Chris’s Stage 4 Mucosal Melanoma Story
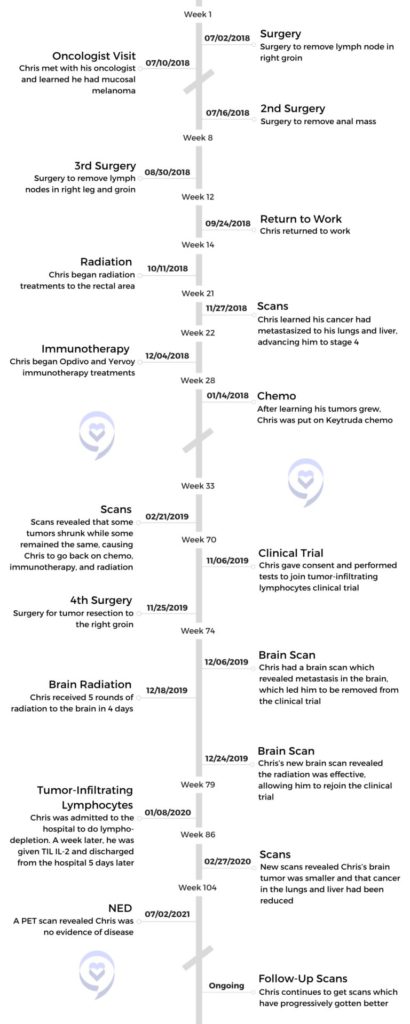
With no pain or abnormal symptoms other than a small zit-sized lump, Chris did not think much of his condition. After a new lump appeared, he decided to get checked. Doctors were also unassuming but recommended he remove the lumps through surgery. Shortly after, Chris was diagnosed with stage 4 mucosal melanoma.
With a low survival rate, Chris found hope in a clinical trial for tumor-infiltrating lymphocytes (TILs) but was removed from the trial due to brain metastasis. With the trial window closing, Chris raced to get radiation treatments done in order to rejoin the trial and was successful, as was the clinical trial.
Chris shares his mucosal melanoma story with us, including why he chose to maintain a positive outlook, the side effects he experienced from cancer treatments, his aspirations of sharing cancer advocacy, and his advice for those on their own cancer journeys.

- Name: Chris W.
- Diagnosis (DX):
- Age at Diagnosis: 41
- Staging:
- Stage 3C
- Advanced to stage 4
- Symptoms:
- Sweaty rectum
- Zit-sized lump in rectum that grew
- Lump that developed in right-groin
- Treatment:
- Surgery
- Chemo
- Radiation
- Immunotherapy
- Opdivo and Yervoy
- Ipi/Nivo
- Tumor-infiltrating lymphocytes (TILs)
I feel like I’ve learned to live a more meaningful life because of the experience. I don’t have the physical or mental energy to want to go do what I used to do. The energy I do have, I want to put towards more positive good and being able to help.
Chris W.
The interviews have been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms & Diagnosis
Tell us about yourself

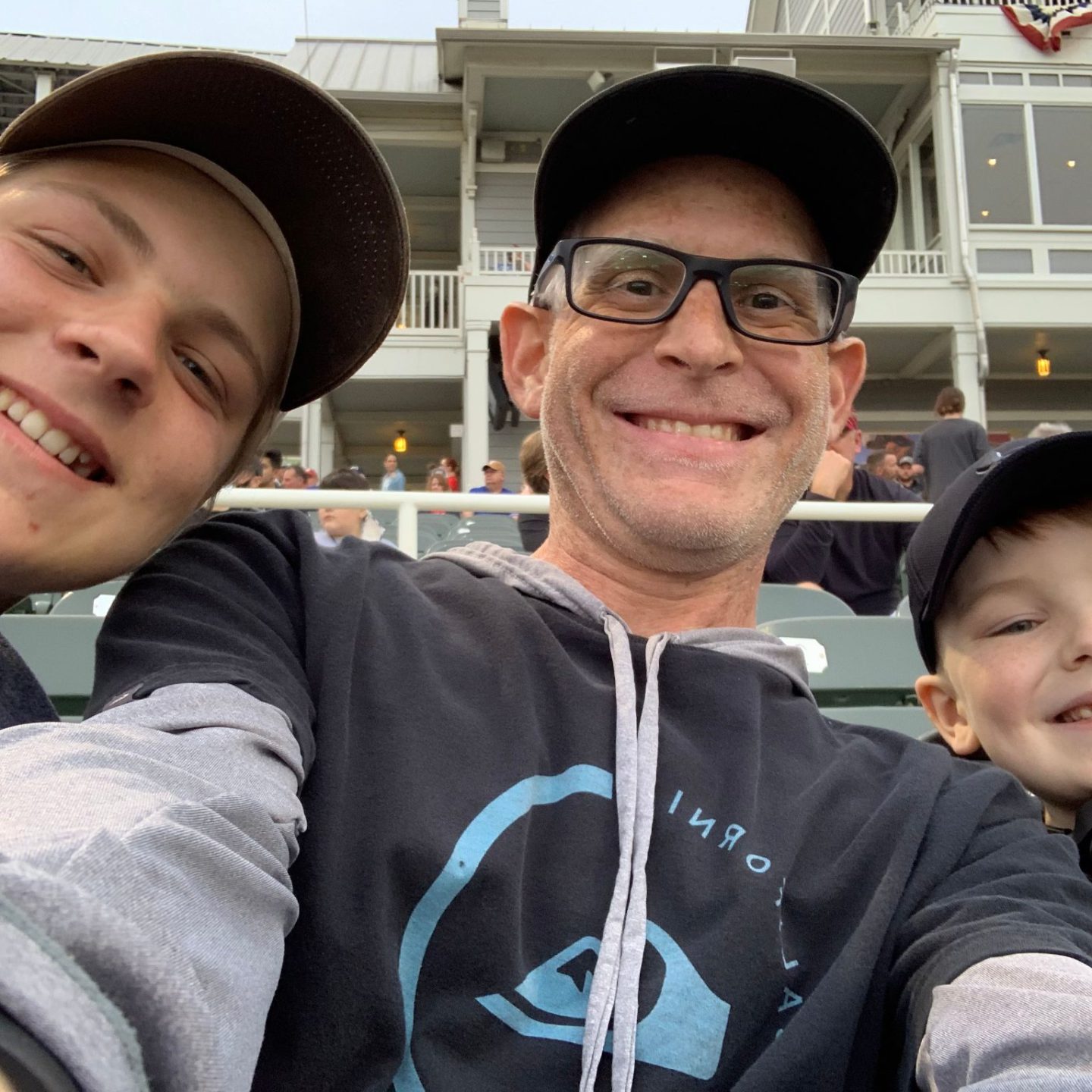
My name is Christopher. I’m 41 years old. I live in Dallas, Texas. I’m originally from Colorado Springs and moved to Southern California when I was younger. I grew up there until right before high school and have lived out in Dallas ever since.
I’m into any action sports like snowboarding and anything with an adrenaline rush. I played baseball growing up as a kid and am a very proud uncle of 8 nieces and nephews.
I’m very excited to be here and share my experience.
What were your first mucosal melanoma symptoms?
At the beginning of 2018, I had a sweaty rectum and I didn’t know what was causing it. There was a very small lump on my rectum. I thought it was a zit or something like that. Over time, it ended up growing to maybe the size of a dime. There was no pain, there was no bleeding. I had heard what hemorrhoids are and I assumed that’s what it was so I didn’t do anything about it.

A few months after that, in May of 2018, I started noticing a lump that grew in my right groin and it grew rather quickly. I went to the doctor to have him look at that. I didn’t associate anything between the 2 lumps, but I had the doctor look at it and he said, “Here’s some antibiotics. Take them for 10 days and come back.”
I came back after nothing happened. He gave me a different antibiotic and it was the same thing. He referred me to a general surgeon to get it looked at and he said he thought the lump in my groin was most likely a femoral hernia but he wasn’t sure. The only way to find out is to get in there and cut it out. He said if it was a hernia, he would fix it and we would go from there.
»MORE: What Does Cancer Feel Like?
Receiving a cancer diagnosis
When I woke up, he said it was not a hernia, it was a lymph node. He was able to get it out with clear margins and send it off to pathology. Since I had that week off, I went to the proctologist and he said [the results] didn’t come in yet, but they should be there by that afternoon or the next day. He said until we find out, we’re going to put things on pause.
I got a call from the surgeon, and he said it was the metastatic form of malignant melanoma. He said don’t look it up and don’t tell your family, but make a call to the oncologist immediately.

I got a call from the surgeon, and he said it was the metastatic form of malignant melanoma. He said don’t look it up and don’t tell your family, but make a call to the oncologist immediately and gave me the number. Since it was late on a Friday afternoon, I went ahead and made the call and got an appointment for the following Tuesday on the books.
I did tell my family. I wanted to make sure I had support. I didn’t want to do any of it alone so they all came with me. We went to my first appointment and the oncologist said that this is very specialized. There are numerous types of melanoma, but since it is so specific, I need a second opinion. They recommended I go down to MD Anderson so I started making the calls for that and that’s what jump-started everything.
»MORE: How To Tell Your Family and Friends You Have Cancer
Did you have any additional symptoms?
No, just the lump on my rectum and the one on my groin. The one on my groin ended up growing to the size of a golf ball. That was it. No fevers, no random sicknesses I couldn’t explain, or any aches or pains anywhere. It was just those lumps.



Dealing With A Diagnosis
Did you know much about melanoma pre-diagnosis?
Absolutely not. I was so in shock that you could get melanoma in places other than your skin. I’ve heard of cutaneous or skin cancer and anytime I’ve ever heard the word melanoma, that’s the association. The fact that you could grow melanoma where the sun doesn’t shine just blew me away. I was just shocked.
How did you react to your cancer diagnosis?
I had one moment where I bawled and cried in the shower one day. When I got out of it, I dried myself off and it was significant. I’m like, all right, starting fresh. I was thinking I’m just going to be overly optimistic and positive. That’s how I was going to approach everything and handle it all. I didn’t want to feel doom and gloom and have everybody around me be the same. I figured if I set the tone for everything, then that would jump-start between my family, my friends, and the doctors.
I was thinking I’m just going to be overly optimistic and positive. That’s how I was going to approach everything and handle it all. I didn’t want to feel doom and gloom and have everybody around me be the same.

I tell people that I had to come outside of my own self in a sense from whatever it was I wanted to be or do. I had to be so focused on gaining control because I felt so out of control. I don’t want to say hopeless or helpless, but you’re at a loss because this is so unique and different. They’re saying that this most likely could kill you. Everybody’s got an expiration date, you just don’t actually know what it is. Getting told something like that is having them take the sand in the hourglass, flipping it over, and going, now the clock’s ticking. That’s how it felt.
What type of melanoma were you diagnosed with?
Being that I live up in Dallas and I got my initial diagnosis here, when I got down to the specialist, I had a second surgery. Once we knew what everything was, they removed the lump on my rectum and did a PET scan. When I got down to MD Anderson, that’s when he told me specifically that it’s mucosal melanoma and that it forms in the mucous membrane.

Anywhere you have, mucosa, whether it’s the vagina, rectum, ear, nose, and throat, that’s where it is, but it’s extremely rare. Mucosal melanoma makes up 1% of all melanoma and the survival rate is like 5 years, which is 14%. Since it forms in the mucous membranes and it’s always disguised either as a lump, a polyp, or a hemorrhoid it’s usually at stage 3 or 4 by the time it is diagnosed. I had local metastasis that went from my rectum to my lymph node so I was stage 3C as a diagnosis and eventually became stage 4 once it ended up going to all my different organs and everything.
How long did it take for your staging to advance?

The 3C diagnosis was in July 2018. I had those 2 surgeries while I did a third surgery where they pull out all the lymph nodes from both of my groins and the remaining cancer that was still in my rectum. After I recovered from that, I did radiation and I got a scan at the end of November [that showed] it went from 3C to stage 4. Right after I finished my radiation to my rectum and I healed from all that, I went to go do another PET scan for staging and it didn’t come back to my rectum, but it went everywhere else.
How did you process having cancer?
You could feel the vibe, having to fill out my will and do all that end-of-life stuff, it was intense. It was extremely emotional. I would have done anything in the world to stay alive.

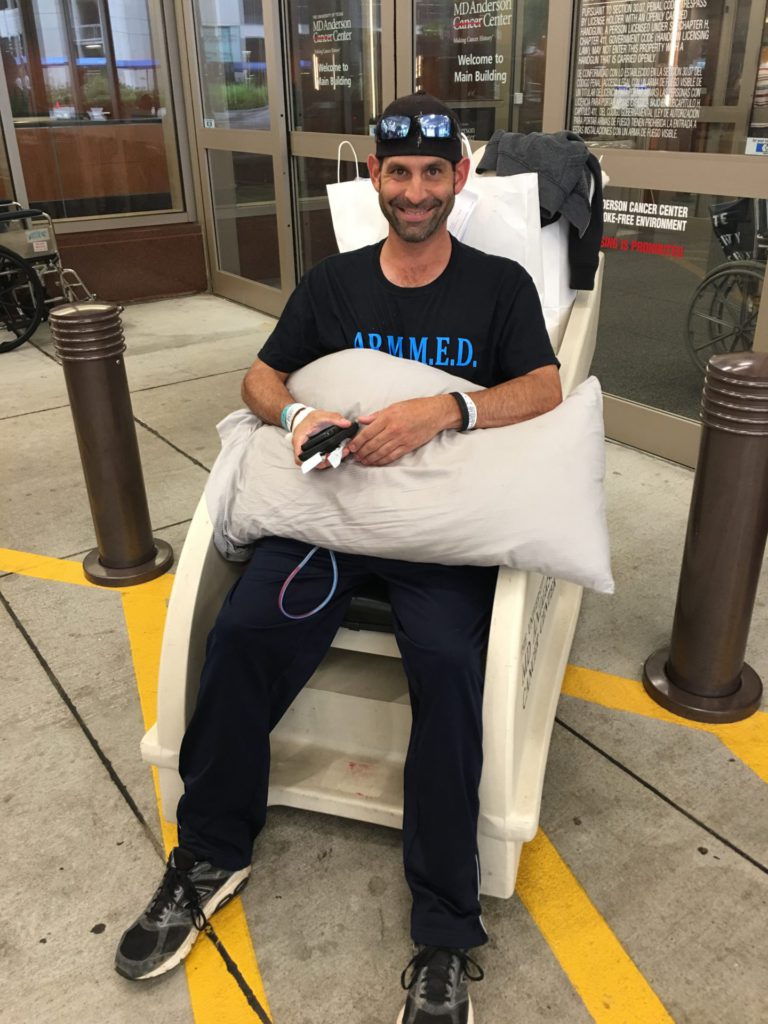
I was clinically declining. It was a very sad situation in a sense, because the entire time throughout my treatment, I always had this optimistic positivity. Even though I was walking around with stage 4 cancer, you wouldn’t tell by looking at me because it riddles you from the inside when you do all the different types of treatments like immunotherapy. You don’t look sick like you do with chemotherapy or other types of treatments. I never really looked or felt until the very end of it. I had metastasized and was on a lot of narcotics actually, for all my cancer pain so I was kind of numbed to a lot of things.
I often tell people to imagine how high they can fly when they feel like Superman. That masked a lot of what was going on. But emotionally, I was torn up inside. I was so optimistic and so positive until I finally did start looking like I was clinically declining. You could feel the vibe, having to fill out my will and do all that end-of-life stuff, it was intense. It was extremely emotional. I would have done anything in the world to stay alive. If you said I need to drink a gallon of gasoline, I was going to do it. Whatever needed to be done, I was going to do it. I just looked at it like, I have no choice. If I’m going out, I’m going out trying.
When I even had colitis for 3.5 months due to all the immunotherapy treatment, that was the only time that I ever actually looked sick, because I’d lost so much weight. That’s the whole thing with this cancer. You’re walking around stage 4, terminal deal, but you don’t look like it. It’s just intense.
Treatment


What other cancer treatments were you on?
They said their number 1 thing is always going to be immunotherapy. If there’s no cancer that showed up on my PET then I was going to do follow-up treatments. Because the cells are so small, they’re trying to travel so it’s a maintenance thing. It was like a year or so, they said, of doing immunotherapy treatments and a single dose sometimes mixed with chemo or something. That was my go-to as soon as it metastasized. We skipped that and went straight to combination immunotherapy of Opdivo and Yervoy.
»MORE: Types of Cancer Treatments
What side effects did you have from cancer treatments?
I ended up having 3 surgeries to the same spot where that original lymph node in the groin was and then the lymph node dissection surgery. That exact same lymph node grew back in the same spot. I had 3 surgeries on the same spot on my leg, so I have nerve damage from my knee to my hip. My hair is all white and I used to have dark brown hair. The treatments completely wiped everything out and it came back including my eyelashes. I still have chronic pain and chronic fatigue. I deal with the immunotherapy treatments through my thyroid so I have hypothyroidism. I have to take medication for that for the rest of my life. I ended up having to do sperm banking right before my first radiation on my rectum because that was going to kill my chances of ever being able to have children.



»MORE: Fertility After Cancer Diagnosis
The clinical trial and all my treatments completely wiped out all my melanocytes, so as my pigment is trying to come back I’m very susceptible to sunburns. I have to definitely wear UPF clothing, hats, sunglasses, long sleeves, and pants year round and a lot more sunscreen than I used to. Also, the immunotherapy treatments, caused uveitis right before I went into my clinical trial and I developed cataracts. I’d never even been to an optometrist or an eye doctor. I had perfect vision. I ended up having cataract surgery and now I need prescription glasses.
Describe your clinical trial
Imagine that your cells and the TILs are Pac-Man and you’ve got billions and billions of Pac-Man. They go throughout your body and they eat up all the cancer like all the dots and cherries until they’re gone. Once they do, it’s gone forever.

The clinical trial is called TILs and it stands for tumor-infiltrating lymphocytes. It’s not where you just go in and get an infusion into medication. It’s a process. After you’re signing consents there are a series of tests to make sure you’re healthy enough to go through it. EKGs, blood labs, and things like that. You have to have more than 1 tumor of a minimum size so they can extract 1 and then monitor the other. What they do is they pull that tumor out and they send it out to a lab and then extract those cells and grow them into the billions.
It’s a 22-day process prepping you to enter the hospital. You enter the hospital and get a PICC line in and you have to do 1 week of chemo that is a lymphodepletion. It brings your cell count down to 0 so your body’s like a blank slate. Then they take the TIL, they manufacture it into the billions and then they give those back to you intravenously. They follow that up with up to 6 doses of IL-2 interleukin. That jumpstarts the cells to get them to go.
Imagine that your cells and the TILs are Pac-Man and you’ve got billions and billions of Pac-Man. They go throughout your body and they eat up all the cancer like all the dots and cherries until they’re gone. Once they do, it’s gone forever. It’s not in remission, it’s not asleep, it’s not waiting to wake up. It’s not there. If it was to pop back up, you still have all those billions of cells in your body of your TIL and they’ll be there forever and just eat it up.
From start to finish, you’re looking at anywhere from a 3 to 4-week process, from the time you get your first surgery until you enter the hospital, then you do your week of chemo depletion. The hospital stay for me was about 12 days which is a minimum amount. It’s like taking the dial, turning it all the way down, and then turning it back up. All your levels and blood counts and everything got to come back for them to release you. While you’re doing that, you get the 6 doses of IL-2 after your TIL. That, I’d say, would be the last actual treatment that I ever did. I did the surgery and the chemo depletion, and they gave me my TIL and then IL-2 to follow.
How did you join this clinical trial?
I signed all my consents in November 2019, and I was actually supposed to enter the hospital in December 2019. Right before I entered the hospital, they found brain metastasis and it kicked me out of the trial. They said I might need to consider calling hospice and settling my affairs because the only way to get back in was to reduce or stabilize my brain metastasis. In order to do that, we needed radiation treatment, but the trial was closing. It was phase 2 and cohort 4. They had to wrap this up. They started the trial around 2015 or so. I was on a very strict timeline to get that fixed. The very last day for me to scan or re-scan to show that my brain metastasis was good was Christmas Eve.
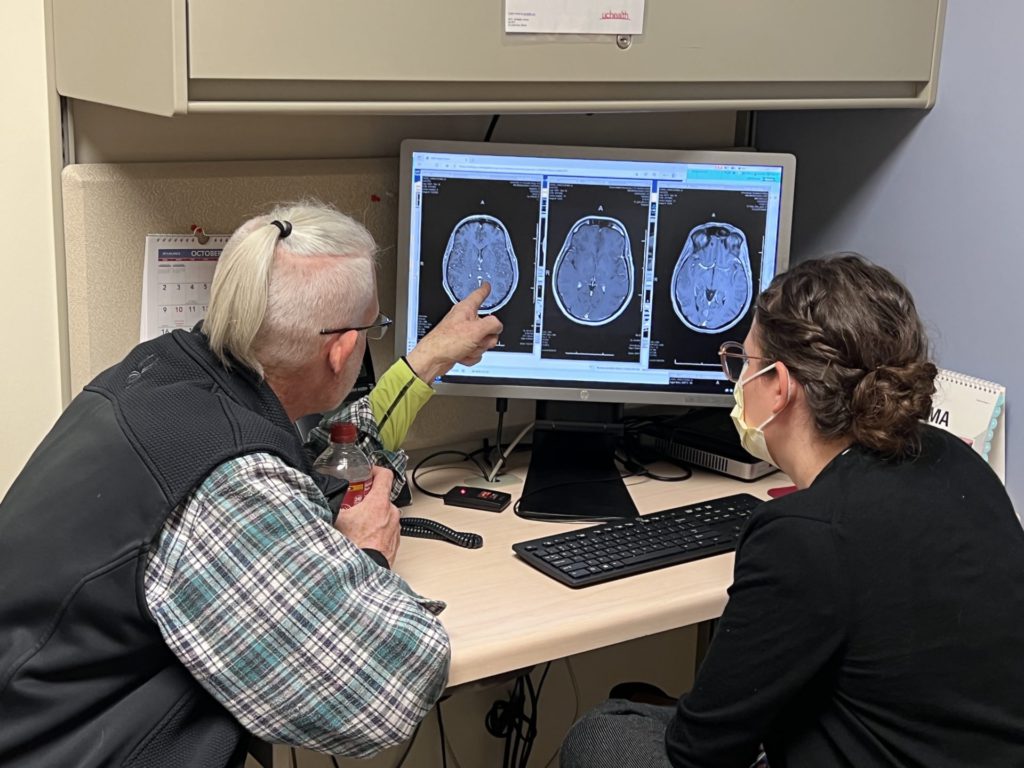
I ended up needing 5 doses of radiation. I went to the radiologist and saw them, but they couldn’t make the mask until I had the insurance approval. Once I got the insurance approval, I finally was able to make the mask but I didn’t have time to do 5 days of radiation. So I did it in 4 days. On the fourth day, they gave me a double dose. That was on December 23rd. Then I went and scanned on Christmas Eve and I had to wait and fill out my will and end-of-life things.
I flew out to Colorado on January 2nd and saw the doctor on the 3rd. She said everything was all good. Well, not all good. It had pseudo-progression. It goes up before it comes down, but it was good enough to let me back in the trial. I entered the hospital on January 8th, 2020 started doing my chemo depletion on January 15th, 2020. That’s when they gave me my TIL and then I did my 6 doses of IL-2 and I was released from the hospital on January 20th, 2020.
What were the results of your clinical trial?

In January 2021, a year to the date, they told me that I was able to get back into the trial. My scans showed that I did have a complete metabolic response. Nothing lights up on a PET anymore, everything is completely gone.
The way the trial works was, the day they gave you your TIL when you’re in the hospital, they call that day 0 or day 1. From then on, it’s 6 weeks you scan, and then 6 weeks after that, you scan. After that, you scan every 3 months. I started showing that everything was working on my scans. It wasn’t drastic marks, but it was either stable or in reduction, nothing new.
Within less than a year, I want to say about 9 months, they started showing signs that I had a complete metabolic response. We followed up on my next set of scans with additional PET scans, along with my CTS and MRIs. In January 2021, a year to the date, they told me that I was able to get back into the trial. My scans showed that I did have a complete metabolic response. Nothing lights up on a PET anymore, everything is completely gone. There are a couple of spots, but they’re necrotic and calcified so they use those as the markers when I still go and get scanned every 3 months. That’s all I do now every 3 months, I go in and I get full body CTS, abdomen, pelvis, and also a separate one for my neck, and I do brain MRIs.
Life With Cancer

Believing in your healing
I just didn’t know how I was going to get there. I always saw myself like, you’re going to make it. You can’t really describe how you’re going to do it until it’s done. In my mind, I always thought I was going to make it. I never doubted at all that I wasn’t. As bad as everything got and hurt, I still was just like, if I was going out, I was going to go out with a legacy that people wanted to talk about. Other family members, doctors, and a lot of people told me they didn’t think I was going to make it, but I said, if I set the tone then everybody else will follow.
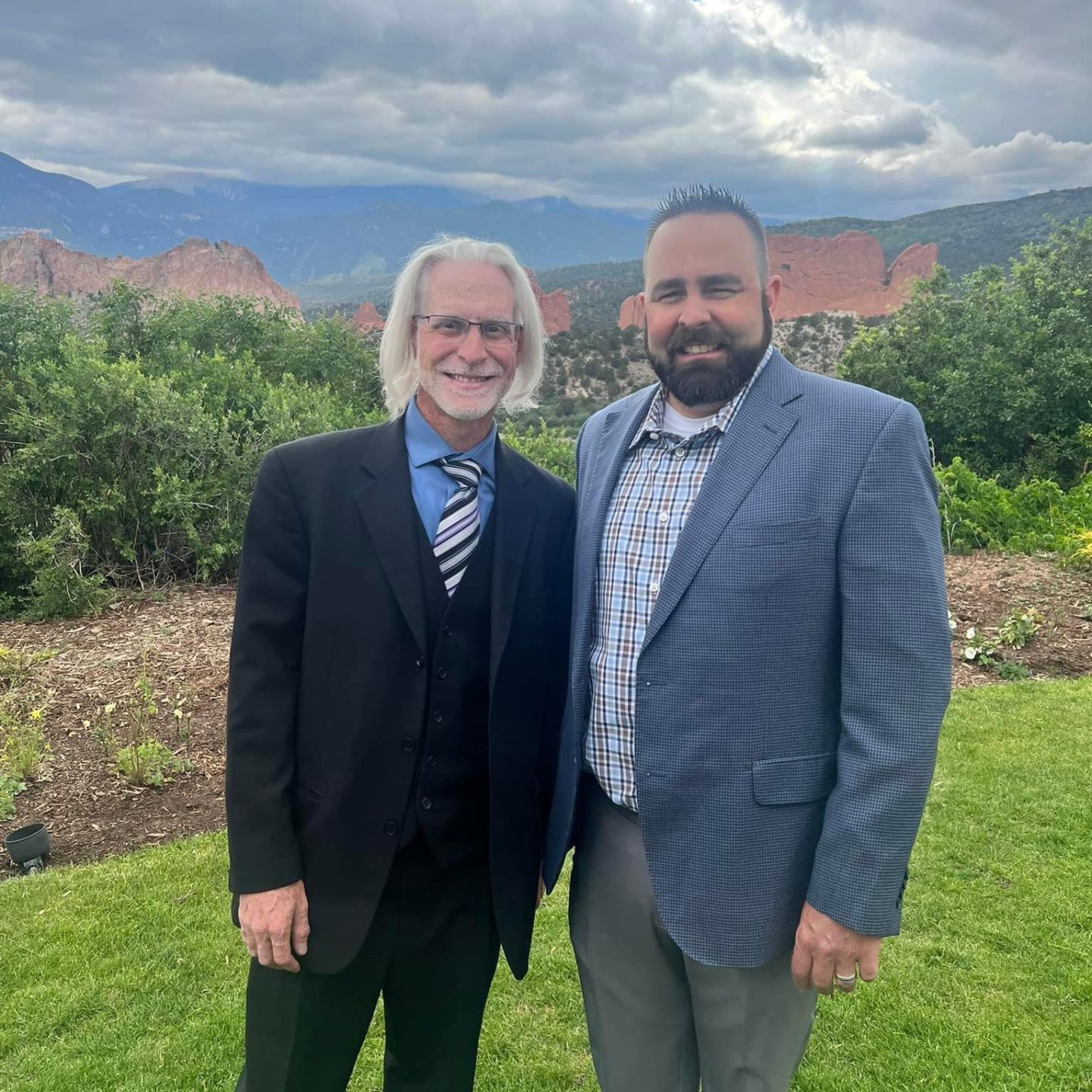
Describe your medical care team
I’d never been to an oncologist prior to this for any reason. I barely even knew what it meant. I had 3 different organizations I worked with and all of them were very receptive because I came in like this bubbly, positive, we’re going to beat this attitude and tone. Everybody was very receptive and welcoming.

I did have some doctors that thought they were so smart, but their people skills were not the same because they were in labs their whole life. I had a fellow that came and gave me the news that [the cancer] had metastasized. I had no clue, and he came in and told me like I already knew. That always kind of upset me.
Advocating for yourself as a patient
I was very persistent on what I wanted and when I want it and had a sense of urgency. I used to be a home builder, and that’s what I was doing at the time when I was going through all of this. It was always my mindset if they’re scheduling anything, it needs to happen now, not later. I had a definite sense of urgency. If there was time in between, it seemed like wasted time. I was very persistent about always staying on top of that. Usually, everybody was willing to work with me on that.



I was very well received in terms of getting my different oncologists to work with each other. They would prescribe my treatments down at MD Anderson, but if it was any chemotherapy or immunotherapy, I did that in Dallas. All my radiations and surgeries I would do down there. They were like, you’re young, you can take it in terms of all the treatments. I was like, yeah, let’s not wait till tomorrow. We can do it today.
I had a definite sense of urgency. If there was time in between, it seemed like wasted time. I was very persistent about always staying on top of that.
»MORE: How To Be A Cancer Patient Advocate
Dealing with pain as a result of cancer

Most of the pains I have now, for the most part, they’re upper body, chest, shoulders, and neck. I was put on what they call a comfort pack, which consisted of a fentanyl patch, hydrocodone, and Dilaudid. When I was actually going through everything, I was up to a 75-milligram patch and then 240 hydrocodone once a month, which is like 8 a day, plus Dilaudid for breakthrough pain. After I had a complete metabolic response, I had weaned off the fentanyl patch and I never really took much of the Dilaudid because they just make you sleep. I reduced the amount of hydrocodone I took. I don’t have to take them all the time or every day, but if I need to, I still have some hydrocodone to take.
Is there a cause for mucosal melanoma?
Being that it is so rare and only makes up 1% of all melanoma, there are maybe 700 or so people a year in the US that get diagnosed with this, they don’t know what causes it. There’s no standard 1 treatment that works for all.

I did do the genetic testing and everything from the pathology, and I had a CDK4 amplification and an MDM2 mutation. It was like, all right, we’ll start here in terms of targeted therapy with the immunotherapies. The CDK4 is the same amplification that a lot of breast cancer patients have. Their initial thought was doing Keytruda, plus a chemo but it was always going to be in a combination of something because there was no one thing. It was, we’re going to try this and see how well that works. Then we move on to this. It felt like whack-a-mole.
Returning to work after cancer
I told myself I’m not going to make all my decisions in life based on money. I was working just to work, I wasn’t really living life.
I was a new home construction manager prior to now. When I was going through all my treatment, I was able to go in and out of work on short-term disability when I needed to.


The thing with that career is there are long days, you’re walking houses, you’re in the truck, out the truck, the cold, the heat, and everything. When I got out of the hospital in January 2020, I had to go return to work by May 1st of that year. I was going to have to cover my insurance. It just didn’t make financial sense to cover my insurance because I have to maintain insurance. I was still on all those pain meds until I started reducing all that. It gave me a certain kind of energy. Once I started coming off of that and weaning myself down, I didn’t have that same energy.
I would go every day, but when I got home, if I didn’t eat and shower, I wouldn’t. I was so exhausted that I was just done. Come the weekends, I was still so beat up that I just didn’t want to go anywhere or do anything. Over time, I came to resent having to go back to work. Maybe it was what I was doing, because initially when I first got diagnosed, I was so busy with work that I didn’t take the time to go to the doctor and get myself checked. About a year ago, I departed from the job I was working at. I told myself I’m not going to make all my decisions in life based on money. I was working just to work, I wasn’t really living life. I was just working to pay the bills and rinse and repeat.
Reflections
I feel like I’ve learned to live a more meaningful life because of the experience. I don’t have the physical or mental energy to want to go do what I used to do. The energy I do have, I want to put towards more positive good and being able to help.

Finding new purpose in survivorship
I was starting to tell my story more often and talk about everything and I could see the kind of reception I was getting, and it’s made me feel so good.

I refused to believe that I went through everything to not have it be of value. Not necessarily monetary value, but to the other people that want to have an example of, you got this too. What did you do? How did you come to the other side? I still don’t necessarily know how I’m going to do it, but I’d love to be an inspirational speaker. I want to be able to travel around and tell people about my story and go to conferences, and symposiums, work with foundations, clinical trial folks, survivorship, immuno-oncology, ASCO, SITC, and AACR. It’s just more meaningful.
Long story short, I feel like I’ve learned to live a more meaningful life because of the experience. I don’t have the physical or mental energy to want to go do what I used to do. The energy I do have, I want to put towards more positive good and being able to help.
What advice do you have for someone on a cancer journey?
I always looked at it like I said, I was setting the tone and the positivity thing because I’m a big believer in, your mental well-being is connected to your physical well-being. They both got to be in harmony. If you’re in a place or position in your life and it’s causing you anguish and stress, it’s just not worth it.
When it comes to cancer, it’s the whole sense of urgency and self-advocacy. You got to remember, you’re the ones that are paying the doctor. You’re the ones paying the oncologist. They work for you. You don’t just sit there and listen to them. I see the gaslighting, I see the ego, it’s all out there. Take control because it’s the patient to the patient. It’s not, the doctor says this and that’s the rule. Most of the time it’s the patients right now that are educating the doctors on this specific stuff. I meet with people weekly on Zoom calls and there are almost 20 people on a call. That’s probably more than any doctor has ever had in a room. Have a sense of urgency. If you’re not happy with what you’re doing, stop doing that.
The importance of getting checked by your doctor when something is off

Just assuming it’s something when you don’t know for a fact, it can kill you. I tell people, have a sense of urgency, take the time, and make it a priority.
From the time I was diagnosed until the time we went through the clinical trial was 18 months. Within that 18 months, I had radiation to my rectum, my lungs, my kidneys, and eventually my brain. I had 3 major surgeries and then a fourth. Once I had my clinical trial, I did 2 different types of chemo and immunotherapy combo 6 times, and immunotherapy single twice. I was so intent on having something in my system that after the sixth dose of Ipi/Nivo, I had full-blown colitis and I probably had it going into that dose, but I lied my way into it. I did not mention my symptoms when they first popped up for the colitis, which was a reoccurring theme I found myself in.
But if anything is ever off or wrong with your body, go get it checked, period. It doesn’t matter where it’s at or what’s going on. Just assuming it’s something when you don’t know for a fact, it can kill you. I tell people, have a sense of urgency, take the time, and make it a priority. I didn’t make it a priority when I was first diagnosed, or prior to that. That’s why it was diagnosed at 3C because I didn’t go. Anything that’s ever wrong, always go get checked.

Another thing is, it’s okay to talk about the emotional stuff. I just started doing that over the last couple of years. It was so rare, that people had more questions than I had answers for.
I recommend anybody and everybody out there believe in yourself because you’re the one setting the tone. Definitely, if anything’s ever off, go get checked. Who cares about the consequences, take off work, do what you got to do, but definitely say something. Do something.
More Melanoma Stories
Ellis E., Melanoma, Stage 3A
Symptom: Changing mole on arm
Treatments: Lymph node resection, immunotherapy, targeted therapy (BRAF inhibitor)
...
Rich B., Melanoma, Stage 3B
Symptom: Appearance of suspicious dark spots
Treatment: Immunotherapy
...
Jenn S., Melanoma, Recurrent (Stage 0 & Stage 3B)
Symptom: Appearance of asymmetrical, multi-colored, large mole on the shoulder
Treatments: Surgery, skin checks
...
Treatments: Surgery, chemotherapy, radiation, immunotherapy, tumor-infiltrating lymphocytes (TILs)...
Caitlyn M., Melanoma, Stage 4
Symptoms: Severe pain on the side pain that worsened over time, pelvic pain and a feeling of pressure resembling labor, swollen lymph node on the cheek
Treatments: Multiple surgeries to remove tumors, targeted therapy (Opdualag/nivolumab and relatlimab-rmbw)
...





2 replies on “Chris’s Stage 4 Mucosal Melanoma Story”
My son is dealing with this as now. We r all just devastated. I am happy that u r doing well. Many blessings for continue good health
Such a very remarkable story. Thank you for sharing your journey through the treatment gauntlet. Sadly I fear too many people don’t heed your advice to be your own advocate and encourage the medical personnel and insurance/reimbursement entities to hustle up, not delay and start treatments sooner than later to improve survival and response rates. Your courage and resolution in the face of this very dangerous and mortal scenario are amazing and inspiring!