Susan’s Chronic Lymphocytic Leukemia (CLL) Story

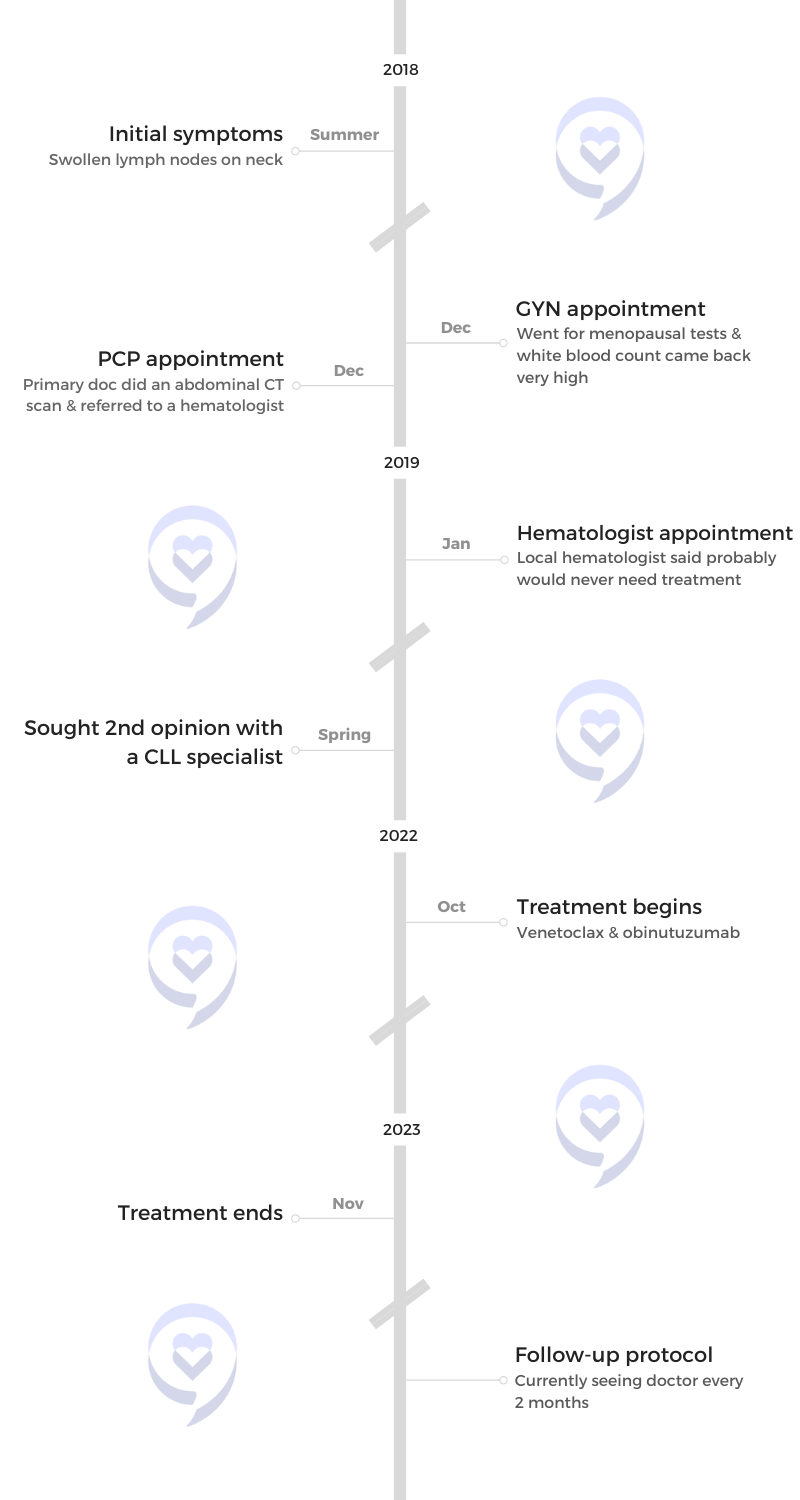
Susan was diagnosed with chronic lymphocytic leukemia (CLL) with 13q deletion in 2019. She noticed a lymph node on her neck one day and was initially brushed off as just having a virus or allergies.
A few months down the line, a closer look at her blood work revealed some significant irregularities in her numbers, which ultimately led to the CLL diagnosis.
She emphasizes how being an informed patient is so important. She knows how essential it was to understand her disease and have the knowledge. More importantly, she stresses how important it is to find a CLL specialist.
In addition to Susan’s narrative, The Patient Story offers a diverse collection of CLL stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Susan K.
- Diagnosis:
- Chronic Lymphocytic Leukemia (CLL)
- Initial Symptoms:
- Swollen lymph nodes on the neck
- High white blood count
- Treatment:
- Venetoclax & obinutuzumab
- Introduction
- Pre-diagnosis
- Diagnosis
- Treatment
- Discussing treatment options with the medical team
- Watch and wait
- Nearing treatment time
- Treatment getting pushed back due to infection
- Treatment plan
- Ramp-up dosing
- Side effects of venetoclax & obinutuzumab
- Follow-up scans & appointments
- Your medical team’s role in your care
- Importance of communication between your doctors
- The importance of seeing a CLL specialist
- Important CLL markers
- Reaching remission
- Hopeful for new CLL treatments
- Advocacy work
- Words of advice
Introduction
I live in the greater Boston area, about 25 miles north of Boston. I’m married with two children of my own and I have two step-kids. My daughter has a baby. My granddaughter’s three and a half. She’s the love of my life.
I’m the founder of a nonprofit. I used to be a social worker. I ran a program for low-income folks to help them out of poverty. I did that for 25 years. I was also a wardrobe stylist at the time. I put them together and started a nonprofit that empowers women through fashion and it’s called The Midlife Fashionista.
I’m also a style and beauty influencer for women over 50. I blog and I do my photos.
I’m still involved in Uncommon Threads so I have a pretty full life.
I also co-founded Kicking Cancer in Heels with Michele Nadeem-Baker, who I’m sure everyone knows.


Pre-diagnosis
Initial symptoms
I’ve been a very healthy person my whole life. I rarely got sick.
I did have some low-level fatigue for as long as I can remember. I never felt like I could keep up in sports. I always felt a little achy and tired. But other than that, no health issues.
In the summer of 2018, I was feeling the back of my neck and noticed a lump. I went to the walk-in center and they said, “You must be fighting a virus. A lot of people get swollen lymph nodes. It’s really nothing.”
It happened again. I noticed another one pop up. I went to my doctor and she said, “You probably have allergies.” I did so I didn’t think anything of it.
I went to my GYN for some menopause blood work. She called me and said, “Your white count is extremely high. You need to see your primary.”
I went to my primary right away and they were very concerned. They did CAT scans and ended up sending me to a hematologist. My numbers were not normal, my lymph nodes were not normal. That was the beginning.
It was really important for me to do the research and to see someone who lived and breathed CLL, who did the research, and who was developing some of the drugs and the trials. It was really important that I saw that top person who really knew everything about CLL.
Finding out about the abnormal blood tests results
There’s always a zillion questions that go through your mind. Is it cancer or is it something else? What’s going on with me? My brain always goes to the worst-case scenario. I was definitely afraid.
When I heard that I had CLL, I actually knew what it was. I have a very close friend who was diagnosed about 10 years prior. I had been through the journey with her and I knew what it was when I finally got my diagnosis.
Finding the right medical team
I started with a local hematologist. She was good, but I decided I wanted to be in Boston.
I ended up with a general hematologist who specialized in CLL at Massachusetts General Hospital and from there, I ended up at Dana-Farber with Dr. Matt Davids, who only sees patients with CLL.
It was really important for me to do the research and to see someone who lived and breathed CLL, who did the research, and who was developing some of the drugs and the trials. It was really important that I saw that top person who really knew everything about CLL.


The difference with seeing a CLL specialist
I started locally at an offshoot of Dana-Farber in my area, but it’s just not the same. They’re very good, but they’re just not as specialized.
Dana-Farber did far more tests than they did locally. They dug deeper. They looked more at the markers and the prognosis indicators. There’s a huge difference.
Finding out the results of the scans
It was crazy because I’d gone for the scans then my daughter and I were sent to Florida. We were the faces of the Soma Intimates Mother’s Day campaign.
I knew there was something really serious. I didn’t know exactly that it was cancer, but I had a feeling. It was really scary. It interfered with my having a good time down there. I was really trying my best, but in the back of my mind, I thought, I’ve got to get home. I’ve got to call specialists, I’ve got to get on this.
It was probably a month. I had that little bit of a delay for 3 or 4 days while I was away and I couldn’t really do anything. Then I ended up seeing somebody right after.
Diagnosis
Reaction to the diagnosis
I was diagnosed in January 2019. The doctor said, “You have CLL. It’s very rare. You probably have never heard of it.” I said, “Yes, I’ve heard of it. My friend has it.” I knew a lot about it.
My friend was doing very well at the time. She had gone a number of years without treatment. She was in watch and wait so it felt good knowing that she wasn’t in treatment and she was doing so well.
But I always thought it was so strange because how could you walk around with cancer and not be treated? How does that work? Isn’t that kind of scary and weird?
I also think that my great-aunt probably had CLL. She had long, chronic leukemia and ended up dying of a heart condition when she was in her late 70s. She was diagnosed with leukemia for a long time. I’m not sure exactly if it was CLL, but I have a really good suspicion it was just because it was so long and chronic.

Find your tribe. Find your family. It can be friends, can be neighbors. Find people who can support you.

Family processing the cancer diagnosis
They’re unbelievable. I have not one complaint. They have been so supportive, so incredible.
My husband comes with me to every appointment. My kids have done their research. They’ve looked up CLL. My son has come with me to appointments during COVID.
Everyone was so careful. They were living life extra protectively just for me, wearing masks everywhere.
Even now, they will tell me who they’ve been with, and what they’ve done, and let me make the decision if I think it’s safe for me to be with them without a mask. They just couldn’t have been better.
Whether you have a family locally or you don’t have a family that is supportive, find your tribe. Find your family. It can be friends, can be neighbors. Find people who can support you.
Treatment
Discussing treatment options with the medical team
Everybody reassured me that I may never even need treatment. My markers were really good. I was feeling good. I wasn’t getting chronic infections. They kind of instilled that message into me that it’s going to be a very long time. “You may not even need it. Many people don’t even need treatment.”
Unfortunately, my numbers rapidly increased. I started at around 20,000 or maybe a little bit more than that when I first got diagnosed. Five years later, I was at 347,000. My white count number was multiplying much faster than the doctors had expected.
We could see it over the years when they graphed it out. There was a pattern. It was going up pretty quickly. I would need treatment probably within five years and they were totally right. Totally accurate.


Watch and wait
In the beginning, I threw myself into seeing holistic doctors. I even went up to Montreal, Canada, to be seen by one of the world-renowned holistic doctors. I was determined I was going to beat it with a good diet, exercise, mindfulness, and everything that’s good for you.
It didn’t make any difference. I wasted an awful lot of money.
I’m not saying that it’s not a good thing to do because living healthy is good. But what I’ve learned is that for CLL, it’s a different beast. It’s blood cancer. It’s very different than solid tumors.
Everything that I was doing did nothing. I put a lot of time, a lot of energy, and a lot of money into trying all these different things that really weren’t effective.
At some point, I just said, “You know what? I’m just going to enjoy myself. I’m tired of saying, ‘I’m not going to have that piece of cake. I’m not eating any sugar or I’m not going to eat any meat.’” I did change and went more toward moderation.
Exercise is important. I do a lot of walking. I’ve tried to reduce stress. I’m a very anxious person and I carry stress in my stomach, my back, and my neck. I really tried to find ways whether it was taking a really brisk walk or sitting down to clear my mind and listening to some calming music just to ground myself and calm myself down.
Stress is really tough on our bodies. Forget not eating Twizzlers. I think trying to manage stress is probably even more important.
Watch and wait is a strange beast. You’re walking around with cancer not knowing if you’re getting treatment or not or if it’s tomorrow or next year.

Nearing treatment time
The last year before treatment, I was definitely starting to feel a little more fatigued. On certain days, it wasn’t holding me back from doing anything.
But about two months before I started treatment, I began to have daily fevers. At 3 o’clock, 4 o’clock in the afternoon, like clockwork, I would start to chill and my temp would go up to 100°F, 100.5°F. I’d take acetaminophen and within three hours, it was gone.
It was the weirdest thing. But that was an indicator that I was going to need treatment.
My numbers were climbing, my platelets were dropping, and my hemoglobin was dropping.
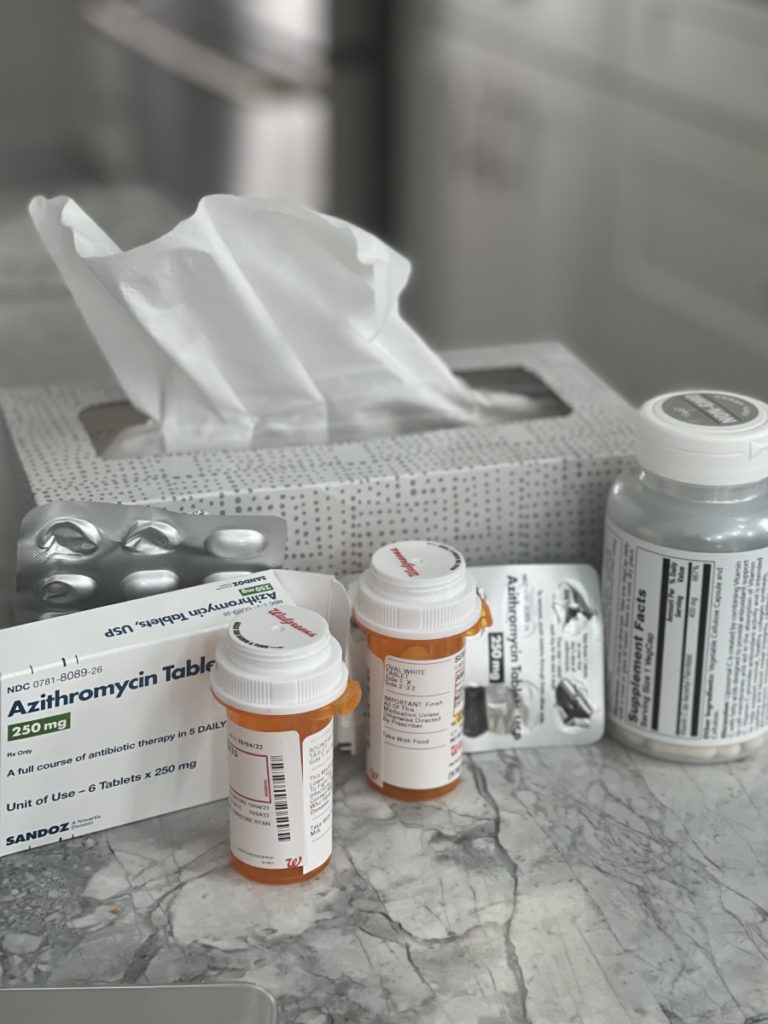
Treatment getting pushed back due to infection
The treatment was scheduled for September 2022. Right before treatment, I wanted to be with my family normally.
We had dinner on my daughter’s porch. I wore a mask and thought, Boy, I’m going to be extra careful and I’m going to wear my mask with everyone because COVID and getting sick is not a good thing if you’re going to start treatment.
Then I just said, “Oh, forget it. You know what? This is my last opportunity to kiss my granddaughter’s face and her neck and squish her tight,” so I did.
The next day, she came down with a bad cold. We all got it, but I got it worse, of course. I got a very bad sinus infection that lasted for a month. During that time, I was really sick. I needed to start in September, not October so it pushed things off a bit, which was unfortunate.

Treatment plan
Because of my markers, the doctors agreed that I should be on a fixed-duration treatment. I had already researched the options and talked to my doctor about the options. It was venetoclax and obinutuzumab.
However, at the point when I needed treatment, a new trial came out with one arm of venetoclax and obinutuzumab and I think the other arm was venetoclax and acalabrutinib. It was figuring out which is the best option through the trial.
But because I didn’t know which arm I was going to get and I had already made up my mind that I wanted venetoclax and obinutuzumab, that’s what I stuck with. And I think it was a good choice.
Ramp-up dosing
With this combination, you start with obinutuzumab, which is an infusion. Before the venetoclax was introduced, I think it was about a month.
For obinutuzumab, they start at a low level then they go up very slowly until they reach the full dose. It can take quite a while to get to your full dose. There’s a lot of hospital time involved.
I had to go home with an IV in my arm, come back the next day fighting 7 a.m. traffic for 2 1/2 hours, get blood work done, and then if you’re okay, you can be sent home.
They introduce venetoclax at some point then they do the same thing. You have to ramp up slowly.
I had to be in the hospital for a full day. Sometimes it was a 12-hour day. They do blood work. They give you the venetoclax and you can’t go home until they know you’re doing okay, you don’t have any severe reactions, and then they ramp that up.


Once you’re completely ramped up, it’s less time. For me, the worst thing was the fevers for sure. The other tough part of it was just so much time in the hospital, but, hey, a small price to pay.
Side effects of venetoclax & obinutuzumab
There was some fatigue that went along with that. The worst thing that happened to me was it killed off so many cancer cells all at once. I went from 347,000 white blood cells down to 4,000 in 48 hours. It was crazy.
I did have a reaction. I started with uncontrollable fevers every day where I was shaking, like convulsive fevers. I’ve never had anything like it in my life. They’d start at the end of the day.
When you have a fever and you’re on treatment, you absolutely need to be seen because you can be neutropenic, you can have all kinds of serious issues going on, and infection.
The medication worked too well. It was actually a good thing. Even though it’s so scary and it’s not what you want, this is good. Your body’s reacting. It’s killing off cancer cells.
Dana-Farber was closed. I would have to go to the ER. We went to the ER three or four times. It was really tough. You’re so worried about COVID.
On one of my visits, they really needed to keep me overnight, but the ER doctor talked to Dr. Davids and they both agreed it was actually too risky. My numbers were so bad that the risk of infection in a hospital was worse than just going home and coming to Dana-Farber the next morning for a shot of pegfilgrastim.
I got through that. That was a few weeks of hell, I won’t lie. But after that, I did really well.
They introduced the venetoclax and a lot of GI issues are associated with it. I had none.
My infusions ended in March and I’m on venetoclax till the end of November. Hopefully, I can be off of everything and go into remission.
The medication worked too well. It was actually a good thing. Even though it’s so scary and it’s not what you want, this is good. Your body’s reacting. It’s killing off cancer cells.


Follow-up scans & appointments
I go to Dana-Farber every two months for blood work. I don’t know if I’m in remission. I don’t know how long it will be. They haven’t told me yet — could be six months, could be four months.
I’m getting there. I’m seeing the light at the end of the tunnel. Two months is very manageable right now.
Your medical team’s role in your care
Right now, it’s just my CLL specialist. However, there are other cancers that are associated with CLL because it affects your immune system, which weakens your body, and melanoma is one of them so they have me see a specialized dermatologist who deals with cancer. She knows everything about CLL. She is incredible. I’ve got this other set of eyes watching skin changes.
There are skin reactions that a lot of patients get on some of these medications. One of my friends had a reaction. Her local dermatologist thought it was eczema or psoriasis or something and treated it. It was, in fact, the wrong treatment because it was related to the drug that she was on.
I’m really lucky. Forget two hours of traffic. I’m so lucky that I live near some of the best care in the world.
When you’re with someone who is a specialist, you get that top level of care. It’s really important.
Importance of communication between your doctors
Things like having your records sent over from other doctors and encouraging your doctor to speak with your team so that everyone is on the same page. Those are really important things.
Even when I have a mammogram, I have my results sent to Dana-Farber. I have them sent to my primary so that everybody is on the same page and everyone has all of the records and knows.
The importance of seeing a CLL specialist
My doctor’s in the labs. He’s working on trials and doing research. When you’re with someone who is a specialist, you get that top level of care. It’s really important.


Important CLL markers
These markers are prognostic indicators, kind of a roadmap of what your disease might look like. What types of treatment might be more effective? If you’re at higher risk, then they would like to see. It’s really an assessment.
Thank goodness we have these tests available because they really help the doctors navigate. I have 13q deletion. No one wants to have any markers, but it’s not the worst one to have. I’m mutated, which is a very good thing.
Then I have something which is very unknown. In CLL, they look for NOTCH1, which is a very bad marker. You don’t want to have NOTCH1. I have it, but it’s not specific to my cancer cells.
The doctors said, “Don’t worry about it. Think about it as a weed. You pull it out. You don’t know if it’s a good weed. You don’t know if it’s a bad weed. It’s so rare. We really have no idea. But don’t lose sleep over it because we just don’t know.”
The markers have been really important for me as my treatment plan is being put into place. They were able to figure out what the best course of action was for me.
Reaching remission
They know it’s working. My numbers are really good. I won’t know until probably late November if I’m in full remission, which would be amazing.
If I am, I’ll be going off of everything and I’ll hopefully be good for five-plus years. That’s what the research is showing. There’s an 85% chance of that, which is good.
Even though I’m 61, I’m considered younger so I think that’s in my favor, too. I don’t have other conditions, which is a good thing.
If there are some cancer cells left, then I still will go off of the treatment, but it will be more like going back to watch and wait again. I’ll be monitored more closely. I’m shooting for remission.


Hopeful for new CLL treatments
There are so many trials going on. There’s so much research going on. There are new drugs coming through all the time.
My doctors basically said, “Let’s get you into a long remission. Who knows, right? By then there could be a cure. We don’t know.”
I’m very hopeful. We’ve made huge breakthroughs in cancer treatments and research. I’m not going to be a glass half-empty. I’m going to be a glass half-full.
Advocacy work
Michele Nadeem-Baker and I met virtually during COVID. I joined a support group that she was running. I learned she lives 30 miles from me and she’s my age. It was amazing to find someone younger to connect with.
We put our heads together. The first thing we did was start a virtual support group called CLL Women Strong for women who are living full lives with CLL. We have an incredible group of women from all over the country.
We want to take things a step further and tap into her background in communications and journalism and my background in social work, fashion, and beauty. We put it all together and started Kicking Cancer in Heels, which is an online community for women who are impacted by all kinds of cancer to bring hope, inspiration, and resources.
We do interviews and Instagram Lives on everything from women who have started businesses during their cancer journey to makeup tips and a little bit of fashion to stress management. We share some stories, too.
It’s become this incredible community. We offer it to everyone, whether you have cancer or not, but also to people who might have someone in their lives, a woman in their lives with cancer. It’s really all-encompassing.


Words of advice
Do your research. Find a really good doctor. If you can’t find a CLL specialist in your area, find a top hematologist who works with a lot of CLL patients. Ask that hematologist: out of your practice, what percentage of patients are CLL?
Find your community. Write down your questions, be your own advocate, and be knowledgeable. Knowledge is power.
Some of our support group members actually come to Boston once a year from out of state so they can get another opinion and speak to one of the top CLL specialists. If there’s a large city around you with a specialist, perhaps it is worth driving to once a year and just doing virtual appointments in between.
Have your doctors communicate. I can’t recommend enough finding a specialist so if you can’t find one, at least connect with one. Have them on board for you.
Being careful, especially during COVID
It’s tough. The world has gone on. Everyone’s sick of COVID. Unfortunately, COVID is still around. It’s not sick of us.
It does present challenges for the immunocompromised population like me. I have opened up my life a little bit. I’ll do outdoor dining. I’ll see friends outside.
We had a gala for Uncommon Threads. I haven’t been to our gala in years. This is the program I started so it’s really important for me to be there.
I took a chance and went, much to my doctor’s dismay. He was not happy with me, but I wore a good mask. I had to take it off when I spoke. I was determined that people were not going to hug me. But of course, everybody hugged me. I just said, “You know what? It is what it is. Hopefully, I’m going to be okay.”
There are so many challenges, even in hospitals. Dana-Farber just removed the mask mandate. A friend of mine who was in treatment at Dana-Farber before COVID says no one wore masks. That was the way it was. That was normal.
I will wear a mask when I’m in a store, in a crowd, and in a hospital. Hopefully, it’s protective. That’s all I can hope for. It’s not just for COVID. It’s for RSV, flu, everything.


I flew to Florida right at the very beginning when we heard that COVID was probably coming our way. I flew down and we didn’t have masks. We were so busy wiping the seats down with disinfectant, which did nothing because it was airborne.
I was very lucky. All of us were very lucky that we came back without getting sick because as soon as we got back, all hell broke loose. It was all over the news.
I’ve been lucky I’ve not had COVID yet and I hope to keep it that way, but the odds are not in my favor. Most people have had it already.
During treatment, I can’t get another vaccine so I haven’t been boosted. It’s not going to do anything for me during treatment so my doctor said, “Don’t even bother. It’s just not going to be effective. You might as well just not have it right now.” I have to walk around like I’m unprotected.
Tips on finding the right specialist
There are so many good websites out there. CLL Society gives a list of doctors who specialize in CLL. Do your research. It’s really important.
To me, it was crucial that I was with someone who was an expert in the field who wasn’t dealing with 20 other blood cancers but only focused on CLL. Everyone’s different, of course, but it was very important to me.
Get on Google. It’s a wonderful thing. It can be a bad thing, too, but there is a lot of information out there.
Get a second opinion. I feel like it gives you a point of comparison. Interview your doctors. Find out who you’re most comfortable with, who really has the knowledge and expertise that aligns with your disease.
If you can’t do that, if you don’t have a specialist in your area, then do telehealth. If you even have to travel and you can travel, visit a specialist so that you get that other opinion. It’s so important.

Take down notes
I use the Notes app on my phone. When I think of a question, I write it down so it’s a running list. So many times you think of a question then you forget it later.
As you go through your cancer journey, keep jotting down those questions so that when you do go to the doctor, you have them readily available.
Some people keep a notebook. That’s fine, too. I find my phone is just the easiest for me. I can check them off as I get them answered and put the answers there.
Keep yourself informed
There are so many questions that are important to ask your doctor. You want to know about drugs. You want to know about interactions. You want to know about treatment options. You want to know about watch and wait and what that means.
How should I be living right now? Are there activities that I should be avoiding, foods that I should be avoiding, or foods that I should be eating? You could have a list of 100 questions, which I did.
I actually went to many cancer websites and got some really, really good lists of questions then I added to it. The more informed you are, the more research you do, the more knowledgeable you are, then the more powerful you are as your own advocate.
Being your own advocate is so important. You can catch mistakes, too. Doctors are human. Medical staff are human. Mistakes do happen. Sometimes, you might catch something just because you know what that term means what that blood test means, or what that medication interaction is. Do your homework.
When you’re diagnosed with any kind of cancer, let yourself feel. You are not going crazy with this tsunami of feelings. It’s just all these feelings rushing in. You’re angry, you’re mad, you’re sad, you’re grieving, you’re questioning. Did I do something to cause this? Let yourself feel, but don’t stay stuck in it because it is not going to be helpful to rehash all the stuff all over again.
Don’t let cancer run your life. I have cancer. I am not cancer. It is not my identity and I can still be happy and live a full life with cancer. It’s really important. I think it can be depressing to know that you have something very serious.


Don’t get stuck in the cancer diagnosis
I have to push myself. To be honest, I can get really stuck in it. My husband calls me a glass half-empty and sometimes I can be so I really have to work hard.
Self-talk is so important. Do things that make you happy. Exercise. Be with your community whether it’s over Zoom or it’s in person.
It’s so important to have friends and family who are supportive of you. Keep them close and tap into your resources. You really want to have that person to call when you’re feeling lousy and have them talk you off the cliff.
Live your life
Don’t let cancer run your life. Understand your disease, but live, too.
Even though I couldn’t go to big weddings or big parties, we found ways to have fun and bring joy to our lives. My husband’s a trooper because he’s doing the same thing that I’m doing to protect myself.
We recently went to Vermont. My daughter has a vacation house there. We invited friends. Four days before, they were really careful. They wore masks everywhere. Everyone tested prior. We ate outdoors and we had a blast.
Get creative and try to find ways to bring joy to your life and happiness because life is short for all of us. No one knows what the next five seconds are going to bring so just live your life and enjoy your life.
The more we connect, the less alone we feel. It’s really important.


Inspired by Susan's story?
Share your story, too!
More CLL Stories
Serena V., Chronic Lymphocytic Leukemia (CLL)
Symptoms: Night sweats, extreme fatigue, severe leg cramps, ovarian cramps, appearance of knots on body, hormonal acne
Treatment: Surgery (lymphadenectomy)
Margie H., Chronic Lymphocytic Leukemia
Symptoms: Large lymph node in her neck, fatigue as the disease progressed
Treatment: Targeted therapy
Nicole B., Chronic Lymphocytic Leukemia
Symptoms: Extreme fatigue, night sweats, lumps on neck, rash, shortness of breath
Treatments: BCL-2 inhibitor, monoclonal antibody
Symptoms of CLL
Learn about how some of the common CLL symptoms first present themselves from patients who have been diagnosed with CLL.



