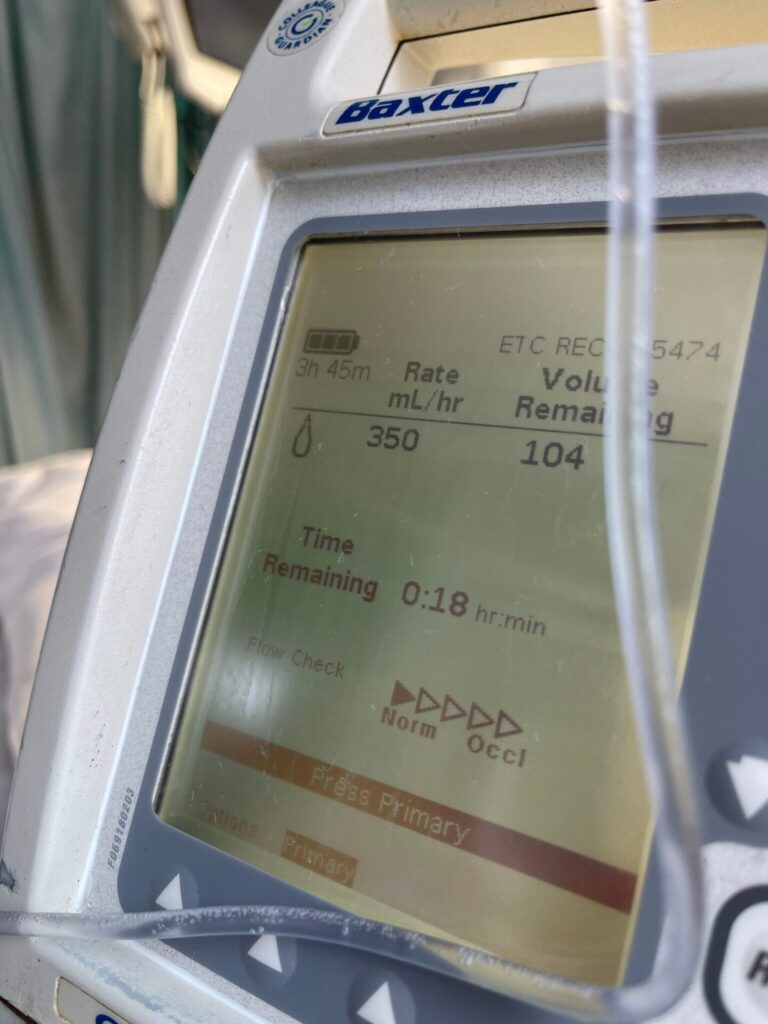
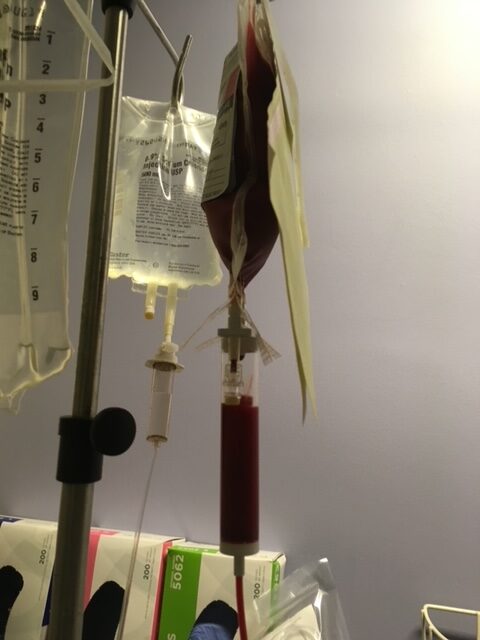
The treatment was absolutely brutal. They started me on R-CHOP. The plan was for 6 to 8 treatments, depending on how the cancer reacted and the tumor. The cancer itself did react pretty well, but the tumor? Not so much. From January 27th, we started R-CHOP, which is an extremely heavy dose and it’s a 21-day cycle. Every 21 days we have the treatment.
It’s about 5 bags of treatment in one day. They ran it through over a 4-hour period. The first few treatments, ran it through over an 8-hour treatment because it takes time for you to get used to the treatment. The next day, after treatment, you have to give yourself a white cell injection to try and stimulate white cell production. That was the most painful part. After that, I think that’s when all the bone pain sort of comes in and all the violent vomiting and that sort of stuff.
We did scans every 2 months. We got to treatment number 6, and they said, “Well, we’re going to have to go all the way out to 8 because the tumor just hadn’t reacted.” It was very slow to react to the treatment. We got to treatment number 8, which emotionally, was very up and down. I had white coat syndrome, and the thought of going back to the hospital after each treatment was just brutal. It was sickening. Certain smells would set you off. Even just body smells from other people, soaps, anything like that would just make me very sick.
I didn’t want to see [my doctors] at all because I knew how I felt afterward. It made me so sick and violently ill. Just the thought of going back and seeing them, or even speaking to them, just made me sick.

»MORE: Chemotherapy FAQs & Patient Stories
How was your medical care team?
They were very good. The people were wonderful. My oncologist, I still see him every 6 months. They’re just great people and the nursing staff are lovely. They go through a lot. I think it’s a very thankless sort of job but they are wonderful people. I think it takes a special kind of person to do that job.
What advice do you have for someone on cancer treatment?
Tell [your doctors] everything that you’re feeling. They may not be able to help with the way you’re feeling, but any kind of side effect that you’re feeling they may be able to either change the treatment or they might give you some painkillers or something that might help with those side effects.

There are numerous amount of side effects of chemotherapy. I had bad IBS and reflux. The bone pain. If you’re going through our trial especially, things like the bone pain are quite intense. Even without movement, just lying on the bed, it felt like the weight of my own body was crushing my bones. Plus, if you do have abnormal sort of reactions, they need to know about it so that they can adjust the treatment. So you should tell them everything.
What did you do to combat mouth sores?
Depending on the treatment that you go through, some people react differently. I tended not to delve too much into other people’s stories because you do react differently and I just wanted to react to how I was feeling. For example, in the first 2 weeks of the after-treatment, I couldn’t eat. My mouth was full of ulcers and sores. All I could taste was the chemotherapy itself, which was a horrible, horrible taste. It kind of felt like I was sucking on metal. It was a really strong flavor as well. It’s very painful. The mouth is all swollen because of the sores and vomiting a lot. You can’t keep anything down either.

You have to find ways to numb the mouth. Things that worked for me were baking soda and salt, mouthwash helped to clean the sores and to numb the pain. It also helped just to clean the mouth as well, to get rid of the sores. Oddly enough, chewing gum. I don’t recommend eating a lot of sugar or those sorts of things, but it did numb the mouth enough that I could try and eat something.
Fasting – I didn’t set out to fast at the time, but for the first 2 weeks after, I really couldn’t eat because of the way I was feeling. Again, when you’re vomiting that violently on an empty stomach, it’s infinitely more painful. If you can get something in, even if it’s like liquid food, something to help or to have to bring it up, it helps. It also reduces the acid burn you get from the reflux in your esophagus. It was really good for all the esophageal mucus and that sort of stuff. That was really helpful for me, I think.
»MORE: Managing Nausea and Vomiting from Chemotherapy
Radiation & Immunotherapy
How often were you getting scans during cancer treatment?
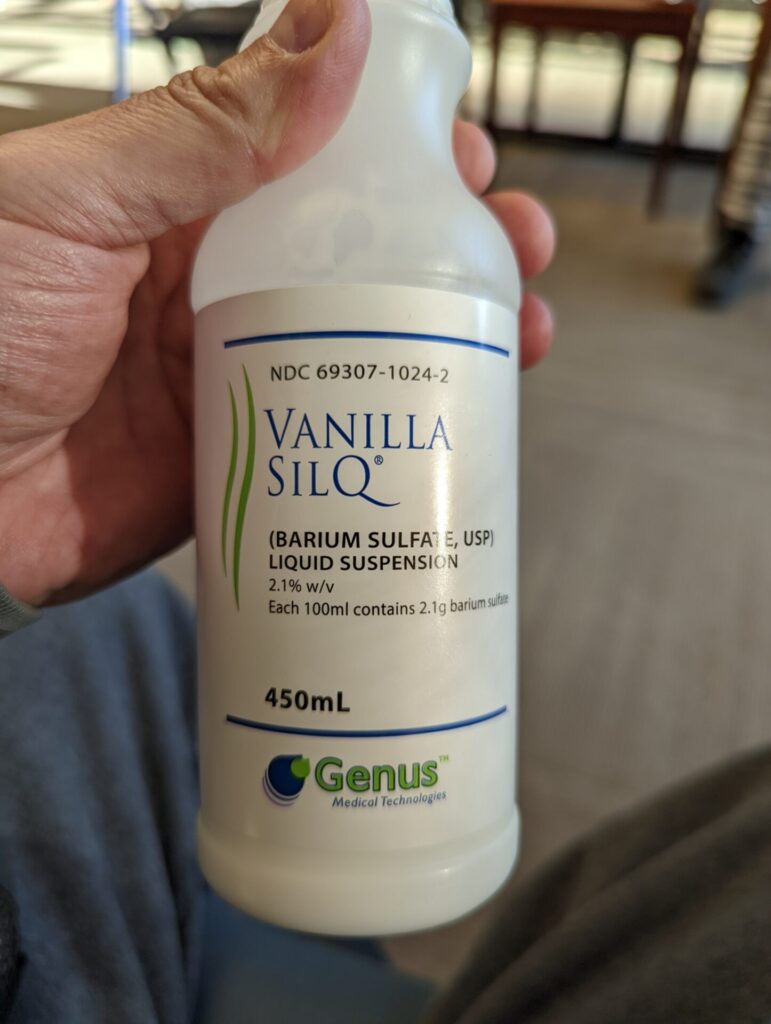
I was getting scans every 2 months. They were doing CT scans, PET scans, tests, and all sorts of things. After the eighth round, we did CT scans and the result was the main tumor had only shrunk by just under about 28%. It hadn’t responded as well as they wanted it to, but my blood was clear at the time, so that was good, and my spleen was clear. Most of everything else was okay, but the tumor itself was still only a 28% reduction and still growing.
Beginning radiation to shrink the tumor
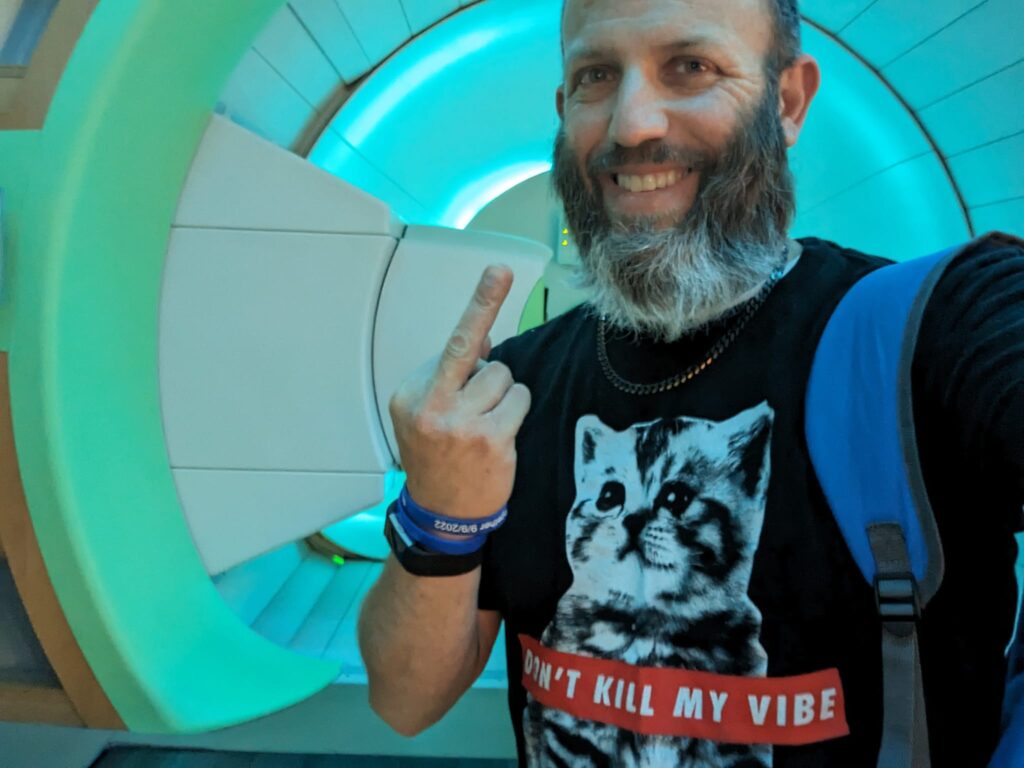
The next day, we did 18 rounds of targeted radiation on the tumor itself and on the main tumor. I say ‘main tumor’ because it lives with lymphoma. The lymph nodes are all malignant as well, and they were all clear by the eighth round. That was good.
The radiation, I thought, was a cakewalk. That was easy, but I did still take my anti-nausea medication because the one day that I didn’t, I did vomit. You still do get nausea from the radiation. I didn’t have any other side effects really, so there was no pain involved or anything. It’s just a 2 minute done and dusted hit on the tumor.
After that, we did more CT scans, blood tests, and update tests just to work out where the tumor was up to. The radiation did help a little bit. It reduced it by another 10%, so they were pretty happy with my progress and labeled me as stage 2 and stable. That was pretty good. I was thinking, hopefully, if we can keep it in that stable in that remission, everything would be good and maybe we can go back to Japan and start living again.
Switching to another cancer treatment

Then they decided to put me on a rituximab 2-year program. Rituximab is the first part of the R-CHOP treatment. That’s what the “R” is for in R-CHOP. Every 2 months I have a rituximab treatment, and this would be for 2 years. Then this would hopefully give me an extended remission period. I was hoping for maybe 5 or 10 years of remission. And of course, we did scans and tests every, every treatment as well. That was every 2 months. We did that for 14 months. That took me to January of 2014, exactly 2 years to the month.
Were you able to stay in remission with rituximab?
They rediagnosed me again as very high stage 4, so it had come back even while I was going through the rituximab treatment. The 2 months before we had done scans and tests and I was stable. I was fine. In that 2-month period, it was back to stage 4 and again just everywhere. I was back to square one. That was really disheartening because the 2-years before I said, okay, this will keep me in remission, because I knew it would come back. I just didn’t think it would come back until after these 2-years.
I thought I was going back to Japan and my wife and I were going to start living again. Even if it was just stage 2 remission and I still had the tumor there, it wouldn’t worry me. But now it’s stage 4 again. So that whole 2-years are just back to square one. It was very difficult emotionally and mentally.
Clinical Trial
Joining a clinical trial for bendamustine
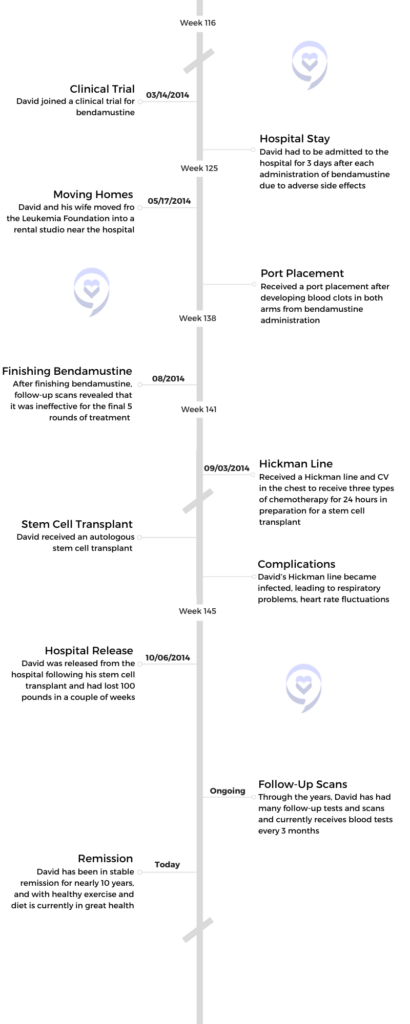
They got me into a clinical trial here in Brisbane for bendamustine. It’s not a new drug, but it just hadn’t been used in Australia for some time. They decided to use it in a clinical trial. It was supposed to be as effective as the R-CHOP, but not have so many violent side effects.
For some people, maybe it worked. For me, because it was a clinical trial, I had a clinical nurse who was with me every day, every step of the way. They were checking on me and wanted every detail. I kept a diary for each day on how it was making me feel, so it was very tight. It’s very good that way, but it kind of made me feel like a lab rat too, because they’re sort of experimenting on everything.
How did you feel about joining a clinical trial?
I was nervous about it because I didn’t want to go through R-CHOP again. I was mainly concerned about how that made me feel. I was concerned about whether or not I wanted to go through more treatment. They assured me that the side effects were not as bad and it wasn’t as violent.
The fact that it was a clinical trial did make me a little bit nervous as well. I was thinking, has it been used or is it an untested drug? I did find some information on bendamustine itself, and it had been used in other places for some time, which sort of put my mind at ease. It was kind of like that lab rat feeling going into it.
But again, the staff was so nice. They were nice people. The clinical nurse that I had kept tabs on me all the time, and she’d call and talk to me every day and see how it was going. It wasn’t so much about writing down everything that you’re feeling, all the side effects, and that sort of stuff. She just wanted to make sure that I was feeling okay emotionally about the trial, and that helped.
I think there are a lot of benefits to doing a clinical trial. For example, when you have a clinical nurse there keeping an eye on the treatment, they make sure that everything is done correctly. Everything is done right. This helped because one of the things about treatment number 4, one of the bags that the pharmacy sent to us was out of date by nearly 2 years. She picked up on those sorts of things, so it was it was very handy. It did make the whole thing a lot easier, I think.
Did you have side effects from bendamustine?
As for the treatment itself, the first one I thought was really easy. I had to drive myself to the hospital. I didn’t have anyone to drive me. My wife can’t drive, so I drove. It was done over 2 days, each treatment. I came home at night between them. During the first treatment, I drove home and immediately I started having non-neutropenic fevers. It skyrocketed, my fevers. I was feeling like I just couldn’t do anything and I was hot, I was red, and I wanted to lie down on the bed and sleep it off. But my wife called an ambulance and took me back to the hospital, which is a good thing because I wouldn’t have made it through the night otherwise. The fevers were too high.

They kept me in for 3 days. The following day, they gave me the rest of the treatment. Apart from the fever and the treatment itself, I didn’t have as much bone pain, muscle pain, or anything like that. There was a little bit of nausea and vomiting, but nothing like the R-CHOP. It was very easy and mild compared to that. The second treatment was the same, and again, they kept me in hospital for 3 days.
After that, we did updated scans. The first 2 treatments worked quite well on the cancer. They were pretty positive about it, so I felt it was all good. I can handle the fevers and stay 3 days in hospital if it’s working.
My wife called an ambulance and took me back to the hospital, which is a good thing because I wouldn’t have made it through the night otherwise. The fevers were too high.
We got to treatment number 3 again and the fevers were out of control. They kept me in for 3 days. They were still treating me the second day, but this time my treatment arm was starting to fill up with blood clots and they were quite long and very pronounced. There were superficial blood clots in my arm, but they went from my shoulder down to my wrist so they couldn’t keep feeding it through my arm. So they went to my left arm and the next treatment did the same thing to my left arm. By treatment number 4, both my arms were filled with blood clots.
»MORE: Cancer Treatment Side Effects
Receiving a port
Then they had to put in a port on the right side of my chest. That was the scary part because it had filled up both my arms with blood clots, and now they wanted to feed it directly into my heart. I was a little bit worried because they told me it’s because the heart just gets it out quickly and disperses it, so you should be okay. But I still had these massive, long, very painful blood clots in my arms, so it was very concerning. We did update scans on the fourth treatment. The first 3 treatments had been quite effective, but by treatment number 4, it had stopped working. We went to treatment number 6, we had more update scans and again, it had stopped working. They went out to the full 8 rounds.
By treatment number 6, they worked out how to keep the fevers down before treatment, but the scans after treatment number 8 showed that the first 3 had worked quite well, but from there, they did nothing. Then they prepared me for the autologous stem cell transplant. Because I couldn’t work through all this, I didn’t have much income. So we were living in a foundation here called the Leukaemia Foundation.
Between treatments in the clinical trial, we had to move, so we had to find a place close to the hospital. We found this tiny little studio and we had to move between treatments. There were a good 5 or 6 days after each treatment that was on a 21-day cycle, the same as the chart, but there were about 5 or 6 days where I felt pretty good. Before the next treatment, I almost felt normal again, so that was pretty good. That gave me time where we could organize and move into our little studio.
Stem Cell Transplant
Opting for a stem cell transplant

They told me before going into it that I had to make out a will because they really didn’t expect me to come out of it.
After the eighth round, we did more scans. The clinical trial was still going for a couple of months afterward to track my progress. Because it hadn’t done much from the third treatment, they decided to go into the stem cell transplant. I had to get a Hickman line or CV line implanted in my chest on the left side. That had 2 rubber tubes sticking out of my chest there, plugged straight into my heart, and 2 little connectors that just hung out so they could run the different treatments through. There were quite a few different treatments that were going to basically destroy my body and then reintroduce new stem cells.
They used these different types of chemotherapy over 7 days for 24 hours at a time. That was an absolute nightmare. That was a much worse feeling than the clinical trial. I didn’t want to do it. I even asked my oncologist if it was going to be worth it and how much time would it give me. Do you think I would live if I didn’t do it? But again, the time was down to months. I was only thinking about my wife, so it was a tough decision to make.
They told me before going into it that I had to make out a will because they didn’t expect me to come out of it. That was really tough. It was consent. Being concerned about what could happen during the transplant, they strongly suggested that I make a will before going into it. The months afterward, my oncologist admitted that he didn’t think I was going to get through it. It was tough, but obviously, we decided that it was at least worth trying. I didn’t think it would be as bad as the R-CHOP, so I figured, well, I got through that. I can get through this.
The difference is that this was numerous amounts of chemotherapy going through. It’s 7 days, 24 hours at a time, but there’s no rest period at all. Then on the eighth day, they would reintroduce my stem cells to try and help me recover. That was the good news, that the year before, after my blood was clear, they collected my stem cells at the end of my R-CHOP treatment before I started radiation. My stem cells were quite high. They were 99.4% viable, so that was one good thing I had going for me. During treatment, I was fasting and I was still – on the days that I could – getting some movement around. I was quite fit before going into it, so I was lucky in that respect.
Complications during transplant
During the transplant, my Hickman line, the CV, and the plastic tubes for my treatment became infected. They had to decide whether or not to keep going with the transplant or not, or just remove the tubes and keep going. They decided to keep going, but they had to put the treatment through my arms and the port in my chest. So they had to pull out the Hickman line, and that was concerning as well because I still had clots in my arms as well, and they were still feeding it through my arms.
From there, because of the infection, I don’t know if it was just due to the infection or not, but I stopped breathing numerous times and it got so bad that the nurse would have to come and check on me every 10 minutes or so to check if I was breathing or not. I had bad heart fluctuations, the arrhythmia in my heart, so I would pass out. I’d stop breathing, I’d wake up, I’d have this oxygen mask on, and I’d have ECG electrodes stuck on my chest, trying to measure my heart rate and things like that. They kept those monitors on all night. I was trying to sleep and it was really difficult. Especially because the nurse kept coming in to check if I was breathing or not, so I didn’t get much sleep. That was really difficult.
They had to quarantine my room, and of course, the only person that came to see me was my wife. She was sitting there watching that all day, and that was difficult for her. Years afterward, she would – if I was sleeping, because I was stuck in bed for years after that – she would wake me up just to make sure I was breathing. It was a bit of a traumatic stress for her as well, I think.
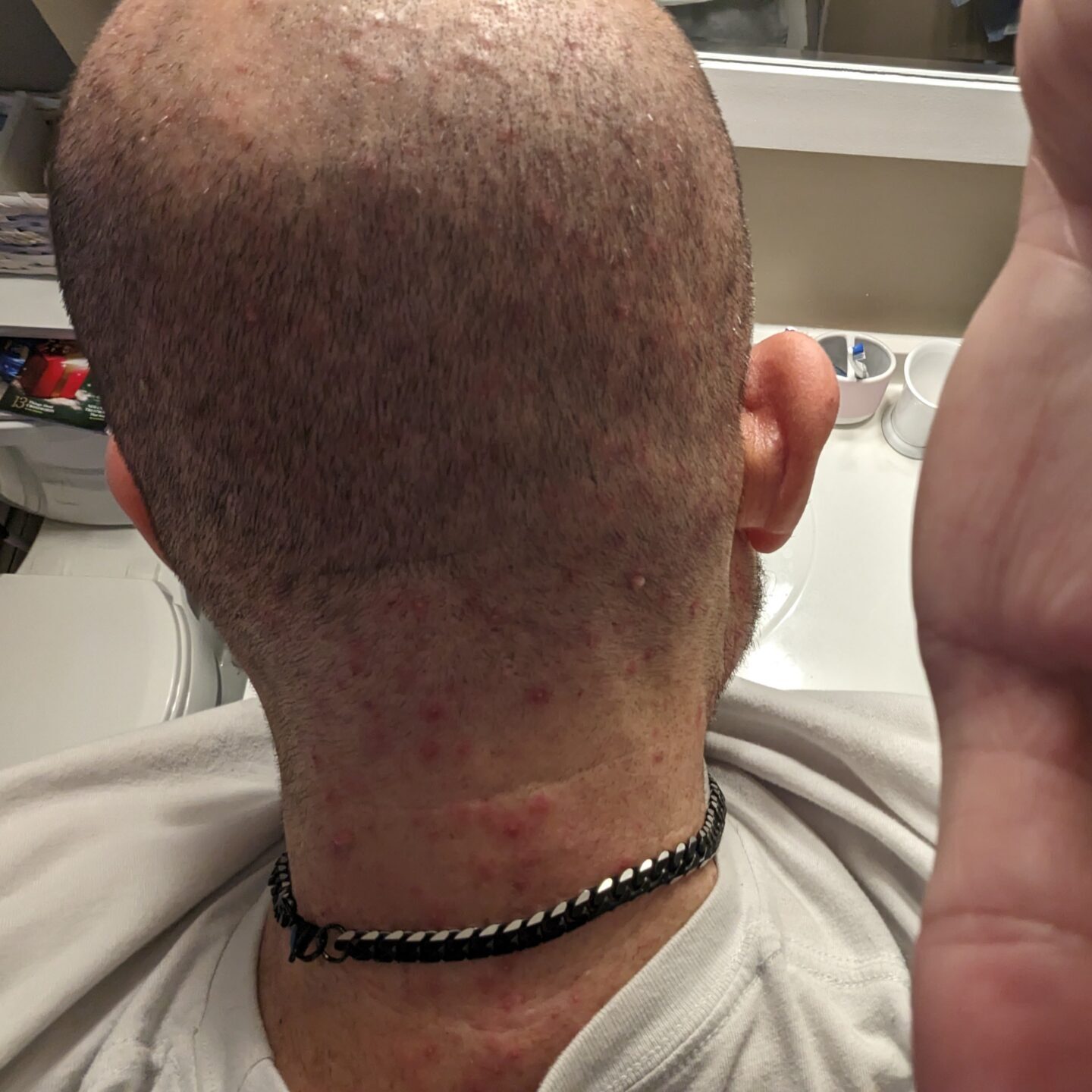
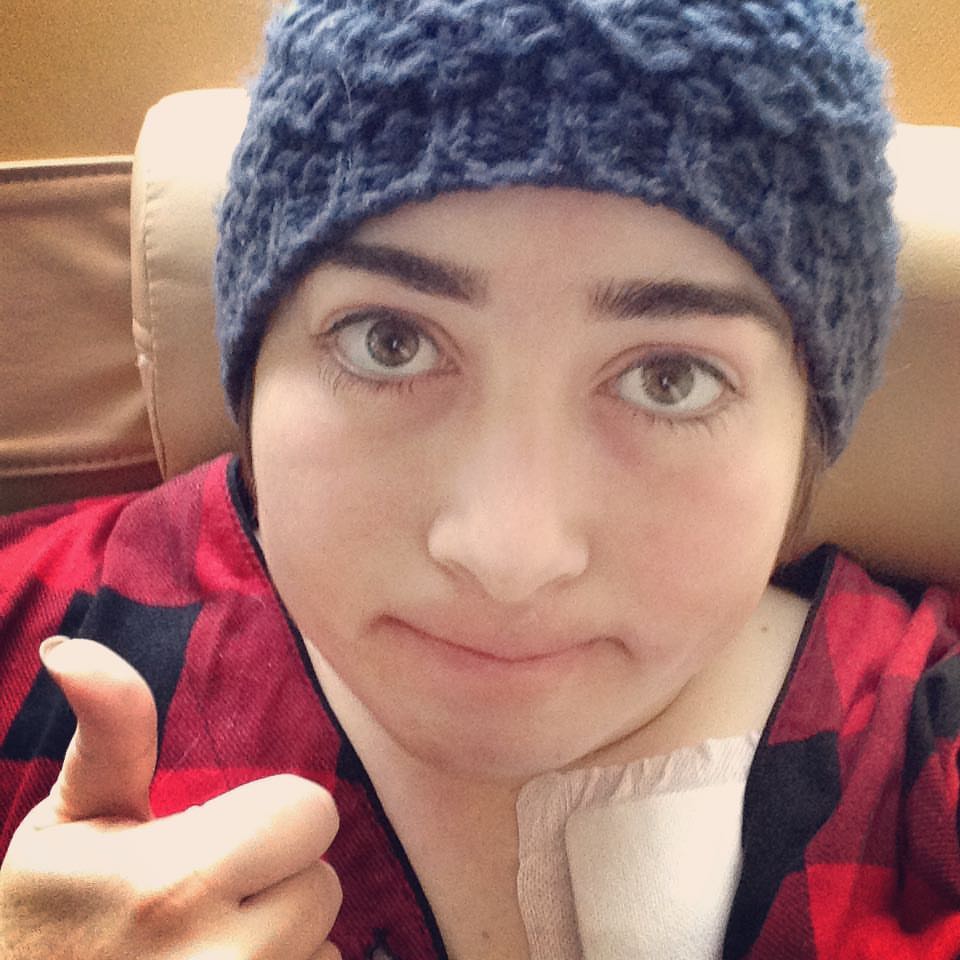
I went in on the 3rd of September in 2014, a couple of weeks just after the clinical trial, and I came out on the 6th of October. I kind of looked like a raisin. I went in looking like a grape and came out looking like a raisin. I lost about 100 pounds. I couldn’t move. I was in a wheelchair and had a walking aid to get to my studio. I couldn’t move from there for quite some time.
Did you have follow-up scans post-transplant?
After that, we had updated tests and scans. I had blood tests and I had to see my doctor every week. We did scans every 2 months or so. We did CT scans, and even just the fluid for the CT scans, PET scans, and things like that would make me sick for days. I still couldn’t move. Whenever I was in the hospital, I always was in a wheelchair and then I had a walker. It was like baby steps. I couldn’t move more than half a foot in front of each other. It took me quite a long time to get moving again.
Reflections

This month, January 2024, is actually 12 years to the month of the original diagnosis. A couple of months to live to 12 years and still going, getting better and better.
The importance of diet and exercise in staying cancer-free
Time heals everything, I guess. Getting the right food helps as well. Throughout the whole period, we never ate takeaway food, junk food, or anything like that. It was all my wife’s cooking and my cooking. Always home prepped, home-cooked meals. That, I think, was the key to surviving Later on, progressing to where I am now, it has been all diet. I’m now 9.5 years in remission.
This month, January 2024, is 12 years to the month of the original diagnosis. A couple of months to live to 12 years and still going, getting better and better, and it’s all come down to my diet and exercise. It’s been a big help.
»MORE: Learn More About Cancer Remission
Do you have any advice for cancer patients?
Staying positive is a very big thing. It’s very difficult to do in situations like that. We all get in stressful situations in life, but I think a lot of the stress that we feel is internal because of the way we think about the situation. I like to break down every situation into small, easy, achievable steps. If you feel like you’ve got a mountain to climb in front of you, don’t look at the mountain. Just focus on the next step. I think dealing with the situation as it came made it easier for me.
I didn’t try to look at everyone else’s story too much, although it was nice to get information and helpful tips, but you’re going to react to things differently. Impossible is nothing but motivation. To me, when you get a bad diagnosis, it doesn’t mean that’s the end of everything. They told me many times there were situations where I almost didn’t make it. But if you stick with it, if you believe in yourself, even if everyone around you tells you that it’s going to be like this, that doesn’t mean it’s going to happen.
Just because it hasn’t been done doesn’t mean you can’t do it. They just haven’t seen it yet. So believe in yourself, believe in God, have faith in yourself, and you will get there. It is frustrating, it takes time, and even if it’s slow going, even one step forward is still getting you one step closer. Don’t try not to fall into the trap of, “Poor me. Here we go.” That’s all I can say – just focus on moving forward. Get the job done and you will get there. I promise you.
Thank you for sharing your story with us, David!

I’m happy to help and I hope my story does help some people who are going through this sort of treatment as well.
More Follicular Lymphoma Stories
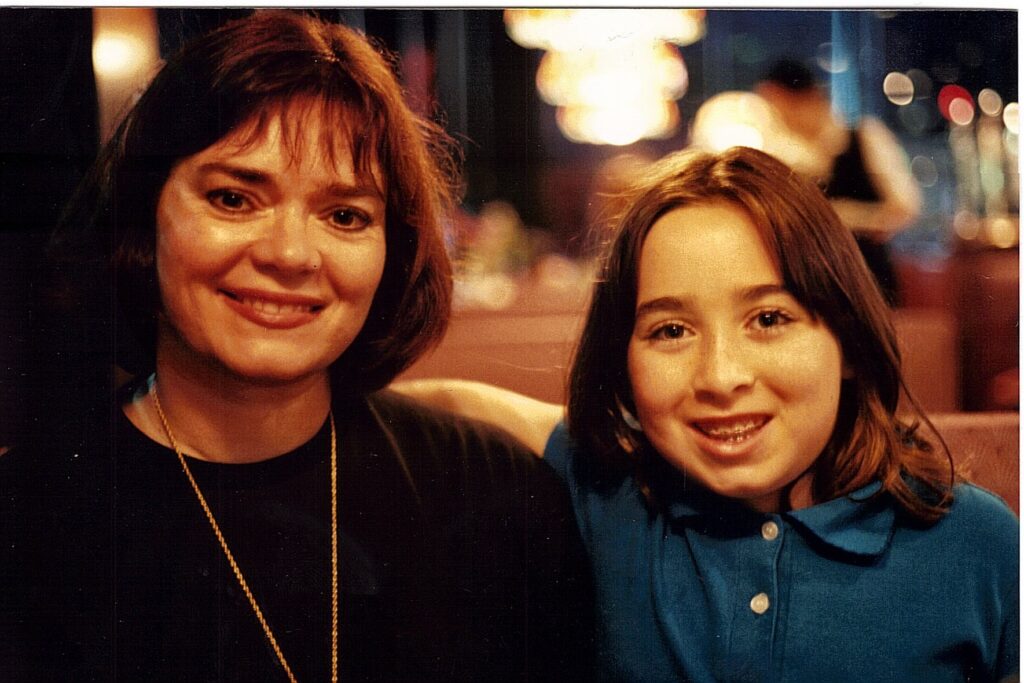
Hayley H., Follicular Lymphoma, Stage 3B
Symptoms: Intermittent feeling of pressure above clavicle, appearance of lumps on the neck, mild wheeze when breathing and seated in a certain position
Treatments: Surgery, chemotherapy
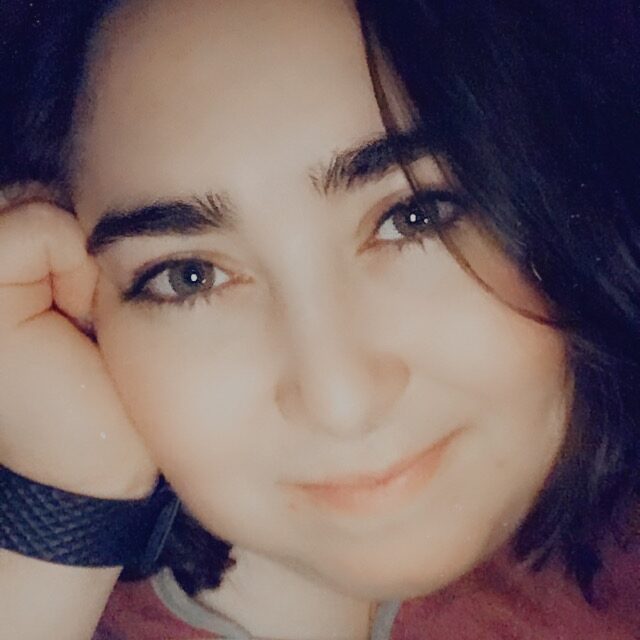
Laurie A., Follicular Non-Hodgkin Lymphoma, Stage 4
Symptoms: Frequent sinus infections, dry right eye, fatigue, lump in abdomen
Treatments: Chemotherapy, targeted therapy, radioimmunotherapy
Courtney L., Follicular Lymphoma, Stage 3B
Symptoms: Intermittent back pain, sinus issues, hearing loss, swollen lymph node in neck, difficulty breathing
Treatment: Chemotherapy
John S., Follicular Lymphoma, Stage 4
Symptom: Swollen lymph nodes
Treatments: Clinical trial, chemotherapy