Lena’s Stage 1 Diffuse Large B-Cell Lymphoma (DLBCL) Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

Lena was diagnosed with stage 1 diffuse large B-cell lymphoma (DLBCL) and shares her journey from pre-diagnosis to life after cancer.
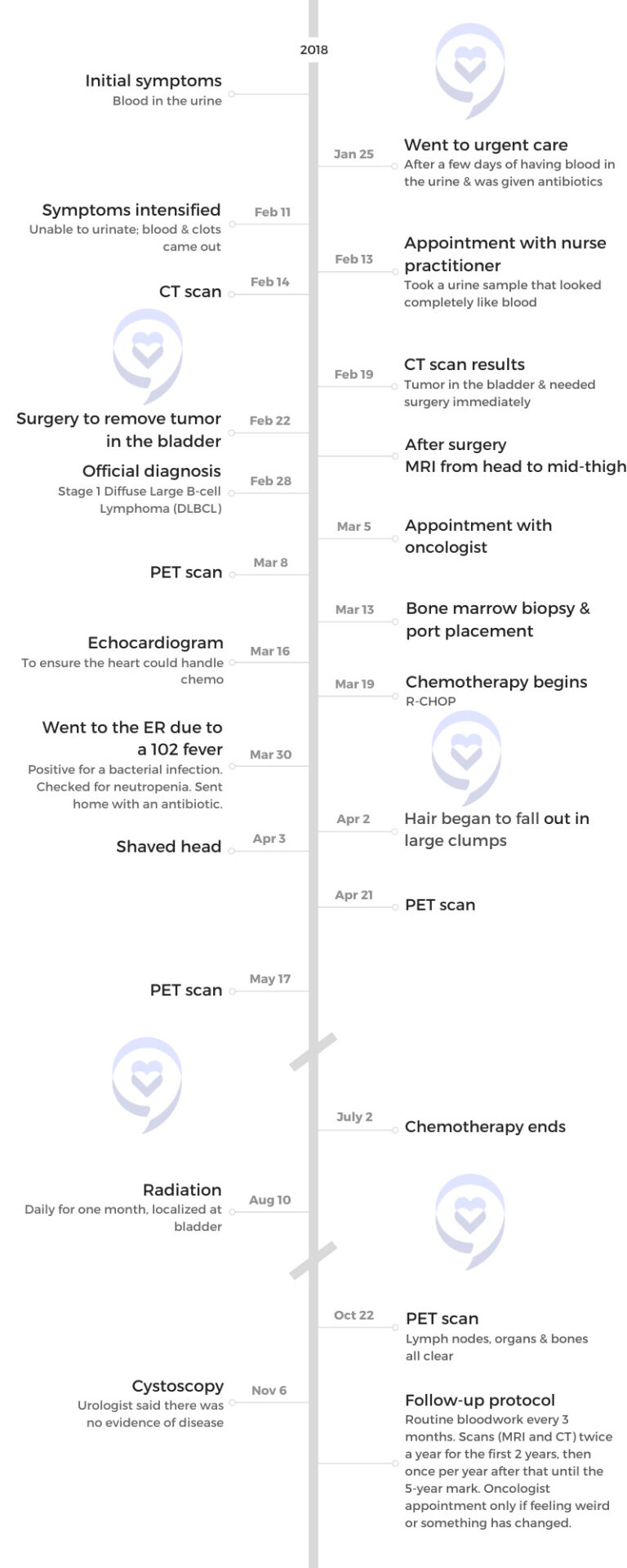
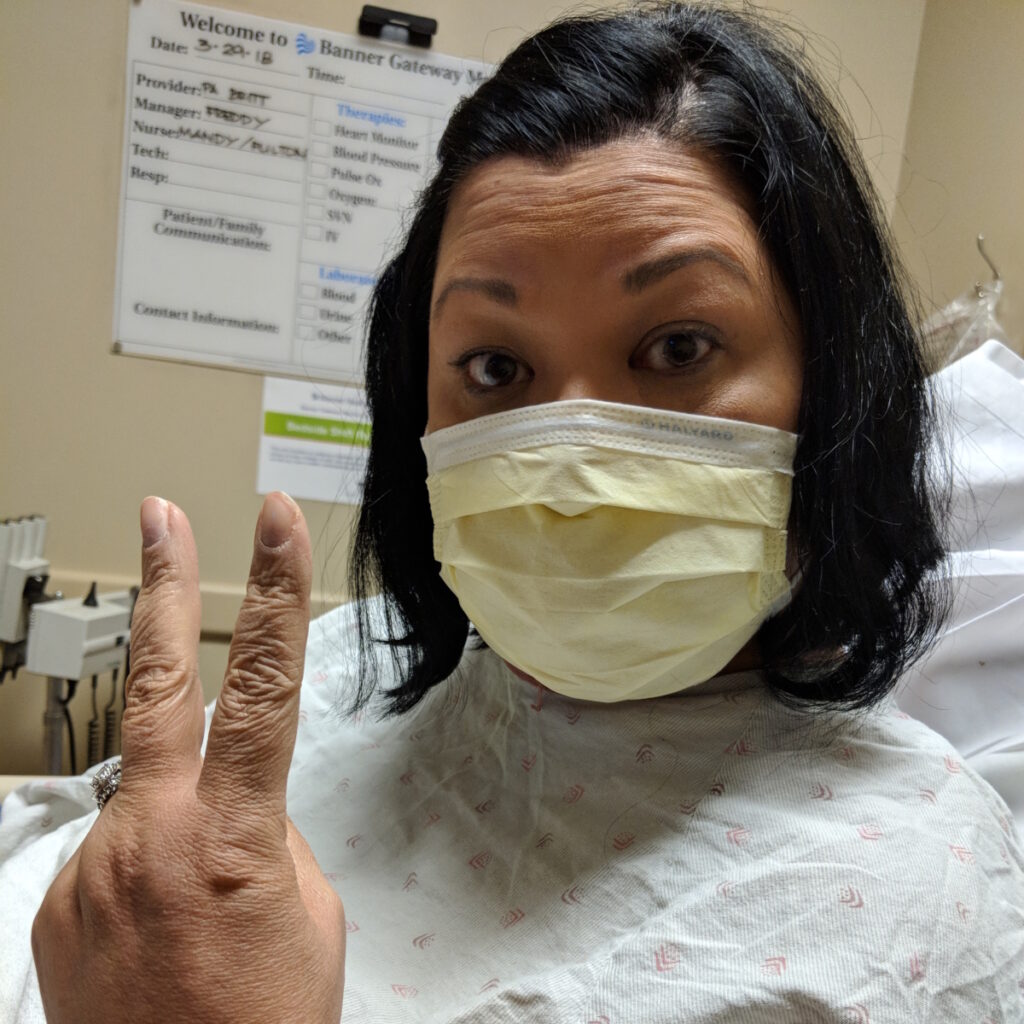
Initially, she had blood in her urine, which she thought meant a UTI. After being treated with antibiotics, her symptoms first alleviated and then worsened, which eventually included clots in the blood. Further tests revealed a bladder tumor. Despite having no typical signs of DLBCL, the diagnosis came unexpectedly after she had surgery to remove the bladder tumor.
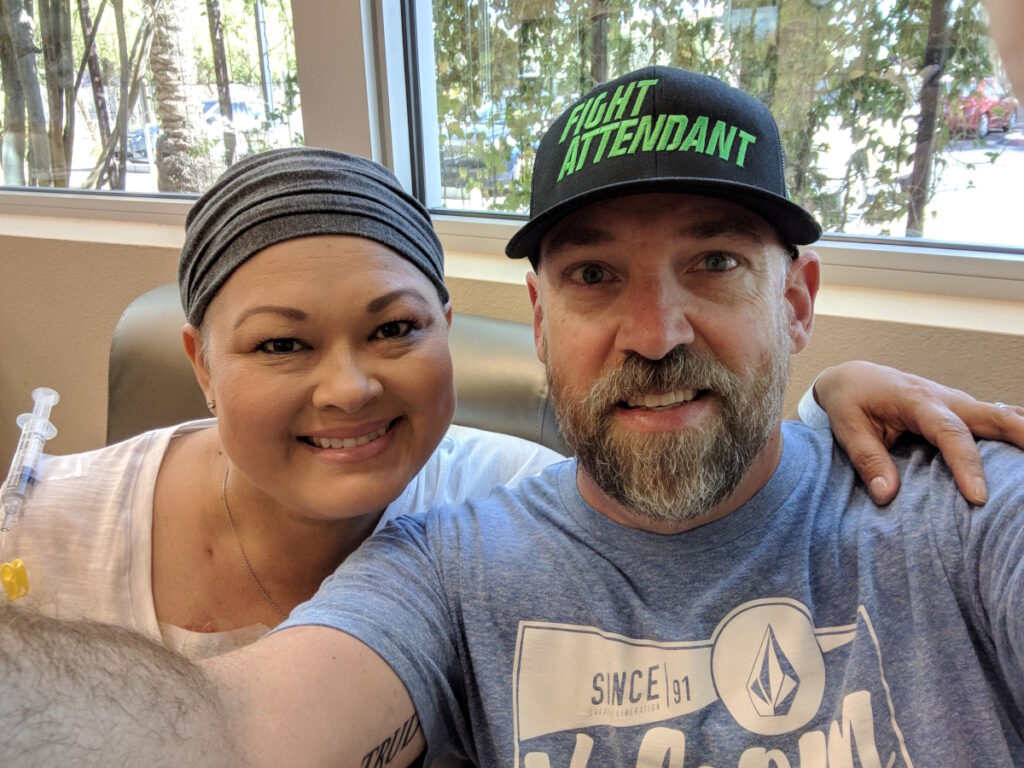
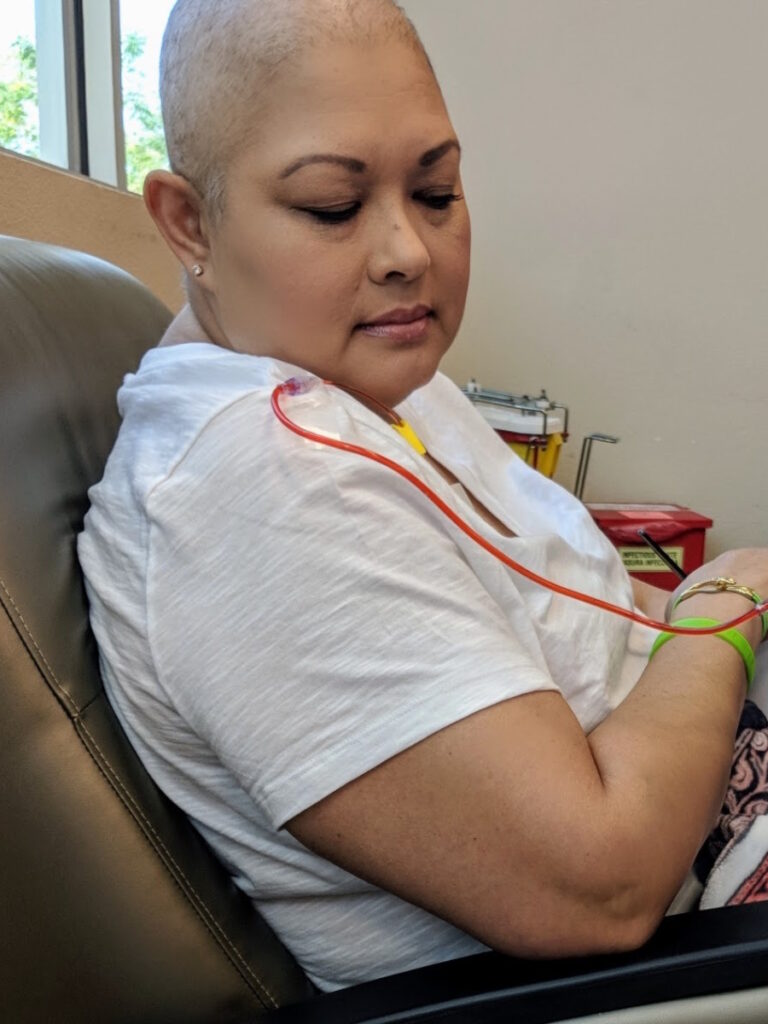
Lena recounts the challenges of chemotherapy, including severe reactions to certain medications and the emotional toll of losing her hair. Following chemo, she underwent a month of radiation, which she found relatively easy compared to the previous treatment.
She highlights the various side effects faced during and after treatment, such as neuropathy, loss of taste, and early menopause. She also emphasizes the importance of managing emotional well-being, seeking support during and after cancer treatment, and staying strong throughout the cancer journey.
She shares her positive approach, acknowledging the support received from family, friends, and medical professionals. She encourages open communication with doctors, advises against excessive online research, and advocates for finding the right medical team and support groups.
In addition to Lena’s narrative, The Patient Story offers a diverse collection of diffuse large B-cell lymphoma (DLBCL) stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Lena V.
- Diagnosis:
- Diffuse Large B-cell Lymphoma (DLBCL)
- Staging:
- 1
- Initial Symptom:
- Blood in urine
- Treatment:
- Surgery
- Chemotherapy: R-CHOP
- Radiation


This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
Don’t give up. Stay fighting. Stay strong.
Introduction
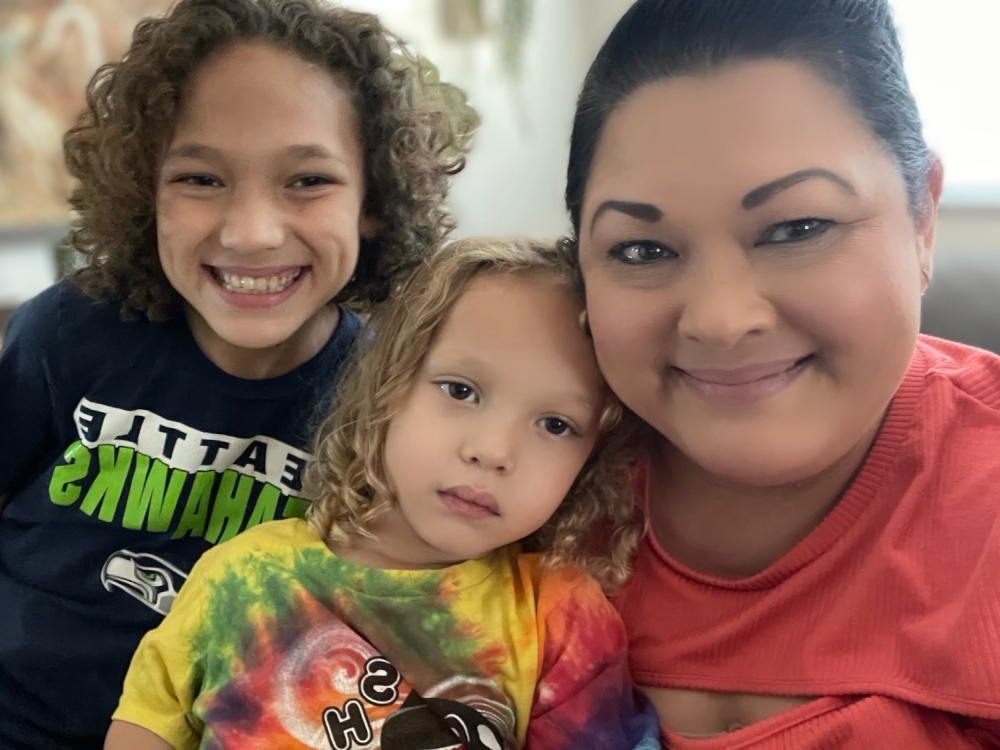
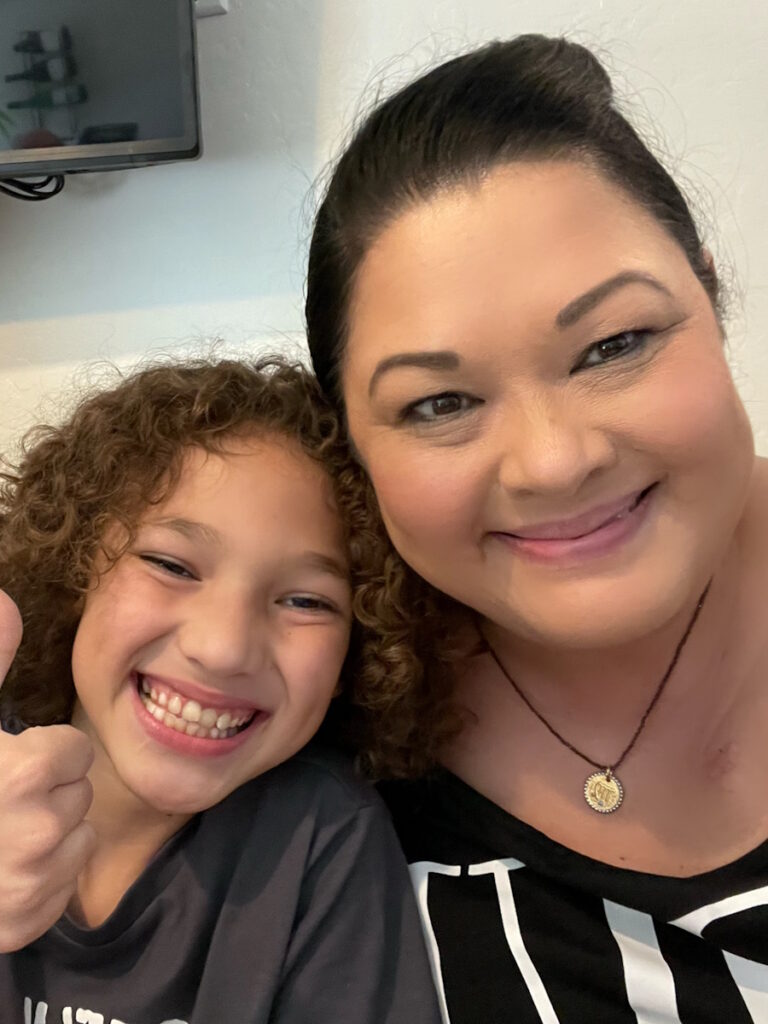
I’m 53 years old. I’m a wife, a mother, and a grandmother. I enroll students for a university in Arizona. I live just outside of Phoenix in Mesa.
My husband has a motorcycle. We like to go motorcycle riding in the winter when it’s cooler because it’s so hot in the summer.
We have lots of kids around us and grandkids that we like to spend a lot of time with. We are a blended family of six children, ages 32 to 14. The 14-year-old lives with us. He’s our last one in high school.


I love to bake. I love to cook. I socialize.
I do a lot of work with The Leukemia & Lymphoma Society here. We did Light The Night. I have been nominated as a visionary of the year for 2024. I’m super excited about that.
We have learned to be very grateful and live our best life. Every day is a blessing.

Pre-diagnosis
Initial Symptoms
I had no symptoms that are typically involved with diffuse large B-cell lymphoma. I didn’t have any pain, fever, night sweats, or weight loss. I was told after the fact that it typically affects men who are over 65.
I thought I had a UTI. I had a little bit of blood in my urine. I went to urgent care and they did the routine test, gave me an antibiotic, and sent me home. That alleviated the blood in the urine for a few days then it came back heavier and with clots in it. That’s when we knew there was a problem.
It was completely out of the blue. I was healthy. We were newlyweds. We were about a year and a half into our marriage. We sold a house that we had as a rental and we were doing some work on the inside of it. We were celebrating my son’s birthday the next month.


I remember going to the bathroom at the restaurant three times. I thought I was getting a period. I wasn’t sure, but I had no pain. The next couple of days, it seemed like there was always blood and I thought I had a UTI or it was in my kidneys. The reason I went to urgent care was to make sure there was nothing else going on.
I took the antibiotic they gave me for a week and the blood had alleviated. There was no blood for about 3 or 4 days then it started to come back slowly and I thought, Maybe this infection is coming back. Maybe it’s farther into my kidneys than I thought. I still didn’t have any pain, fever, or any other symptoms but the blood.
There were clots in the blood so it was getting harder to urinate because the clots were blocking the way. I was trying to use the bathroom and it hurt. I couldn’t go at all because there was a blood clot blocking the way. I didn’t realize that at the time, but I figured with everything that had happened that was the issue.
I was crying and my husband said, “We’ve got to get you to somebody.”
Trying to Get a Urologist Appointment
The next day, I called a urologist and told them what my symptoms were. I had to call six of them because they were so busy. One of them was backed up for about six months and I thought, I can’t wait that long. That’s a long time.
I found an opening the next day, but it was with a nurse practitioner. I said, “I’ll take it. I will absolutely take it. That’s fine.” I saw her and gave a urine sample, but it looked like a cup of blood. She said, “Everything that we’ve tested looks very interesting so I’m going to send you over and we’re going to get a scan done.” That’s when I went, “This is not good.”
Getting Referred to a Cancer Center
I went over the same day to check in and I drove into the parking lot and it was Ironwood Cancer & Research Center. That’s when I thought, Oh boy, is this cancer? I didn’t know because she didn’t know and she didn’t tell me it was. She said, “We’re going to take a look at it because we don’t know what’s going on.”
The urologist was amazing. He took out most of the tumor. He couldn’t remove all of it because it was attached to the wall of my bladder.
Getting a CT Scan
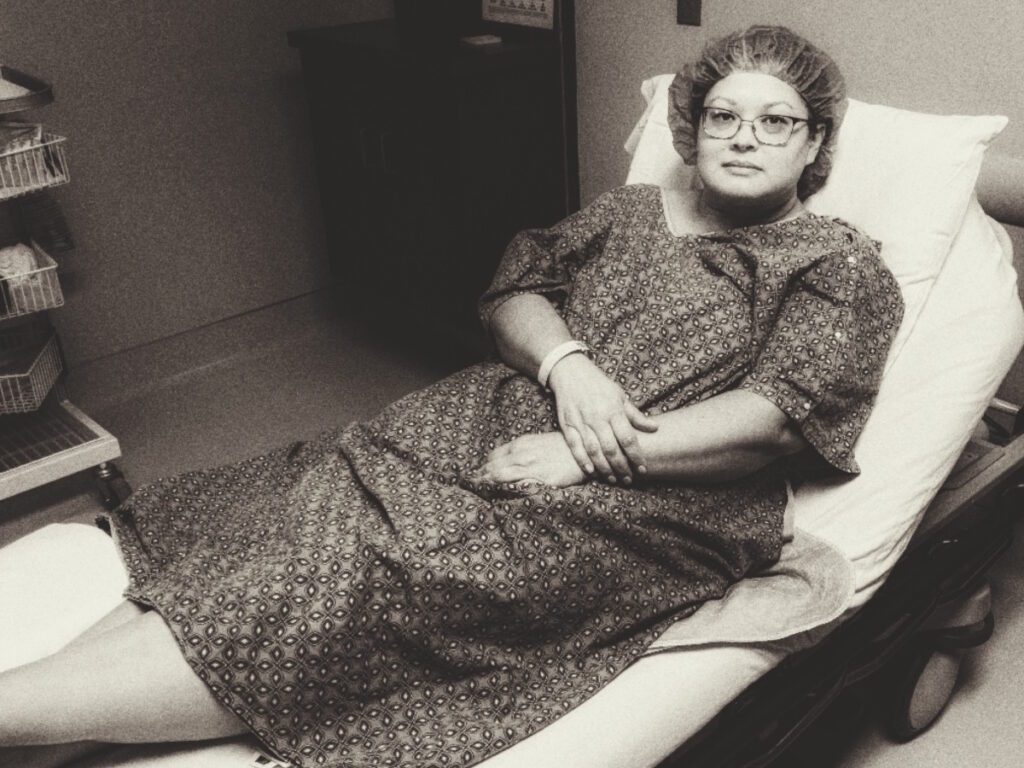
I had the scan done on Valentine’s Day. On Monday, which was President’s Day, I got a phone call and they said, “We’ve looked over your scan. You have a tumor in your bladder.” It was about 5 cm, which is the size of a lime. They said, “We’re going to have to remove it immediately so we’re scheduling you for surgery on Thursday.” This went from zero to surgery.
Surgery to Remove Tumor
I had the surgery done and the urologist was amazing. He took out most of the tumor. He couldn’t remove all of it because it was attached to the wall of my bladder. He said if he removed it all, it would have perforated my bladder and that’s a whole different lifestyle for me so he opted to leave part of it there to protect my bladder.
Going in, they thought I might have bladder cancer and he said the tumor looked nothing like bladder cancer, which typically resembles a flower. We thought maybe it was a cyst. At that point, we thought, Wow, it’s not cancer! That’s great! We didn’t even think it could be a different kind of cancer.
After my surgery, the doctor spoke to my husband and my mom who had flown from Montana to help. He said, “We’re going to send this off for a biopsy.” I went home with a catheter for a week to help my bladder heal.
Had we not caught it when we did in February, I would not have made it to my birthday in September. It probably would have killed me before then.

Diagnosis
Getting the Official Diagnosis
The day I had my catheter removed, the doctor accidentally called my husband on his way home from work, thinking it was my number. He ended up telling my husband my diagnosis and my husband had to tell me, which I can’t imagine being in his shoes.
He came home and pulled me away from my mom to take me into the other room and said, “Dr. Matthews called me accidentally, but he told me what’s going on. You have diffuse large B-cell lymphoma.”
I was trying to be so optimistic. I said, “I have no idea what that means.” He said, “It’s a type of cancer in your blood and he’s very thankful that we caught it because now you can get treated for it. You’re going to do six rounds of chemo and a month of radiation possibly.”
Thankfully, it was caught because Dr. Matthews told me this type is very aggressive. Had we not caught it when we did in February, I would not have made it to my birthday in September. It probably would have killed me before then.
I knew nothing about staging. I was stage 1, which means it didn’t spread to any other areas of my body so that was why they did the bone marrow biopsy. They wanted to make sure it wasn’t in my bones.
The scans were to make sure it wasn’t in any of my organs that were around my bladder. My bladder pretty much contained it all, luckily, because it could have spread to my liver, to my stomach, and all of those organs right there. My bladder held it in and that’s what saved me.

Reaction to the Diagnosis
My mom is a breast cancer survivor. She was on hormone replacement therapy, which is what caused her to have breast cancer. She had a mastectomy done. She’s a fighter. She’s tough, she’s fierce, and she’s feisty. She’s a little Thai woman and she’s hilarious. I take after her quite a lot in that area.
I sat there in shock after my husband Dave told me and thought, Wow, really? Are you sure? I got upset a little bit because my dad wasn’t there. We shared the news with my mom and she had this look on her face. She stood up, slapped my arm, and said, “You’ll be fine,” and walked out of the room. I said, “She’s right,” and that was the attitude I had the whole time. This isn’t over. I’m just starting.
‘I have a lot of life to live. Can we get started ASAP?’
Treatment
Discussing the Treatment Plan
After we had determined my steps, I was referred to an oncologist at Ironwood Cancer & Research Center, which was a mile and a half from our house. I met with Dr. Monique Chang. I had my mom and my husband with me.
The minute I went in there, I said, “Look, I have a lot of life to live. Can we get started ASAP?” She said, “Oooh, you’re a spitfire.” And I said, “I am. This is not going to get me. We’re going to do this.” And she said, “Absolutely.”
We set up the appointment for chemo, but I had to have an echocardiogram, a port placed, and a bone marrow biopsy. They wanted to make sure that it wasn’t in my bones. Those were the next steps before my first treatment.
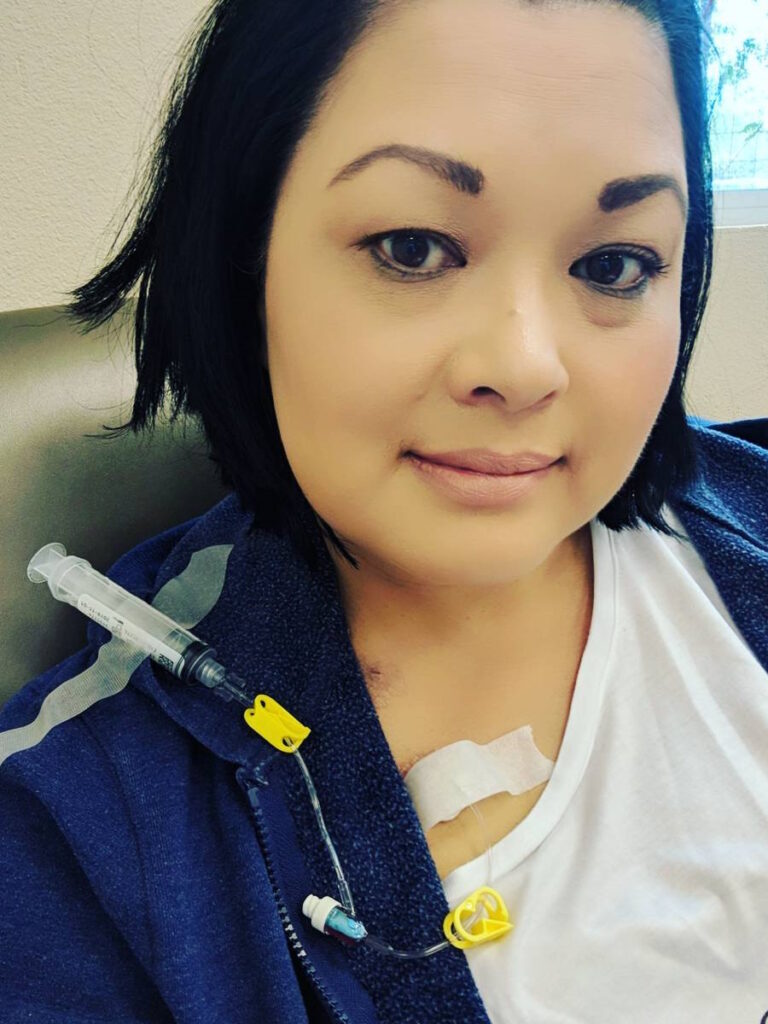
Chemotherapy
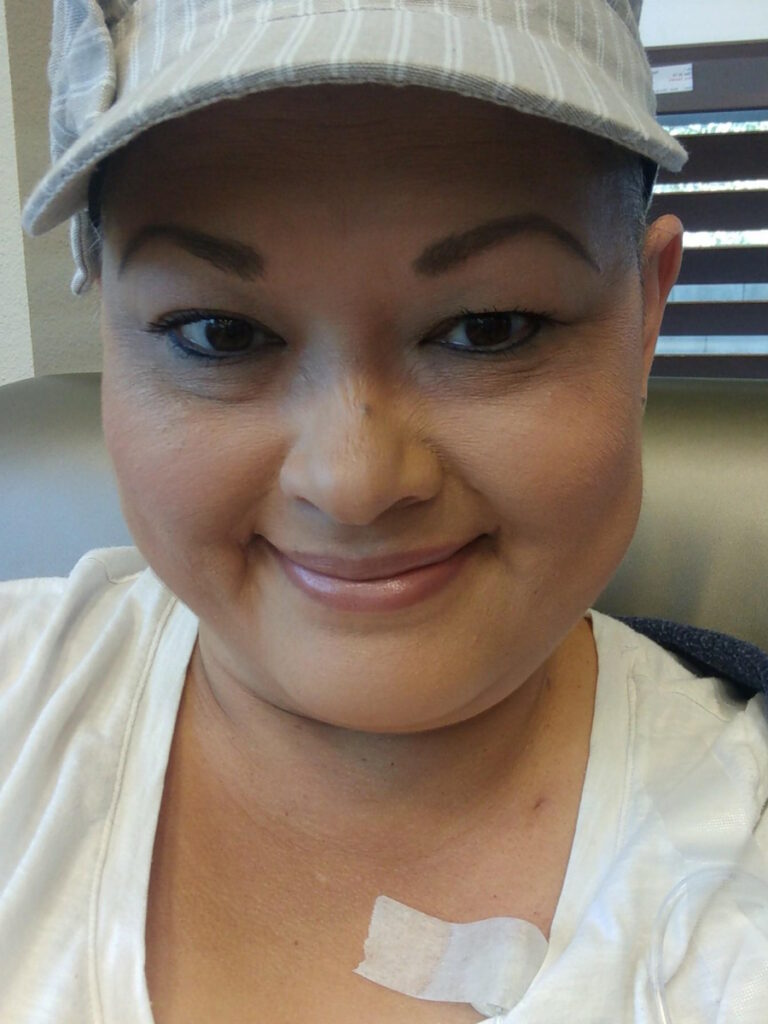
I did R-CHOP, which is a very common treatment for DLBCL, but I also have the Neulasta device on my arm. The device itself didn’t hurt. It helps rebuild your bone marrow so it’s very painful when you’re healing from that.
The injection is the day after chemo. It injects you for about 30 minutes and it’s painful the next couple of days out. It was probably about a week after that that you ache. Your bones ache because it’s regenerating all those white cells for you.
I did chemo every three weeks from March to July 2nd. My very last treatment was on my husband’s birthday.
Radiation
After chemo, I did a month of radiation. The doctor wanted to make sure they got everything. It was one treatment daily for the whole month of August 2018.
Radiation was a piece of cake for me because I didn’t feel anything. They made a pillow that fit my body in the area where they were scanning it and I would just lay there. It was under 30 seconds every day and I was out of there. The wait in the waiting room was longer than the radiation itself.
After chemo, I had a stutter so it took me a while to be able to talk again to where I could piece a sentence together.
Side Effects of Cancer Treatment
R-CHOP was difficult. On my very first chemo day, we went at 7:30 in the morning and they told us it was roughly 5 to 6 hours. For us, it was almost 11 because I reacted to vincristine, which they call the Red Devil.
It was brutal. The first time I had it, I turned red and felt like my insides were made of lava. I felt like I was melting. It was that bad of a reaction. They slowed down the drip for that and that helped so I never had a reaction again.
In between each medication, they gave me Benadryl so I was completely groggy by the end of the day. Honestly, I’m not sure how my husband got me out of the car and into the house. I remember that being a very, very long day.


I had to take prednisone as well, which is not my friend. I know that it’s very helpful for a lot of people and it’s part of the regimen for this particular type of cancer.
I was taking five doses of prednisone a day for five days each time I had the treatment. I gained a lot of weight because of it. Normally, cancer patients lose weight because of chemo and being sick and nauseous. That may be the case, but the prednisone started packing on the pounds.
I had bad neuropathy. I still suffer from neuropathy. Five years later, I still have some issues. Not as bad as they were, obviously, but with every chemo session, I would get a headache right at the base of my skull and nothing would make it go away. It would go all the way down my arm.
By the end of chemo, I couldn’t tell the difference between hot and cold. My fingers and toes were numb. My hands and feet were a different color. They were grayish. I heard it’s a typical change. There was another patient there who she said all her toenails and fingernails fell off. They turned black and fell off from chemo.
Many different things can happen to you. I tried acupuncture to alleviate some of the pain, but it did not work for me. They tried to put me on gabapentin and other antidepressants, but the side effects from those were so bad that I didn’t want to do them.
I never regained a period so I got pushed into early menopause and had heavy, heavy hot flashes. I would have them for minutes at a time for probably about six months, midway through chemo until the end of that year.
I still have hot flashes, but they’ve slowed down. I didn’t take any hormone replacement therapy after my mom went through what she did. I said, “Absolutely not. I’m not going to do it. I’ll naturally let my body figure it out.”
After chemo, I had a stutter so it took me a while to be able to talk again to where I could piece a sentence together. I would try to talk and it would not come out. That took me close to a year to feel like I could speak normally again.


My very last chemo treatment was almost as bad as the first one. I was disappointed because it’s your very last one and you’re thinking, Oh, I’m done. This is great! I’m finished! It kicked my butt and I was down for about a week. Typically, after each treatment, I would be out of it. It was never the day after. It was the day after that for 2 or 3 days when I didn’t feel right at all.
I lost my sense of taste for almost two years. It’s still off. I love coffee, but it does not taste the same as it did at the beginning of 2018. It’s not the same.
I didn’t have any side effects from radiation. They told me, “You could have blood in your urine.” I freaked out when I heard that, thinking, I don’t ever want to see blood in my urine ever again. They said I could be fatigued. They said I could have burn marks. I had none of those so I was very lucky.
I’m not going to sit here and feel sorry for myself because it’s hair. It’s going to grow back. My mom’s came back after her treatments. It will come back.
Hair Loss Due to Chemo
My son was eight when I was diagnosed. We honestly weren’t going to tell him. I said, “We can hide it. I’ll be okay.” I told the nurse, “I’m not going to lose my hair.” And she said, “Oh no, sweetie, you’re going to lose your hair. You don’t have a chance to keep any of it.” I thought, I’ll be the one that does. It’s okay. I’ll be the one, trying to psych myself up.
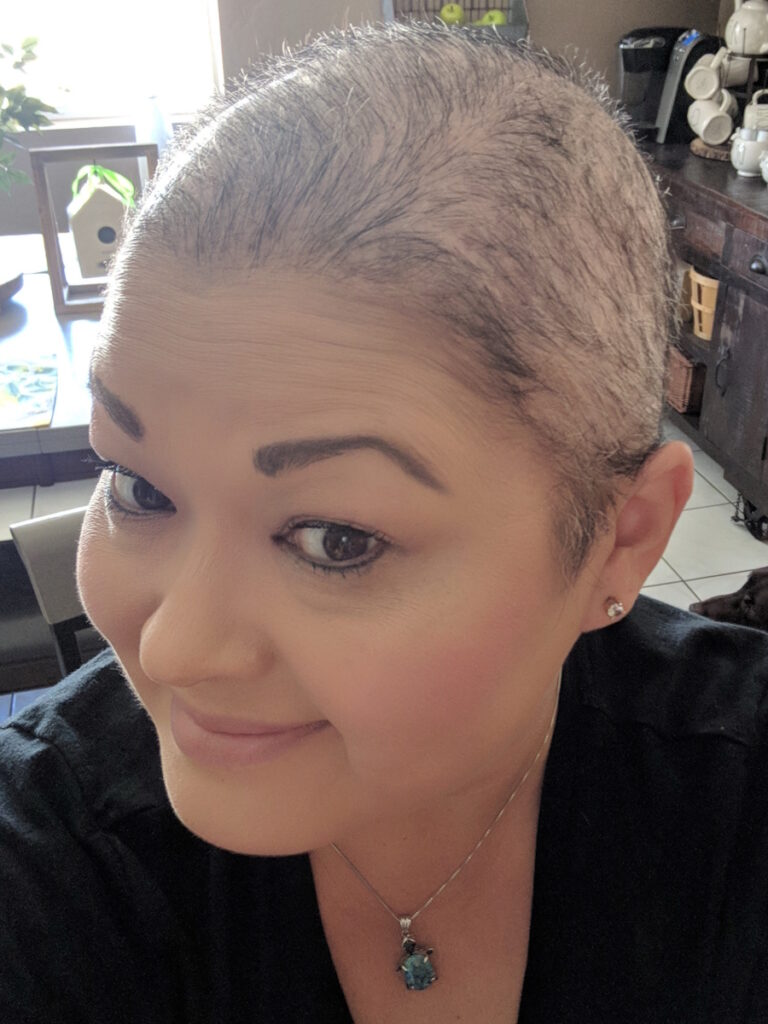
I woke up one day and our white bedding had a big pile of hair. I started brushing it and the sink was full of hair. That was after my first treatment.
I cried for about an hour and a half, sitting there, pulling it, and combing it. I could feel where I had little patches and thought, I’m not going to sit here and feel sorry for myself because it’s hair. It’s going to grow back. My mom’s came back after her treatments. It will come back.

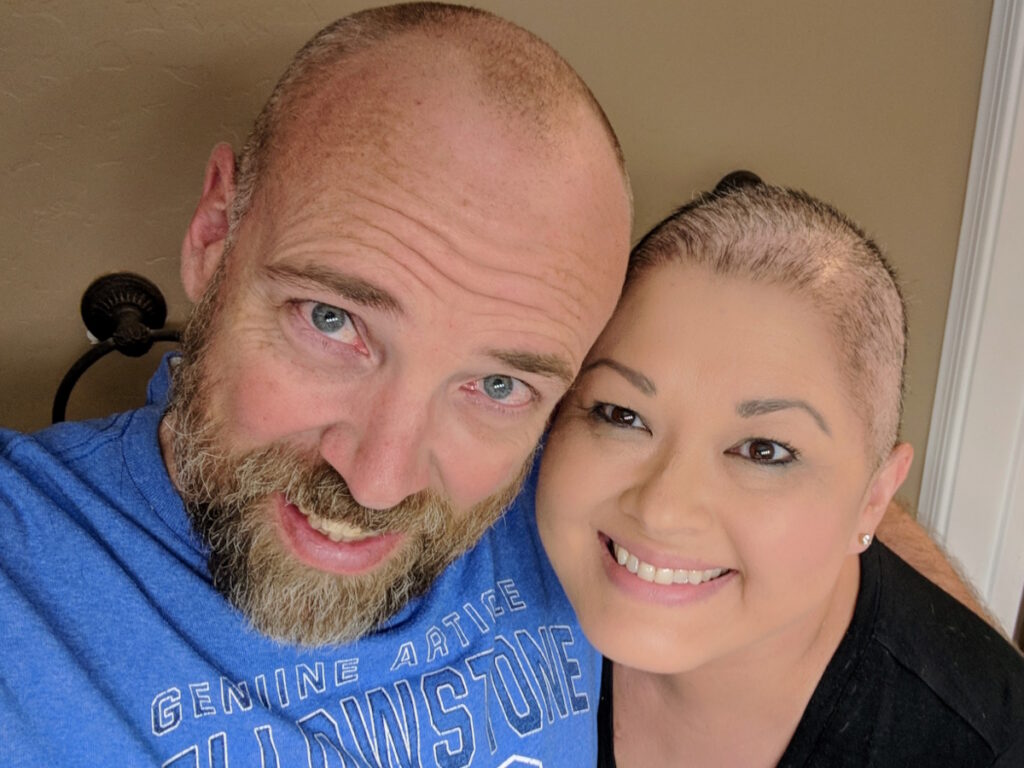
That night, my husband shaved my head. Not gonna lie, it was hard. It was hard for him. He didn’t want to do it. I said, “I need you to. I can’t do it by myself.” At the time, our son came in and said, “You shave my head, too,” so we all shaved our heads together.
It’s tough. It does grow back. My hair grew back weirdly. Initially, it grew back white and stubbly. That all fell out and then it grew back to salt and pepper, which was appropriate for my age, but it was curly like I had a perm. That lasted about a year. Then as it grew out, it returned better than it was. It’s thicker and healthier than it was before.
Managing the Side Effects
The neuropathy is much better. I use CBD oil; that was the only thing that relieved the pain. I take CBD gummies to help me sleep.
I’ve been suffering from neuropathy for about a year and a half. I was trying Tylenol, ibuprofen, and Aleve, and nothing was working. I thought, This is something I’m going to have to deal with. I’m alive. If this is the worst of it, I accept it. I’m still alive.
One of my friends and I were standing and having a conversation and she said, “Have you ever tried CBD?” I said, “No, I never really gave it a thought.” She said, “You should try these.” I thought no because in my mind, you’re going to smoke weed and I didn’t want all those weird side effects either. I thought, No, it was never my thing. I’m not that girl. I don’t want to do that.
She said, “There’s no weed in it. Let’s try it.” She had a little tincture bottle in her purse and she put two drops under my tongue. Within an hour and a half, the pain was completely gone and it never came back.
It’s not going to work for everybody. I got lucky that she suggested it because I probably would have never done it on my own.
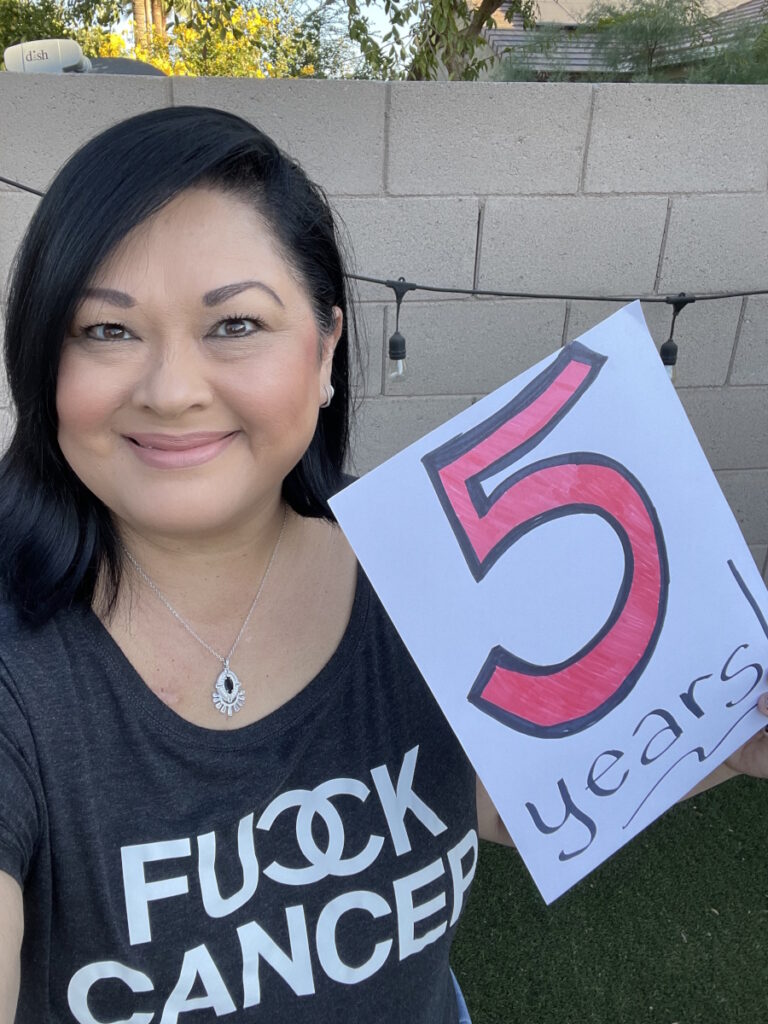
Once you reach the five-year mark with this particular type of cancer, you are considered cured.

Monitoring with Scans
I was pretty good about keeping a journal. I’m very organized. I kept every piece of information because I still have chemo brain. There are things that I’ve forgotten that people remind me of and I can’t remember.
I had the CT scans and PET scans often when I was going through treatment. I had one at the beginning, one at the midpoint, one right before my final treatment to make sure it was going to be my final treatment, and one after my final treatment.
I’ve had to have a cystoscopy where they go up into your bladder with a camera. My urologist at the time was wonderful. He has since retired, but I never felt any pain and he was amazing. He was a good source of positivity.
I don’t have to have a cystoscopy or scans anymore. If I start to feel anything off, they told me to come back and they’ll check me out completely.
At the end of chemotherapy, they said that everything looked clear. November 6th was my final cystoscopy after chemo. That was when Dr. Matthews said there’s no evidence of disease so that is what I count as my anniversary date.
Dr. Chang told me that once you reach the five-year mark with this particular type of cancer, you are considered cured. I was thankful that she removed my port when she did because many patients have to keep a port in for at least a year or two after treatment. She was confident enough to let me get mine removed.
I said, “I can sleep on my stomach again. I don’t have this object protruding out of my chest and I don’t have people staring at me.” I don’t care if you stare at me now. This is a badge of honor, honestly. It was a good feeling to hear that there was nothing left.
When I saw Dr. Chang not long ago, she said, “You did it.” I said, “You helped me do it because there’s no way I could have done it alone.” She’s amazing. She’s in the Phoenix top 100 physicians and she’s incredible.
Even on my worst, worst, worst day when I was miserable and in bed crying because I was in so much pain, I knew there was light at the end of the tunnel.

Managing Scanxiety
I know it’s not realistic for all people, but if you can, have somebody go with you. My husband typically would go with me and wait with me. I would go in there with a positive attitude.
I know it’s hard. It is hard. Even on my worst, worst, worst day when I was miserable and in bed crying because I was in so much pain, I knew there was light at the end of the tunnel. I had to keep going because if I gave up, what good would I be to my kids, my grandkids, and my family who were watching me struggle and were helpless?
You’re the one in charge of your emotions every day. You have to get a hold of that and stay positive. Because if you let go of that and you sink into this hole, it’s really hard to get out of it.
I wanted my normal life back and it was never going to be like that again.
Life After Cancer
I had a hard time after treatment because I went into a bad depression, which made no sense. I’ve been used to this routine and being taken care of by these specific people. Then when you’re done and you don’t have that routine anymore, even your friends fall by the wayside. They check in once in a while. This is pretty common from all the people I’ve talked to so it’s not their fault.
When you think about somebody going through cancer and then they’re done with their treatment and they’re in remission, a lot of times people think you’re okay. We’re not okay.
I went through a lot of mental struggles. I had to go see an integrative oncologist. She was like a counselor. She tried to get me back to my new normal, which I was sick of hearing. I wanted my normal life back and it was never going to be like that again.

If you have a doctor that is not listening to you, it’s not the right doctor for you.
Shared Treatment Decision Making
I had a terrible family doctor who had the worst bedside manner and who wasn’t sympathetic. I’ll never go to another doctor who doesn’t understand and listen to me first of all.
A lot of times, people need a second opinion if they’re not comfortable with their doctor. With the surgeon whom he referred me to, I researched on her before I even saw her. When I talked to her, I thought, If I’m not comfortable when I talk to her, I don’t care what kind of accolades she has, I will find another doctor, because I’m very much one that will speak out and advocate for myself.
She listened to me and my needs. When I told her I was going through the pain with neuropathy, she was the one who sent me to the integrative oncologist who then asked, “Lena, what do you need most? I can put you on antidepressants. I can put you on this.” I said, “I don’t want to take medicine. I’ll do lion’s mane to rebuild my brain. I’ll do whatever it takes. I don’t want to take any more pills.”
She worked with me. She suggested acupuncture. She suggested lots of other things that were great. If you have a doctor that is not listening to you, it’s not the right doctor for you.
If you’re going through something, you have to reach out and let someone know. There is a ton of support.
Words of Advice
I shared a lot of information on social media not because I wanted attention for what I was going through. I wanted to share my feelings and be honest with people. I had people messaging me, saying, “Hey, my mom just got diagnosed.” “My brother got leukemia.” I’m able to use what little voice I have to try to help those people get through it.
I’m a big advocate for speaking up for yourself. If you’re going through something, you have to reach out and let someone know. There is a ton of support. I found that out after the fact because I lost friends with cancer through my journey. You have survivor guilt plus depression plus not going to treatment anymore. I miss my nurses who were fantastic in my recovery.
You’re in a whole new cycle of life that you’re trying to navigate and you still have it in the back of your head. Every doctor’s appointment, every time I go for a scan, every time I have blood work done, I think, Something’s going to go sideways.


Talk to somebody, even if it’s a stranger. LLS has all kinds of resources and support. They were huge in helping me find support. My oncologist had a list. They had support groups at Ironwood Cancer & Research Center. They were supportive. They had mental health checks.
I wish people would reach out. It’s important. If you’re feeling any type of way, do something about it because sitting there is not going to help. You’ve got to talk to somebody.
When you get diagnosed, do not Google anything. Don’t have family members do it. Don’t have friends do it. I was told that immediately and I listened. Had I done it, that would have probably put me down a rabbit hole of despair and giving up. Everyone’s journey is completely, completely different so stay on track.
Listen to your doctors. If they’re not listening to you, find a new doctor
Find support groups. There are tons of them out there. That’s how I found The Patient Story. I was posting about Light The Night when Instagram suggested The Patient Story.
There is hope. Don’t give up. Stay fighting. Stay strong.




Inspired by Lena's story?
Share your story, too!
More DLBCL Stories
Jen N., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4B
Symptoms: Blood-tinged phlegm, whole-body itching, shortness of breath, lump near collarbone, night sweats, upper body swelling, rapid weight loss
Treatments: Chemotherapy, immunotherapy, lumbar puncture, autologous stem cell transplant
Jim Z., Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Sudden and severe head and neck swelling, purplish facial discoloration, bulging neck veins
Treatments: Surgery (resection and reconstruction of the superior vena cava), chemotherapy
Nolan W., T-Cell/Histiocyte-Rich Large B-Cell Lymphoma (T/HRBCL), Stage 4
Symptoms: Debilitating fatigue, flu-like symptoms without a fever, swollen lymph node under the left arm
Treatments: Chemotherapy (R-EPOCH & RICE), bone marrow transplant
Mike E., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Persistent, significant back pain
Treatments: Surgery, chemotherapy



