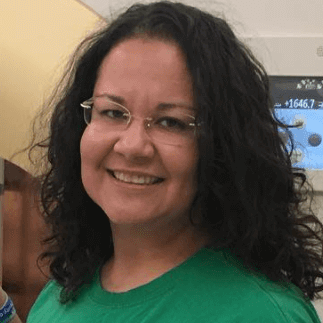
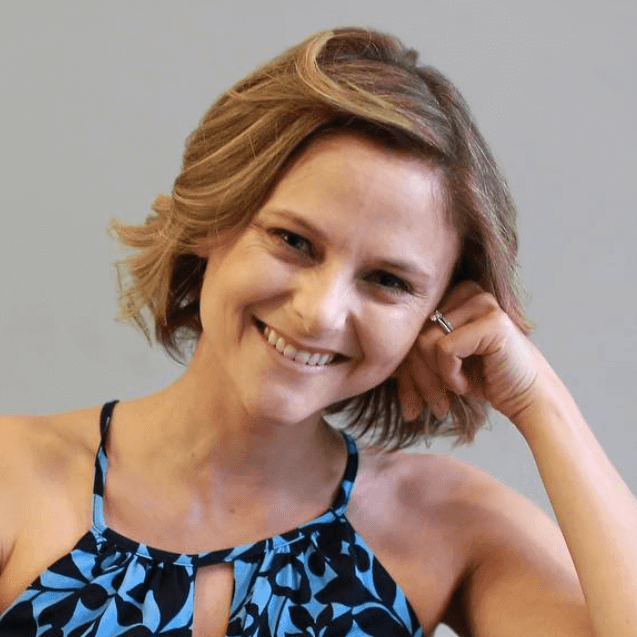
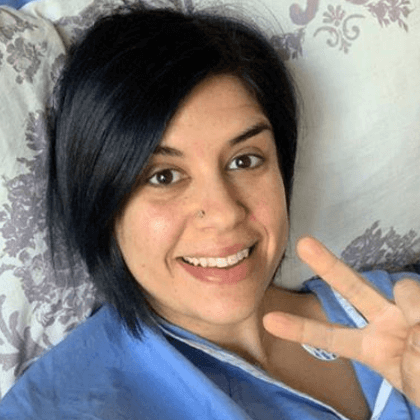
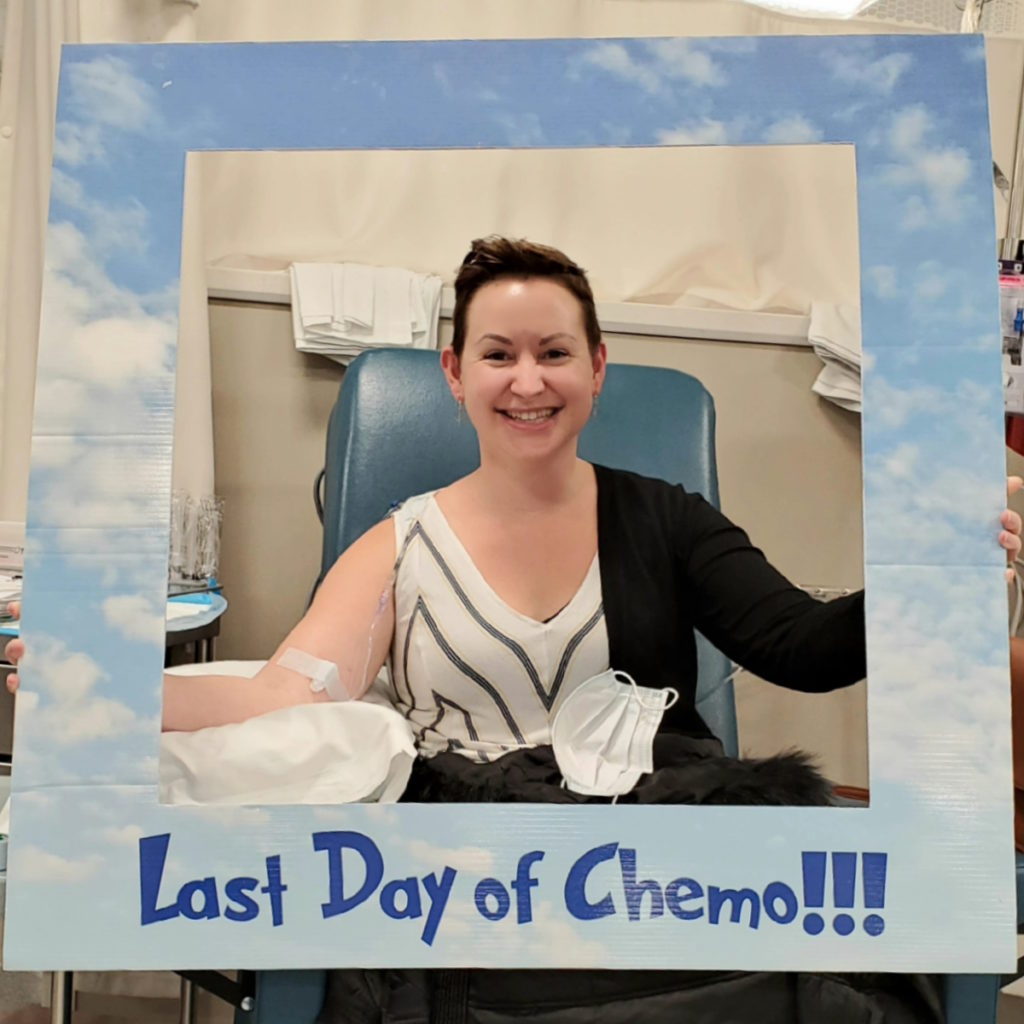
Terri Ann DiJulio’s Recurring Stage 1 Lung Cancer Story

Terri Ann DiJulio has been diagnosed with lung cancer three times. In her family, six members have been diagnosed with the same cancer.
One of the most interesting parts of her story is that she never had any symptoms. Her lung cancer was discovered through an incidental pulmonary nodule found when she went to the emergency room due to feeling pressure in her chest.
With her survivorship comes a profound sense of responsibility to do something, to make a difference so that it can help other people. She believes she’s here for a reason and wants to do something meaningful with this gift of life.
In addition to Terri Ann’s narrative, The Patient Story offers a diverse collection of lung cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Terri Ann D.
- Diagnosis:
- Lung Cancer
- Staging:
- 1
- Initial Symptoms:
- None; incidental lung nodule finding
- Treatment:
- Lobectomy
- Stereotactic body radiation therapy (SBRT)
- Wedge resection
I’ve been diagnosed three times over many years of being stable so now, it’s always in the back of my mind.

I never had symptoms. My lung cancer was discovered through an incidental pulmonary nodule found in the emergency room.
Introduction
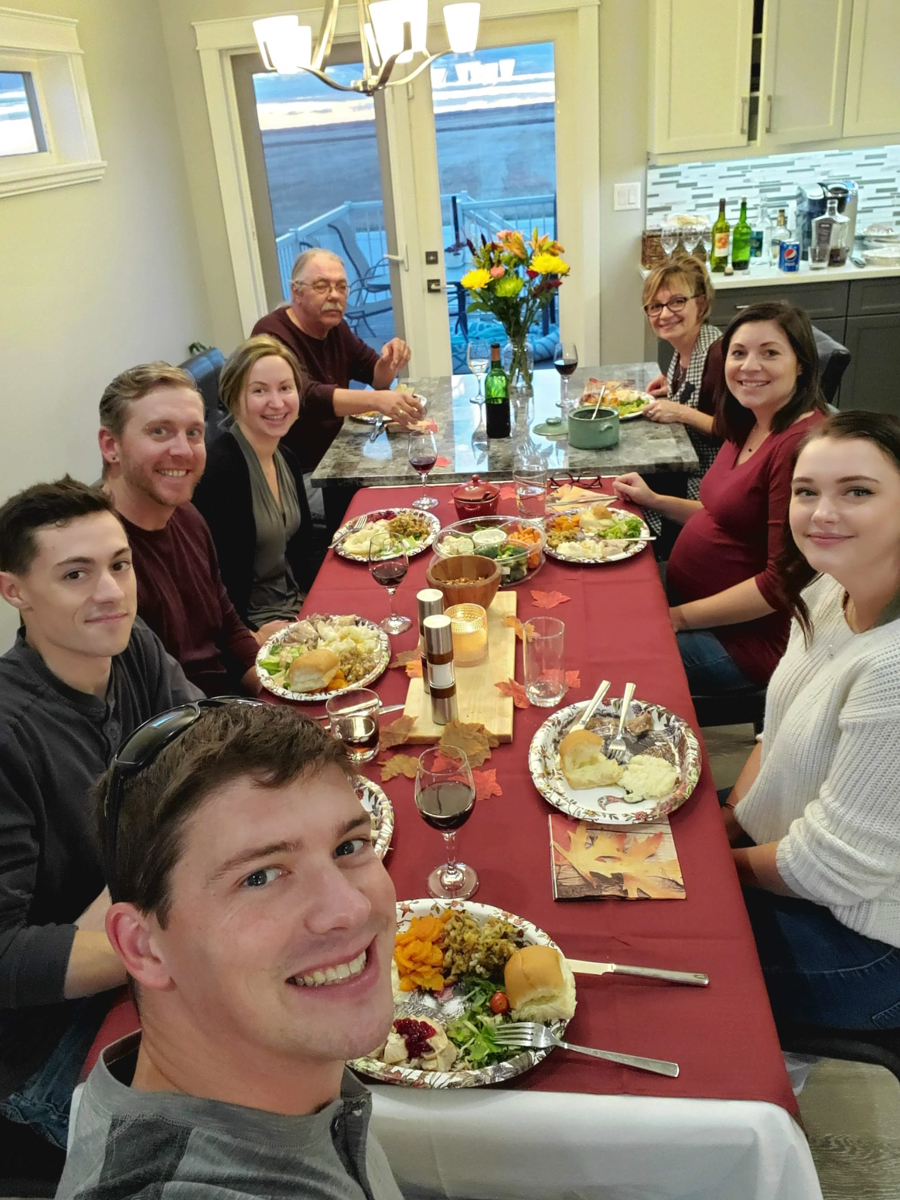
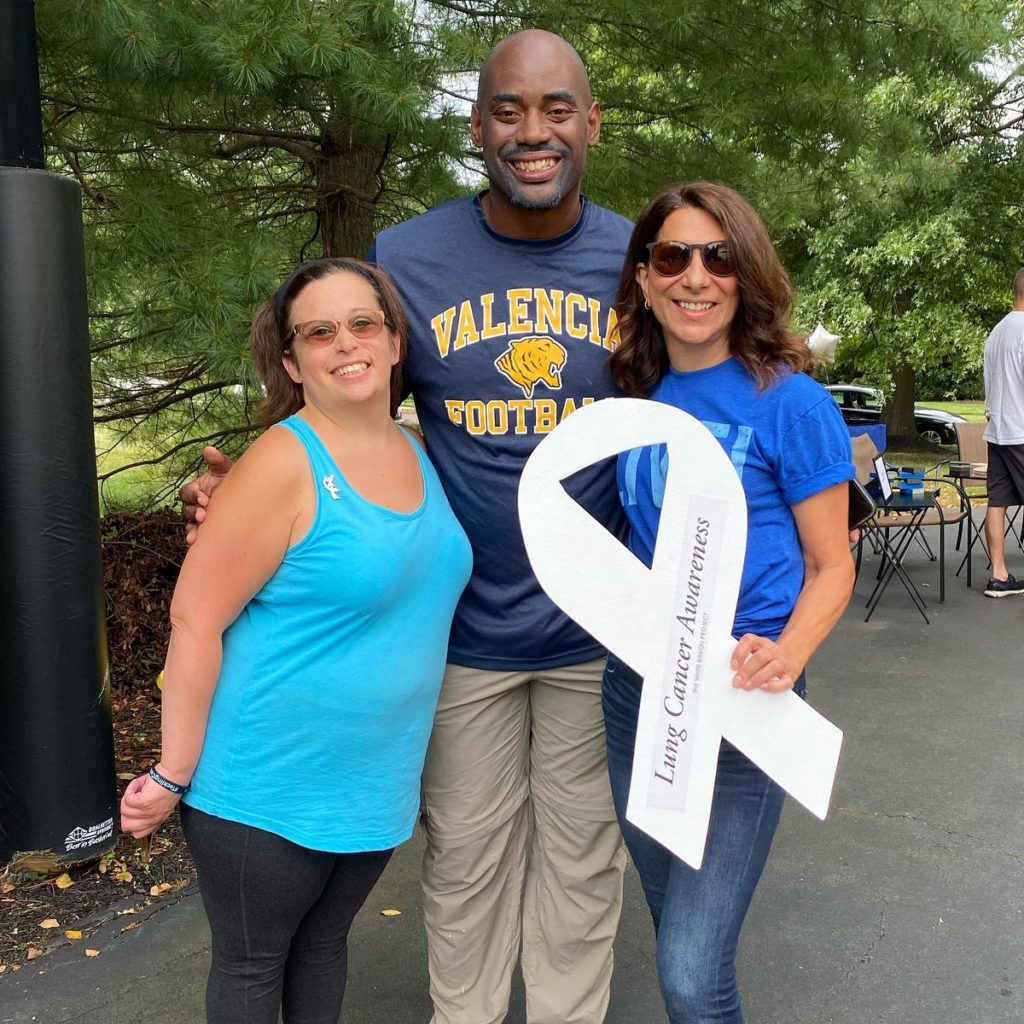
I’m an avid cyclist. I actually use cycling as a fundraising tool for [the] lung cancer community.
I’m an artist. I have an art studio in my home. I had a 35-ish-year career in event planning and just dissolved my company to move into the next chapter.




I do a little bit of everything. I was considered a master craftsman in jewelry design and metalsmithing. But, unfortunately, that is a little bit toxic so after my second lung cancer diagnosis, I gave that up.
Right now, I’m working in encaustics, which is working with warm wax, and I’m also working with alcohol inks.
I like to write, read, art, and cycle.





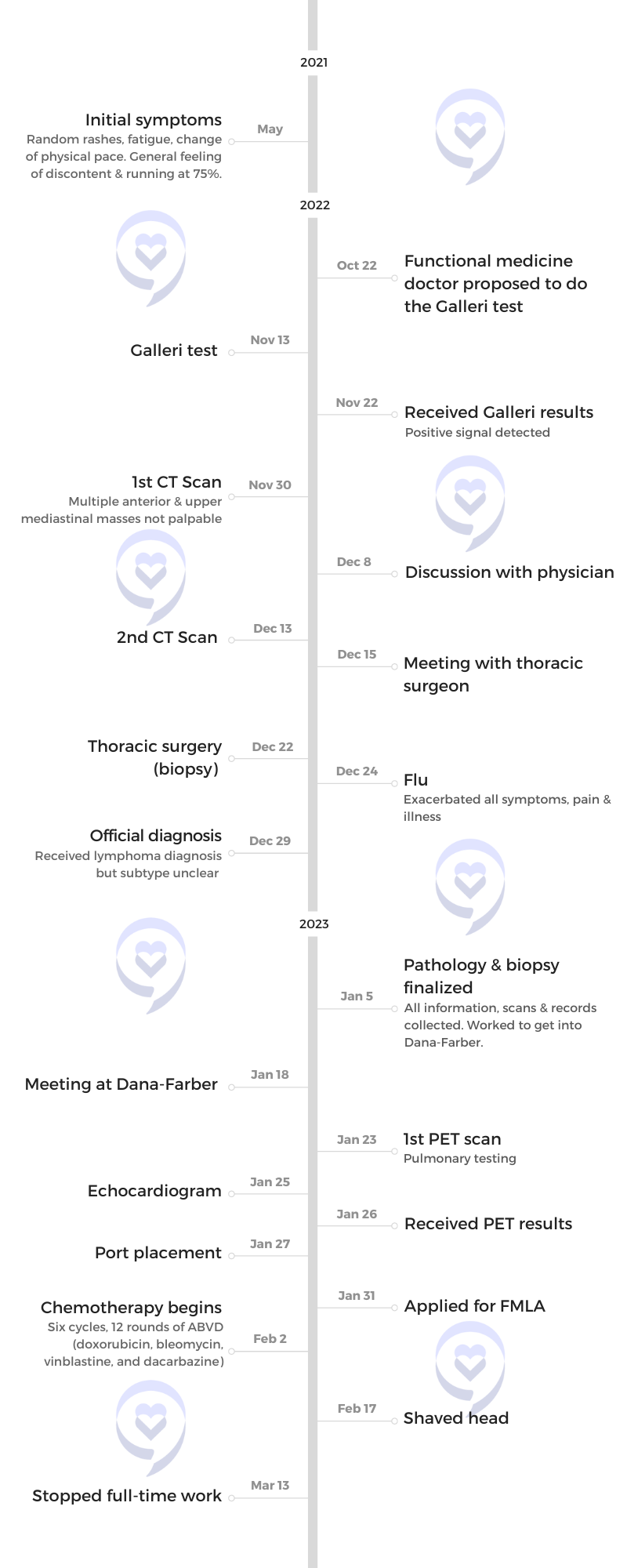
First lung cancer diagnosis
No initial symptoms
The most interesting part is I never had symptoms. My lung cancer was discovered through an incidental pulmonary nodule found in the emergency room. Because it was early stage, my lung cancer had no symptoms whatsoever.
My primary care physician urged [me to go] to the emergency room because I was feeling pressure in my chest. My heart turned out absolutely fine. I was just a little stressed at work. Turned out to be anxiety. It was a blessing that I had a very stressful job and ended up in the emergency room.
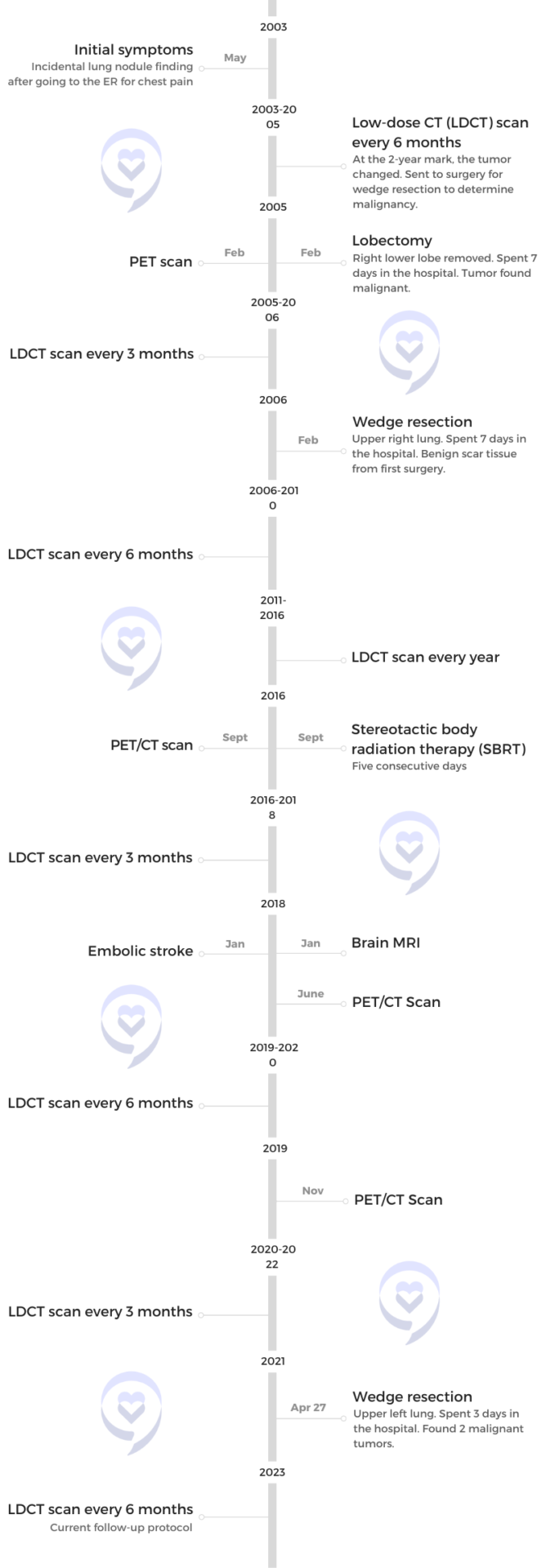
They found a nodule in my right lung. They watched it every six months for a couple of years. It was a follow-up program now more formally called an IPN (incidental pulmonary nodule) management program that a lot of hospitals have.
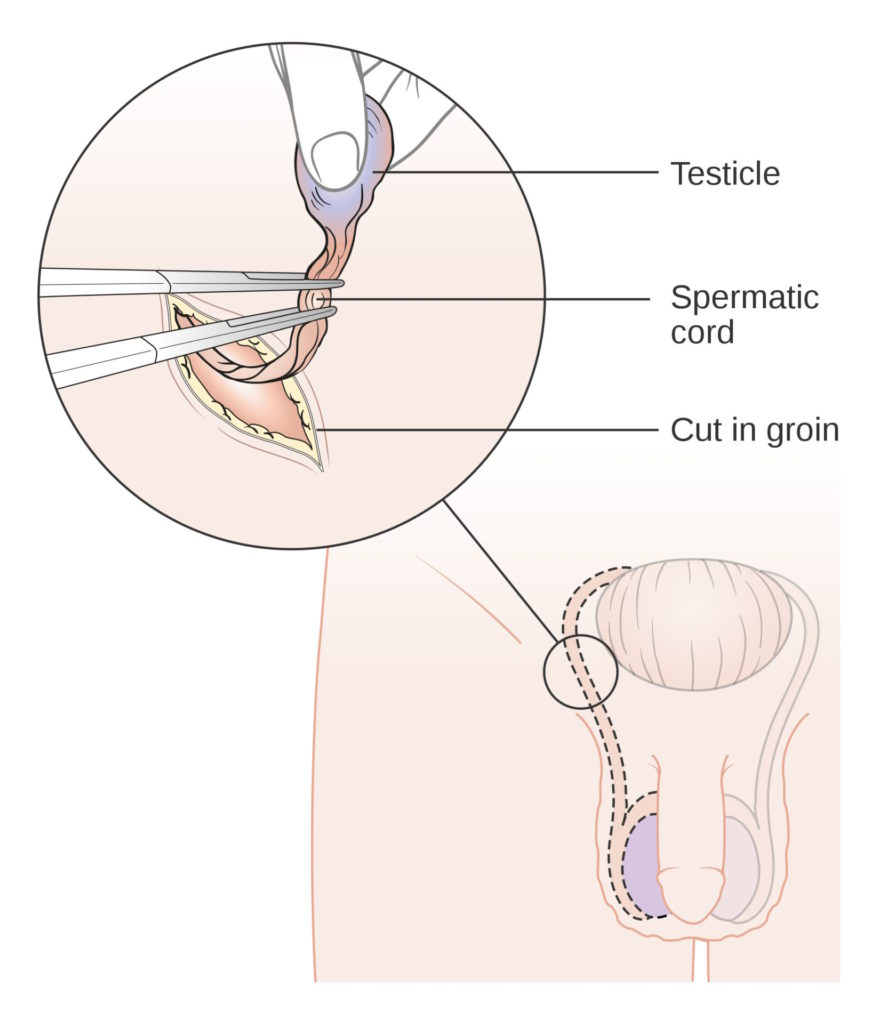
When it changed, I was sent to a thoracic surgeon who was going to biopsy it while it was on the table. It was malignant [so] they removed the lower right lobe of my lung during surgery.
I was 42 when it was found and 44 when it was diagnosed. We watched it for two full years.
I knew nothing about lung cancer then. Everybody kept saying, “We think it’s something you were born with.” It hadn’t changed. Every time I went, it was stable so I actually didn’t think about it during those two years.
Since then, I’ve been diagnosed three times over many years of being stable so now, it’s always in the back of my mind.
A year after my first diagnosis, my mother was diagnosed with lung cancer [in] the exact same way.
Removing the lower lobe of the right lung
The following year, they found something in my upper right lung so back to surgery I went. The good news is that turned out to be scar tissue from the first surgery. I was watched every six months for five years and then annually from then on.
I was no evidence of disease for 11 years between my first and second lung cancer diagnoses. Typically, at around the 10-year mark, you’re in the clear. But I wasn’t.
A year after my first diagnosis, my mother was diagnosed with lung cancer [in] the exact same way. She went to the emergency room thinking she was having a heart attack and it turns out that she had stage 3 lung cancer.
I’ve had lung cancer three times. I was the very first one in my family diagnosed. Six of us have been diagnosed with lung cancer. Two of us were diagnosed early. Two of us survived the disease.
We’ve never been able to participate in studies. When everybody was first diagnosed, they weren’t doing that so we don’t know. We did find out the mutations of one family member who died two years ago.

Based on where it was located, the surgeon told me the only surgical option was to remove my entire lung.

Second lung cancer diagnosis
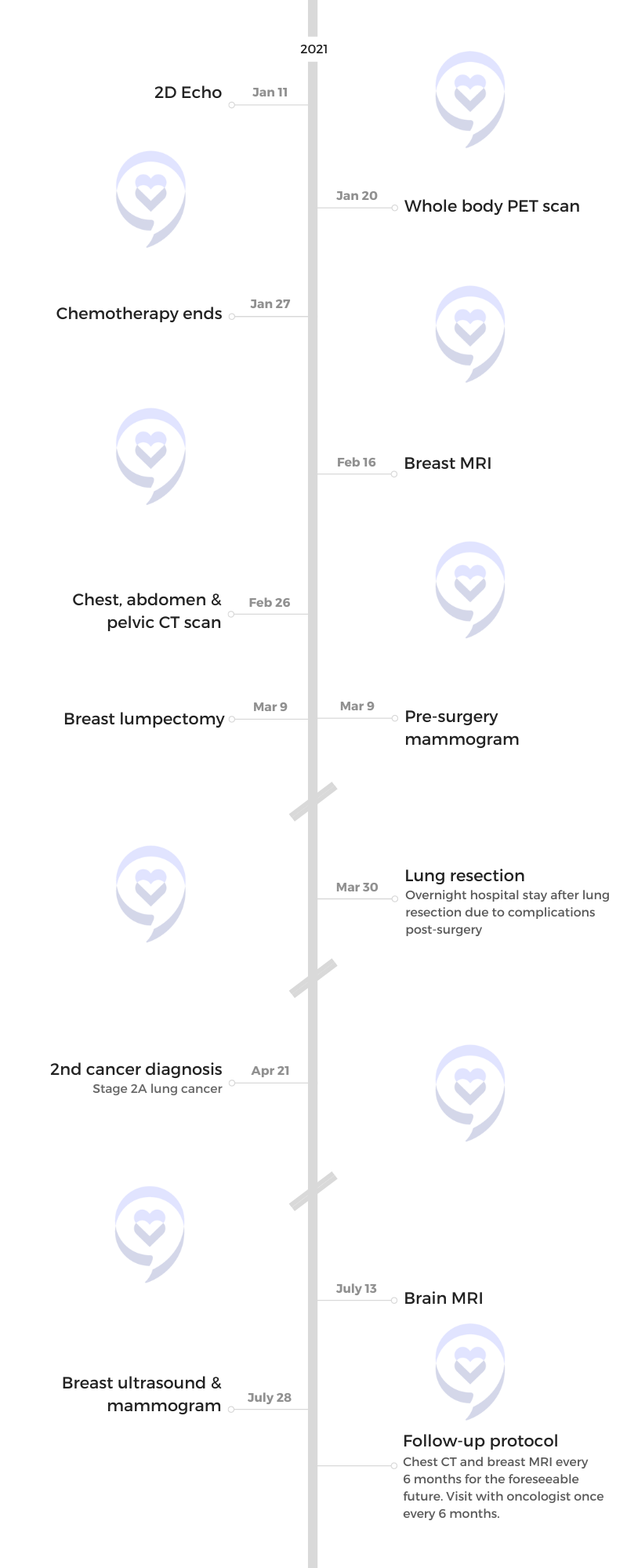
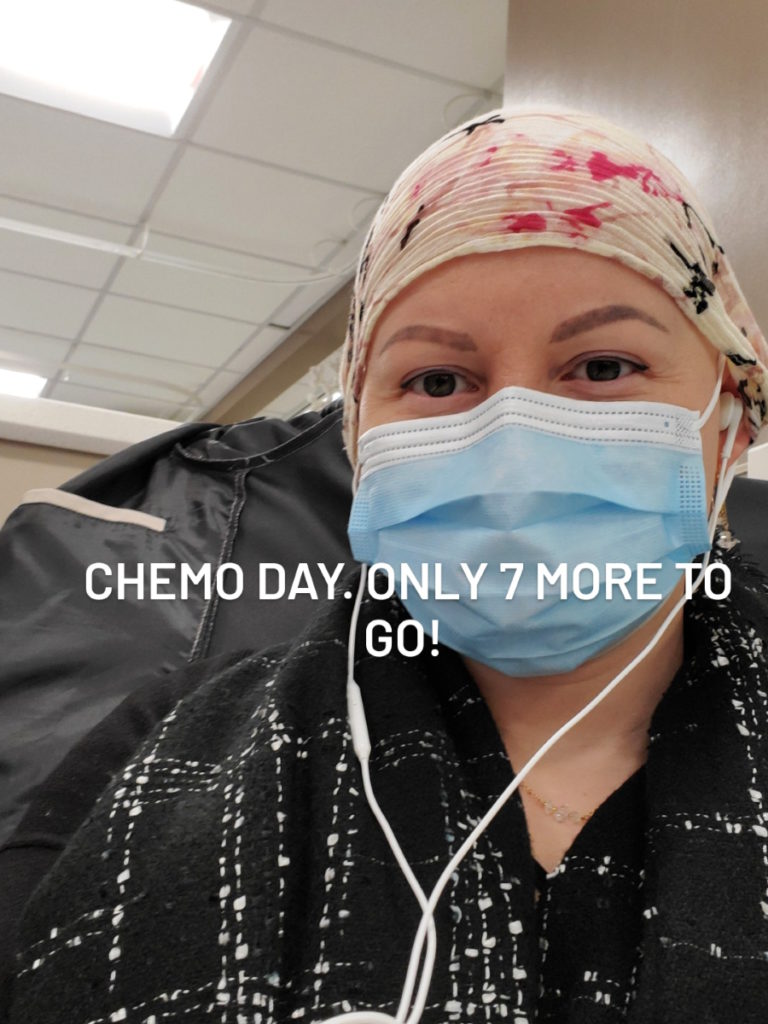
Because I was in a management program, we also discovered the second early. My pulmonologist left clinical medicine [so] I had to find a new pulmonologist. We are lucky to have Penn Medicine in our backyard. My uncle was going to a pulmonologist there so I went [to] his pulmonologist.
I was on annual X-rays at that point and he said, “I can’t really see anything on an X-ray. Go get a CAT scan, come back, and we’ll probably just do annual screenings.” I got a CAT scan, went in for my appointment, and that’s when he told me I had lung cancer for the second time.
It was in my right lung. I’ve already had two surgeries [on] my right lung. It was small but based on where it was located, the surgeon told me the only surgical option was to remove my entire lung. The tumor was pretty small so we didn’t want that.
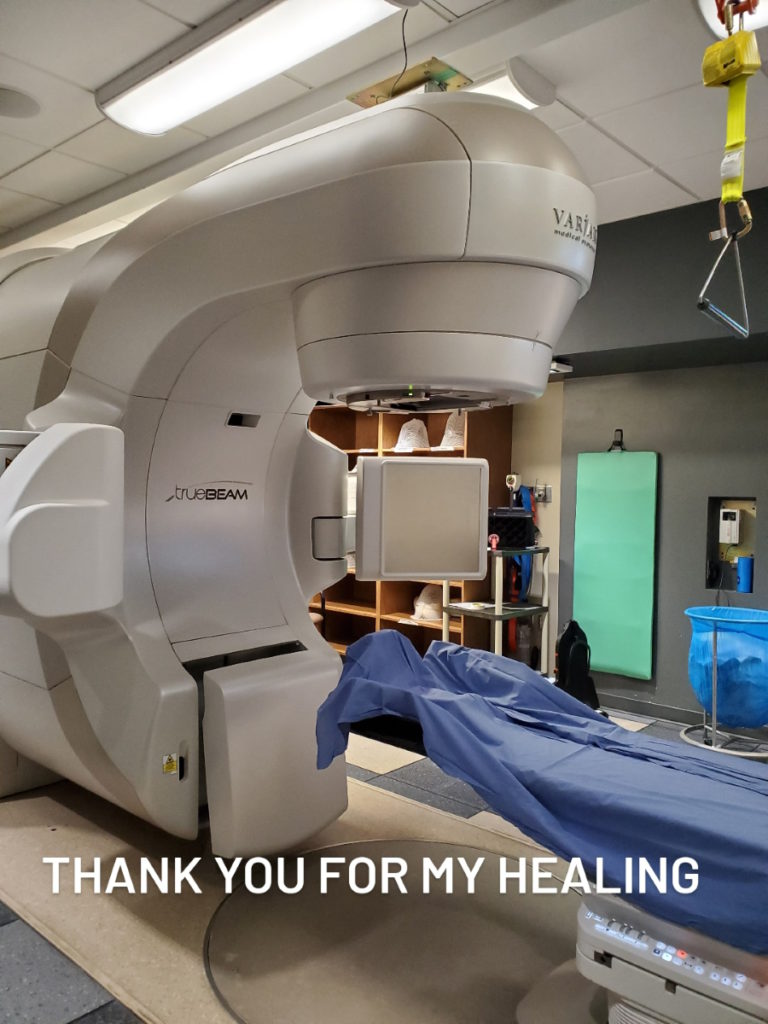
I met with radiation oncology and they were able to treat me with SBRT (stereotactic body radiation therapy), which is like targeted radiation. It pretty much obliterated the nodule.
When I was first diagnosed, that treatment was not available to me or my mother because they weren’t doing SBRT on a moving organ. You could have targeted radiation on your brain, but you couldn’t have targeted radiation on your lungs. But since the advances in treatment, I was able to have that.
I suffered an embolic stroke. Nobody really knows why other than it could have been related to my cancer diagnosis.
Differences in treatment options
My first surgeries were so difficult. I was in the hospital for over a week each time — very painful chest tubes, months of recovery, [and] thoracotomies. It was hard.
[With] radiation, [on] my third day of treatment, I went for a 20-mile bike ride. Ten days after my treatment, I was exhausted and spent about two days in bed. That was the only side effect I had from radiation.
I’ve been so lucky because my first one was diagnosed early. We’ve been watching it so every diagnosis I have has been at an early stage.
Follow-up protocol
After about six months, they found a cloudy spot on one of the vertebrae in my spine. At that point, I was following up with my pulmonologist. They sent me to medical oncology because we weren’t sure if it was damage or metastasis.
I’m happy to say it wasn’t metastasis. It was from radiation.
[In January 2018], I suffered an embolic stroke. Nobody really knows why other than it could have been related to my cancer diagnosis because a blood clot shut down my internal right carotid artery. It took me probably eight months to recover.
From then, I was stable, [had] no evidence of disease, and followed up every six months for two and a half years. Then they discovered something else and I was switched to every three months until my third lung cancer diagnosis.

‘If I go with radiation, is it possible that that will hinder treatment down the road should I have a fourth diagnosis?’

Third lung cancer diagnosis
They found a tumor in my left lung, which was my good lung.
I was getting low-dose CT scans every three months. When they discover something they’re unsure of, I get a PET/CT to see if anything lights up.
They saw something suspicious; a solid nodule that wasn’t there before. We wanted to watch it until it comes to the point [that] we’re pretty sure this needs attention. Sometimes the treatment or the biopsy is harder on your body.
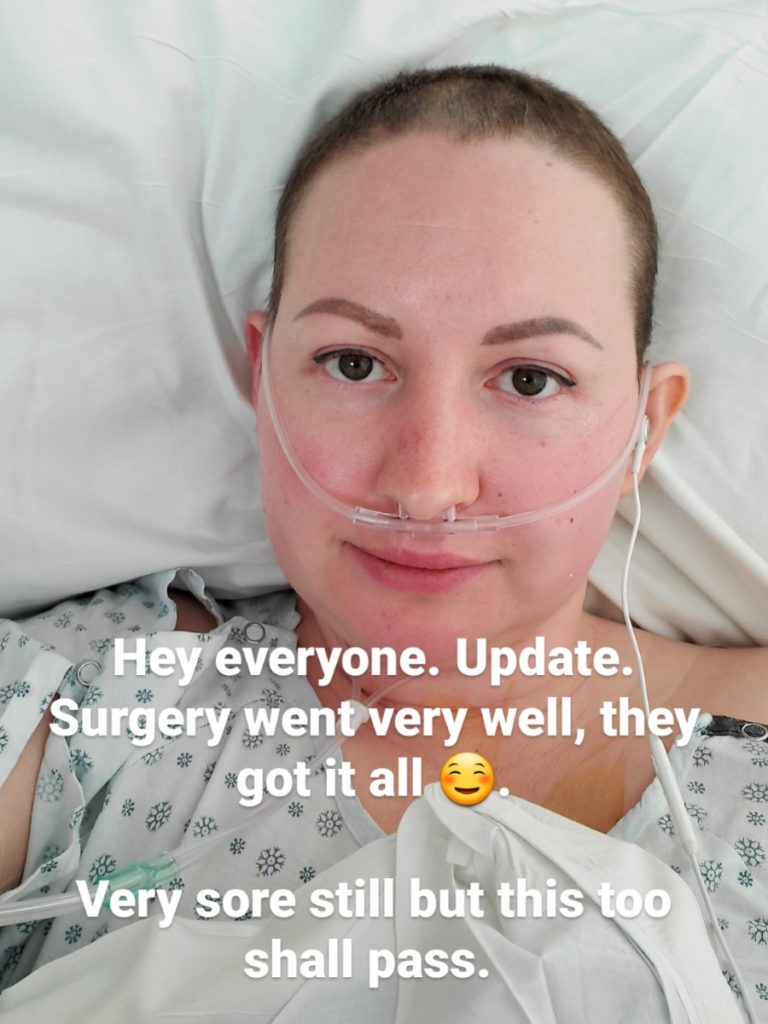
It got to the point [where] it’s changed. It’s grown. It needs attention. I met with a thoracic surgeon and all the different doctors. Then I came back to my pulmonologist to make the final decision.
Quite frankly, I didn’t want surgery. I had an awful experience with my first two surgeries. I wanted radiation.
My radiation oncologist said, “You’re strong and healthy. Surgery really is your best option. But if you want me to radiate this, I can get it. It’s your choice.”
I asked him one question that changed my mind. “If I go with radiation, is it possible that that will hinder treatment down the road should I have a fourth diagnosis?”
He said, “It’s possible that if you go with radiation, you won’t be able to have surgery down the road because of the damage radiation will do to your lung,” and that is all I needed to hear.
The surgeon felt confident that he could get it and that the surgery would be easier. I chose surgery.
‘A second tumor glowed that didn’t show up on any of your scans.’
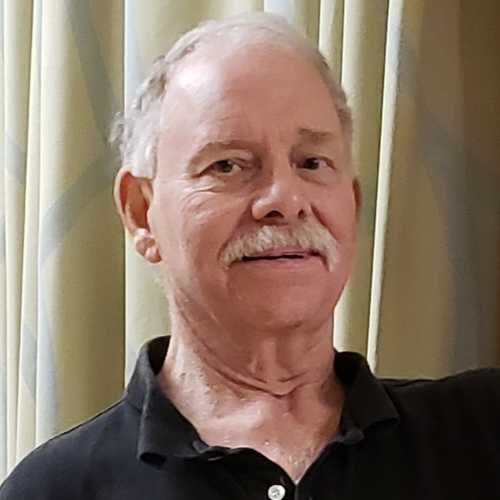
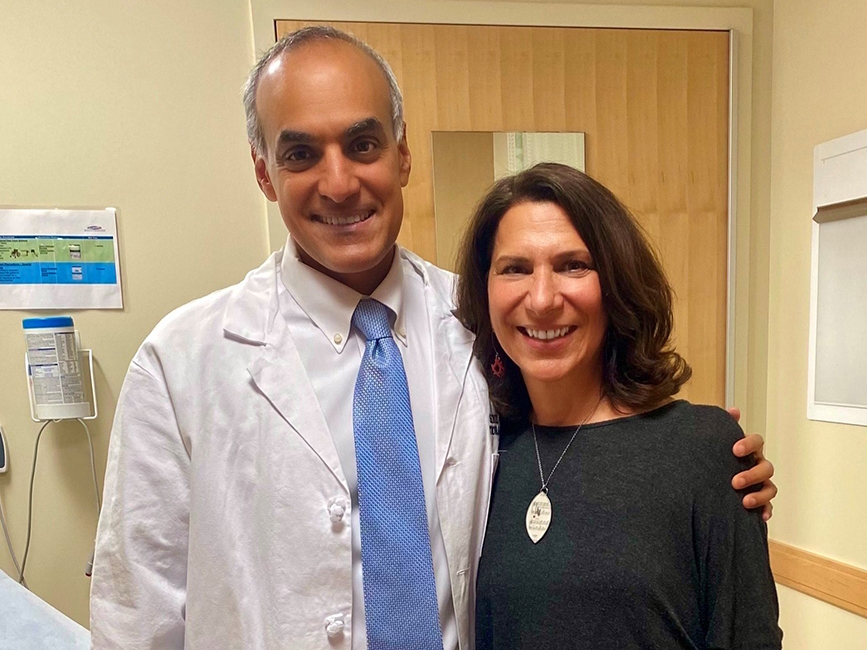
Terri Ann’s surgeon
Participating in a clinical trial to study TumorGlow
When I asked how he was going to find the tumor, he said, “My fingers are small. We’re going to make the incision and then we feel around for it.” I said, “That’s what they were doing all those years ago.”
My surgeon was a principal investigator in a study [for] TumorGlow. He said, “I don’t know [if] it will really help you, but you can be in the study.” It was a randomized phase 3 trial for an imaging agent. They inject you with a fluorescent dye the night before your surgery.
He said, “We don’t know if you’ll get it or not. I locate the tumor in the operating room. They open the envelope and if you get the study, we can use the special camera that allows the tumor to glow and we cut it out.” I said, “I’m in. Please sign me up.”
I’m a total lung cancer science geek now because of all the advocacy work I’ve done so I wanted to do it. I qualify.
I woke up from surgery and said, “Did I get the special envelope?” They said, “Not only did you get the special envelope, a second tumor glowed that didn’t show up on any of your scans.”
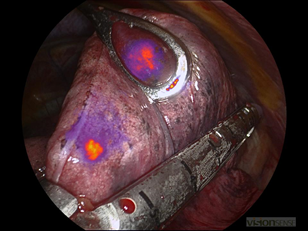
Both tumors were in my left lung. They’re really pretty close to each other.
Finding a second tumor
Both tumors were malignant. Because my doctor knows who I am and how active I am, he took out as little lung as he needed to with clean margins. I went right back into my world after I recovered from my surgery. I’m still able to cycle, be active, and do all the things that I love to do.
That imaging agent was just FDA-approved for lung cancer in December 2022 so it felt amazing to participate in that, that it helped me personally, and that now it can help all these other patients.
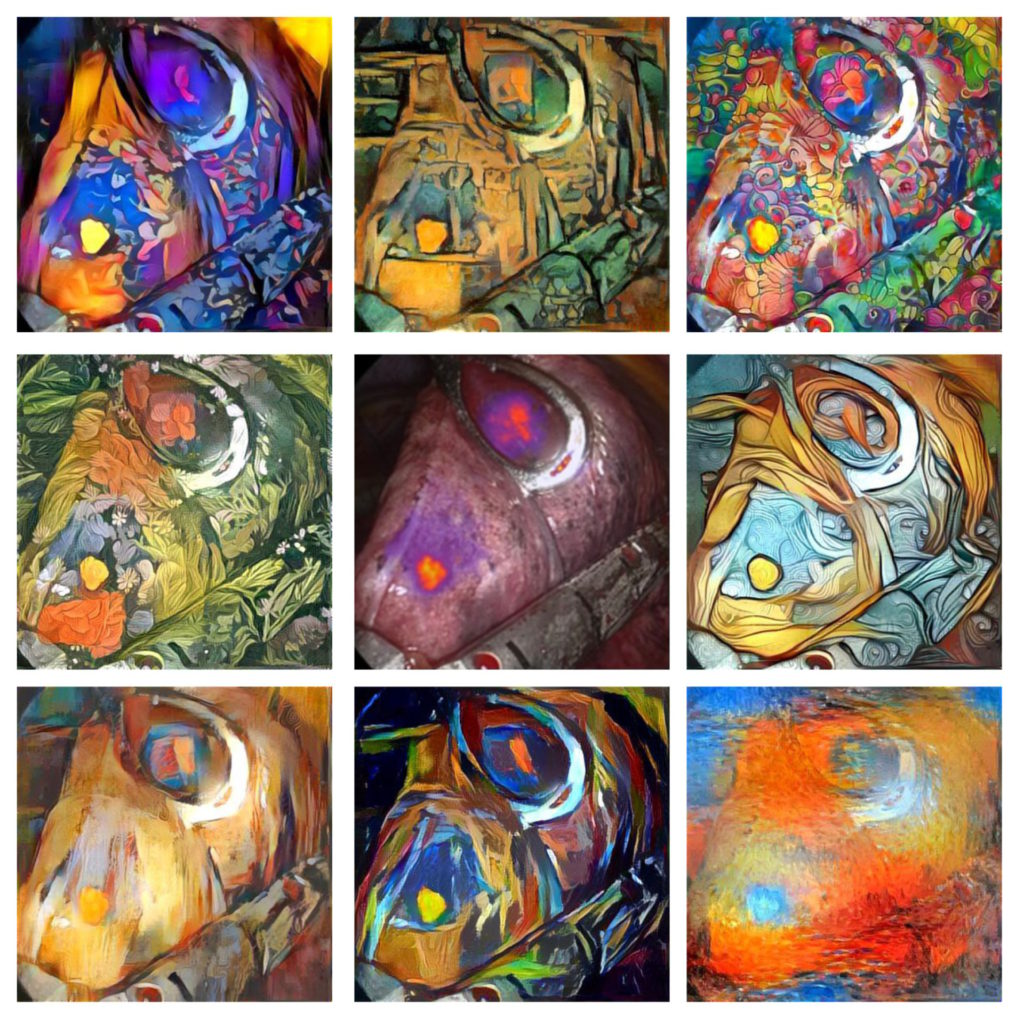
I have a picture of my glowing tumors. My best friend knows how much I love beautiful things. I sent her that image and she sent back these altered images of that surrounding it. We titled it “Beauty and the Beast” and I now have it as a piece of artwork.
Both tumors were in my left lung. They’re really pretty close to each other so he was able to get them both out in the same wedge. He checked my entire lung. At the time, these were the only tumors in my left lung.
I like to know how things are going to work. It’s just the type of patient I am. I don’t like surprises.
Participating in treatment decision-making
I wanted assurance that it wasn’t going to be the same. I also like to know how things work. I like to understand. I remember the first time asking my doctor, “Walk me through it,” and that’s when I learned.
He said, “We collapse your lung.” I said, “How do I survive surgery if you collapse my lung?” Your other lung does all the work. When he was describing a thoracotomy, he said, “Then we cut and use a rib spreader.” I actually looked at him and said, “Okay, now I think I’ve asked one too many questions.”
I like to know how things are going to work. It’s just the type of patient I am. I don’t like surprises.
I’ve been blindsided a couple of times [when] I walked in thinking everything was going to be fine just to find out it’s not.

Reaction to a third lung cancer diagnosis
I always knew in the back of my mind that this is just part of my life, but it’s still really stressful. Even with early-stage lung cancer, knowing they can cut it out, radiate it, treat it, and you can still live, it’s still very stressful and weary, quite honestly.
It’s always in the back of my mind. It never leaves. In the cancer community, we fondly refer to it as scanxiety. You get your scan then you have to wait to find the results. Typically, I’m fine, but I’ve been blindsided a couple of times [when] I walked in thinking everything was going to be fine just to find out it’s not. That never leaves you.
Managing scanxiety
What I try and focus on is that there is nothing I can do. Until I know there is something that needs action, I’m not going to waste the precious time I have worrying about it. It can be in the back of my mind and I can acknowledge it, but I don’t have to allow it to be all-consuming.
I can continue to live my happy, beautiful, blessed life and worry about it when I have something to worry about. Otherwise, I try and put it in the back of my mind.
Exercise helps me clear my head. With everything that has happened in my family, I’ve done a lot of work on being present. I’ve done a lot of internal work. I’ve done a lot of reading. Being present and trying to bring myself into the present moment is what helps me when I’m dealing with uncertainty.
What am I doing right here [at] this moment? All I know is what’s happening [at] this very moment. Learning techniques to keep me in the present moment helps tremendously with scanxiety.
We desperately need advances in the lung cancer space. If I can do something to help those advances, then I’m happy to do it.
Preparing for the clinical trial
There were a ton of documents I had to sign. Quite frankly, for being such an informed patient, I didn’t read every word. You have to go through a book — all the things that can happen, all the things that might not happen. I just signed the papers.
The prep wasn’t that bad. I went the day before [and] was injected with the fluorescent dye, which took about half my day because I had to be monitored, then I got to go home. The next day, I came back for my surgery.
Deciding to participate in a clinical trial
This was an easy decision for me. It was enhancing a treatment that we felt confident was going to be successful.
I really didn’t think there would be any benefit to me other than assisting the surgeon. In this particular situation, not only did it benefit me but the fact that it could help other patients is what was most appealing to me. It was taking science to another level.
I imagine it’s scary for later-stage patients going into clinical studies where they’re hopeful it is going to work to slow down the progression of their cancer.
There are so many components to being involved in a clinical study. Putting my good result aside, the most appealing to me is that we desperately need advances in the lung cancer space. If I can do something to help those advances, then I’m happy to do it.

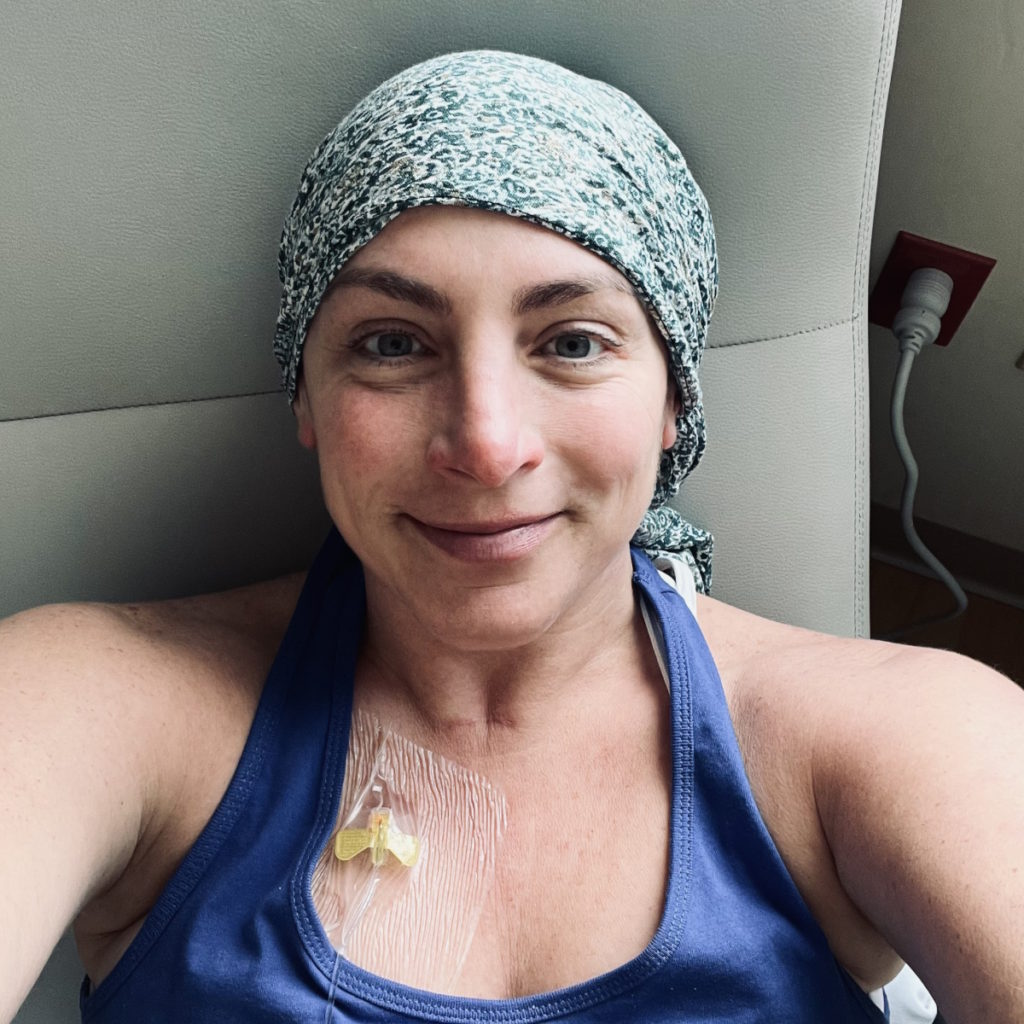
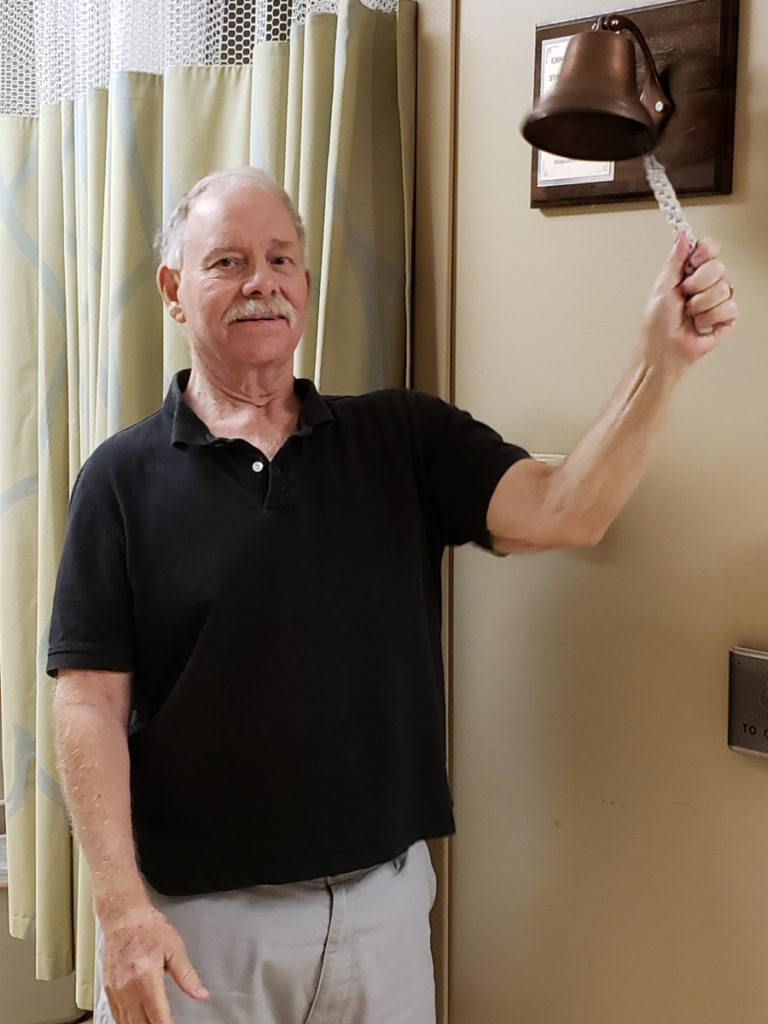
Thirty days after surgery, I went on a 30-mile bike ride to celebrate. I could never have done that 18 years ago.

Recovering after lung surgery
This surgery was so different than my first surgery. I was only in the hospital [for] three days. I came home, took it easy, and gradually worked my way up.
I started with walking. But 30 days after surgery, I went on a 30-mile bike ride to celebrate. I could never have done that 18 years ago. I was still in pain 30 days after surgery. I wasn’t cleared. That was pretty miraculous and something to be celebrated.
Follow-up protocol
I had COVID in August 2022 and had some lung damage so [I] was put back onto a three-month follow-up because we weren’t exactly sure what was going on.
I was just released back to a six-month follow-up and we’ll probably stay there for a couple of years as long as everything stays stable. I’m considered no evidence of disease right now.
Every once in a while, I get a text or an email from one of my doctors saying they have a patient that’s interested in advocacy.
Being a patient advocate
I’m a pretty outspoken advocate for our community. I get really involved in fundraising and legislative policy.
I tell them all the things I’m involved with and that our community would welcome other patients. If any of their patients want to get involved, [they’re] free to pass along my information. Every once in a while, I get a text or an email from one of my doctors saying they have a patient that’s interested in advocacy.
I end up working with fellow patients of my doctors, telling them all the ways that they can get involved if they’re interested. I tell my doctors who I am, what’s important, how I can help, and how I want to help.
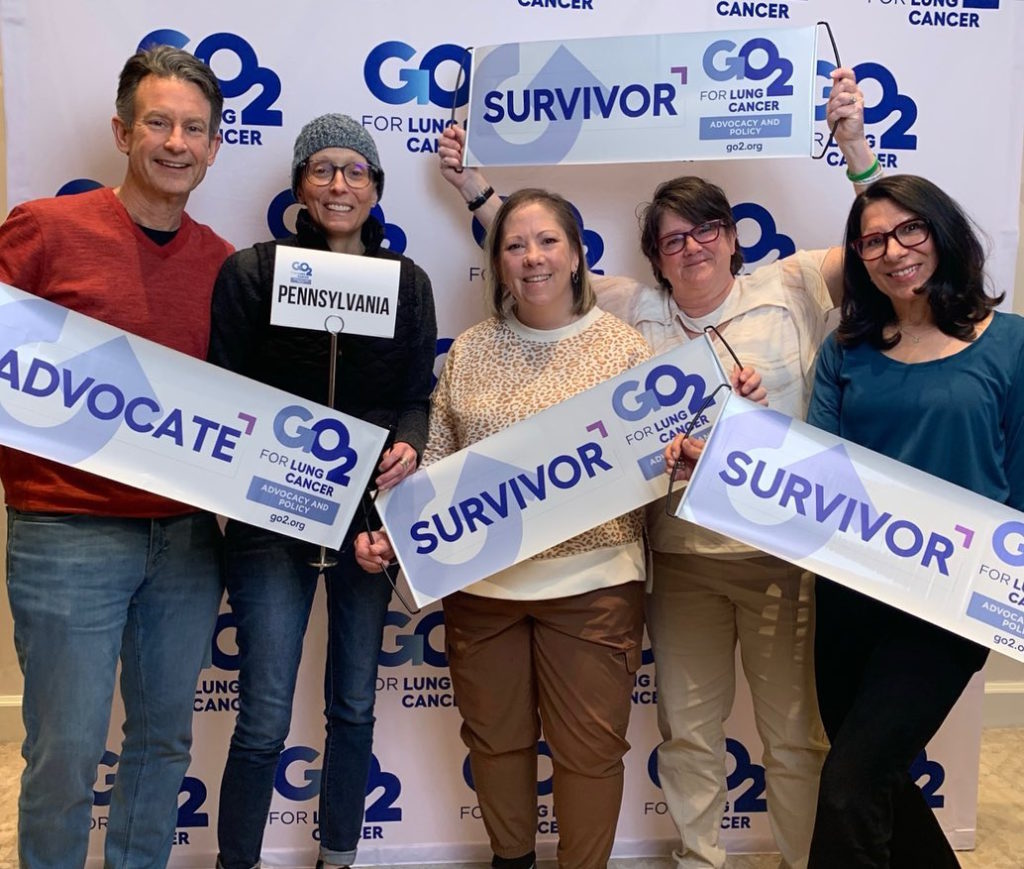
We go to Washington as a community and ask our representatives to support an increase in the lung cancer research program.

Legislative work for lung cancer support
Some of the legislative work we’re doing is asking for an increase in federal funding.
Lung cancer kills more people than any other cancer, period. As women, we have a greater chance of dying from lung cancer than from breast cancer. Lung cancer receives a lower amount of federal funding than other cancers.
We go to Washington as a community and ask our representatives to support an increase in the lung cancer research program. The lung cancer research program is through the CDMRP (Congressionally Directed Medical Research Programs) through the Department of Defense because the military has a greater risk of lung cancer from all the chemicals and everything the military has to go through.
We asked for an increase. We got $25 million. We’ve gone in and asked for $60 million. That’s some of the legislative policy work that we’re involved with.
I’m also a consumer reviewer for the Lung Cancer Research Program. I get to see firsthand all the great research that’s coming through, but all the great research that has to be turned away, too, because we don’t have enough funding so that’s why we need more funding.
I’m here for a reason. I want to do something meaningful with this gift of my life.
Educating people on lung cancer
I try and get out and speak as much as possible. Through my lung cancer journey, I personally have found my calling. I will speak to anybody who will listen about the risks and facts about lung cancer so that we can spread the word.
If I tell you and you tell someone else and you’re in a conversation at a cocktail party and you mention this conversation, it’ll trickle down the lane. Maybe that person will say, “Oh, I’ve got risk factors. I’ll go get screened.”
We need to educate each other. We need to treat lung cancer patients with dignity [and] kindness, not ask them the smoking question, the elephant in the room. Move forward with getting people screened, finding the disease early, and advancing research treatment options.
With my survivorship comes a profound sense of responsibility to do something, to make a difference, to do something with my family’s journey so that it can help other people, potentially the next generation of my family. They’re not here, but I am and I’m here for a reason. I want to do something meaningful with this gift of my life. And I found it through this.
Learn about lung cancer from first symptoms to navigating life with cancer »

No one is going to be more invested in your lungs than you are.

Words of advice
Taking extra steps
I have an amazing medical team. My medical team consists of an interventional pulmonologist, a medical oncologist, a thoracic surgeon, and a radiation oncologist. Because of my family history, I’m not a typical early-stage patient because my body seems to keep producing malignant tumors in my lungs.
I go to my pulmonologist and when something is discovered, we talk about treatment options. Even though I’m followed by my medical oncologist, when we discover something, I usually meet with my interventional pulmonologist because he helps me weigh out the best treatment option. Is it radiation? Is it surgery?
I’m the type of patient that likes to really understand what’s going on. I ask a lot of questions. I want to understand the treatment options so I can make an educated decision.
I encourage other patients to ask as many questions as they want to make sure they understand. No one is going to be more invested in your lungs than you are. They can be the most amazing doctors, but it’s still your body.
I’ve been blessed with doctors who understand that I’m not questioning them. I’m trying to understand and educate myself.
Being an involved patient & a self-advocate
I don’t know that I was as committed to the process in the beginning as I am now.
My very first pulmonologist would hold my scans up on the screen and patiently answer all of my questions. He would point out everything so I understood it. By my second diagnosis, I was used to looking at my scans and understanding what my lungs look like.
I’ve been blessed with doctors who understand that I’m not questioning them. I’m trying to understand and educate myself.
I learned so much more going through my mother’s lung cancer journey and my aunt’s lung cancer journey because they had different stages of lung cancer. I’m a pretty well-rounded patient now. I understand not only my cancer, but I understand later-stage cancers, too.
Knowing can save your life. Not knowing can make the journey so much harder.

Following the doctor’s orders
I did what I was told, which I don’t always do, but I follow up. I take follow-up very seriously.
I encourage other patients: if the doctor tells you to follow up, follow up. Take it into your own hands. Make those appointments and make sure that you follow the schedule.
Early-stage lung cancer can look like riding your bike 400 miles over five days for a charity ride. Early detection saves lives.
People get busy, but people get scared, too — afraid of the unknown or not wanting to think about it. Knowing can save your life. Not knowing can make the journey so much harder. Break through that fear, follow up, and stay on top of it.
Make sure doctors know who you are. It’s just as important as what your disease is if not more.
Make your needs known
I make sure my doctors know who I am. They all know I’m an avid cyclist. They all know I’m fairly athletic. They all know my personality, that I’m optimistic [and] that I protect the joyful things in my life. I think that benefits me because then when they’re treating me, they know better what my goals are.
For example, I met with one doctor on the tumor board because we were looking at ablation. I decided against ablation, but when I met with this doctor, he said, “Oh, right, you’re that patient that cycles all over the country. Okay, let’s see what we can do here.”
When the doctors know you, I feel like they’re a little more invested when they understand your priorities. I do encourage everybody to make sure doctors know who you are. It’s just as important as what your disease is if not more.
I’m a direct communicator so I just tell them who I am and I tell them my goals. I told my surgeon, “How long do you think until I can ride my bike? Because that’s really important to me.” I asked those questions before surgery was even scheduled so I could understand.

If you can find out if it has a mutation, there might be a better first-line treatment for your particular type of lung cancer.

Learning about genetic mutations & the importance of biomarker testing
Something that was surprising to me is I thought it was automatically done. I asked for it.
If you’re at a point where you’re going to have a tumor or nodule biopsied, make sure you ask, “Are you taking enough tissue to do biomarker testing?” If you can find out if it has a mutation, there might be a better first-line treatment for your particular type of lung cancer.
I made an assumption that all facilities were just automatically doing this testing and they’re not. I would definitely suggest that all patients ask and actually demand it because it could be life-changing if you have a particular marker that can be treated a certain way.
Every cancer can be different. My first, second, and third lung cancer could have all had different mutations. It’s not guaranteed that it’s always the same cancer so it’s really very important to do biomarker testing.
I encourage patients to find other patients to speak with to help mentor them through the process.
Finding support as a lung cancer patient
For newly diagnosed patients, it can be really overwhelming. I didn’t know what I know now when I was first diagnosed. I went on the Internet and, even though I was [at] an early stage, anything about lung cancer was really pretty discouraging.
We have a lot of advocacy groups. We have lung cancer advocacy groups [and] groups geared towards certain mutations.
I’ve spoken to a lot of newly diagnosed patients and connected them with other patients in a similar situation. I’m also in a buddy program through GO2 for Lung Cancer.
I find that it’s really helpful to talk to other people who have gone through what you are going through or about to go through. That can offer hope, offer information, [and] guidance on how to conduct your meetings with your doctors. I encourage patients to find other patients to speak with to help mentor them through the process.
Thank you to The Patient Story for all you’re doing for our community and for patients everywhere, for helping spread that word to our community and to the cancer community as a whole. We need patients to know they’re not alone. There are resources out there.


Inspired by Terri Ann's story?
Share your story, too!
More Lung Cancer Stories
Yovana P., Non-Small Cell, Invasive Mucinous Adenocarcinoma (IMA), Stage 1B
Cancer details: Had no genetic mutations; IMAs comprise between 2-10% of all lung tumors
1st Symptoms: No apparent symptoms
Treatment: Lobectomy of the left lung
Dave B., Non-Small Cell, Neuroendocrine Tumor, Stage 1B
Cancer details: Neuroendocrine tumor
1st Symptoms: 2 bouts of severe pneumonia despite full health
Treatment: Lobectomy (surgery to remove lobe of lung)
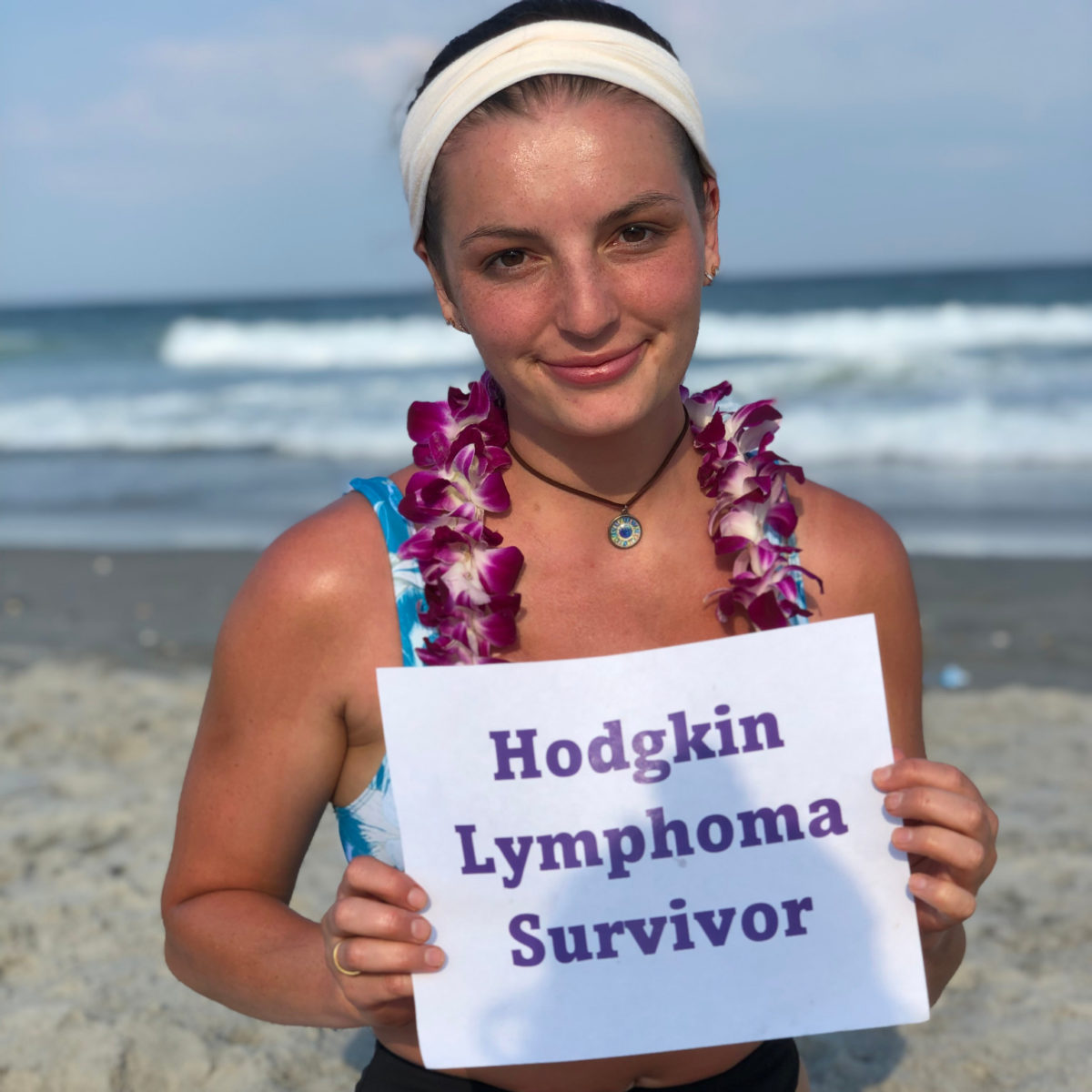
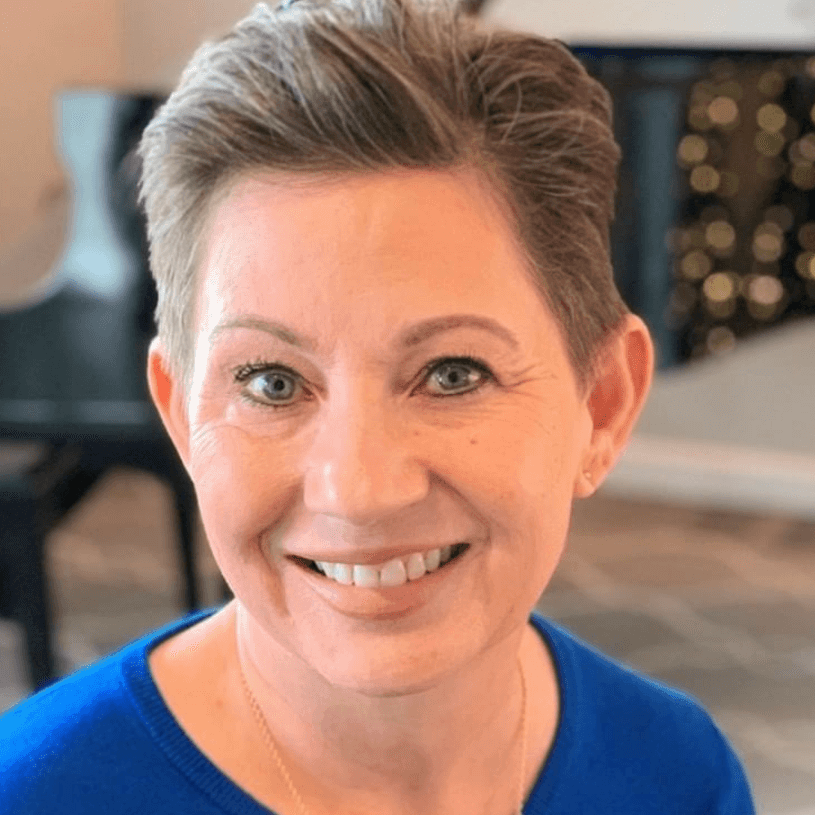
Terri C., Non-Small Cell, KRAS+, Stage 3A
Cancer details: KRAS-positive, 3 recurrences → NED
1st Symptoms: Respiratory problems
Treatment: Chemo (Cisplatin & Alimta), surgery (lobectomy), chemo, microwave ablation, 15 rounds of SBRT radiation (twice)
Heidi N., Non-Small Cell, Stage 3A
Cancer details: Non-small cell lung cancer (NSCLC)
1st Symptoms: None, unrelated chest CT scan revealed lung mass & enlarged mediastinal lymph nodes
Treatment: Chemoradiation
Tara S., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Numbness in face, left arm and leg
Treatment: Targeted radiation, targeted therapy (Alectinib)
Lisa G., Non-Small Cell, ROS1+, Stage 4 (Metastatic)
Cancer Details: ROS1+ tends to be aggressive. It can spread to the brain and to the bones.
1st Symptoms: Persistent cough (months), coughing a little blood, high fever, night sweats
Treatment: Chemo (4 cycles), maintenance chemo (4 cycles)
Stephen H., Non-Small Cell, ALK+, Stage 4 (Metastatic)
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Shortness of breath, jabbing pain while talking, wheezing at night
Treatment: Targeted therapy (alectinib), stereotactic body radiation therapy (SBRT)
Ivy E., Non-Small Cell, EGFR+, Stage 4 (Metastatic)
Cancer details: EFGR-positive
1st Symptoms: Pain & stiffness in neck, pain in elbow
Treatment: Two targeted therapies (afatinib & osimertinib), lobectomy (surgery to remove lobe of lung)
Ashley R., Non-Small Cell, EGFR+ T790M, Stage 4
Diagnosis: Stage IV Non-Small Cell Lung Cancer
1st Symptoms: Tiny nodules in lungs
Treatment: Tagrisso (Osimertinib)
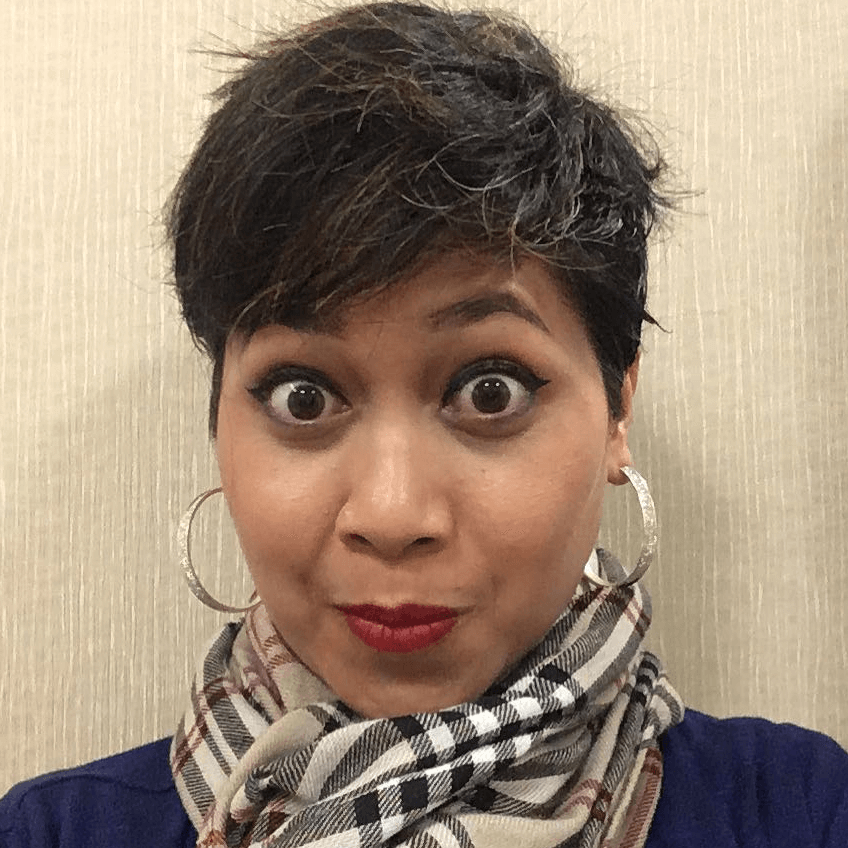
Shyreece P., Non-Small Cell, ALK+, Stage 4
Cancer details: ALK+ occurs in 1 out of 25 non-small cell lung cancer patients
1st Symptoms: Heaviness in arms, wheezing, fatigue
Treatment: IV chemo (carboplatin/pemetrexed/bevacizumab), targeted therapy (crizotinib, alectinib)
Amy G., Non-Small Cell Squamous, MET, Stage 4
1st symptoms: Lump in neck, fatigued
Treatment: Pembrolizumab (Keytruda), SBRT, cryoablation, Crizotinib (Xalkori)
Dan W., Non-Small Cell, ALK+, Stage 4
1st Symptoms: Cold-like symptoms, shortness of breath, chest pains
Treatment: Radiation, targeted therapy (Alectinib)
Tiffany J., Non-Small Cell Adenocarcinoma
1st Symptoms: Pain in right side, breathlessness
Treatment: Clinical trial of Tagrisso and Cyramza
Montessa L., Small Cell Lung Cancer
Cancer details: Small cell lung cancer
1st Symptoms: Chest pain, lingering cough
Treatment: Chemotherapy (Cisplatin switched to carboplatin, etoposide), chest radiation, brain radiation (prophylactic)
...