Kelly’s Stage 3 Colon Cancer Story
Kelly, a small-town entrepreneur from Illinois, received a life-altering diagnosis of stage 3 colon cancer shortly after celebrating her 50th birthday. Despite her active lifestyle of flipping houses, running a tumbling gym, and being an avid runner, Kelly noticed concerning symptoms such as blood in her stool. Despite initial dismissals by her primary doctor, Kelly persisted in seeking answers, ultimately leading to a diagnosis of a sigmoid colon tumor.
Her journey took an unexpected turn during surgery when complications arose, prolonging her hospital stay. Despite setbacks, Kelly’s determination to advocate for herself remained unwavering. She navigated through treatment options, including chemotherapy, with a strong sense of autonomy. Kelly’s decision to undergo chemotherapy was not without doubts, but her resilience and determination prevailed as she faced the challenges of treatment.
Chemo has proven to be a daunting experience, marked by side effects. However, Kelly’s perspective on life underwent a profound shift. Embracing each day with a newfound appreciation and a sense of urgency, she encourages others to live without regrets and prioritize self-care.

- Name: Kelly B.
- Diagnosis (DX):
- Colon Cancer
- Staging:
- Stage 3
- Symptoms:
- Blood in stool
- Cramping
- Bloating
- Treatments:
- Surgery
- Chemotherapy
- 12 rounds
Cancer or no cancer, you’ve got a life to live.
Kelly B.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms
Tell us about yourself
My name is Kelly. I’m from a small town in Illinois of about 800 people. I was diagnosed with stage 3 colon cancer on November 1st. I wasn’t expecting that from my 50th birthday.

I own two self-employed businesses. I started flipping houses 5 years ago – I’m on [house] number 9. It was a hobby and it turned into an obsession. I absolutely love buying old houses and turning them into something brand new. Picking colors, flooring, and all that stuff. I’m the tear out girl, so I do most of the construction work pulling things out myself, such as drywall, cabinets, you name it, I’ve done it. I can do everything but electrical.
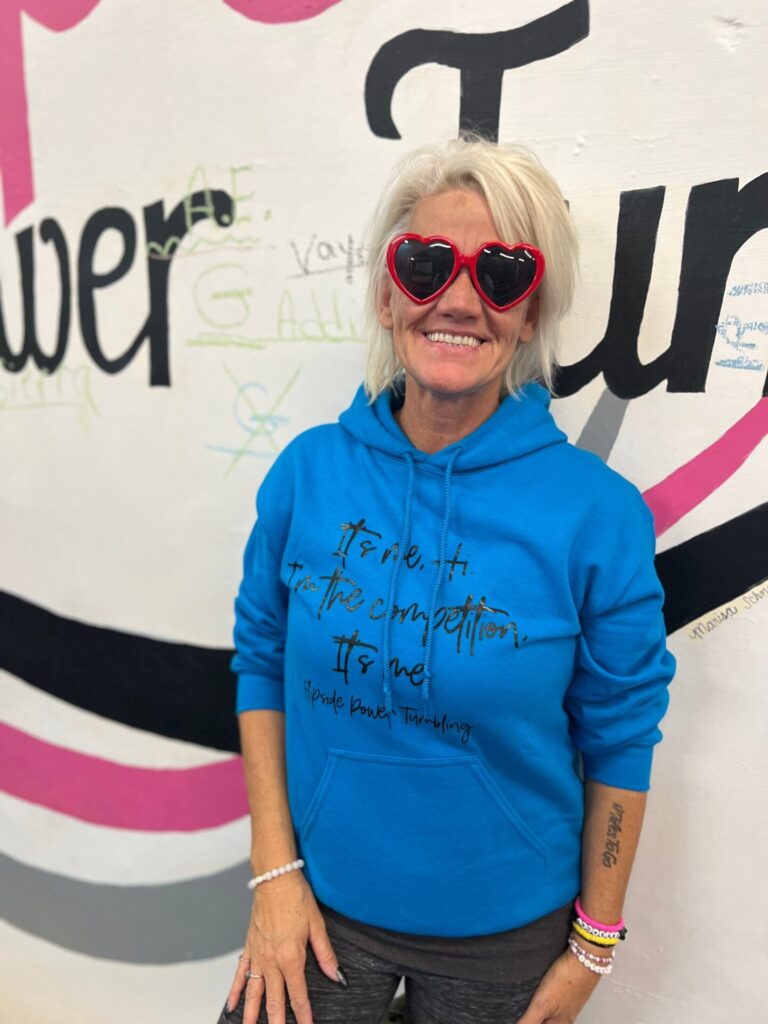
I also own a tumbling gym with a hundred athletes, and we compete competitively throughout the state of Illinois. We attend nationals once a year. Sometimes we go to West Virginia or to Florida. It depends on where we’re at that year. I have since taken a leave of absence from both jobs due to the diagnosis.
My hobbies are running. I love to run. I ran the marathon and half marathons. I’ve been running consistently for years. I journal a lot, even prior to the diagnosis. I was just settling into accepting the empty nest thing after my son went off to college 3 years ago, and getting into a groove. I love to travel to Florida. I’ve been back and forth to Florida 6 or 7 times in the last year, and that’s actually when I started seeing signs that something wasn’t right, in June.
What were your initial symptoms?
My first symptoms were that I had blood in my stool. I was actually in Florida in June, celebrating my 50th birthday with all of my kids, and I chalked it up to something that I ate. Maybe it wasn’t blood. I talked myself out of it thinking it was something that I ate or I was drinking red ice drinks a lot.
It continually kept happening and it seemed to happen more when I was in Florida, which I thought was strange. I didn’t have anything other than blood in my stool, which I knew wasn’t normal. I thought it could be anything, really. I didn’t think for a second that it was colon cancer.
I associated cancer with low energy, losing weight, and just not feeling well. I felt really good…Doctors kept telling me I was fine.
»MORE: Colon & Rectal Cancer Symptoms
I came home from my trip, scheduled an appointment with my primary doctor, and saw them at the end of June. They told me that they thought it was hemorrhoids and I shouldn’t be too worried about it. I again saw them because it continually happened probably 2 or 3 times a week.
I wasn’t losing any weight, so I really wasn’t that concerned but I was concerned enough to continue to call my primary doctor. I saw them again in July. I wanted blood work to see where my levels were at. My dad died of a brain tumor at the age of 56, so I went in for cancer screenings once a year, but nothing came up.
What did blood work show?
I had blood work done. My NPV level was the only thing that was flagged as low. I think it was at a 7 and they were not concerned about that at all. I took that and decided I’ll just keep coming back until somebody gives me some answers.

I went back 2 times in July and 2 times in August. They finally sent me to a specialist in October – a gastro specialist. He saw me and he said he would schedule me for a colonoscopy, but told me not to be worried. I did, at that point, start to have some cramping in my stomach and maybe a little bit of bloating. Again, I just turned 50 in August, so I thought maybe it was menopause. Maybe I was just getting old.
Did you suspect you had cancer?
I associated cancer with low energy, losing weight, and just not feeling well. I felt really good, even though I was continually having blood in my stool and a little cramping. Doctors kept telling me I was fine. I finally did go see the specialist and he said it was all good.
Diagnosis
Receiving a colonoscopy
I’d never gotten the call back to go get a colonoscopy. Here I am 3 months later after being diagnosed with stage 3 colon cancer. That was frustrating because nobody would take me seriously until I went and got another opinion. She scheduled me for CAT scans of everything from the waist up to rule that out, then the waist down.
They found a large mass in my colon so they set me up for a colonoscopy. I did the colonoscopy prep on my favorite holiday, Halloween, which is awful. The prep didn’t go well for me because I’m a puker. I was not really pooping like I was supposed to. I was throwing up.
We did the colonoscopy on November 1st, and the doctor came in after I woke up, they took us to a little room, so I figured it was not good news. He said it was 100% cancer.

How did you react to your diagnosis?
I’ve been going to the same doctor for years. It’s not like I didn’t trust them, but I had to trust myself more, and I knew something wasn’t right.
I said, “Okay, let’s go to Applebee’s. I’m hungry.” My daughter was devastated. I thought, okay, we’ll just deal with it however we need to deal with it. That’s it. I wasn’t feeling heard. I knew something was wrong. I didn’t know what was wrong. I’m pretty good at being able to tell what’s going on with my body. I’m very in tune with my body, my feelings, my thoughts. I felt like I was being dismissed.
They kept telling me over and over again, “It could be hemorrhoids.” I said, “It’s not hemorrhoids. I’ve never had hemorrhoids in my entire life. Even when I gave birth to 3 children who are now adults.” I knew it wasn’t hemorrhoids. I started to get a little bloated towards the end of October, but again, I chalked it up to menopause. I almost talked myself out of my symptoms because nobody would listen to what I had to say, and I’ve been going to the same doctor for years. It’s not like I didn’t trust them, but I had to trust myself more, and I knew something wasn’t right.

»MORE: Reacting to a Cancer Diagnosis
He said that the tumor was so large that they could not get the camera through on my colonoscopy, even though they changed the camera to a NICU baby size. The mass was too big. I didn’t really understand that because I’m a tiny girl. If I had such a large mass, how could I have not known that? The mass ended up being 11 inches big.
Creating a cancer care plan
When he told me I had cancer, I said, “Okay. Let’s go. What do I do now?” He was urgent, and said, “We need to go now. You need to see a surgeon. You need to schedule this and that.” I was clearly not in a hurry because I’d been dealing with this for months, so I was like, let’s just take our time here, people.
But that’s not how it works when you’re diagnosed with cancer. That was the crazy thing. They said I could have had the tumor for 5 to 8 years. Dr. Kerry was the first one to actually listen to me, listen to my symptoms, and want to rule anything out. She suggested the CAT scans. Of course, I went along with that because I wanted to know what was going on.
After I was told it was 100% cancer and it was time to see the surgeon, they scheduled me in. I went to see him the first week of November. He wasn’t too concerned about getting me in for surgery right away because the tumor was so slow growing that I could have had it for, he said, 5 to 10 years.
Did you have a family history of colorectal cancer?
They assured me that I didn’t do anything wrong because nobody would get me a colonoscopy. I didn’t have any family history of this. It sounds silly, but my friends and I made a pact to get colonoscopies at some point because my best friend’s husband died of colon cancer. So that makes the story a little bit crazier.
Surgery

Not rushing to get surgery
After I saw Dr. Kerry, things moved really quickly. I met with my surgeon, Dr. Modi, who is phenomenal. He’s like a little Doogie Howser and he didn’t push me to go too soon. He gave me a couple of weeks. He told me to go live my life. He knew the tumor was rather large, but he was very confident that he would get it out with the robotic arm hands. Surgery would take about 3 hours, so he gave me 2 weeks to go do whatever I wanted to do.
I really wanted to travel. My kids wouldn’t let me do anything. They were scared it might rupture. I teach gymnastics too, so I went back to work and did my thing.
Describe your surgery
I went in for surgery on November 21st, and that’s when things got really real, because the surgery didn’t go the way I expected it to go. I thought for some reason it was like going to the spa. I packed books and things like I was going to recover fast, and it didn’t happen that way.
My tumor was in the sigmoid colon. Surgery was my only option to get the tumor out. There was not going to be any radiation or chemo at that time. They’d remove the tumor and then we would go from there. We didn’t expect the tumor to be 11 inches, and it was in my sigmoid colon. I had also told my surgeon that I did not want the poop bag. I didn’t even know the correct terms for that. There were certain things I was not going to do, and I guess I wasn’t a really great patient, but I advocated for myself.
Complications during surgery
He ended up taking my colon out of my body, setting it on the table, fixing it, and putting it back in.

We went in for surgery on November 21st. It was supposed to last 3 hours. Apparently it lasted 7, because my prep didn’t go well. When he had me on the table, it was supposed to be laparoscopic, robotic, for incisions to get the tumor out, but he ended up having to open me up because I started to fill up with poop.
He ended up taking my colon out of my body, setting it on the table, fixing it, and putting it back in. The strange thing is, I remember going in at 7:30 in the morning and I had no doubt it was going to go very easy. When I came out of it and I started to wake up, there were so many people in the room and it was dark outside. I knew something wasn’t right and that it didn’t go as well as he had expected it to go. He ended up having to call in a colleague to help him with all of the feces.
When I woke up, I wasn’t too happy because I had the incision, but I didn’t have the poop bag. I didn’t have to worry about that because there was a certain way I was going to live my life after this, and it wasn’t going to be with that. No disrespect to the people who have [a colostomy bag]. I just knew that it was not going to work for me. I didn’t want that. I wanted choices. If I had to make that choice, it was a no.
Hospital Stay
How was your hospital stay?
In the hospital, things did not go well. We thought that I had an infection or a leak where the incision was and in my colon. I guess I didn’t. In the hospital, I don’t remember a ton.
He went to have an anastomosis. Putting my colon back together, filling everything around me with water to see if there were any leaks. My surgeon was convinced there were leaks. I was convinced there were no leaks. I just didn’t feel like he gave my body enough time to recover. He wanted me to sign consent to open me back up to see if there were any leaks. I refused to sign the consent form. I knew that my body just needed more time, so he sent me down for CAT scans.
I will say this, when you are throwing up and you lose control of your bowels…I was puking and throwing up at the same time, it was the most humbling experience for me. I am trying to get on the CAT scan table and crawling over after surgery. It was like doing the army crawl to get on the table to do the CAT scan. That was my lowest moment in the hospital. I really felt like things were not going to go well. I probably did have an infection and that was just the way it was going to go, because I was not going to let them open me back up. I couldn’t do it. I wasn’t strong enough. I had accepted it.
»MORE: Types of Cancer Treatments



My kids were devastated, but I also knew that if I was just given a little bit more time, my body would come back a little bit. I have to trust my gut through this entire journey. Everybody’s got a lot of opinions, but I knew I didn’t want to go back under the knife. I wasn’t going to do it. It didn’t matter, life or death. I wasn’t going back under and got the CAT scan results back and there was no leak.
Leaving the hospital
I took more antibiotics and they took out the NG tube. For a couple of days, I thought they were just getting the infection out, so after my CAT scan came back normal, I said, “Get the NG tube out. I’m done with that.” It was triggering me to vomit a lot. That was the worst feeling in the world for me at that moment. Two days later, the doctor said, “If you can eat and drink a little bit, we’ll let you out of the hospital and you can go home.” That is what I did, miraculously.
I was technically only supposed to be in for 3 days and I ended up being in for 5. I was still on track because they said the most was 7 days. I really think they released me to get me out of there. I was not an easy patient to deal with. I’m stubborn. I kept telling them, “Give me more time, give me more time, and I’ll get out of here on my own accord.”
The importance of advocating for yourself
I think it’s super important to advocate for yourself. Cancer or not, you are the only person that’s in control of your own feelings and yourself. You know your body. If you know something’s not right, it’s not right. I just cannot stress that enough to people. If you think something’s not right, it’s not right. Keep looking for people until you find a physician that will listen to you. You’ll eventually get there.

I was lucky it only took me a few times, but it took me a span of 6 months to know something wasn’t right and then to be diagnosed with stage 3 colon cancer. It was unbelievable. When they diagnose you with cancer, it goes boom. I didn’t want a stage 3 diagnosis. I wanted a stage 2, but one of my lymph nodes out of 32 came back positive for cancer cells.
I think it’s super important to advocate for yourself. Cancer or not.
»MORE: How To Be A Cancer Patient Advocate
Just keep pushing. Push for yourself. After I was released from the hospital, I had some time to look for an oncologist. Unfortunately, I live in an area where there’s not a lot. There’s not a lot that specialize in colon cancer. I was determined to find at least 3 different people so I could figure out what the best course of action was for me. I don’t follow everybody else’s rules. I don’t. I do what I want when I want to. I’m extremely independent and stubborn, and it’s not a one size fits all.
What did doctors recommend next for treatment?
I wasn’t a candidate for radiation. The first oncologist that I saw was actually pretty fantastic. He recommended chemo 6 times over a 3 month period, but he was more nonchalant about it. Do it or don’t do it. It didn’t really matter to him. I wasn’t comfortable with chemo at first and I said I’d get back to him.
I went to my second opinion, which was the University of Iowa Cancer Care Clinic in Iowa City, and I met with an amazing doctor, Naomi Fei, and she sat me down and said, “You need to do chemo,” and also backed it up. My surgeon was really hell bent on me doing chemo as well because I said, “I don’t think I’m going to do it.” He said, “If it were my mother, daughter, sister, or family member, I would want them to do chemo.” My second opinion at Iowa City said that it’s like an insurance policy. It’s preventative care.

My surgeon got all the cancer. It had not metastasized to any of my other organs, thank God, for as long as they think that I had it. She recommended 12 rounds of chemo for 6 months. I didn’t want to hear that. I had told my children – like I said, they are adults – that if my scans were clear and it had not metastasized and my bloodwork looked good, I was just going to live my life. They gave me maybe 5 years, and I was okay with that. I just turned 50, I could do another 20, but I just wasn’t comfortable with the chemo.
Chemotherapy
Did you decide to still do chemo?
I came home from Iowa City. I had a third opinion but I canceled that appointment. I sat by myself for hours and hours. I don’t know how you guys feel about Jesus, but he talked to me. I’d already told my kids, I’m not doing it now. I’m gonna live my life, sell my house, and move to Florida. Then, this is going to sound crazy, but I made friends with my ceiling fan. When you’re down, you spend a lot of time in your bedroom. You spend a lot of time by yourself.
I had a lot of conversations with myself, took a lot of funny notes in the middle of the night when I couldn’t sleep. I decided, plot twist, that I would do 12 rounds of chemo for 6 months. I just finished up with my second round a couple of weeks ago. I called my kids and I said, “I will do chemo. I will get through as much of it as I can.”
It still didn’t register with me that I had cancer up until just a few weeks ago. I hadn’t processed it yet. I didn’t feel sorry for myself. I’ve yet to really cry or get upset. I’m not angry. I really feel like I would be doing a disservice if I didn’t take the chance and do the chemo to live a little bit longer, because there’s many people that didn’t get the chance to do the chemo. My best friend’s husband, like I said, died of colon cancer 31 days after diagnosis. I couldn’t imagine at least trying to get more time. Of course, my kids were elated when I agreed to do the chemo.
Describe your experience with chemo
I’m going to tell you that chemo is not nice. I went in and got my port with my surgeon and I’ve seen him since then. He wants me to keep my port in longer than I expected – a few months after I get done with chemo.

Unfortunately, my third round of chemo was supposed to be last Friday, and we had to cancel because my white blood count was down by 140 points. That might have been the first time that I cried because I just wanted chemo. I just wanted to keep marking off the numbers and be done. I have no control over this, and I’m a woman that has control issues, a little bit of OCD, and a whole lot of ADHD. I’m a planner and I was devastated because my body said, “Not right now.”
Colon cancer chemo is not what people expect. I go in for my chemo and sit in an infusion chair for 4 hours. At first, it was a little terrifying. It’s really just sitting still for 3 or 4 hours. I didn’t like that at all. Being hooked up and watching the poison drain into my body, I didn’t like it. I’ve acclimated and I’ve had 2 treatments. I go in and infuse for 4 hours and then I have to go home with a chemo pump bag for 46 more hours.
When I tell people that they don’t really get it, I didn’t either. It’s for this certain type of cancer. You go home, you pump for 46 hours, and then you disconnect. We’ve decided to disconnect the needle from the port at home, which is going very well.
Have you had side effects on chemo?
The side effects of chemo…I might as well be pregnant. I’m very sensitive to smells and things anyway. With the chemo, I probably threw up at least 25 times, but I also don’t like to take my meds. I’m not a pill taker. I’m a self-care, “I’ll just deal with it.” Even if I’m sick, I just want to deal with it and mask it. Chemo had other plans for me. We tried to mask the nauseous feeling as much as we could.

The first treatment didn’t go well. The second treatment, I did do all of my meds, but I still probably vomited about 10 times. My energy level was hard for me to get back to normal. I pump for 3 days and then I have 4 days of feeling miserable. It’s really one week of total hell. I start to get better the next week, but it’s every 2 weeks. By the time I get to the good stuff, I have to go back into the chemo chair.
Like I said, my third infusion was canceled and I go back in for blood work on Tuesday. Hopefully I’ll be back in the chemo chair on Wednesday. People are like, “You’re the only person that cried because they couldn’t get their chemo,” but I just want to be done with it. There’s a lot more to do.
Reflections
Has cancer changed your outlook on life?

I’ve always had a different outlook on life. I felt like, prior to the cancer diagnosis, you really don’t know how much time you have left, you don’t know what’s coming. You don’t know what’s in store for you. I lived my life like that prior to cancer, but now my friends call me a little unhinged. I know I can’t just say I see things differently, but I literally see things differently. The colors to me are brighter. I don’t quite understand that. The sky is blue, the grass is greener, the snow is whiter. I just see things differently.
Happier? I can’t say that I’m happier with the cancer diagnosis, but I really think that God was trying to slow me down a notch, because I’m a workaholic. I own two businesses, gymnastics and flipping houses. I think this was his way of saying there’s more to life than just work. You need to calm down, and I have. I’m definitely unhinged. The hardest part about this cancer diagnosis is people telling me how I’m supposed to feel. That is extremely difficult for me.
I look at people differently. It’s not that my healthy friends are wasting their life by any means…But I’m not tired. Maybe during my chemo weeks, I’m tired and I take a few naps here and there, but if I’ve got some good time…Like yesterday, I painted the kitchen with my daughter. We just go get things done. There’s no excuses. Cancer or no cancer, you’ve got a life to live. Doesn’t matter how long it is. Go do it, people. Just go do it.
Do you have any advice for someone on their cancer journey?
My best advice would be, no regrets. If you’ve got things to say to people, say them. If you’ve got things to do, do them. Everybody always waits like they do have more time, and we don’t. Cancer or no cancer, like I said, go and live your best life.
Be selfish. I’m not a selfish person. I’m very empathetic. I do a lot of things for other people. I have my whole life, and now I’m like, if I don’t want to do it, I’m not going to do it. It’s okay to put yourself first, and that’s a lesson that took me a really long time to figure out. Without cancer, I don’t think I would have got that. I think I would have continued to do things for people, but I have to take care of myself. Saying no to doing things is so much easier than it was before.
Cancer or no cancer, you’ve got life to live.
With that being said, travel, take trips, don’t hesitate, and love people. Love yourself, love your family, and let go of some of the stupid shit that doesn’t matter anymore.
More Colorectal Cancer Stories
Monica D., Colorectal Cancer, Stage 1
Symptoms: None; caught at a routine colonoscopy
Treatment: Surgery (low anterior resection with temporary diverting ileostomy)
Edie H., Colorectal Cancer, Stage 3B
Symptom: Chronic constipation
Treatments: Chemotherapy, radiation, surgeries (lower anterior resection & temporary ileostomy)
Shayla L., Colorectal Cancer, Stage 4
Symptoms: Stomach sensitivity, food intolerances, exhaustion, blood in stool
Treatments: Chemotherapy, surgery (hepatectomy)
Tracy R., Colorectal Cancer, Stage 2B
Symptoms: Bloating and inflammation, heaviness in the rectum, intermittent rectal bleeding, fatigue
Treatments: Chemotherapy, radiation, surgery
Paula C., Colorectal Cancer, Stage 3
Symptoms: Painful gas, irregular bowel movements, blood in stool, anemia, severe pain, weight loss, fainting spells
Treatment: Surgery (tumor resection)
Nick S., Colorectal Cancer, Stage 4A
Symptoms: Change in bowel habits, size & consistency, blood in stool, abdominal pain, fatigue
Treatments: Surgery (sigmoid colectomy), chemotherapy (capecitabine, oxaliplatin), immunotherapy (bevacizumab, pembrolizumab)