Richard’s Stage 4 Relapsed DLBCL Non-Hodgkin’s Lymphoma Story
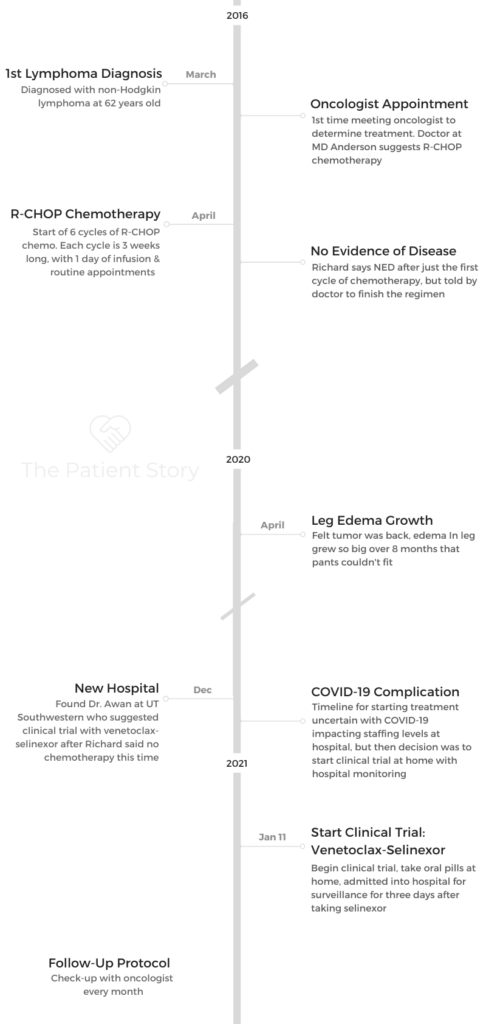
Richard shares his stage 4 diffuse large B-cell lymphoma (DLBCL) story and having to undergo treatment 2 different times after his cancer relapsed 5 years later.
After finding a new medical team, Richard decided to participate in a clinical trial testing venetoclax and selinexor to treat DLBCL.
Explore his story below to hear all about his experience with chemotherapy vs. the clinical trial, dealing with side effects and the support he needed to get through it all. Thank you for sharing your story, Richard!
- Name: Richard P.
- 1st Diagnosis (DX)
- Non-Hodgkin’s Lymphoma
- Age at DX: 62 years old
- 1st-Line Treatment
- R-CHOP chemotherapy
- 6 cycles
- 2nd DX
- 5 years later
- Relapsed/refractory non-Hodgkin’s lymphoma
- Diffuse large B-cell lymphoma (DLBCL)
- 1st Symptoms of Relapse
- Excessive swelling in leg
- 2nd-Line Treatment
- Clinical trial: venetoclax & selinexor

Richard’s Story on Video
- Richard's Story on Video
- 1st Diagnosis & Treatment
- The Relapse
- Describe the venetoclax-selinexor clinical trial
- What was the regimen?
- What interested you about the venetoclax-selinexor trial over other options?
- Describe the clinical trial regimen of venetoclax and selinexor
- How often do you take the selinexor?
- Describe the experience so far on the venetoclax and selinexor
- Describe any other side effects you dealt with
- Describe the difference between the chemotherapy and this clinical trial
- Chemo regimen's impact on family
- How are you monitored during the clinical trial?
- How was the progress of the venetoclax-selinexor trial?
- How does it feel to see so much progress made during this clinical trial?
- How long will you be on the venetoclax-selinexor?
- Managing your cancer like a chronic illness
- What turned you off about the CAR T process back in 2016?
- Clinical Trials & New Research
- How do you feel about participating in a clinical trial?
- Describe what it's like being in a clinical trial
- What convinced you to participate in the clinical trial?
- The doctor-patient relationship was key in deciding where to go for care
- Highlight the importance of the caregiver and the role that they play, these unsung heroes
- Why is it so important to find new treatments that might lead to better quality of life?
- The promise of new research
- What's your message to other patients about participating in clinical trials?
- What has helped you get through prolonged cancer treatment?
- How important is it for people to share that and for other people to listen to the stories?
Thanks to Karyopharm for its educational funding support of our program. The Patient Story retains full editorial control over all of published content.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
1st Diagnosis & Treatment
Tell us about yourself
It’s great to be part of this. I love to tell people what’s happening and how things are going with my clinical study and just life in general, and just get another friend out there.
I moved here from Chicago 42 years ago, and so I think I’m going to stay. I’m married. We have 2 children. They’re adults now. Elizabeth’s my business partner, and we have a tamale company.
Richie, my son, is into real estate. In fact, last year, he was cited the best property landlord for the homeless. He helps people transitioning back into society from wherever. He and his friends buy apartment buildings, and they cut them in half to make them dorm-room size and fill them up.
My wife just left the design business that she was in for years. I say she was set free! Now, she works with my daughter in the bodega we opened for the tamale company.
We had a catering kitchen, and catering dropped off the map. We had to do something. We opened up a bodega, which is like a corner store.

Describe how you processed the cancer diagnosis
I was like, ‘Okay. How did I get it? Where did it come from? How do I get rid of it?’
Those were the 3 things that entered my mind.
I thought, “I want to go to the MIT of cancer research.” I found out that that would be MD Anderson. That’s only 4 hours from here, from Dallas.
I would go down. I called them that day. “I need an appointment. I’ve got this and this.” They said, “Okay. Have all your records sent down here.” I sent my records down there. In 2 days, I had an appointment.
»MORE: Patients share how they processed a cancer diagnosis
Describe the treatment you underwent
That’s where we did the R-CHOP chemotherapy. After one round, there was no evidence of disease, no evidence of cancer. I thought, “That sounds good. The chemo knocked it out. Let’s go! I’m done.”
They said, “No. You’re going to have to do 5 or 6 more [cycles].” So I did. At the beginning, I was really health-conscious in my diet and exercising and trying to stay fit, but I really had to step it up now that I had a culprit in my body. It wanted residence.
What were the R-CHOP side effects?
It was hair loss and appetite loss. ‘It’s just lose, lose, lose all the way around me,’ I thought. That’s why I needed to get out of the chemotherapy. I wanted to stop.
My going total plant-based diet was a big aid to that. Total plant-based was just something else to get excited about. What can I do? What kind of mushrooms beat cancer?
No sugar. That was the first thing that went. No sugar, then dairy, then just total plant-based, and I was liking it. The new menus were interesting. It was exciting.
»MORE: Read other cancer patient experiences with chemotherapy

The Relapse
How did you know the cancer was back?
5 years later, it came back, and I knew right away what it was. The tumor came back.
I call it the ‘culprit’ because I don’t like to name it what it is. Because it’s not going to stick around.
Because the tumor came back, I had edema in my leg. I tried to self-treat for 7 or 8 months. I just upped the vegan thing and tried to do more exercise and massage and sound baths. I would do Reiki.
What made you seek cancer treatment?
My friend lives in Houston, but I’ll go down there and ride bikes. He just looked at my leg and said, “Oh, man, whatever you’re doing is not working fast enough. You need to have that looked at.”
I made the appointment to see Dr. [Farrukh] Awan. He just said, “Okay, you can continue what you’re doing, fine with me, or you can do this, or you can do this.” Then he said, “You know, there’s a non-chemo test I’d like you to take.”
I said that we have a tamale company. It was in the beginning of the tamale season, where it just goes berserk, so I just said, “How about January?”
He goes, “Yes, you’ll still have [the cancer] in January, I’ll still be here, and we can still do the same thing.”
COVID-19 slightly shifted the path forward
Then COVID was at its peak. He just said, “No, we can’t start now. We’ve got half the staff, people are getting sick. It’s taking twice as long to see just one patient because of all the work you have to do sterilizing everything.” He just goes, “No, you can’t start.”
Then 2 days later, called me up, said, ‘Hey, we can do this. We can do this as outpatient.’
Describe the venetoclax-selinexor clinical trial
What was the regimen?
I started with the selinexor and venetoclax. Then it caused nausea. My doctor kind of punched me in the arm, said, “Don’t be a cowboy. Take the [anti-nausea] medicine.”
He’s right. I take it so you don’t have the symptoms, but you’d still have that feeling in your stomach.
What interested you about the venetoclax-selinexor trial over other options?
My doctor said, “You can take it and go to work. Come in, and we’ll watch you the first few times you take it, the first few weeks, because in the beginning it’s a step up [in terms of dosage].”
You increase the amount, the dosage of each drug itself. Then they want to watch you in the hospital to see for the first 3 days after you take selinexor.
That’s typically about 2.5 days for when I still take it because I only take that [drug] once every 7 days.
Describe the clinical trial regimen of venetoclax and selinexor
Every day I take venetoclax. That’s 7 tablets. They’re about the size of your average vitamin C tablet. It can be mistaken for that, about the same color tint.
7 of those, and I just take them all at once. I take a bunch of water, make sure I can open my throat and just take all of them down. Also, an hour before that, they gave you some medicines to prevent nausea. I take those, set my alarm, then take the venetoclax after that.
Then there are also other drugs you have 2 hours before you go to sleep to prevent nausea from when you wake up, but I usually don’t take that. I’m asleep, and it doesn’t bother me. I don’t notice it when I wake up. It hasn’t been that intense with me.
Every day, 7 pills. Overall, including the venetoclax, I take probably 13. Then the other pills are very small, for nausea. Another is something to help my lungs, keep me breathing better. They include:
- venetoclax
- prochlorperazine/Compazine
- olanzapine
- loperamide
- ondansetron
- acyclovir (“twice a day, one in the morning and one in the evening”)
- allopurinol
- selinexor (“a tiny blue pill that’s packed full of energy”)
How often do you take the selinexor?
Once every 7 days. I think it’s 80 milligrams, which I think is 4 tablets.
Describe the experience so far on the venetoclax and selinexor
I’m going into my fifth cycle, which will be my fifth month. The first 3 weeks, they admitted me to the hospital for 3 days.
I loved it. [UT Southwestern] was a great, great hospital. I had a view in Dallas overlooking Love Field. The 22-foot windows, ceiling to floor windows. It’s during COVID, so nobody could come see me, not even the nurses. They didn’t want to come into the room, only if they had to take blood. Then they’d come in and out.
I got lots of work done, made lots of phone calls. I read a lot and got to watch a lot of planes land in Love Field at night. It was great.
The second [hospitalization], they said, “Well, you’re doing so well. We don’t think you need to do it the third time.” When you go in, they say, “Because you’re on Medicare, if you think you’re being [discharged] too early, if you want more time, you can protest that and you can stay.”
I did that the second time. They said 2 days; I got to stay 3. It was great. Nobody was around. I’m inside my own little resort. My wife used to love to see me go, too. “Oh, sorry to see you go!”
They have a full menu. You can order all from 6:30 in the morning until 7 o’clock at night. You can order anything you want, all day long. It was great.
The third time, the third week, they say, “Oh, you’re doing so well. We don’t think you need to go into the hospital.” When they [mentioned] Medicare, I said, I’m switching it around. I think I should be admitted. I’m using my Medicare rules, so let me in!
I guess they thought I was funny, so they let me go in one more weekend. I was the poster child for the selinexor.
Describe any other side effects you dealt with
Well, it is pretty invigorating. In fact, I was never a night owl, but now I am. It’s like I don’t require that much sleep, although I do sleep very well.
TPS: You’ve had the opposite of fatigue. You had somehow a lot of energy.
That’s right. That’s the only place I know it’s coming from, is the tablets I’m taking. That’s what I think.
Describe the difference between the chemotherapy and this clinical trial
It’s like night and day. The R-CHOP is torture. It’s not the disease that’ll kill you; it’s the treatment. At MD Anderson, it’s just massive acres and acres of zombies walking around. That’s what I saw.
You got to talk to people because they’re everywhere. They’re on every transportation around the area coming in. You can’t avoid it. You can’t avoid not addressing it. It’s like, “Hey, what are you in for? How did you end up here today?”
People are more than eager to tell you, kind of waiting for somebody to ask them.
It was a day of travel and a day of chemo. You need a day to rest before you travel again. That was never any fun.
It didn’t get better for a week. Then it got better, and then I’d say, “Oh no, I’ve got to go back. Here we go again.” But I was getting better. It was necessary for me to do that. That was the only thing I knew at that time.
Chemo regimen’s impact on family
If you don’t have support at home, you’re out of it. If your kids don’t want to eat that way or they don’t want to try new things, you’re cooking for yourself.
That’s no fun. I know just how much support [patients] need to do something as simple as changing what you eat.
How are you monitored during the clinical trial?
Every other week, I have blood work. Once a month, I see the doctor. I’ve had two PET scans, not crazy about that because that’s just all sugar, but it gives a great picture.

How was the progress of the venetoclax-selinexor trial?
I saw pictures of the intruder, the culprit (the cancer). When I started in January, it was like spreading into my kidneys and my whole lymph system. I saw [the tumor] in January.
It’s like a little tiny pea-size today. It’s gone. I felt that yesterday when I was having my PET scan. It’s just flat, nothing there.
No picture, no anything. It turned out great.
How does it feel to see so much progress made during this clinical trial?
This works. It’s gone. This worked or is working. I need to stay on this.
Every day, there are new studies coming out. I’ll do this for a while, keep it at bay, and then soon something will come up and say, “Here’s a clinical study. Take this pill one time, and you’re good.”
That’s what’s on the horizon. When I was first introduced to CAR T in 2016, it was just like, “I’m getting out of here. No way, you’re not doing that to me.”
My wife and I asked the physician’s assistant, who was telling us all about CAR T. It was just like, “No way, you’re going to do that to me.”
Now it’s come a long way, too. The next thing is right around the corner.
How long will you be on the venetoclax-selinexor?
In fact, today my doctor said, “Forever,” because of the type of lymphoma I have, the diffuse large B-cell, unless I do the CAR T. As Dr. Awan said today, “Or you get the next thing that’s right around the corner.”
It’s rapidly happening all the time. More and more studies have been approved.
Managing your cancer like a chronic illness
I’ve just got to do it. Do what you’ve gotta do. What’s next? I don’t want to get all caught up in that. I just said, “Yes, that’s fine. I got it. I know how to do it. Let’s go on. What’s next?”
If you have trouble, think of it as you’re a boy scout. You’re working for your badge, and you’re going to get it because everybody else has got a badge, so you want that banner with all the badges on.
I did talk to a patient. I don’t remember their name or anything, but they said that we live better than the Vanderbilts ever did or any of those people, the wealthiest of the wealthy people.
We live so much better than they did, because they didn’t have the same medical institutions that we have now. If they got a cold, they could catch pneumonia and die. Running water and bathrooms and all that.
We live better than the Vanderbilts ever did and the Rothschilds put together. It’s only getting better. It’s like, “What will they think of next?”
I’ve got more wealth than the Vanderbilts.
What turned you off about the CAR T process back in 2016?
Because you’re in the hospital and completely annihilate your immune system. You’ll be there for about 2 weeks. The last place I want to be is a hospital when you have no immune system. That’s where sick people are. It seemed so harsh.
Then if they ever take your T cells out, send them to “college,” and then we put them back in, and there’s still a chance for all this stuff [to happen].
My wife and I asked the physician’s assistant. We said, “If this was your daughter, would you give her this treatment?” He couldn’t look at us, so we just said, “See you.” That was our answer.

Clinical Trials & New Research
How do you feel about participating in a clinical trial?
We could be trendsetters. You’re part of this. When you beat cancer, how would you feel?
Yes, put me on the poster. We’re part of it. If you don’t think you can change the world, you’re doing it.
Describe what it’s like being in a clinical trial
Every day they ask for the time you take the medication, the dosage and any comments. I have my list right here that I was reading before that I know what to take. Then there are my alarms on my phones. There’s a difference between being in a clinical study [and the chemo].
It’s not like going through chemo when you’re out of commission for 2.5 weeks because of what you did to yourself 2.5 weeks ago, submitting yourself to chemotherapy.
[This time] I got my life back. Whether I had to take pills, I never thought I wanted to be the person who has the daily pill things all the time, that I keep them hidden and keep them in a sequence order that I take the pills.
I move them to one side of the cabinet because there’s so many of them. Like I said, there’s 13 different ones. When I take them, I move it to the other side of the cabinet so I don’t forget. Then the next time I see them, I’ll move them across.
I have my list in there and take it because the clinical study, when you’re taking the dosage at home, they really want documentation. They want a back up. Not like, “Did he take these?” “Yes. I think so.”
What convinced you to participate in the clinical trial?
Dr. Awan was really encouraging. He was just like, “You’re great. I support what you’re doing, but after tamale season when [the cancer] is still here, I’ll be right here, and we can start whenever you decide.”
That was the complete opposite from MD Anderson, where when I went down there, they were like, “We’ll get you started now.”
The doctor-patient relationship was key in deciding where to go for care
He’s a great guy. In fact, everybody on the staff is really good. They just talk to you, not as a patient. They just talk to you and tell you what’s going on.
They say, ‘Okay, here’s what it is. Things are looking really good. Do you have any concerns or questions?’
They tell you what’s coming up. When they started to increase my dosage every week, it got more intense on the nausea. I don’t want to play up that so much.
It’s there, and I don’t want to talk about it, because it’s not something to emphasize. You know ahead of time it’s going to be there. You take the pills, boom. It’s good.
I’d love to talk to somebody, some other patients, because mainly I have not ventured into going on the internet and finding out all about it. Finding out all this stuff, it’s like, “No, that’s not for me. I’m just going to keep on doing what I’m doing, live my life, selling tamales and forgetting about it.”
Highlight the importance of the caregiver and the role that they play, these unsung heroes
I have a caretaker, Debbie, who takes care of me. I can count on her because I can go off in the other direction pretty quick.
We [patients] just got [the cancer], but they have to orchestrate the whole thing. They’re taking care of you. They’re making sure you stay alive, that you eat.
My wife can make some gorgeous meal. I’m just like, “Oh, wow.” Then I just take one bite and just say, “I can’t. I just can’t.” She says, “That’s great. That’s fine. Just put it away.”
She helps me keep up with my friends because I don’t talk a whole lot about it, about my illness to my friends or actually anybody. I let my wife talk about it. If you need to know, she knows. It’s like, “Oh, how old am I? Oh, yes.” She keeps track of all that.

Why is it so important to find new treatments that might lead to better quality of life?
Just being able to move and feel good and get about, not be sequestered somewhere, it’s freedom.
I was just real fortunate to have my whole family behind me and actually caring more than I did sometimes when they make you do something.
Somebody would always take me to Houston [for chemo], either my daughter or my wife. That was a 2.5 day deal. The 4-hour car rides are always the best conversations.
[It’s manageable] if you’ve got the support. I stay out of it most of the time. [My wife] tells me what’s on MyChart. Of course, I keep up on my medication. My phone or my alarm goes off, and my phone throughout the day for different reasons.
The promise of new research
I’d like to encourage somebody to keep on going, because it does get better. I have [diffuse large B-cell lymphoma]. It’s not going to go away, but like I said, the next thing is right down the line.
CAR T would wipe it out forever. There’s an over-the-counter CAR T coming out, more or less over-the-counter. It’s simplified, which makes it a lot easier.
I was talking to my physician’s assistant. I bring in a record of what I take, what time I take it, how much of it I take and any comments. I had everything all filled out.
He’s like, “Wow, this is amazing. You have everything documented.” I said, “I was told to keep it documented.” He goes, “Yes. Some people have taken so many other medications for different things, that they’ll say like, ‘Oh, I forgot to take it this week.'”
It’s like, “Wow.” It has to be built into the system, I would think, like the dosage. I could not just forget, like, “Oh, I forgot to take those.”
What’s your message to other patients about participating in clinical trials?
The first thing I asked was what’s the success rate, and they’d tell you, realistically. Then I want to hear all the benefits. I don’t want to hear all the fine print, all the side effects.
The one big thing that we talked about: upset stomach. There was this, along with the other side effects. There could be more of a possibility to be struck by lightning. Who knows all those side effects.
Just go into it thinking you’re going to be cured. The [positivity] helped me. I can see myself at the end of this. Even now, there’s no evidence [of disease], but I still have a ways to go.
It never really leaves you, the idea of [the cancer] coming back, but that’s okay. I’ll deal with that.
What has helped you get through prolonged cancer treatment?
Know that there’s a god. You’ve got to find out for yourself. What better time than when you’re close to what you might think is the end of your life or something? What a better time to connect?
Have you ever heard of Wim Hof? He’ll change your life. He’s also known as the Ice Man, and he does breathing treatments. He’ll climb the Himalayas in his gym shorts. He’s an amazing guy, and he does these breathing techniques. You do a round of those in the morning, and you’re charged.
Meditation is very important because I’m alone a lot. You better like being with yourself, especially during all the quarantine we went through.
You have to want to be an introvert. You spend a lot of time alone, a lot of guided meditation. There’s some great ones on the internet. I use them all. I don’t want to commercialize this thing and name somebody’s name.
Meditation is great. Stay active. Stay physically active. Walk. Walking also jogs the brain. If you walk with somebody, it makes the job move quick, too.
How important is it for people to share that and for other people to listen to the stories?
It’s cleansing. It’s part of the healing. I’m talking to you; I made it this far. I’m going to tell you what else is going on. You learn a lot about yourself.
Maybe you put some limits on yourself that then when you hear yourself say it, you’re like, “Whew, did I say that? I guess I am like that.” It brings change. Change where you have to.
There’s encouragement everywhere. I just want to pass that on.
Inspired by Richard's story?
Share your story, too!
More Diffuse Large B-Cell Lymphoma Stories
Jen N., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4B
Symptoms: Blood-tinged phlegm, whole-body itching, shortness of breath, lump near collarbone, night sweats, upper body swelling, rapid weight loss
Treatments: Chemotherapy, immunotherapy, lumbar puncture, autologous stem cell transplant
Jim Z., Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Sudden and severe head and neck swelling, purplish facial discoloration, bulging neck veins
Treatments: Surgery (resection and reconstruction of the superior vena cava), chemotherapy
Nolan W., T-Cell/Histiocyte-Rich Large B-Cell Lymphoma (T/HRBCL), Stage 4
Symptoms: Debilitating fatigue, flu-like symptoms without a fever, swollen lymph node under the left arm
Treatments: Chemotherapy (R-EPOCH & RICE), bone marrow transplant
Mike E., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Persistent, significant back pain
Treatments: Surgery, chemotherapy



