Kelly’s Stage 3 Colorectal Cancer Story
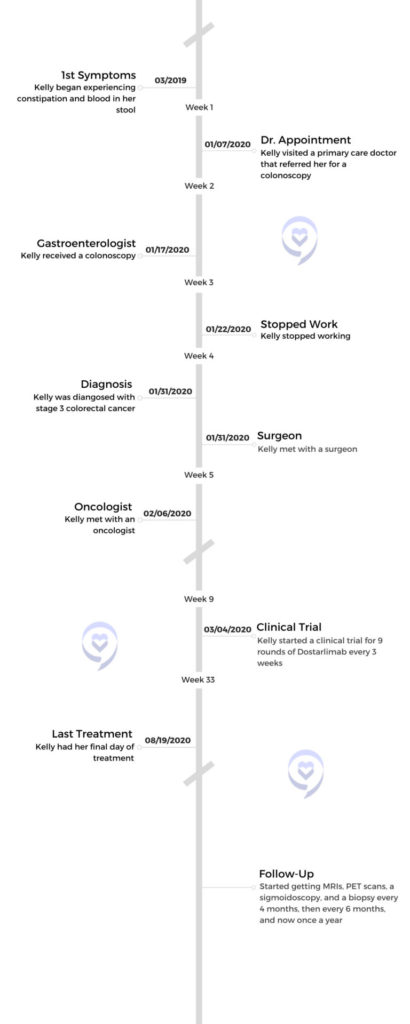
About to give birth to her first child, Kelly, and her doctors assumed her new digestive symptoms were related to her pregnancy. After having her son, Kelly’s symptoms of constipation, blood in her stool, fluctuating appetite, and weight loss worsened. Multiple doctors wrote it off as internal hemorrhoids, but Kelly continued to search for answers.
After several doctor visits, Kelly finally found a doctor who was willing to listen and ordered her a colonoscopy. It was at this colonoscopy she learned she had a tumor in her colon, beginning her journey with stage 3 colorectal cancer.
Kelly shares her story with us and how being 1 of 4 patients in a successful Dostarlimab clinical trial helped her avoid radiation and surgery, why it’s important to trust your gut, and her journey through preserving fertility. She is now cancer-free and has just given birth to a beautiful baby girl.

- Name: Kelly S.
- Diagnosis (DX):
- Colorectal cancer
- 1 cm from the anal opening
- Colorectal cancer
- Staging: 3
- Symptoms:
- Constipation
- Blood in stool
- Abnormal-smelling stool
- Fluctuating appetite
- Weight loss
- Treatment:
- Clinical trial
- 9 rounds of Dostarlimab
- Clinical trial
Give yourself grace. It’s the biggest thing. Everyone has different seasons in life. Whether it’s cancer or something else that you’re going through that’s traumatic, upsetting, or hard, give yourself grace.
Kelly S.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms
Tell us about yourself

My name is Kelly Spill. I now go by Kelly Bonito since I got married, but I like to go by Kelly Spill. I’m a mom, I’m a wife, and I am in network marketing because I want to be home with my kids as much as I can and spend time with them because I’ll never get that time back. I’m also a cancer survivor.
What were your first symptoms?
My symptoms began when I was 8 months pregnant with my son. I had no idea that they were symptoms of the cancer that I had. I thought that it was because I was giving birth in a month. As a new mom, I had no idea what my body was truly going through, what to expect, or anything like that. The doctors basically said the same thing. They were like, “You’re giving birth in a month. This is kind of what happens with your body. It’s nothing to worry about.” Looking back, that’s definitely where my symptoms began. Some constipation and blood in my stool.
Did you experience digestive issues like this before?
Nope, never. I told them and they just brushed it off.
Did your symptoms improve after having your son?
When you’re not feeling yourself, you keep telling someone you’re not feeling yourself, they’re hearing “new mom,” and they go right to internal hemorrhoids, you start to think that that’s what’s going on because you start to question yourself.
After I had my son, it was the same thing. It didn’t get better by any means and it didn’t necessarily get worse right away.
When I told them what was going on, they still said the same thing, “You just had a baby. Things are still a little bit out of whack. This is the way it goes. If it persists, give us a callback and let us know.” About a month and a half or so after my postpartum checkup I ended up calling them again. I went back and they gave me an exam and the doctor said, “I’m 99.9% positive you have internal hemorrhoids.” It caught me off guard because when I gave birth, I didn’t have any hemorrhoids at that point. But as a new mom, I really didn’t know much. I was like, maybe they disappeared.

He said, “If this persists, go see a primary doctor.” I said, okay, and it did. I wasn’t feeling right. I don’t really know what I was feeling but I just wasn’t feeling like me. I went to go see a doctor. She took my blood work and gave me an exam. She said, “I’m pretty sure you have internal hemorrhoids.” My blood work came back fine, so that was a little confusing.
When you’re not feeling yourself, you keep telling someone you’re not feeling yourself, they’re hearing “new mom,” and they go right to internal hemorrhoids, you start to think that that’s what’s going on because you start to question yourself.
»MORE: Signs of Medical Gaslighting as a Cancer Patient
Shifting focus away from health
Time went on a little bit. My husband and I were living in San Diego, California at the time and I was like, I’m just gonna put this aside a little bit. Let’s worry about our move. We have a newborn at home. Let me get back to the East Coast, closer to family, and hopefully, things will get better. I pushed my health aside for a few months.

Did you feel like you were being heard by your doctors?
As a new mom, I really just didn’t know anything. I don’t know a lot about the internal of the body and what’s going on when you have a baby. There’s a part of me that was like, okay, that makes sense. Then there’s another part of me that felt like something was wrong. I’m stuck in the middle, which made me think, let me just worry about what I have in front of me, and then I’ll get to that when I get to that.
Her symptoms worsened
My appetite went away…I weighed about 115 pounds at that time. Losing that much was a lot for me and it just didn’t seem right.

We ended up moving cross-country, which was stressful in itself. I’m sure the stress didn’t play a very positive part in the process, but we moved back. By that time, my son was 5 months old. Between him being 5 months and 8 months old, my symptoms got way worse. The constipation got worse, the blood got worse.
Something that stuck out to me was the smell that I was smelling. That’s always a little embarrassing for me to say, but I’ve learned that when I have said that, this is actually something that other people have experienced as well with this cancer. So I do like to say that. It was almost like a sewer smell. It’s something that I’ve never smelled before.
On top of that, I would lose my appetite. I’d be really, really hungry and then I would bite one thing and I’m like, I’m full. I don’t want this anymore. My appetite went away. I’m assuming that’s why I lost about 7 to 8 pounds. I weighed about 115 pounds at that time. Losing that much was a lot for me and it just didn’t seem right. I would wake up every morning and be like, I don’t feel good. I never feel good.
Searching for Answers
She said, “You need a colonoscopy, don’t you?” I was like, yes, desperately. She said no problem. She got me the referral. I got an appointment that next week at a GI…and that day, I found out that I had a tumor.
Did you talk to family or friends about your symptoms?
I told my husband one day, I just don’t feel right. I don’t know what’s going on, but I don’t feel right. I will always remember that moment he was like, “Is it because you don’t want to go to work?” I’m like, I would love to not go to work. But no, it’s not the reason. I just don’t feel good and I don’t know what it is. I also have cramping as well.
There was one day I was getting ready for work. I went to the bathroom, I looked down, it was not that time of the month for me, and there was an alarming amount of blood. That’s when I was like, something’s wrong. Throughout this process, I was taking pictures of what was happening in the bathroom because it was just so not right. Of course, I tell my mom everything. I think a lot of us probably do if we have a good relationship with our mom. I’m sending her pictures, and that day I sent her a picture of that. I was like, Mom, what’s going on?

I went to the bathroom, I looked down, it was not that time of the month for me, and there was an alarming amount of blood.
What happened on your trip to the E.R.?
Because we moved across the country, health insurance was a problem for us. He’s my husband now, but we were not married then, so I did not have good health insurance, so I couldn’t see a primary doctor. There was no one there to take me. She said, “You know what? We’re going to the hospital. We’re going to the E.R.”
I went to the E.R., and the same thing happened. They heard that I was a new mom. He said, “You probably have internal hemorrhoids. Lay off the spicy foods,” and told me what other foods to lay off. He took my blood work that day and it came back fine. Then he called a family clinic for me to get me in there quicker to talk to someone there.
I left and I was like, every time I say I’m a new mom, there isn’t any thought process to what I was going through. It was like, bam, internal hemorrhoids. That’s always something that I’ll remember, being pushed off by so many doctors.

Did you get any scans done at the E.R.?
No. I wish I got a CAT scan that day at the hospital. They could have given me one. If they did, they probably would have seen something, but they didn’t.
A nurse encouraged her to keep searching for answers
I went to a family clinic and saw a very nice doctor. Something I’ll never forget is one of the nurses who brought me back said, “If you don’t find your answer here, you know your body best. Keep searching.” I wish I remembered her name at the time because I would go back and say thank you. It really resonated with me. You do know your body best and don’t want anyone else to tell you differently.
I saw him, I ended up sending in a stool sample. Nothing really came of that visit. I feel like, looking back, that’s why I was there, to talk to that nurse. From that moment on, I kept talking about how it’s feeling to friends and family. I was very skinny at that point, so everyone was wondering why. I kept saying, I really don’t feel well.
One of the nurses who brought me back said, “If you don’t find your answer here, you know your body best. Keep searching.”
Getting a referral for a colonoscopy

Finally, someone said to me, I know a primary doctor. She takes your insurance. She’s really good, give her a call. That’s exactly what I did. I went in, I showed her the pictures of what was going on. No questions asked, she said, “You need a colonoscopy, don’t you?” I was like, yes, desperately. She said no problem. She got me the referral. I got an appointment that next week at a GI and had that colonoscopy the next day. I didn’t eat anything because it was an early appointment and that day, I found out that I had a tumor.
»MORE: What it’s really like to get a Colonoscopy
Did you suspect you could have cancer?
Because I didn’t feel well for so long, because I was losing so much weight, my appetite was lost, and all these other things were happening, I had a feeling that it wasn’t going to be good. You just kind of know.
»MORE: What Does Cancer Feel Like?
Diagnosis
After my colonoscopy, I went home. I felt my emotions. I cried, then I put them aside…I was like, I can’t let them take over me right now because this is going to be a process.

Awaiting biopsy results
When I went through the colonoscopy and I came out, the doctor came in, and he said, “You have a mass tumor.” He couldn’t tell me if it was cancerous at that point. They did a biopsy. The way he was talking to my mom and me, we knew it wasn’t good. My mom said, “Should we call Sloan or do you have a suggestion on what to do next?” He said, “Absolutely. Start calling people. The best thing to do is get a CAT scan somewhere and have something to show along with this colonoscopy. We’ll be giving you a call in about 2 weeks to let you know if you have cancer or not.” That was the longest 2 weeks ever. I had a feeling that I did have cancer because of the way I’ve been feeling. Still, anytime my phone lit up, I’m like, is this it?

It happened about a week and a half after. I always remember because the day I got my colonoscopy was actually my husband’s birthday. Those dates are always in my head from that moment on. My mom and I were in Walmart, trying to get our minds off things, just looking around. I don’t think we went for anything special, just to get out of the house. I got the call in Walmart and was like, alright, I have cancer. My mom and I had a feeling and we were like, alright, what’s next?
How did you react to your cancer diagnosis?
After my colonoscopy, I went home. I felt my emotions. I cried, then I put them aside. We went out to dinner. I was like, I can’t let them take over me right now because this is going to be a process.
Choosing a hospital for cancer care
That day, my mom was very on it with a lot of things. I’m so thankful for that. She said, “Okay, I’m going to start researching. We’re going to pick 3 hospitals to go to. We’re going to see where we feel comfortable. We’re going to hear out what they all have to say, and then we’re going to choose.” That was our plan. We also had my aunt researching a bunch of places as well. Thankfully, I have a very great support system.
We didn’t make it to 3 hospitals. Sloan was our first stop and our last stop. I felt like family from the day that I walked in there. That’s where it really all began.

Getting married and resolving insurance issues
I don’t think I really processed anything until afterward, which was a whole other side of having cancer. We had so many things to cross off our list that it was always, what’s next? Time was ticking and I felt so sick.
We also had a health insurance issue. From finding out I had cancer when I got the call, before going to Sloan, my husband and I had to get married because I had to get on his health insurance. So at the time, we couldn’t get in anywhere. Nobody would marry us, everyone was full, and everyone was booked. My mom goes to a church around here and she called someone and was like, I really don’t think that she’s going to marry you because you didn’t go through the whole process of the marriage meetings that they do in the church. She ended up calling the pastor there and asked, “Can you please marry them?” After hearing her story she said, absolutely.



We quickly got married a few days later. It was a random Monday in January and I was able to hop on my husband’s family insurance plan. He’s a teacher, thankfully, but it was still tough because we were paying $1,700 a month from that moment on until last October. We’re a new family starting out, we just had a baby, we just moved across the country, I now don’t have a job, I’m going through cancer, and now we’re also paying rent. This is like half our rent, how much we’re paying for health insurance a month. There was always something that we were worrying about more than having time to process what was going on.

I don’t think I really processed anything until afterward, which was a whole other side of having cancer. We had so many things to cross off our list that it was always, what’s next? Time was ticking and I felt so sick.
»MORE: Financial Toxicity of Cancer Treatment
Receiving an official diagnosis
After we got married, I ended up going to Sloan a couple of days later in New York City. My surgeon told me I had stage 3 colorectal cancer. The tumor is 1 centimeter from my anal opening. I most likely will never be able to carry a baby again, and I will most likely have a colostomy bag for the rest of my life.
Every little thing he was telling me, I’m taking it in. I’m like, okay. Then I said to him, “My husband and I were supposed to elope in Switzerland this summer. Can I at least go to Switzerland this summer?” He was like, “No. Absolutely not.” That’s when I lost it. That’s when my bubble burst. Was that really what upset me? Definitely not. But that was what made everything go over the edge. That’s when I lost it. I remember being like, I’m okay, I’m all right. We’re gonna get through this. But what made me feel really bad is, I bring this guy that I meet in California, home to New Jersey. We have this baby, and we’re not even fully married yet, or we were just married, and now I can’t even bring another baby into this world with him. I felt so bad for him as well because it’s such a tough situation, I felt.
My surgeon told me I had stage 3 colorectal cancer. The tumor is 1 centimeter from my anal opening. I most likely will never be able to carry a baby again, and I will most likely have a colostomy bag for the rest of my life.
Treatment

Did your doctor discuss fertility with you?
He did talk about it. He talked about pinning my ovaries. The reason I wouldn’t be able to carry my baby again was because of the radiation and where it was going to be. It was all in my lower area and everything would be all fried up so I would go into early menopause. The pinning of the ovaries is a chance that it wouldn’t happen, so that was a decision that we were also planning on making. Do we do that? Do we not do that? What’s the best thing to do? That was a hard decision.

He did say I had time to go through fertility and freeze embryos or eggs. I did have some time to do that so that was our next step. It was the fertility first, then it was going to be chemo, then radiation, oral chemo, and then surgery.
We went to RMA and we started the shots. We chose to do embryos, and that was the most painful part of my cancer journey by far. I had the eggs growing in my ovaries. Then I had my tumor sitting a centimeter from my anal opening. Because of where it was sitting and everything growing here, everything was so enlarged. I also feel like after I had a colonoscopy, it irritated it a little bit. I was in the most pain in my life. I remember there were times that I’d have to go lay down and I was in a fetal position. There was nothing I could do. Or I would sit in a hot bath but it was the most painful part of my journey by far.
»MORE: Fertility After Cancer Diagnosis
From there, a little bit of light came. I got the call that we got 4 embryos. That was really nice to hear. Especially as a woman, you’re like, at least I have that. It was fun to hear that we had 2 girls and 2 boys frozen. It shed some light, some happiness in our house. After that, it was game time.
What were the next steps in your cancer treatment?
The way that he talked about what I’d be feeling, what I’d be experiencing physically, and how it would change my sex life, was really, really hard to hear. Going through my whole cancer journey, that appointment is what scarred me.

I had my next appointment at Sloan. I talked to my oncologist. They’re so amazing. They’re so family. We talked a lot about emotions. We talked a lot about how are you feeling, what’s going on physically, mentally, and always checking in. She said, “Alright, next appointment we are going to be talking about putting a date on treatment.”
In between there, I was also seeing the gynecologist because we were talking about pinning up my ovaries still. So I was doing some things in between. We decided to not do that. Then that next appointment we were making it for chemo, oral chemo, radiation, and surgery, but we were really just focusing on the chemo part.
I did talk to a radiation doctor which was one of the scariest appointments that I had. The way that he talked about what I’d be feeling, what I’d be experiencing physically, and how it would change my sex life, was really, really hard to hear. Going through my whole cancer journey, that appointment is what scarred me. I’m glad that it wasn’t something that was going to be happening right away and that we focused on one thing at a time.
Joining the Dostarlimab clinical trial
We decided we had nothing to lose, so let’s go for it. At that time, I was the fourth person in the whole country to go on this drug.

We were about to start chemo and we had an appointment for March 4th. At that appointment, I had a research nurse come and she mentioned that they may have another option for me. My mom was with me as well and we were open to hearing it. We went into another room, we sat, and she presented this trial drug to us. When you’re so sick and – I was also 28 – you’re young, there are big words that are being used. There are so many things that they’re talking about that I have no idea what’s going on. It’s hard to understand.
My mom was sitting there with a notebook, writing things down, ready to research it later. She explained things as much as she could, but there wasn’t a lot of research on this drug because it’s a trial drug. Mom and I looked at each other, we’re like, out of all the things that she just said, the symptoms don’t sound as bad as chemotherapy. Should we give it a whirl? We decided we had nothing to lose, so let’s go for it. At that time, I was the fourth person in the whole country to go on this drug.
At the time, I knew it as a bunch of letters and numbers. It didn’t have a name yet. It’s Dostarlimab. There were 3 people in front of me and I didn’t really know much about it at that time. I had no idea the people in front of me, what their process was. I had no idea what this drug could do for someone at that point.
How were you selected for this clinical trial?

My tumor had a test for a certain gene, a certain mutation. I’m not sure what it is off the top of my head, so I always have my mom here, but it’s some kind of MMR deficiency. They also tested me for Lynch syndrome as well. I ended up not having Lynch syndrome. I know that people that were on this drug or are on this drug, do.
The tests were already done, which is why they were able to present me with the opportunity. They knew that I was a match for it. From what I know with colorectal cancer, only 5 to 10% of people are able to go on this drug that are a match. It’s a very low percentage, but you never know if you are a match.
Signing the papers, I was so sick that I barely remember a lot of that. My mom did a lot of it, she helped me. I don’t know how people go through cancer, not having someone who can sit there and do that with them. I don’t know where I would be without my mom doing that. Anyone who does go through that, I give you so many props.
After that, it was 9 treatments, 1 every 3 weeks, and it was only for 30 minutes.
Was it an infusion treatment?
Yes, I did have a port.
How did you feel being 1 of 4 on this clinical trial?
I don’t think I processed that. Being young, being so sick, being in so much pain, it was like, alright, cool, let’s just get started. At that time, I also didn’t process what goes behind the clinical trial drug. Really, what is it? All I knew is that they didn’t know a lot about what could happen. That’s the only thing that I knew. At that time, I was like, let’s just see what happens here.

Did you experience side effects from this drug?
I didn’t have any side effects. If anything, I was a little tired. I don’t know if that’s because I was also a mom with a very young baby or if I was very tired from having cancer and being sick. But I didn’t have any side effects.
It was a 30-minute transfusion. Every time I was there, I was not there for hours. I didn’t have to bring it home with me. I wasn’t worried about losing my hair, which was really nice. I didn’t have any burning sensations. One thing they were always checking was my thyroid to make sure that the levels were okay because that was something that could be off. They said if something were to happen with my thyroid, I would be taking a pill for the rest of my life. I always said that’s fine with me. If that’s the worst thing that comes from this, I can deal with that. Other than that, I didn’t feel any side effects.
Was the drug effective in treating your cancer?

“There are 3 other people in front of Kelly who have been on this drug. Those 3 people’s tumors disappeared by the end of treatment 9.”
I had my first treatment, then 3 weeks later I had my second treatment. After that one, I was feeling a lot better. I didn’t know if that was great or not great. I was just in the moment of, okay, I feel good today.
This is definitely TMI, but it’s always great to share that kind of stuff. I felt myself. I was in the bathroom for a long time – not constipated, the other way around. I remember calling my mom saying, is this normal? Is this okay? She called Sloan and they were like, “This is a great sign. It means that her body is flushing out what’s been clogged for so long.” I was like, okay.
After all that happened and I came out of the bathroom I’m like, wow. I feel like a whole new person here. It’s crazy because that was only the second treatment. By the fourth treatment, my tumor was halfway gone and we did a PET scan, we did an MRI, and then we also did sigmoidoscopy, and they always do a biopsy. They do 3 for research and one for them. Looking at the camera when they were doing the sigmoidoscopy, the doctor was like, “Your tumor is halfway gone.” That’s something that we did not expect to hear. It was amazing to hear that.
I had to get blood work done that day. Usually, I don’t get blood work done in New York. My mom was there and one of the research nurses came up to her and said, “I don’t know if you know about any of this, but there are 3 other people in front of Kelly who have been on this drug. Those 3 people’s tumors disappeared by the end of treatment 9.” My mom told me this. She’s like, “I didn’t know if I should tell you. I don’t want to get your hopes up.” I remember that moment we walked out of New York when she was telling me, and we were walking on the street and we both started crying. We also were like, we don’t want to jinx it, so we don’t want to tell anybody. Of course, we did tell our family after that because it’s hard to keep that secret.
As exciting as it is to hear, I always looked on the other side. I am only number 4 on this drug. I don’t know if it’s going to work for me. I don’t know if I’m going to be one of those people that my tumor is going to disappear and I don’t want to get my hopes up. So as excited as I was, I always had that little bit of reality of, I’m not sure what was going to happen.
Survivorship
Never let yourself down. Know how important your body is because you do know yourself best and your gut feelings follow them. They’re there for a reason.
Maintaining a positive mindset

After that, we continued with scans, sigmoidoscopy, and treatment. The tumor was slowly getting smaller at that point. As exciting as that was, radiation was still on the table for me. A lot of times when I had moments to myself and I was really thinking about things, I was still thinking, am I ever going to be able to have a baby again? I’m a very strong-minded person, so when I go through these thoughts, it’s usually just me, myself, and I, and I go heavy on what I’m thinking about. I’m like, okay, we’re going to see what’s going to happen and stay positive. There’s going to be a light at the end of the tunnel no matter what it is. There’s going to be some type of positivity within this journey of mine. That’s really what brought me through my cancer was my mindset and my positivity.
What were the results after you finished cancer treatments?
By treatment 9, my tumor had disappeared. It was amazing to hear. I’ll always remember that the radiation doctor called me. I’m on the phone with him and he’s like, “Alright, we set up your appointment for radiation,” and talked a little bit about that. I’m a huge introvert. I don’t ever ask questions about anything. I always feel like I’m annoying somebody, but I’m thinking, why am I still going through radiation? There’s no tumor. I actually said something which is so out of my comfort zone. I’m like, “Why are we making this appointment? I don’t have a tumor anymore. It’s disappeared.” He was like, “What do you mean?” I said, “I was on a research drug. I was told I don’t have a tumor anymore and I was also told I don’t have cancer anymore from the biopsies. I don’t understand why I’m still going through radiation.” He was like, “Let me call you back in about 10 or 15 minutes.” I said ok and hung up the phone.
By treatment 9, my tumor had disappeared.
My husband was home. I’m like, I don’t know what’s about to happen. I’m really nervous. He said he was going to call me back in 10 or 15 minutes. What is this? Is he going to call me back? People say that and it’s like hours or it’s days. I’m pacing back and forth, and he calls me back and said, “Kelly, there was an amendment in the protocol. I mean this in the nicest way possible, but I hope to never speak to you again. We are not going through radiation.” I was like, “Thank you so much.” That right there was the best day of my life.
The importance of being a patient advocate
Never let yourself down. Know how important your body is because you do know yourself best and your gut feelings follow them. They’re there for a reason.
Describe your experience with survivorship
During those 2.5 years, my mental state and emotions caught up to my physical state. I didn’t know that that was even happening. I was having anxiety attacks, panic attacks, and I had no clue why.

It’s been hard. I still was asking about having a baby at our appointments and my oncologist was like, “I really advise you to wait about 2.5 years. In between those 2.5, your cancer is most likely to come back during that time. If you’re pregnant and your cancer comes back, it’s a whole other ball game you’re playing.” I was pretty upset to hear that because, in my brain, I’m like, no cancer. Let’s get this baby going. So that really hurt me.
Looking back, that was the best decision I could have done, because I didn’t realize that I didn’t process anything that had happened. I realized that I was very strong-minded. During those 2.5 years, my mental state and emotions caught up to my physical state. I didn’t know that that was even happening. I was having anxiety attacks, panic attacks, and I had no clue why.

I remember talking to someone who had also recently gone through colorectal cancer, and her story is very different than mine. I met her through one of my good friends who I grew up with, and she was like, “Oh, you’re a year and a half in? Here it comes. Get ready because your mental state is now catching up.” After she said that, it made complete sense, but I had no idea that that was even a thing. That was really hard and I really needed to take a breather.
It was hard for everyone else around me to understand because everyone is like, “You don’t have cancer anymore. Life’s good.” It couldn’t be further from the truth. Listening to your body, listening to yourself, and telling yourself you are going through this. This is something that is still catching up to you that you have to process.
Reflections
What’s helped you process your cancer journey?
I did a lot of self-discovery and self-growth programs. I did a big one based in San Diego, California. That was really helpful for my personal development and understanding of who I am. I’m still doing that. Getting into yoga, getting into meditation during this time became a hobby of mine. I was making sunglasses chains for myself and my friends. I ended up selling them, but it was calming for me.



I still am processing to this day. I’m almost 3 years out and it’s definitely tough. Also, I’m about to have a baby tomorrow. That’s a whole other process too. I keep thinking of how much my body has been through in a short period of time. But it’s an everyday kind of thing. You have to take every day by the hour. I’m always processing, I’m always looking back at things, and I tend to really try to pull out the positives. For example, our air conditioning broke yesterday, and baby’s about to be here, and my husband is like, “Oh, of course. This is the way our life goes.” There’s just always something coming up and that is how life goes. There’s always going to be problems and it’s how you deal with them. That’s something that I’ve learned throughout this cancer journey, too.

What advice do you have for someone on their cancer journey?
Give yourself grace. It’s the biggest thing. Everyone has different seasons in life. Whether it’s cancer or something else that you’re going through that’s traumatic, upsetting, or hard, give yourself grace.
A lot of people go through a lot of things and talk about it. I think being vulnerable is really important. It gives somebody else space to open up. You never know who someone knows and what they’re going through. If you’re able to open up to someone else, it is very therapeutic for you and it’s very therapeutic for someone else and it’s relatable.

Give yourself grace. It’s the biggest thing. Everyone has different seasons in life. Whether it’s cancer or something else that you’re going through that’s traumatic, upsetting, or hard, give yourself grace.
Thank you for sharing your story, Kelly!
Thank you for taking the time to hear my story and to help bring awareness to this cancer as well. That is something I do want to say. There is a huge rise in our country in young adults being diagnosed with colorectal cancer. Bringing awareness to that is very important to me because of our situation. Thank you so much for giving me the opportunity to bring more awareness.
More Colorectal Cancer Stories
Jackson A., Colon Cancer, Stage 3
Symptom: Sharp abdominal pain
Treatment: Surgery (emergency transverse colectomy)
Jay W., Colon Cancer, Stage 4
Symptom: Occasional presence of blood in stool
Treatments: Chemotherapy, surgery (installation of port and liver infusion pump, colectomy, hepatectomy, liver ablation, removal of liver infusion pump)
Kelly C., Colon Cancer, Stage 4
Symptoms: Constipation, bloating, severe abdominal pain
Treatments: Surgeries (colectomy, colostomy, hepatectomy), chemotherapy
Marc Anthony S., Lynch Syndrome and Colon Cancer, Stage 2A
Symptoms: Blood in stool, severe constipation, persistent exhaustion, constantly feeling cold
Treatment: Surgeries (sigmoid colectomy, lymphadenectomy)
Crystal W., Colon Cancer
Symptoms: Blood in stool, intermittent severe lower abdominal pain, urinary tract infection (UTI) with strong odor, fistula
Treatments: Surgeries (cystectomy, oophorectomy, and hysterectomy), chemotherapy
Albita G., Colon Cancer, Stage 4
Symptoms: Blood in stool, pain during defecation, constant constipation, steady weight gain in the midsection despite exercising
Treatments: Surgeries (colectomy, hepatectomy, hysterectomy), chemotherapy, radiation