Harriet’s Diffuse Large B-Cell Lymphoma Story
As an avid exerciser and ballroom dancer, Harriet knew something was wrong when she had difficulty after 2 minutes of walking. This led her to the ER, where she assumed she’d receive fluids because she was dehydrated. Doctors insisted she have a CAT scan of her stomach before sending her off. It was then that they discovered she had a large mass sitting on 3 organs.
Harriet was admitted to the hospital that same day and received biopsies and tests which revealed a non-Hodgkin’s large B-cell lymphoma diagnosis. She began her care at Columbia University Medical Center and started EPOCH chemo to combat, what her doctor called, a very treatable cancer.
Today, Harriet is cancer-free and the author of Living Well Despite Adversity. She shares her journey with and discusses how she coped with fear and anxiety through visualizations, positive psychology, being outdoors, and creating coping cards, as well as her advice to others on their own cancer journeys.

- Name: Harriet C.
- Diagnosis (DX):
- Non-Hodgkin’s Lymphoma
- Diffuse Large B-Cell
- Non-Hodgkin’s Lymphoma
- Symptoms
- Weight Loss
- Difficulty walking
- Stomach pain
- Feeling unwell
- Treatment:
After cancer treatment, you’re on a forever healing journey.
Harriet C.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms & Diagnosis
Tell us about yourself
My name is Harriet and I’m from Long Island, New York. In terms of what I am beyond a cancer diagnosis – because we’re a lot bigger than our diagnosis and our illness. I actually kept that in mind during my treatment. I’m a clinical social worker and I have a private practice, ironically working with people, going through grief and loss and all types of critical life situations and transitions.
Before this, I was also a social worker in the school system, working with the little people, the 4-year-olds. For the last 15 years or so, I’ve been working privately, so I have clients.
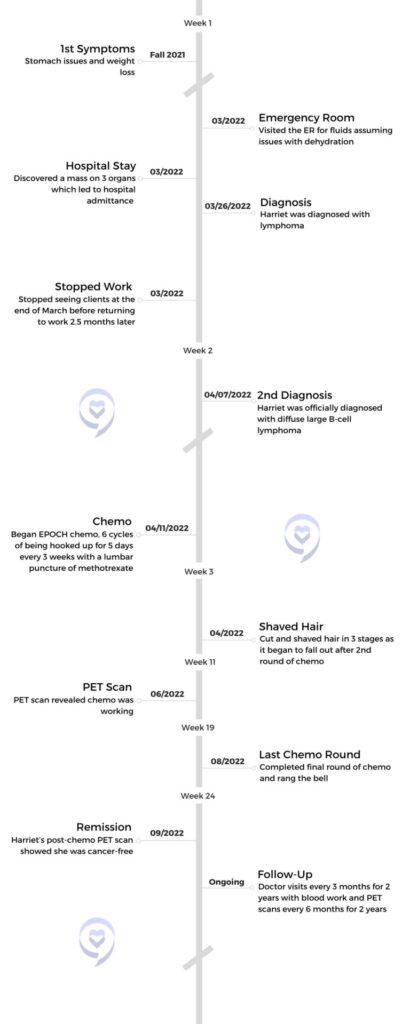
I do speaking. I wrote a book a few years ago, Living Well Despite Adversity. I’ve always been in this field with this theme in life. Fast forward to March of 2022, I got my diagnosis of non-Hodgkin’s large B-cell lymphoma.

What were your initial symptoms?
A few months before I got diagnosed, I was having stomach issues. I think we all have weak links in our bodies. The stomach has always been my weak link. 20 years ago, I had ulcers and I’ve had reflux. I’ve always had irritable bowel and stuff in my gut, but I’ve always managed it and I don’t do medicine. I was seeing a great integrative doctor, but it would flare up here and there.
In the fall of ’21, I went for an endoscopy. Everything seemed fine, typical. A little bit of gastritis. I also tested positive for H. pylori. Instead of going on the rigorous antibiotic routine, which is like 12 pills a day for 10 days, my integrative doctor has known me for 20 years and said, “You’ll never tolerate that. I’m going to create a cocktail for you of natural things.” After a month of taking them, I went back for a repeat of the test for H. pylori and it came back negative, so that was wonderful.
I was still not feeling great, although I went away on vacation and was pushing myself through, I still had energy. I was taking my ballroom dancing classes. I was seeing clients. I was doing everything, but still felt I was losing some weight and I couldn’t afford to lose weight. I’m a very small, thin person. I don’t like to say this, but most people struggle the other way. I try always to gain some weight. I was losing some weight, 2 or 3 pounds. I wasn’t eating a lot, I didn’t have much of an appetite, and my husband would say, “Maybe you should go to the emergency room.” I didn’t want to go to the emergency room.
Going to the emergency room
One day we were at Long Beach on the boardwalk walking. I’m an avid walker. We hike, we walk, I’ve been an avid exerciser for years. I couldn’t walk. I had to sit down after 2 minutes. I said, “This isn’t me.” Three days before that, I was doing my ballroom dancing, learning the tango. I have a video I showed the doctor. I said, “Three days ago I was doing a tango. What is this?”

She said, “You have a large mass growing inside you sitting on 3 organs.”
I was at Long Beach, couldn’t walk, came home, and said, “I probably am dehydrated. Maybe I should go to the hospital for some fluids.” We went to the hospital in the city because I have a connection there. We went to Lenox Hill and the doctor said, “We need to run a CAT scan on your stomach to see if these are the symptoms you had a year ago.”
It was fine. She said, “You don’t have to drink the whole drink. Just do a little to placate me.” I did the CAT scan and I’m not one to do extra stuff medically, but I did it and it was taking a very long time for results. I thought, uh oh, something is not right. Instead of an hour, it was like 3 hours sitting there pacing and going to the bathroom, because when I’m nervous, I have to keep going.
She finally came out and it was a different [doctor] than the original one who had changed shifts. I saw her face right away. She said, “I don’t even know you. The other doctor at least knew you for 15 minutes. I’m a stranger and I’m giving you very bad news.” I was like, oh my God. She said, “You have a large mass growing inside you sitting on 3 organs.” I was stone-faced. My husband broke down crying like a baby. Even now, I get the chills. I didn’t have any words. She said, “We’re going to admit you. We have to run more tests. This is an initial diagnostic and we have to do biopsies.”
What was your reaction to hearing you have a mass?
I thought to myself at that point, if it’s truly sitting on 3 organs, it’s really big, really fast growing, and I only have a few months to live, I told my husband at 11:00 at night, “You’re going to put me in hospice.” This is the worst news you could possibly get from a complete stranger. I came in for a hydration and this is what it is. That’s how I found out, and then they brought me up to the room.
It was midnight, completely dark. He had to leave. Spouses weren’t allowed to stay. There was a roommate and I just laid there in bed and my whole life ran through my brain. I said, okay if this is God’s will, I really don’t want to die yet. I also don’t want to suffer, but I’ve had a good life and I went through all the stuff in my life and I said, I can’t be bitter because I’ve had a lot of great stuff, but I would like longer. I don’t really know how I got through the next few days until I actually got the real diagnosis 6 days later.
Receiving an official cancer diagnosis
They did biopsies. I apparently was yellow. They said, “Didn’t you see that you were yellow?” I didn’t. I had 2 severely blocked liver bile ducts. So 2 days later they went in, they biopsied, and they put in 2 stents to open it up. I had no clue. That was Sunday. I got the final diagnosis on Saturday. I have no clue how I went through 6 days like that.
The doctor called me up and said, “I have the best news possible within the cancer world. What you have is called non-Hodgkin’s lymphoma, which is very, very treatable. So if you had to have cancer, this is one of the better ones.” That week, my verdict was changed. I went from thinking that this is it, sitting on 3 large organs, 1 of which is the pancreas. My verdict was changed and I felt better about it.
Shortly thereafter, I started treatment. I took the recommendation of this doctor who actually is a family member, who was a head of gastro at Lenox Hill for many, many years. He did some quick research and said, “I’m finding you the top person who specializes in this,” and he sent me to this woman [at Columbia]. I did not seek second and third opinions. I went to her.
What you have is called non-Hodgkin’s lymphoma, which is very, very treatable. So if you had to have cancer, this is one of the better ones.
Treatment
What cancer treatments were you on?

I was doing chemo. It’s called EPOCH treatment. I had 6 rounds every 3 weeks. It was intense because it was 5 days of chemo. I did the first round in the hospital. After that, my doctor encouraged me to do outpatient. She said, “You’re a good candidate. You’re basically healthy. You’re in good shape. I want you to try it,” because I was scared to do it at home. She said, “If it doesn’t work out, you’ll do the next 4 in hospital. You have nothing to lose.” So I did.
They hooked me up to a fanny pack, and for 5 days, I’m hooked up to this chemo drip. In the hospital, it was to the big pole. But once I was home, it was a little fanny pack that I carried around 24/7 for 5 days. Then I would go in 2 of the days that week to change the bag, to get the next one, to get hydration, and to check my blood. Then Friday, at the end of the week, I went in to get unhooked. I actually was hooked up Monday, went in Wednesday, and went back Friday to get unhooked. That was week 1, and then week 2 and 3 I was off, and then we started again. It was every 3 weeks. That was my cycle.
For every one of those intervals, I had a lumbar puncture, which is not very pleasant, and they injected methotrexate. I think that was more preventative. They wanted it in my central nervous system, my brain. That part was fine. It was like 5 minutes of injecting that once they put the needle in the spine, but that was every cycle.
Did you experience side effects from cancer treatment?

I said to the doctor, “This may sound nutty, in the scheme of things, but I have this terrible fear of nausea and vomiting.” You see all these movies with cancer patients and they are sitting by the toilet. She said, “I’m going to tell you something. Number one, this isn’t one of those that will cause a lot of that. However, you’re going to take the anti-nausea medicine always ahead of time, prophylactically. You’re never going to wait to start to feel it. You’re going to be ahead of the game, even if it means you take it every day or 3 times a day. Whatever it is, you’re not going to wait.”
I took her advice, and I know it sounds funny. I never threw up once. I mean, one time I had a little tiny episode, but that was a big fear. I laughed when I was telling her. She said, “It’s a lot of people’s fears. You don’t have to laugh. It’s okay.”
My other big fear was that I am so sensitive and allergic, and I don’t do well with a lot of antibiotics. I have a very sensitive gut. I had to be on a lot of antifungal, antiviral, antibacterial, and miracle of miracles – and I have a lot of miracles in my story – my stomach was fine with all the antibiotics I had to take every day, including very high doses of steroids. Steroids, I wasn’t concerned with, but the antibiotics I was. It was all fine.
The side effects I had were fatigue, weakness, loss of appetite, and mouth sores. Every time I came to see her for every interval, she’d say, “Are you having joint pain? Are you having neuropathy?” I didn’t, but I did have mouth sores that lasted about a week each cycle.
»MORE: Cancer Treatment Side Effects
How did you cope with mouth sores?
I drank some smoothies and sucked on ice. I really didn’t have much of an appetite. I can remember eating watermelon. That was the most soothing thing in the world for me was watermelon. I was being treated in the summer, so watermelon was in season.
Mental Health
Using positive psychology to overcome fear

My biggest fear and my biggest side effect which was bad news, was weight loss. Like I said, I couldn’t afford to lose more weight. I went down to 80 pounds. I lost over 20 pounds. That was not even including the weight loss from before. All I could think was that my body was not going to survive it. It’s going to cave in and I’m going to die just from the treatment.
By round 4, I was down so low and that’s when my anxiety got really high. How is my body going to withstand more treatments? And it did. I did a lot of self-talk and I was always out in nature when I had strength. Every week on a Sunday, my husband and I went to a nature park. Even if we sat on the bench, and walked a little, that was soothing.
I was always watering my plants. I teach positive psychology concepts to clients a lot. I’m a student of it. That and logotherapy, which is the therapy of meaning and purpose. I was really trying to input a lot of the stuff that I work with clients on myself. Little bits of joy and pleasure each day. Get up. What are your plans? Go outside. I was sitting out on my deck most of the summer. Even if I didn’t feel well, I would lay there on the lounge. I tried very hard to cope in a way that was helpful to me.
I did a lot of self-talk and I was always out in nature when I had strength.
Did you join any cancer support groups?
As a therapist, people said to me, “You can join a support group.” I said, “No, I cannot.” I lead support groups, women’s groups, and all kinds of stuff. I said, “I can’t be in a group and hear everyone else’s stuff.” That was my intuitive sense. I didn’t think that was going to help me. I had friends who called and said, “This one had what you had and she came through it great.” I said, “You know what? Thank you. I don’t want it. I can’t hear everyone. I have to go through this my way and maybe down the road I will use it, but not right away.”
I had in my mind this image of a horse with blinders who put one foot in front of the other and plowed through. I never went online to look. I did not want to hear the side effects of medicines, because then I’d have every one of them. I didn’t want to hear stories of people who ended up with a stem cell [transplant] or this [treatment] failed. I never Googled and looked things up online.
»MORE: Read More About Cancer Support
What’s one thing that helped you on your cancer journey?
I wanted to do something a little more creative, so I started doing these cards. Here’s one for example. [Holding up a card with a picture] Here’s the horse with blinders. I wrote on it, and then my husband would laminate it. “A horse with blinders keeping on the straight path, putting one foot in front of the other.” Then I would write on the back my intention. “My intention is to be grateful for this aspect of myself that has served me well.”
I call these my coping cards, but I will show you one that I did from the beginning. I took this from my first lumbar puncture. The technician who was setting me up said, “What are you holding?” I said, “I’m holding a card.” He must have thought I was nuts, but who cares? You do what’s going to help you. The previous summer, my husband and I had done a national park trip. [Holding up a card with a picture on it] This is Zion National Park and that’s me, small against these humongous mountains. I thought that was really powerful. I wrote “Embracing Strength.” In the back, I wrote, “My intention is to allow the strength of the mountains to support and embrace me in coping with this process.”
I would take some of these cards, and I’ve done tons through the treatment and after the treatment. I enjoyed the process of doing them. I love finding the pictures and what they mean to me and writing on the back.
Seeing a therapist during and after cancer

After cancer treatment, you’re on a forever healing journey.
I also did have a therapist who I was seeing, a new person, but very different. Not the typical therapist I found on one of my favorite blogs called Tiny Buddha. People write guest posts. I’ve submitted a lot also, and this woman wrote this guest post about 3 components. Nature, creativity, and mindfulness. I was reading and thought this really hit home.
I emailed her and said I’m going to be starting treatment. I really want to engage in something individual, not group, not typical therapy. Something creative that will get me out of myself and get me out of my own head. Something new. We started working together, and to this day, I still work with her because, after cancer treatment, you’re on a forever healing journey. She is amazing. It was a completely different way of dealing with adversity and anxiety through the arts. I mean, I still draw stick figures, but we did these together and it was an amazing process with this woman. That is a big deal that helped me.
Using visualizations to overcome anxiety
My good friends would say, “You’re never talking about how you feel. You’re talking about all the road stuff and the concrete stuff.” I felt like part of my coping, when I look back is, I shut down from the feeling just to get through it. It was just too much to let myself feel.
After round 4, when I had lost a lot of weight and I was terrified, the anxiety was sky-high. I reached out to a hospital social worker to have a couple of sessions to talk about it. I’m not saying I know it all, but there was nothing I didn’t really know. I would do my meditation.
I had a good friend who would lead me on the phone through visualizations of lavender light coming down and healing. I had a lot of visuals, this being one of them, the idea of a field. I love flowers. My field, at that point, was dark because that’s where my lymphoma was. It was brown and muddy. That was my visual. But [sunflowers] stand tall and proud and they face the sun. They were my protectors around that darkness so that none of the secondary infections if you wanted to go there, would enter. These were my visuals. That was a big coping tool also.

This friend of mine who actually teaches meditation, went through his own cancer horror stories. I would speak to him a few times a week or he’d say, “Whenever you feel overly anxious, call me. We’ll do a 20-minute visualization.” It was very, very helpful. It would quell some of the anxiety.
A couple of times I took marijuana edibles. I didn’t like it. It made my head feel like I was in another world, so I stopped. I inputted whatever I could do naturally that would help. Usually, it was being out in beauty.
What would you say to someone facing anxiety over cancer?
Anxiety is future worry. Regret is past upset. The biggest thing I could say is take one day at a time. If I would start at the first round thinking I’m never going to get through 6 rounds, I would have been a basket case. I would put a stop sign in my brain. If I would start to say, how am I going to do it? I would stop myself and say, we’re going to do 1 round. We’re going to get through 1 round. We have smoothies when the sores come and in the third week, you feel better. You’re going to go to that park and this park and that’s it.
That’s how I really try to do it, 1 round at a time. If I allowed myself to think, oh my God, how am I going to get through it? I would be crippled. At round 4, I did think like that because the weight loss was the highest at that point and that’s when my anxiety levels skyrocketed. It took me a while to manage it, to come back and go through the rest.
The biggest thing I could say is take one day at a time.
»MORE: Cancer and Mental Health
Follow-Up
What have scans shown post-cancer treatment?
I had my scan on Thursday. I had a scan after the fourth to see if the chemo was working, and it was. Then I had a scan after I finished treatment, September 22nd, at the end of my chemo, after I rang the bell. I love that I rang the bell. That was such a great thing. Thank God it was clear. I had one in March and I just had my recent one a few days ago. I have to have them every 6 months for 2 years after finishing chemo. I think I have 2 more in March and then next September.
Do you experience scanxiety?
The scanxiety, I know that’s a new word, is high. We all know we’re going to get something. None of us are here forever. Someone could be diagnosed with something else in 6 months. Why does this feel so much scarier? Why once you have a diagnosis, does it feel like you’re forever with an axe over your head? I haven’t figured that one out yet, but it’s there every time I have a stomach thing now.
I had an episode in the last couple of weeks. My blood work was a little out of whack. Oh, my God, is this it? Thank God it wasn’t. It was clear, but this is where you go. That’s a little hard. I haven’t quite wrapped my head around how it’s so much different than anyone else just because they haven’t had a diagnosis. We’re all waiting our turn, so to speak. Nobody goes through unscathed, but once you have it, it becomes more real that it could be a recurrence.
What did your most recent scan show?
I just got the results Monday, and thank God it’s all clear. I was greatly relieved. I have to say, I was very spoiled. I normally get the results on the same day. I get the PET scan, I do my blood work, and I see my oncologist, but this time I didn’t. I have a Zoom call with her on Friday, but I got the results through the portal. I was nervous to open the portal, but I couldn’t not do it. Thank God, it came out good.

You don’t just go back to life as it was.
When you get a good result like this, and I would imagine everyone feels like this, you feel a sense of renewal. I get a 6-month reprieve. Six months doesn’t mean I can’t go out and get hit by a bus, but I have a 6-month renewal on life. Now what am I doing? How am I going to show my gratitude? How am I going to pay this forward? My husband thinks I’m nuts. He says, “You’re doing enough.” But I feel so compelled to ask, what am I doing with this good news? You don’t just go back to life as it was.
Reflections
What are you doing differently since receiving a cancer diagnosis?

I don’t live that much differently. I’ve always lived with a very keen sense of appreciation and enthusiasm. I have a daughter with disabilities. She went through a critical illness for a year. I had other challenges, believe me. I’ve learned a lot of things about how to live life. I look at this and say this is another jumping point, another level. It’s not like suddenly, now I appreciate sunsets or now I appreciate my family. No, I’ve always had this.
The one thing I am doing now differently is more internal work with this therapist, Elizabeth. Visually, I need to clean out the cobwebs in there so that more beautiful flowers can grow. We hold onto a lot of stuff. There’s resentment and anger and this and that, and I’m working much more on my internal landscape emotionally and psychologically.
When you’re going through it, it’s got to be one tiny step at a time. Don’t think of the long road ahead because it is too overwhelming and anxiety-provoking. You have to be cognitively attuned to one step at a time. Don’t project, how will I do it? Because that’s too anxiety-provoking.
The other thing is, it’s an opportunity to really go into ourselves, to better ourselves as people and not just to say, I appreciate life more. Absolutely, this will give them more gratitude and appreciation, that’s great. Beyond that is, and it’s not selfish, it’s saying let me let go of some of the old stuff. Let me forgive more, let me be more self-compassionate. Everyone, not just people who had traumatic childhoods. Every single person I believe needs this because we all carry this stuff.
There’s a book by Bessel van der Kolk, The Body Keeps The Score. We hold onto our stuff, and how do we know if that’s not one of the precipitating factors of growth? We know we all have cancer stuff in our bodies. It’s just when the terrain is right, they explode and grow. I think it behooves us all to work on our hearts. That’s a big deal.
Choosing to see the miracles
I was very cognizant of miracles every step of the way. I always try to look for the silver lining, but not to be Pollyanna-ish. To just embrace that there is a lot of good throughout and I can just give a couple of examples. I have terrible teeth. I had my teeth flare up. I was so anxious about that. My oncologist forbid me, “You cannot go to a dentist. Your immune system is compromised. That’s the biggest place for germs.” I would pray that my teeth would hold until I could go to the dentist.
In September, after my treatments, the first place I went was the root canal dentist. Who is happy to sit in a dentist’s chair? Nobody except me, I was thrilled. In fact, I took a picture. I was thrilled to be in the dentist’s chair, to finally be working on my awful teeth that served me and held up well. Now every night when I brush my teeth, I say, “You serve me well. I have to do my part in keeping you as well as can be,” even though I’ve lost half my teeth. I’m so cognitive. That was a miracle.
It was a miracle that I went through each cycle without a break. Sometimes people need breaks because they have an infection or because their blood count is too low. I was able to do it each cycle on time. Nothing thwarted it. I hear these stories all the time, “They had to put it off a month…My counts are too low…I ended up in the hospital with this infection, with that infection…” No matter how rough it was, I got through each cycle. Miracle! I could go on.
You have to look at it and say, within the bad, there are these amazing things because it could have been much worse. I was so scared to do my treatment at home. [I feared] it would keep beeping and I would have to run back into the city. Nope. One time it kept beeping and I was due to go back anyways into the city. Because I live on the island, my treatment was at Columbia in the city, so even the bag worked out. It never had glitches in the little fanny pack with the chemo. You need to be intentional about looking for that and then feeling, wow that’s pretty cool.
Thank you for sharing your story with us, Harriet!

Thank you for inviting me to come on. It’s a great opportunity and I hope it’s a source of help or inspiration. We always want to give hope to people going through bad stuff like I went through.
More Non-Hodgkin’s Lymphoma Stories
Jen N., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4B
Symptoms: Blood-tinged phlegm, whole-body itching, shortness of breath, lump near collarbone, night sweats, upper body swelling, rapid weight loss
Treatments: Chemotherapy, immunotherapy, lumbar puncture, autologous stem cell transplant
Jim Z., Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Sudden and severe head and neck swelling, purplish facial discoloration, bulging neck veins
Treatments: Surgery (resection and reconstruction of the superior vena cava), chemotherapy
Nolan W., T-Cell/Histiocyte-Rich Large B-Cell Lymphoma (T/HRBCL), Stage 4
Symptoms: Debilitating fatigue, flu-like symptoms without a fever, swollen lymph node under the left arm
Treatments: Chemotherapy (R-EPOCH & RICE), bone marrow transplant
Mike E., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Persistent, significant back pain
Treatments: Surgery, chemotherapy




