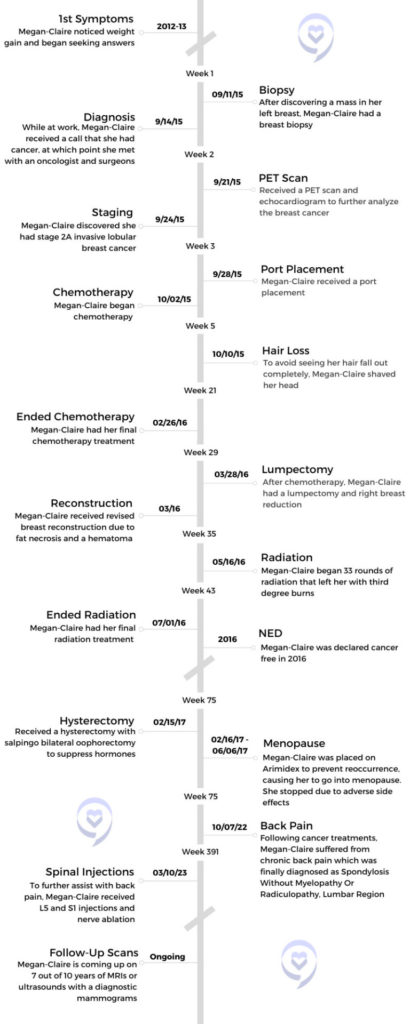
Megan-Claire’s Stage 2A Invasive Lobular Breast Cancer Story
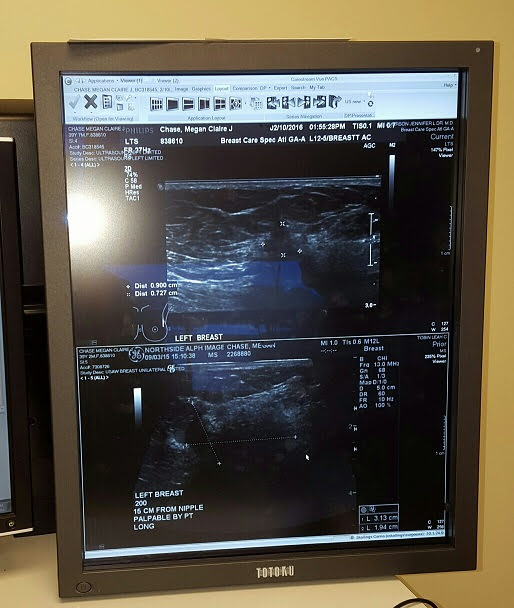
With ovarian and cervical cancer running in her family, as well as issues with her ovaries, Megan-Claire assumed she would get one of those cancers. Preventative early mammograms showed she was all-clear despite developing abnormal symptoms like green bruises, brittle hair, sudden weight gain, and a mass in her left breast. A biopsy revealed she had stage 2 invasive lobular breast cancer which doctors believed had been growing in her for 8-10 years.
As a single woman, Megan-Claire was unsure of how she would afford the cost of her cancer treatments when she came across the number for the social worker assigned to her case. This led to financial breakthroughs through grants her social worker directed her to. Still, being single with cancer led to other challenges such as being her own caretaker.
Megan-Claire shares her cancer story with us, including the challenges of finding good oncology care post-cancer, navigating the adverse side effects of cancer treatments, how she advocated for herself, how her quality of life changed, and her advice for others on their cancer journeys.

- Name: Megan-Claire C.
- Diagnosis (DX):
- Breast cancer
- Invasive lobular
- Left breast
- Breast cancer
- Staging: 2
- Symptoms:
- Green bruises on lower left leg and left arm
- Sudden weight gain
- Dry, brittle hair
- Zit on left breast
- Mass in left breast
- Age at DX: 39
- Treatment:
- Chemotherapy
- Red Devil
- Taxol
- Surgeries
- Quadrantectomy
- Reconstruction
- Fat necrosis and hematoma removal
- Hysterectomy and oophorectomy
- Radiotherapy
- Hormone Therapies
- Lupron
- Tamoxifen
- Nerve ablation and spinal injections for back pain
- ReBuilder for neuropathy
- Chemotherapy
Trust yourself and always remind them that [the doctors] are not the only ones making all the decisions. They can make suggestions for you, but it’s up to you to decide, is that the way I want to go?
Megan-Claire C.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Symptoms & Diagnosis
- Tell us about yourself
- Does cancer run in your family?
- What were your first symptoms?
- Being diagnosed with a rare form of breast cancer
- Did you suspect the mass was cancer?
- Getting a biopsy
- Getting a diagnosis
- How much time passed between you discovering the mass and getting a diagnosis?
- How did you process getting a cancer call?
- Treatments
- What were the next steps after getting diagnosed with breast cancer?
- What did the port feel like?
- How did cancer impact you financially?
- Speaking to a cancer social worker led to financial breakthroughs
- Did your doctors talk to you about preserving fertility?
- Taking classes to learn about the effects of chemo
- Is there still a ChemoFlage class people can take?
- What breast cancer treatments did you undergo?
- Side Effects
- Did you have side effects from cancer treatments?
- What caused your chemo-induced peripheral neuropathy?
- Did doctors inform you about adverse reactions to chemo that might occur?
- What does neuropathy feel like?
- What helped improve your neuropathy?
- Describe what it’s like using the ReBuilder for neuropathy
- Did you have any complications from your surgery?
- What was your experience with radiation like?
- The importance of being a patient advocate
- How did your body react to tamoxifen?
- Quality of Life
- Describe life after cancer
- Meeting others in the cancer community through Camp Hope
- Finding better medical care post-cancer
- Describe not being listened to by your doctor
- Finding medical care that’s best for you
- How did your body react to Lupron injections?
- Seeking new alternatives to prevent reoccurrence
- Describe your hysterectomy and oophorectomy
- How did you feel after that surgery?
- Were you working around the time of your surgery?
- Post-Cancer Complications
- What was the next course of action in your treatment?
- Did you feel relieved that you were in a position after surgery to not need follow-up medications?
- Did you eventually switch doctors?
- Further complications prompted more time off of work
- Were your finances affected during this time?
- Describe your fat necrosis surgery
- What led you to your current primary care provider?
- What helped your back pain?
- What has your quality of life been like with chronic pain?
- How long did you experience relief with spinal injections?
- Reflections
Symptoms & Diagnosis
Tell us about yourself
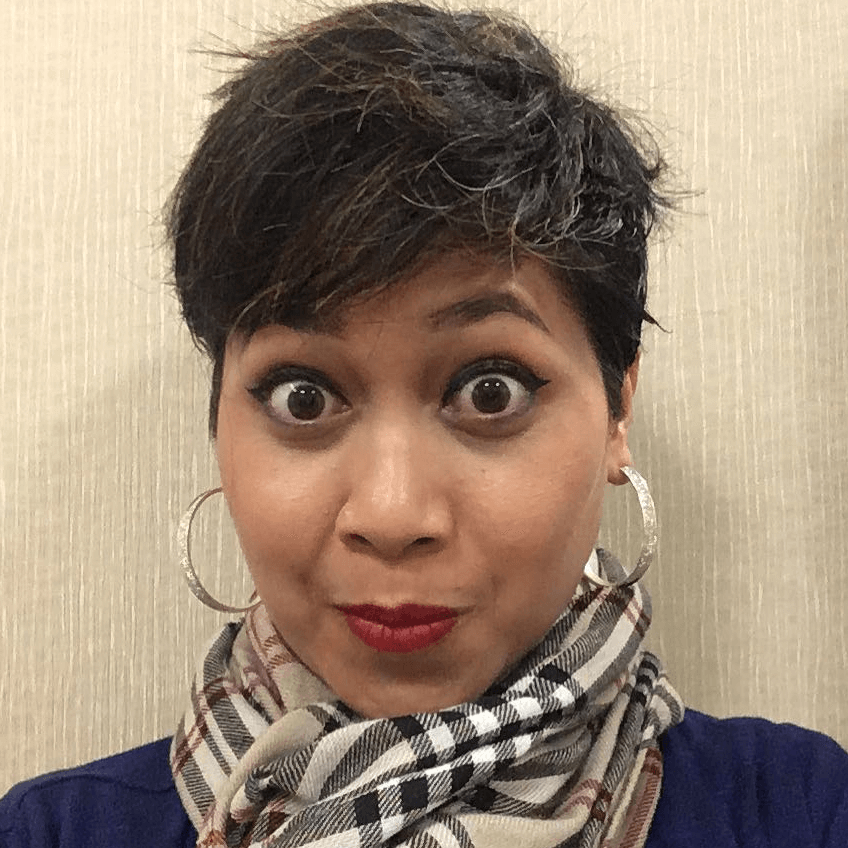
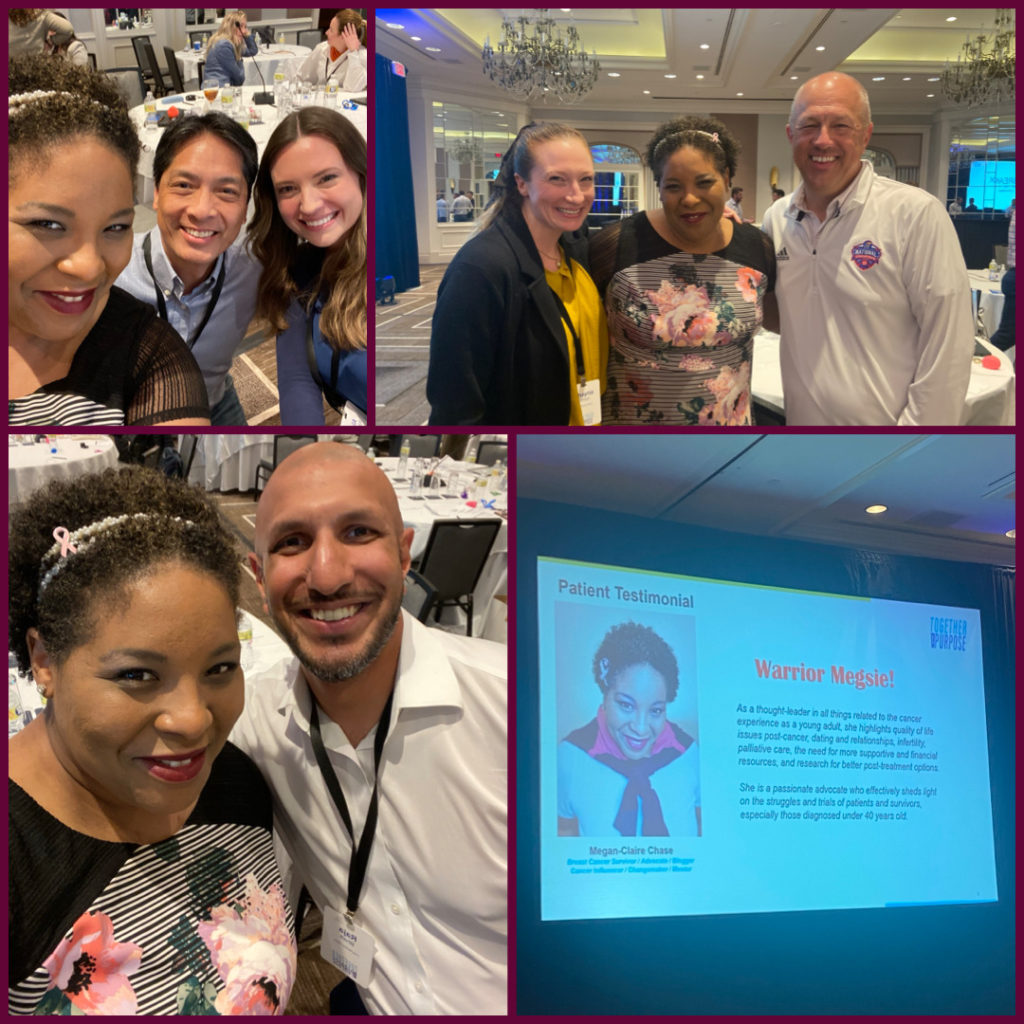
I am Megan-Claire Chase and Megan-Claire is my first name. I’m also known in the cancer space as Warrior Meg. I live right outside of Atlanta, Georgia, in Dunwoody. I get the best of both worlds because it’s right in the middle. I get the suburb feel and on the other side, I get the city feel because I like both.
I grew up in Macon, Georgia and my claim to fame there is that I was a former Cherry Blossom Princess. The whole court portrait hangs on Cherry Street in the Cherry Blossom House to celebrate the cherry blossom trees.



I went to college in upstate New York, the College of Saint Rose. The claim to fame there is Jimmy Fallon went there. I was a freshman when he was a junior, I believe, so I remember seeing him on campus.
I moved out to LA for 5.5 years, then I came back because my mother, who was also an ovarian cancer survivor, now has a rare blood cancer. As an only child of divorced parents, I was like, you only have one mother. So I moved back, but I had to be in Atlanta. I was like, I’m not going back to Macon. It’s a great place to be raised, but not to stay permanently. I also have a cat named Nathan Edgar, also known as Baby Natey. He appears in many things that I do and he will be 20 in August.
Does cancer run in your family?
My maternal grandmother, my Nana, told our entire family, “Know what’s normal for your body because we are all different” and “It’s your patient right to be pushy.”

I always start telling my story with, I always knew I would get cancer. I just knew it, but I thought it would be ovarian or cervical. It took my parents 8 years to get pregnant. They did multiple rounds of IVF and during that third month, my mother was diagnosed with ovarian cancer. That was traumatic and scary.
There was no scenario where both of us would survive and thrive. It was either one of us would die and one would live or both of us would die. It was very dire and she actually started hemorrhaging to death, which is why I was born 3 months early. I was supposed to be born in October. Instead, I was born July 3rd, which also happens to be my grandfather’s birthday. I was the favorite grandchild for a while because of that.

My maternal grandmother, my Nana, told our entire family, “Know what’s normal for your body because we are all different” and “It’s your patient right to be pushy.” She has said that forever, may God rest her soul.
Growing up, I had all of the same issues that my mother and my Nana did with my ovaries and I kept having abnormal pap smears. I really seemed to be on the path of one of those cancers. I got to have a preventative mammogram covered at the age of 35 because of that link between breast and ovarian.
I went and they told me, “You are clear. Come back when you’re 40.” I’m like okay, cool. Totally put it out of my head. They never went over the fact that I have dense breasts. My symptoms – and this is what really throws doctors for a loop – were very different than my white counterparts. That’s why I often tell people, especially those who are black and of color, that your symptoms may present differently. So it’s up to you to really push to make your doctors listen. That’s what happened to me.
What were your first symptoms?


I started gaining weight before that preventative mammogram. The weight just started rapidly happening. As someone who grew up studying theater and ballet, and was a cheerleader in college, I was fit. Then all of a sudden, this weight. I went to the doctors and they said, “You just need to lose weight and eat better.”
Now, these are all from chemo, these curls here. I never had curly hair, never wanted curly hair. My hair used to be straight and to my shoulders. I remember my stylist who had been doing my hair forever said, “Are you missing a nutrient? Because your hair is so dry and brittle.” Then it started falling out on the left side only. I’m like, What? I don’t know what is happening.
This is over about 2.5 years. I got these tiny green bruises on my lower left leg. Again, I am hyper-aware. I’m like, I don’t know what my body is trying to tell me here but this isn’t good. I kept going to the primary doctor and the endocrinologist. I thought maybe it was a thyroid thing. Blood tests kept coming back clear. [I was told], “You’re fine. You just need to lose weight and eat better. Maybe you should sleep a little bit more and get some rest.”
I’m like, okay, these are tiny, green bruises. I’m right-handed dominant. I’m trying to make it make sense and it’s not making sense. Then it gets even more peculiar. I get a circular-shaped, green bruise on the back of my left arm. By this point, my primary finally says, “I don’t know what your body’s trying to tell us.” It was just so peculiar. I’m so mad I didn’t think to get a picture of it at that time. But she said, “If this is still here in 2 weeks, I’m gonna bring a colleague in on this.”
Before 2 weeks was up, I went to the dermatologist because I was like, what is this on the outside of my left breast? She said, “Oh, that’s a zit.” I’m thinking to myself, that’s a very odd place for a zit to be on the outside of your left breast. I guess you’re getting where I’m going with all the left-side stuff. She gave me a cream and it didn’t hurt. It went away in 3 days so I thought, maybe she was right. But that just seemed odd to me.

I will never forget, it was August 31st, 2015. That morning when I’d taken a shower, I had not felt anything. But that night when I was taking a shower, I remember because I used to be a huge fan of the show Supergirl. It was in its first season and I was like, I’m going to get in my jammies. This is my show. I’m in the shower, and because of that weight gain and my breast getting bigger – because I never had big boobs before – I was always feeling them. And then I felt it and I was like, What? Where did this come from? It was on the side, it was as hard as a fist, and it was huge. I was like, what?
Being diagnosed with a rare form of breast cancer

As I started doing more research, I started to realize there’s a whole other underrepresented category. It’s hard enough that I’m a woman, a black woman, and now I’m a woman under 40 years old diagnosed with cancer.
Now we know that had been growing in me for probably 8 to 10 years and that it was missed on that mammogram due to the size of it. Ultimately, once I did get the cancer call, I was diagnosed with stage 2 invasive lobular breast cancer.
Lobular is rare in black women. It’s already an uncommon one. Only about 10 to 15% of women get lobular. It’s also known as the sneaky cancer because it can mask and look like healthy tissue, so a preventative mammogram doesn’t pick it up.
Did you suspect the mass was cancer?
I didn’t automatically think breast cancer or even cancer. I was like, what is this? Because of the feeling of it, because I am very aware of my body, and because my mother now has a rare blood cancer, I’m aware of certain things. I already knew it was a mass, so when I was told, “This is a mass. We need to have a biopsy.” I didn’t freak out because I was like, well, obviously. I also think I was protecting myself.
Getting a biopsy
I remember the biopsy. It happened to fall on 9/11/2015, a Friday. I was the last patient of the day and I just wanted to go home and not have to go back to work and think about it.
The doctor said, “I’m going to take about 8 to 10 tissue samples.” It sounds like a staple gun. To this day, I’m triggered when I hear a loud staple gun. She pulled almost 20 samples, I was counting. Because I’m an empath, I can sense when energy shifts in a room. Even though she kept her facial expression totally neutral, I knew she must have seen something. Why else are you taking 10 million samples? They told me, “We’ll get the results probably Tuesday or Wednesday of the next week.” I didn’t think anything else of it.
Getting a diagnosis
Lobular is rare in black women. It’s already an uncommon one. Only about 10 to 15% of women get lobular. It’s also known as the sneaky cancer because it can mask and look like healthy tissue, so a preventative mammogram doesn’t pick it up.
I went to work on Monday. At this time, I was working in radio on the sales side – wish it was behind the microphone. I was timing a commercial, so I’m always aware of the time. I said, “Man, I’m gonna have to send this back to the client. The commercial is too long.” My phone rang at 3:05 p.m. that Monday, and I almost didn’t answer it, because I didn’t know that number. But my gut was saying, answer the phone.

Because I’m a very dramatic person, I’m running down the hall to an empty conference room. This is back when I could run. Now I have neuropathy, I can’t really do that. And she says, “Megan-Claire, you have invasive lobular breast cancer. We don’t know the stage yet.” That was all. I said, “Invasive lobular breast cancer? What the heck is invasive lobular? Wait…Breast cancer. Cancer!” I started getting hysterical, but she snapped me back by being really calm. She said, “Megan-Claire, take a deep breath. I need you to go get a pen and paper because I have very important information to give you.”
Professionally, I do allow people to call me M.C. – short for Megan-Claire – because I really hate it when people chop off my name and just call me Megan. People asked, “M.C., are you all right? What’s going on?” I said, “Yeah, in a minute.”
I go back, and this is where I realize now I had a bit of privilege, which I didn’t recognize at the time. My primary doctor had already talked to the one that did the biopsy. They had already talked with each other and had gone over who were the top 2 oncologists they’d recommend for my case. Who’s the plastic surgeon they’d recommend for my case. I was given all that information upfront. I thought that was something that everyone’s doctors did for them, and it turns out they don’t. I realize now that was a gift.
I was diagnosed under 40, so that put me in the category of adolescent and young adult. Keep in mind, it was 2 months after my 39th birthday that I get this diagnosis, so I’m not feeling like a young adult. As I started doing more research, I started to realize there’s a whole other underrepresented category. It’s hard enough that I’m a woman, a black woman, and now I’m a woman under 40 years old diagnosed with cancer.
How much time passed between you discovering the mass and getting a diagnosis?
It was about a week and a half. Everything moved very quickly. Monday, I get the diagnosis. That Wednesday I met with the oncologist, that Thursday I met with the breast cancer surgeon, then that Friday I met with the plastic surgeon. It was like bam, bam, bam, bam, that whole week.
I remember thinking, why do I need a plastic surgeon? I wasn’t processing that I’m going to need some reconstruction at some point. None of it made sense.
How did you process getting a cancer call?
I really don’t like getting a cancer call. I honestly wish that they had said, “We need you to come in tomorrow. We’re making room for you and you need to bring someone. No if’s, and’s, or but’s about it.” You would already know this isn’t good, but I’ll have someone else with me who can drive and who’s a little bit more clear-headed. Instead of getting a call while you’re at work.
I did talk it over with my mother on the phone, but I didn’t want everyone at work to know this news. But it was so obvious that when I came back, I was in shock. I had gone pale. Everyone asked what happened, so it just came out. I didn’t want it to come out that way, but it’s because I got it while I was still at work and I didn’t know what to do. A coworker did drive me home because I couldn’t handle anything.
»MORE: Reacting to a Cancer Diagnosis
Treatments
What were the next steps after getting diagnosed with breast cancer?
Discovering I had to get 16 rounds of chemo. I did meet all the doctors and had all the tests then I had my port surgery. Before the port surgery, I hadn’t been under anesthesia since I was a kid. I don’t even remember the last time I was in an actual hospital.
My mother was all concerned for me. The nurse came out to go get her after getting the port inserted and my mother asked, “Is she okay?” She said, “She’s up there cracking jokes and laughing.” It really hit me as I think about it now how, even though I was feeling so miserable before the diagnosis and gained all that weight, I still had some energy left. I have none of that now and it’s harder for me to bounce back from a surgery.
What did the port feel like?
I distinctly remember getting that port and what it felt like to have something foreign inside my body. It felt heavy, it felt strange. The next day I was going to a luncheon for work with all the media companies in Atlanta, and I had this big old thing, and it was pretty darn obvious.
Everyone at that point knew I’d been diagnosed with cancer from the moment that I got the call. And getting all the tests and discovering I had to have 16 rounds of chemo.

How did cancer impact you financially?
I remember thinking, how am I going to pay for this? I’m single. I was not making a lot of money at the job I was in. Also, the health insurance wasn’t the greatest so I’m panicking like, how am I going to do this? Due to some technicality of when my insurance was renewed and when I got diagnosed, I was not eligible for short-term disability.
The person on the insurance side was so callous. She goes, “Well, you really should have thought to get this, to add this to your plan. It’s like a broken leg. You don’t know if you’re going to get a broken leg, but one day you will get a broken leg.” I said, “This is cancer.” I’ll never forget that. I thought to myself, wow. Is this how it is?
»MORE: Financial Toxicity of Cancer Treatment
Speaking to a cancer social worker led to financial breakthroughs

She was my social worker and she was a godsend because once I spoke with her and met with her, she helped me find grants to pay for my chemo and to pay for all those tests… When I tallied everything, all the costs of everything, it was almost $400,000 without insurance.
I’m naturally a very organized person because of my grandparent’s influence. My Nana at the time was a registered nurse. I’m glad she wasn’t alive to see me go through cancer because we were very, very close. My grandfather was a mortician, so they were the perfect couple. They always taught us to make sure you read everything, make sure you keep track of certain things. I just already knew to do that.
You’re given so much information when you get that diagnosis. It’s like paper here, paper there, this one’s yellow, this one’s pink, this one’s blue, here’s a book. I remember going through tons of paper where it was just all text, and I happened to see where it said, “Here is the social worker assigned to your oncologist.” I was like, “What is a social worker doing there?” That didn’t make sense to me. I still don’t understand that term in oncology, but I called it to find out.
Her name was Catherine. She was my social worker and she was a godsend because once I spoke with her and met with her, she helped me find grants to pay for my chemo and to pay for all those tests. What people don’t realize, it’s not just about the chemo, it’s all the other stuff as well. It’s every time you’re going to get your infusion, it’s all the medications that you get when you start having severe side effects. It’s the additional scans and all of this stuff all at the same time. I was able to get assistance for my rent because I was single.
If it wasn’t for her, I honestly don’t know what I would have done because I’ve heard of others where they’re just about to start chemo and then they discover that their insurance won’t authorize it. I thought to myself, oh my God, now I know why people die or why people sometimes have to file for bankruptcy and lose everything when someone gets critically ill. When I tallied everything, all the costs of everything, it was almost $400,000 without insurance.
Did your doctors talk to you about preserving fertility?

Once the port was placed, it was time to start chemo. I remember my doctor saying, “We have established that you’re going to need 16 rounds of chemo. Oh, and do you want to freeze your eggs?” She said that all in one breath. All I heard was chemo and that we needed to start quickly. In hindsight – which is something I advocate because I was single and not married – I didn’t think, maybe I should get a consultation with a fertility specialist. At least have that conversation. But that’s not even covered by insurance. I didn’t think how painful, literally and figuratively, that choice would ultimately be.
»MORE: Fertility After Cancer Diagnosis
I wish someone had a conversation with me a day after that saying, “I know you just heard a lot of information. I want to go over this quickly and make sure you understand before you start chemo this Friday.” I wish that had happened, but it didn’t and I’m still very angry about that now. But at the time, we could tell the concern with my cancer was it was getting so big that they said, “We’ve got to first contain it and then shrink it as much as possible.” So all I was thinking is, dear God, we got to get this done because it hadn’t gotten into the lymph nodes yet. And that’s what they were trying to stop. It was very quick.
In hindsight – which is something I advocate because I was single and not married – I didn’t think, maybe I should get a consultation with a fertility specialist…I didn’t think how painful, literally and figuratively, that choice would ultimately be.
Taking classes to learn about the effects of chemo
I took a class and realized not everyone gets this. It’s called ChemoFlage. I don’t know if they still do it here in Atlanta, but this was back in 2016 at Nordstrom, no less. Because the person who started Nordstrom, his mom when he was growing up, had breast cancer and never felt pretty. That was before plastic surgery was approved for breast cancer. It helped me learn about different things that will happen, such as, you’re going to lose your nose hairs. No one thinks about that. You’re going to feel like you have a cold 24/7. I was like, oh my God, I never even thought about that.

That’s where I met my chemo twin, Erin. She was 3 months ahead of me in her treatment. We had different types of breast cancer, but she was the first person I’ve ever seen bald. When she took her scarf off when we had a break from the ChemoFlage class, I started crying because I was like, oh my God, that’s going to be me. It really hit home in that moment.
Is there still a ChemoFlage class people can take?
I don’t know. I need to find out because it was so helpful for me. It was this older woman who had gone through cancer and she wanted to help share that. I never learned how to tie a scarf on my head before. [I learned] you have to drink so much water when you are on chemo, to the point now I actually have a hard time drinking water because of how much I had to drink to flush out the poison. One of the names of the chemos is known worldwide as the Red Devil. It’s literally red with a skull and crossbones on it. I’m just like, what? What are you putting in me?
What breast cancer treatments did you undergo?
I had 16 rounds of chemo. I had the Red Devil, which is called Adriamycin, and Cytoxan. I would have those together. It’d be 1 week on, 1 week off. Then I had 4 of those, then 12 of the Taxol. Then we had my surgeries and I opted for a lumpectomy.
I thought I had to have a double mastectomy but I had such a great plastic surgeon and breast cancer surgeon. They were so good and they worked very well together. He was known as one of the top ones in Atlanta for those under 40. He told me, “We can conserve your breast based on where your tumor is, depending on how big it is once we go in there.” They did all of it at once, I had 4 surgeries in one. He said, “When you have a double mastectomy, that doesn’t mean that you couldn’t have a recurrence or metastasis.” I was like, wait, what? I now know that he did say metastasis but I didn’t hear that until later.
He told me, “I can conserve your breast.” I remember asking him, “What are these scars going to look like?” He didn’t have any black chests of women to show me. I think it hit him and I’m thinking to myself, I can’t have been the only black person to ask this question. Maybe it was just the way I said it or what have you, but it really hit him. “Can we take a before and after picture of you so I can now show it to other patients?” I said, “Sure you can. I really think you need to have more. But baby steps.” I didn’t think about the whole scarring part. For some reason, I thought I was just going to heal and they’re going to disappear.
After we had the lumpectomy, he said that my breast cancer surgeon took a whole quadrant of my breast out because though they shrunk it quite a bit, they wanted to get such a clear margin that they took a quadrant out and then had reconstruction of my left breast and a reduction in my right breast.
Side Effects
Did you have side effects from cancer treatments?

Were there side effects? I seem to have gotten the mother lode of side effects all at once. Keep in mind, I’m working full-time. One of the first things I did to make things a hair less traumatic – pun intended – was get my head shaved. My stylist actually cried. I had prepared myself to see that. It wasn’t until right after the second Red Devil and the other chemo, because I had 3 different types of chemo, the hair started to fall out. I had to admit it was better to see it come out in tiny hairs than in clumps. I will always be thankful that I heard that little tip in ChemoFlage class because that was hard.
I always tell patients to make sure they’re telling the pharmacist too, because they could be huge in coming up with other ideas for you.

I got these horrible mouth sores. They often give us what’s called – and I do not know the official name of it – Magic Mouthwash. If you say that in any oncology center, everyone will know what you’re talking about. To help prevent mouth sores, your teeth hurt, everything hurts. It only helped a little.
I just happened to mention it to my pharmacist at the cancer center, and we need to shout out some really good pharmacists. Her name is Candace and I told her, “I don’t feel like this Magic Mouthwash is really working. I still have these mouth sores. I don’t know what’s happening.” My tongue was starting to turn black, and the palms of my hands and feet were black. It looked like I was burned. That was freaking me out. She goes, “Have you ever heard of Gelclair?” I’m like, “What is that? It sounds perfect since my name is Megan-Claire.” She said, “I can get you some Gelclair for free.” I was like, you can?
She made a call. I got 8 boxes of this stuff, which turned out to be a lifesaver for free, sent to my home because I had that communication with her and she was like, “Let me help.” I always tell patients to make sure they’re telling the pharmacist too, because they could be huge in coming up with other ideas for you. I would use the Magic Mouthwash first and then swish around the Gelclair, which is clear, and put a coating around my mouth. I was fine after that, but I had other severe side effects. Of course, the nausea. You really have to try and stay on top of it before it gets too much because once it’s there, it’s really hard to lower it.
What caused your chemo-induced peripheral neuropathy?
With one of my chemo treatments I had to get once a week for 12 weeks, I had such a severe reaction in the first 15 minutes of the first treatment – chemo-induced peripheral neuropathy. They had told me, “You might feel a little neuropathy, some tingling, some numbness in your hands and feet around the 8th to 10th one.” I’m like, alright, cool. I did have my hands and feet in cold water because they were saying, “We’ve heard from some patients that helps.”

I’m so glad I can finally find the words to describe it. It felt like a current running from my head all the way to my feet, and I felt my nerves just die. I started screaming in the infusion room. I was the youngest person in the infusion room. They came over and there was no way to even adjust the dosage because the onset was so quick and permanent at that point. I couldn’t walk after that moment. I had to use a cane. Anytime we would go to the cancer center, I’d be in a wheelchair.
Did doctors inform you about adverse reactions to chemo that might occur?
Not before this happened. The oncologist didn’t mention how severe this could be and how debilitating this could be for some people. I feel like they were thinking, “We don’t want to scare the patient,” but I wish I had just known the potential of what could happen. Knowing this may not happen to me, but at least I’ve got this list that I can refer to that other patients have gotten. But we all were surprised at how intense and quick it was. And there are no tests to this day to discover who is more susceptible to chemo-induced peripheral neuropathy.
What does neuropathy feel like?
I compare it to when your foot falls asleep, that’s what it feels like. But it was 24/7 so my brain couldn’t connect, so I’d often fall. I was a huge fall risk and this lasted for years, unfortunately. I did find something that helped that was not medicine, but that’s what it felt like because my brain wasn’t receiving the signals. So when I’m thinking my foot’s hitting the ground, it’s actually not hitting the ground. Then I would fall over.
As someone who was single, going up some steps to get to my car and going down some steps to get to my apartment became a real issue for me, and constantly falling into walls. If I’d fall down, oftentimes I’m by myself. I remember hitting my head once.
I’d finally gotten enough money saved again and I was looking for a townhouse. I was walking with the realtor. All of a sudden, I went down hard and he was like, “Oh my God, are you okay?” I was like, “Oh, I’m fine.” I got right back up and just started walking. It was 6 hours later when the pain set in. That is how long it took for my nerves to actually realize something was wrong and I had a grade 3 sprain. It was a hair away from being a hairline fracture. It was that moment where I was like, I’ve got to find help.

It was so hard getting around and it was my right foot too. I learned how to drive with my left. It really gave me a whole other respect, because I already had respect for those with disabilities and specific handicaps. I have a permanent handicap sign, so when I get out of the car and I look like this, I’ve had people yell at me like, “What are you doing? You don’t belong there.” I’m like, “Y’all don’t even know.” But I can’t walk super duper long distances anymore without that risk. With my hands, I couldn’t even button anything. I couldn’t put my earrings on. You think you are holding on or you think you’re pressing down, but you’re not and that’s what’s so scary.
What helped improve your neuropathy?
Believe it or not, 2 years ago, because Instagram hears everything you say, I saw this ad for a chiropractor. What caught my eye was the fact that he differentiated between diabetic neuropathy and chemo-induced peripheral neuropathy. I was like, I need to talk to him. I went to him. He was located in Marietta, Georgia, and the first question I had for him was, “Did you vote for Trump? Because if you did, we cannot talk.” He was like, “No, no, no. And I’m Canadian.” I said alright then. We’re good.

I have about 60% feeling now in my feet and in my legs so I can feel the gas pedal. I can feel the brake, and that’s because it has been 2 years of me going to his office 2 to 3 times a week and doing all of the things at home.
I told him everything I had gone through and how gabapentin and glutamine didn’t work. All of these things did not work for me. When I was done talking, he goes, “Are you a researcher?” I was like, “Oh my God. Well, I am the doctor of my body.” He goes, “I can help. I’m not saying I can get you back to 100% but we’re going to do some tests right now and assess to see just how bad the nerve damage is.”
What I learned is a lot of it is nerve damage and lack of circulation. He did thermal imaging. You could see where the blood flow stopped, which is why I would get so cold, like cold flashes in my feet.
The big test and this is something anyone can do at home if you have chemo-induced peripheral neuropathy, he did a blow dryer on my neck so I would know how hot it’s supposed to feel. He did it on my hands and I could feel it. Then he said, “Okay, close your eyes. I’m going to do it on your feet.” I’ said, “Okay, are you doing it? I feel like I’ve been sitting here for a minute.” He goes, “Open your eyes,” and he had the blow dryer right on top of my feet. I felt nothing. I remember freaking out and getting so upset. He goes, “No, no. I can help.”
What I started using was called a ReBuilder. It’s stimulations and it has taken so much time and commitment to do, but that last fall I had was so scary to me. I said, I will do what I need to do. Insurance barely paid for it. It cost me almost $4,700. Keep in mind, I’m single. I’ve been through some different jobs. I’m still trying to heal from all of this.

But I got to tell you, with that consistency, I can wear pumps now and I don’t wobble. I can actually feel my toe now. It’s not a full-on feeling. I have about 60% feeling now in my feet and in my legs so I can feel the gas pedal. I can feel the brake, and that’s because it has been 2 years of me going to his office 2 to 3 times a week and doing all of the things at home. We also did shockwave therapy, which goes deep into the tissue. I wanted him to focus mainly on my feet first. I was like, the hands can wait. It’s the feet. The fact that I can actually wear low heels and not fall and I can feel when my foot hits the ground. It’s a miracle.
Describe what it’s like using the ReBuilder for neuropathy
It’s electrodes. The patches, you put in water. I remember I was on the phone with my mother and I was like, “Mother, just in case I electrocute myself, I need you to dial 911.” I was like, “I’m not going to electrocute myself?” He said, “No, these are rubber pads.” You put [them on] your feet and there’s a special spray of solution to help so you would feel and you turn up the ReBuilder until you feel a tap, tap, tap, tap, tap because you don’t want it too strong. It’s on a timer. It gives you 30 minutes straight and you just sit there. So while I’d be working at home, I would be doing that.

Did you have any complications from your surgery?

It ultimately got infections. I was told I wouldn’t need draining tubes because that’s what you get when you have a mastectomy. Well, I turned into a mermaid. I was filled. They had to aspirate 455 cc’s of fluid from my breast. He goes, “God, it’s so rare with a lumpectomy or a quadrantectomy. We normally don’t have to put drains.” I was like, “Well, I think we’ve all learned I’m a little extra. So if you think it’s not going to happen, it’s going to happen to me.” And that is what happened. But the crazy thing is, to this day, I’m totally numb on my left outer side. When they would stick that huge needle in, thank God I never felt it, but it was all so scary to know that I have no feeling.
I don’t know what was going on in there. Everybody is different with how they will heal. Mine just got a lot of fluid.
What was your experience with radiation like?
I had 33 rounds of radiation. I get really mad when others say, “Radiation was a breeze compared to chemo.” I want to set people up for reality. It may be easier for you. I had a really tough time with chemo. I had an equally tough time with radiation because my flesh actually burned off. I now know what a burn victim feels like underneath my arm. You still see the burn scars underneath my arm.



I remember I had a full-on meltdown because I was like, you didn’t tell me my flesh would burn off. You just said I might get a little pink or red. The area where they radiate you actually feels warm like a volcano. It also burned up the side of my neck and a whole huge circle behind my back, too, which I didn’t even notice until I was going to occupational therapy. The OT said, “You’ve got a burn on the back of your back.” I was like, wait, what? I didn’t even know. Thank God I didn’t feel it, but it was huge. I had pictures of all of this too.
The radiation oncologist said at that time, “I’ve seen worse.” I went nuts. I said, “Until you have been through this, you haven’t seen worse. I have never seen worse. I’ve never felt worse. Until your flesh burns off, then you come talk to me.” I refused to deal with her and they had to bring in someone else because I lost my mind. They gave me a day to just calm down. It was a Friday that this meltdown happened, and then I was able to finish the 33. Tthat last 3 were the boosters where it’s super targeted, lots of radiation because of the lobular trying to make sure they’re killing any minuscule cancer cells.

It did take a long time to heal. I had to get special creams. I’m still quite traumatized. My neck, there’s some darkness that is always there. I wasn’t prepared for how traumatic radiation could be because all anyone kept saying was how easy it was.
Also, the fatigue was just as bad as the chemo. You have to go every single day with whatever number of radiation treatments that you need. It was 33 days, every single day. I would get it done in the morning. And then that fatigue just built and built and built. I’m still trying to work full-time at this point. I’m just like, I can’t. I really thought that it would be the treatments that would kill me, not the cancer.
The importance of being a patient advocate
Bring someone with you. That’s one of my biggest pieces of advice because you may be focused on one thing that that doctor said, but they’re hearing all the others.
Right now, I’m coming across as very confident. No, even the most vocal person gets nervous. You feel very vulnerable, very small when you’re sitting on the exam table in your little hospital gown. It’s very hard to speak up in the moment. What I always say is, sometimes you can’t speak up in the moment because it’s just so much you’re trying to process and that is okay. I like to say there are different layers to advocacy.
When you start to think about things, always remember you can write that in your portal. You can call and ask for your oncologist’s nurse. If you’re too scared to bring it up with them or if you need help with translation or if English is your second language and you heard something that didn’t quite translate, don’t be afraid to ask and say, is there a social worker? Is there a nurse navigator? Is there a patient navigator that I can talk to? Because I don’t quite feel comfortable asking my oncologist, which is totally normal and fine, but make sure that you do ask those questions.

That’s what’s so scary about cancer treatments and the surgeries, you don’t know how your body is going to react to any of it because no one can tell you, “Yeah, you’ll probably get this.” Other people didn’t get any neuropathy symptoms. Then why did it happen to me? We don’t know.
It’s okay to write your questions out. I would come every day with a list of questions that I thought of from the previous time or later that day to capture it all. Bring someone with you. That’s one of my biggest pieces of advice because you may be focused on one thing that that doctor said, but they’re hearing all the others. Ask if you can record the conversation so you can play it back later. There are apps where you can record it. I would say, “Can you give me a recap of our appointment of what we just talked about so I can record it and play it for myself later?” Doctors, 9 times out of 10, they will do that.
»MORE: Being A Cancer Patient Self-Advocate
How did your body react to tamoxifen?

In between that time of scans and trying to take tamoxifen is when I started to learn how important it is to have people that look like me on clinical trials. I used to be really against them because in the black community, we talk a lot about the Tuskegee Airmen and Henrietta Lacks. We were told that by our grandparents. It’s not like it was that long ago.
When I started having rare side effects, my oncologist said, “Just get off it and give yourself a break for 2 weeks, and then get back on it.” I was like, “What part of no are you not understanding?” I was taken aback that that was her response.
I turned into a chemist. I was like, let me try and find something that is still in that same family. Again, tamoxifen, that’s typically used if you had estrogen-positive breast cancer. I found a vista then I found another one. I was like, it’s in the same family. I’m thinking, maybe there’s an ingredient that I can tolerate better. So I come back and bring it to her. I remember thinking, I’m not the one with the MD here. Why am I the one coming up with other solutions?
Quality of Life
Describe life after cancer
I had that to start processing what had just happened. I was told by my oncologist that you might feel a little depressed afterward because you won’t be having multiple appointments a week, every week. I remember coming home after Camp Hope after that 3 months and I was like, a little depressed? How about a lot of depression? How about PTSD? I started to get very angry.
My scans were clear those first 3 months and that’s when I officially felt like a survivor. I even remember using that language – I’m a fighter. I beat cancer. I was doing all of that. Everyone at work – because I was gone for about 6 weeks, that’s the only time I took for myself – when I came back, they had my desk all set up with all this pink. I was loving it.
I distinctly remember when that shifted. It was 6 months post-cancer when I started to understand that this impacted my quality of life. This has impacted my career because of my memory. Now the next step was to get on Lupron and tamoxifen to help prevent a recurrence. Because the type of breast cancer I had was lobular and the fact that I was diagnosed under 40, they wanted to have me on it for 10 years to be triple sure.
Meeting others in the cancer community through Camp Hope
Radiation was really horrific for me. After that, it was more healing time. Three months later I would have my first set of scans post-cancer. In between that time, I attended what we have in Atlanta called Camp Hope for all cancer patients. You have to get written permission from your oncologist to go out in the wilderness. Even though I’m not a wilderness person, it was really helpful because it was the first time, aside from my chemo twin, that I met others and more importantly, others who had breast cancer and others who were closer to my age. That was a huge healing moment for me, not even realizing how much I really needed that. A lot of us had surgeries around the same time, so we had to be really careful with doing things and lifting and all of that.

Finding better medical care post-cancer
Ultimately, I did have the same reaction, but I was proud of myself for advocating because I was highly aware that now I’m super sensitive to side effects. That’s what I have discovered and that was never the case pre-cancer. I told her, “I want to thank you for helping me get to this point in survivorship. Thank you for keeping me alive, but I need to divorce you because you’re no longer listening to me. I need help in this post-cancer life and I don’t feel I can trust you for that.” She was shocked. She was like, “No one has ever said that to me.” I said, “Well I have.” It was so mean. I can say it with confidence here, but my voice was shaking. And though I’ve never been married or divorced, I was hurt. It hurt my heart.
It took me a good 2 years to get over that because I felt like a number and where people only care about you when you have cancer and they don’t care about you once you’re in that survivorship stage and how it could impact your quality of life. No one told me that I might never get back to how I was pre-cancer and before all of those crazy symptoms that I had. I remember feeling very betrayed.
I went to a competing cancer center. I’m very grateful that I do live in a big city, so there are options. I remember when that oncologist came in – this time I chose a man. I was like, I want to see the difference here. The first thing he said to me was, “Alright, Megan-Claire. We need to think outside the box for you.” I actually started crying because all my defenses were up. I was prepared to be like, look, this is what needs to happen. But he came in, he was like, “I read everything. You’re very sensitive to side effects. We got to figure this out.” I was like, “Are you making me a partner in my own health care?” His name is Dr. Allen and he’s since retired. But I’ll never forget that moment where I felt seen as not just a survivor, but struggling.
I told her, “I want to thank you for helping me get to this point in survivorship. Thank you for keeping me alive, but I need to divorce you because you’re no longer listening to me. I need help in this post-cancer life and I don’t feel I can trust you for that.”

»MORE: Shared Treatment Decision Making
Describe not being listened to by your doctor
She basically said, “Well, it turned out you had the same reaction anyway. I still think that you need to just be off it for 2 weeks and get back on. It might take your system a little bit to get acclimated to it.” I said, “You’re not listening.” But I did feel so much gratitude for at least getting me to this point. She did tell me, “Those are rare side effects.” I was like, “And I’m experiencing them. You’re really not believing my experience.” I felt betrayed because I was like, “How could I have trusted you so much?” Because then I started to question everything. I was like, did I get the best care? But I do feel like I did get the best care during my active treatment. I do.
Finding medical care that’s best for you
That’s the thing. It’s not about hurting their feelings. If you want a second opinion or you decide to go to another cancer institute, it’s about you. It’s not selfish to think about your needs, and if your gut is telling you this isn’t right, this isn’t a good fit, it is your patient’s right to change.
In the black culture and in some other cultures – because I come from a very mixed family – it’s often you just do what the doctor says. But it’s like, no. You just inherently know that you’re not being heard. I was like, this is cancer. This is my life. If this was just the flu, maybe I could deal with that kind of attitude. But this is literally cancer and I don’t know what’s going to happen next so I need to be with someone who I feel has got me.
How did your body react to Lupron injections?
He was very aware that I was still under 40. I had not had my birthday yet. He was aware that I was single and had no children. He goes, “I really hate to do this. We’re going to have to do Lupron injections. We need to suppress your ovaries.” The whole point of my cancer was that it was almost 100% estrogen positive and then progesterone positive so we needed to have as minimal amount of estrogen coming in as possible.
I remember having to go to the cancer center for the first injection and it was that moment where I experienced PTSD and I didn’t know that it was PTSD. I had to walk through the infusion room to get to where I would ultimately get the Lupron injection. Then they had me wait to see if I had a reaction within that first 20 minutes.
I remember my heart was beating fast, I’m sweating, and I was like, what is happening? I didn’t know that was PTSD but I was getting so triggered by all of the beeping. That’s what people don’t understand outside of cancer land, that if you’re in an infusion room, not everyone gets their own room and you’re hearing all the beeps from the machines and it haunts you. Especially if you had a really tough time with chemo, which I did.
We did the Lupron injection, that first one. I had such debilitating pain to the point I could not walk. My mother had to call Dr. Allen and say, “She’s in so much pain, she cannot walk. She can’t be on this.” Here’s what I loved about him so much, he did not question it. He did not say, “Just have her wait a little bit.” He believed me.
I could not walk. It was so bad. It felt like some of us had experienced bone pain with certain chemos and it’s a horrific pain. It felt like someone had taken a sledgehammer specifically to my legs and broken my bones. That’s the degree of pain I was in. He said, “We can’t have you on this then. I was really hoping that your body could tolerate it.”

Seeking new alternatives to prevent reoccurrence
At this point, it’s getting towards the holidays. I had turned 40. He said, “Let me think on this. You’ve got to break again.” My scans were so clear, I wasn’t going back until another 3 months. When I came back in January from the holidays, he said, “I talked with your gynecologist” who I loved, I’d been with her forever. She had known all this time the issues that I’d had with my ovaries and abnormal pap smears. They talked, and I loved that he did that.

He said, “I talked with Dr. Jeffers, and because of your family history, because your mother had ovarian cancer, because you were already having the size of lemons on your ovaries, you were having a lot of issues, the abnormal pap smears, we feel – and I hate to do this…” He got really emotional, which was lovely to see, but it crushed me too. “You’ve never had children. I always at least want you to have that option to be able to have children. But we really feel that your next step in order to take away the other medications and help prevent recurrence, we need to have a hysterectomy and a oophorectomy.” I was like, an oophorectomy? I never heard that term before. I’ve always heard of hysterectomy, but the hysterectomy doesn’t remove your ovaries. That’s why it’s called a bilateral salpingo-oophorectomy, because it took out both sides, both ovaries.
At that time, I wasn’t thinking emotionally or how that would affect me. I was like, do what you need to do because I can’t go through this again. Let’s just do it. Then I remember thinking, with all the money funneled into breast cancer, do you mean to tell me the only other option is to push me into surgical menopause? At least 20 years ahead of time? That’s strange and that bothered me. That’s what I was focusing on, why aren’t there more options? I don’t understand.
Describe your hysterectomy and oophorectomy
The day after Valentine’s Day, I was like, how appropriate. I’m back in the hospital. That was my first time ever spending the night in the hospital because when I had my breast cancer surgeries, they were on the same day which was insane. I was so panicked, I barely slept the entire time. When I woke up post-surgery, they said, “You might be in the middle of a hot flash.” I had these weird compression things that looked like an astronaut because they went all the way up my thighs and were massaging my legs. When I woke up, I wasn’t in a hot flash. I was in a lot of pain.
When the nurse came in, she said, “Here, take this.” I was like, “How much does that cost? No, I don’t want that.” I was so worried about the cost and that makes me so sad because that’s not what any patient should be thinking about when they are in that hospital bed in pain. With the medications, I was like, “No, I already have that medication. I will take that when I get home.” And here I am, with morphine dripping out of me and my mother’s there. My mother said, “I will speak for you.” I said, “No, I don’t want them to charge me for Chapstick. I don’t want them to charge me for hand sanitizer.” I was so freaked out.
After that surgery, around 2 in the morning, they woke me up and had me walking. They said, “We got to get you walking to see how you’re doing.” It was insane. The difference with this type of surgery was it was robotic. I remember the gynecologic oncologist, she was so tiny. She had tiny little hands and had to get up on a little stool.
I didn’t understand how massive of a surgery that was because I only have 5 tiny scars. They were so small that I didn’t think about just how massive of a surgery that was. It was taking out my uterus, my cervix, my fallopian tubes, my ovaries, all the things. I didn’t think about that. Plus, I still wasn’t a year post-cancer, so I’m still healing from all of that too. In hindsight, I probably should have waited. But we couldn’t wait because we were so worried about the estrogen, and you just don’t know.

How did you feel after that surgery?
You make the right decision for yourself with the information that you had at the time. That’s something my therapist keeps telling me. He’s like, “Don’t get mad. Don’t shit all over yourself. You made the best choice with the information you were given at that time.”
I had to take a week off from work, and I was very panicked about that, because it’s like, God, didn’t I just get back to work? It was a very stressful time.
There was a moment I’m sitting in my living room, and I was told you can’t pick up things. You got to be careful bending. I literally felt my insides, it was so painful. They were shifting because now there was all this room so they needed to figure out where to go.

I got really nauseous. I have a lot of issues now with nausea. Even the Zofran that I took during chemo couldn’t touch it. I guess some of my colon or something, got messed up in there and it was just ongoing nausea. I remember thinking, God, I literally and figuratively feel empty.
Some women are up and doing their thing within 2 days. But I know for my body, whatever the normal person’s time frame would be to heal, I need to double that which is exactly what happened. But no one told me how the insides would shift.
I started to feel back pain. I went in with no back pain. In fact, I went into that surgery, I had lost 65 pounds of weight. I was seeing my shape again because I used to be very fit, slim, and strong. I was so proud of myself coming out of that surgery. Now I’m in surgical menopause, the insides are shifting, and what was this back pain? I did ask, “I’ve got this weird back pain. Is that part of it?” They’re like, “Don’t worry about that. You’re still healing. You’ve got a lot of healing to do.” So again, I was ignored about the back pain.
Were you working around the time of your surgery?
We try all the medications for postmenopausal women. Once again, I had rare side effects and I had just gotten my dream job at a major ad agency. I was so excited. But because all of this stuff is happening, you forget how it’s also affecting your mind with the chemo brain, going under anesthesia multiple times within a span of a few months. I didn’t realize the toll that would take on me.

Those 2 female bosses never told me that I had the option since I was new, that I could take some time off. No one told me that. They said, “You need to make a decision. Choose your health or your work. You can’t do both.” I thought, well, I’m a cancer survivor now. That is not an option for me. It got very dicey, like, I could sue you for that.
I was like, oh my God, I can’t even handle the career that I used to. I used to thrive off of that stress, and deadlines. I felt like I couldn’t do it anymore. It was devastating. That took me about 5 years to recover from because it was 2 women. I was just like, really?
But I was having those side effects. It caused these huge black bruises all over my legs that looked like someone had beaten me. Then we tried another one because that one didn’t work. We tried another one. I tried 6 different medications, both premenopausal and postmenopausal and I had severe reactions to all.
Post-Cancer Complications
What was the next course of action in your treatment?
My dear Dr. Allen said and this is something I’ll never forget, “Megan-Claire, you’re outside of my expertise. I honestly don’t know what else to do so I want to send you to my colleague at another competing cancer center.” Because there are 3 here in Georgia. He said, “I’ve never met a patient where they’re just so sensitive to the side effects and I don’t want to keep causing you harm.” I remember walking to my car and crying. Crying because he has been with me this whole time and he has seen the pain, has seen the struggle, has seen the visible side effects and the invisible side effects.
I went to this oncologist and she said, “I’ve read everything. I’ve read your chart. I’ve talked with both Dr. Allen and your previous active treatment oncologist.” I was like, y’all did your homework. I do not know where she got this stat from but she said, “About 25% of women cannot tolerate any of the medications to help prevent a reoccurrence and they are on nothing.” I wish I had asked what’s your source for that. Also, how many of them were black? Now I want to know the details of that.

I was like, “What do you mean I’m going to be on nothing?” She said, “Your body has been through so much trauma.” That’s the first time I ever heard cancer and trauma in the same sentence. She said, “I hesitate to have you try anything else because of the severe reactions that your body has and you have surgically done everything you can. I think that should be our next course of action, to continue to stay monitored. But you have surgically done everything you can right now.” I left in shock because you never hear that.
Did you feel relieved that you were in a position after surgery to not need follow-up medications?
That was something I thought about. Knowing my risk already, I was like, we’ve already negated me getting 4 or 5 other cancers. But when my dear Dr. Allen retired and all of his caseloads got sent out to different oncologists, I ended up with a Russian doctor. He said, “I wouldn’t have given you chemo” the first time I met him. I was like, you cannot say that to a patient who has experienced so much suffering. Then he said, “I wouldn’t have given you chemo, but I have to say, that’s probably what has kept you alive.”
As I was starting to learn more about lobular, [I realized] we need more research because so many were treating it like ductal. But for him to say that…I really want to tell providers you cannot say stuff like that to your patients when you have seen everything they have been through. It’s written in my chart how it did so much harm to me. I was exhausted. I didn’t even have it in me to look for a new oncologist because I was like, What do I need to do? It was just a really bad time.

He said, “I wouldn’t have given you chemo” the first time I met him. I was like, you cannot say that to a patient who has experienced so much suffering.
Did you eventually switch doctors?
Ultimately, he dropped me in 2018 with no conversation, no nothing. I was supposed to see him yearly. Then my breast cancer surgeon, who’s amazing. She sees me for all of my scans. I remember calling and saying, “I’m supposed to see him once a year.” [She said], “Oh, well, he deemed you too healthy.” I was like, “Well, shouldn’t there have been a conversation? Shouldn’t there be a proper handoff? Shouldn’t you have a conversation with my primary to say these are the things you need to look out for? And if these numbers ever get too high or too low then you need to send her back over here?” None of that happened.
I remember posting that on Twitter. I said, “Y’all, did this happen to anyone else? Shouldn’t there be some sort of conversation with the patient and their primary to have a proper handoff?” Some people said that they did have that and some others didn’t, like me. So to this day, I don’t have an oncologist.
Further complications prompted more time off of work
Fortunately, my breast cancer surgeon and the plastic surgeon are stellar because I had more issues. We’re thinking, all of this is done but it was not done. I kept getting really ill starting in 2018. So ill from trying the medications. In a 3 month period, I ended up in the E.R. They thought I was stroking out. Turned out that I was severely dehydrated. I had my blood pressure go that high.

I drove myself at 2 in the morning because my chest was hurting and I didn’t know what was going on. We tried, yet another medication before all of this. I had such a huge reaction that I got shingles. Shingles are very painful. That was some of the worst pain I’d ever experienced. Two months later, I got pneumonia. I had to take off work. I had gotten a job working as a marketing project manager and I had the best boss ever because I let her know I had pneumonia.
That was when I saw my social worker. I was in palliative care by this point and she had the “come to Jesus” talk with me. She said, “You haven’t been able to allow your body to rest. You’re going to end up permanently in the hospital or dead if you don’t. Take some time off.”
That and pneumonia scared me enough that I called my boss and I said, “I have to take time off.” She asked, “When do you need to take it?” I said, “Now.” She goes, ”Done. Don’t worry about anything.” Her name is Beth. She said, “You go home. You focus on yourself.” I’ve never had a boss like that before. She always supported me, amplified me professionally. She saw the talent, but she was like you need to focus on you.
»MORE: Working During Cancer Treatment
Were your finances affected during this time?

It was hard financially because when you do that, FMLA saves your seat at work. It protects your job, but you only get a small portion of your salary, and I had to pay for my insurance out of pocket. I felt I couldn’t do another Go-Fund-Me, because when people hear that you’re a cancer survivor, they’re like, “Well, what do you need help with?”
I had to take out a loan to keep myself afloat for 3 months because I had to have yet another surgery at the same exact site where my cancer was because I had fat necrosis, which can happen when you get a lumpectomy.
Describe your fat necrosis surgery
It was palpable. You could feel it and it was in the exact same location where my tumor was. My plastic surgeon said, “I know this is messing with your mind, but I promise you it’s not the cancer.” I’d massage it every day, multiple times a day to see if it would go down, but it never did. And I kept getting so ill. I was like, something’s going on.
Luckily, insurance covered 100% of that surgery. Again, multiple surgeries and we go in. We thought it was just going to be a simple surgery. He was going to go into the same scars and pluck it out. As usual, I have to be extra. It turned out that not only did I have fat necrosis, but a hematoma had formed from the original quadrantectomy. When they took the quadrant out, it had attached to the fat necrosis and had formed a crystallized ball. So instead of taking out what we thought was as big as an egg, it was actually the size of a small water balloon. That was how he described it in his surgical notes.
It had gotten into my bloodstream. That’s why my system couldn’t seem to catch up. Ever since he took that out, I haven’t been ill like that since. But it turned out to be much more complex, much more painful than I thought it would. I’m still in shock.

I said, “So when are these scars going to disappear? Because I look like a railroad track.” And I’ll never forget Dr. Mackay. Such a great, gentle plastic surgeon. He took my hand and said, “Megan-Claire, You remember the movie Titanic?” I was like, “Don’t tell me I’m going to be like Rose, what’s happening?” He said, “You remember how big that iceberg was? How massive it was at the top. I want you to think about how massive it must be below if you’re seeing what it is up top. That was your cancer. That is this experience. There was so much that we had to take out, rearrange and reduce with multiple surgeries. These scars are forever.”
You can only process so much. I think a lot of people think, lumpectomy, that’s easy because a lumpectomy with radiation is the equivalent of a mastectomy. You still look like a railroad track. And when he said that, it was so clear to me just how intense all of this was.
What led you to your current primary care provider?

I’m getting teary-eyed talking about this. I really adore my breast cancer surgeon and I adore her PAs. They all have similar personalities and so they monitor me. I actually divorced my original primary care provider and I got another one. This time, I did seek out a black doctor. That’s what’s hard too is to find specialists who are of color and who you mesh with because they can be any color, but you still need to feel that they’re a good fit.
She’s the one that helped me with the back pain because I said, “No one is taking me seriously with this back pain. No one is taking me seriously with this fibromyalgia. Even as I’m talking to you right now, I am in pain. I’m in pain 24/7.” Since that time, I am still monitored. I go now every 6 months and I rotate between an MRI, a diagnostic mammogram, and an ultrasound. It’ll be 7 years, come October. My next scans are in October.
With the back pain, we finally got to the root of that. After going to multiple doctors, I was told by one white neurologist, a white male, “Have you tried Aleve?” I was like, “You can clearly see that there’s a tear near the nerve.” I’ve learned how to read X-rays. I was like, “I would not be sitting here if Aleve worked. Can I have my discs?” And I walked out because I was so livid, like, how dare you say that to me? I had to give myself time to recover from that.
When I found my new primary, she said, “You’ve got so much going on.” It was like a 2-hour appointment. She did not rush me, and I know she had other patients, but she was present. She said, “I think we need to tackle the back thing first.”
What helped your back pain?
Finally, this has been 6 years in the making, we figured out what it was. It’s actually my facet joint and my lower lumbar. It’s near the nerve and there’s degenerative arthritis. Cancer rapidly ages you. I was like, how old am I? 500?

I’ve gotten spinal injections awake. They did try and give me anesthesia and I was like, “This isn’t working.” They’re like, “Oh my God, you’re awake.” I said, “Yeah. I feel everything, y’all.” Then we tried a nerve ablation, burning the nerves. We thought that would work and it only gave me about 4 months of relief. I can tell the latest round of injections is starting to wear off because the pain is starting to increase. I’ll have to go again and get more injections.
What has your quality of life been like with chronic pain?
I was told to just try yoga. I was like, you mean to tell me maybe if I had been believed when I first had that pain, maybe we could have stopped all of this and I could have done yoga? Maybe that would have helped. That’s why I’m bigger, the weight gain, because of all the menopause.
Also, my brain can’t distinguish between whether I’m hurting myself or not because fibromyalgia is running all through me. It feels like a radiating burn. The back pain is in a very specific location, every single moment of every single day. Then, trying to work on my neuropathy. It was just so many things. So when everything is flaring, I get headaches a lot. I’m exhausted.
I didn’t realize how much pain can take over your life until I got like that. That bit of relief from the spinal injections, I was like, oh my God, I actually have energy. I can sleep, I can do that. My God, how have I been existing?
I am single and I’m also a caregiver for my mother, who is still extremely independent and snarky and brilliant. But when she needs me, take her to the hospital when she needs a blood transfusion, when she needs a this or needs to that, I’m having to do that. But there’s not a me to help me out when I come home. So it’s really hard.
How long did you experience relief with spinal injections?
About 4 months and that really disappointed me. Before you’re eligible for nerve ablation, you have to have 2 rounds of those spinal injections to make sure that they actually take. If you don’t feel any relief, then you’re not eligible.
Normally my pain sits between a 6 and a 14. It was like a 1 because I could still feel it a little, but I was like, oh my God, this is a miracle. I finally was able to get the nerve ablation. And that was very weird too, because you do have to be awake for that because as you’re burning the nerve, they have to make sure it’s not going down your leg. I thought this is great, but I thought I would get a year of relief. Even the doctor that performed it, was surprised that it wore off as quickly as it did.
Reflections


What’s something you wish you knew earlier in your cancer journey?
I’m angry that no one set me up with the knowledge that I may never get my quality of life back. That sucks. “Here are some things that we can do to try and help you deal with that.” With all of this stuff happening physically and to my nervous system, I still have a job to do. I have to work full-time.
I’m a creative and I naturally have a lot of energy. I wear myself out just being me. It’s really hard. I got bills to pay. I got my cat, my son, Nathan Edgar. Baby Natey. I got to take care of him, make sure he’s got his food. But I never feel like I get to rest. I want to travel. I want to own my own home, but every time I have savings, I think to myself, don’t spend it because something else might happen with your health and you might have to take off work. That makes me sad too, because I am doing a bit more living and not just existing, but it’s a lot of pressure on my shoulders. I can’t really pursue my true dreams of what I really want to do, which is to be on stage 24/7 because I have to make sure I have money and insurance for my 10 million medications, surgeries, and other procedures that just go on and on and on.



This isn’t going to happen to everyone. That’s what I want to be clear about. I think patients would just like to know the potential. If something does happen or we get some sort of side effect, then we can say alright. Other patients have said this in the past. This is normal or this isn’t normal.
Being self-reliant as a single person with cancer

I find that in a lot of conferences and things that I attend, every speaker starts out with, I think of my family and my kids. Do you think about those who will never have that? I feel very left out being single, and I don’t mean divorced and now single. I mean single. I don’t date. I don’t go out because I don’t know how to not talk about this. I’m in pain all the time. I can’t make small talk or put myself out there emotionally for rejection. Because I’m bigger now, I have that insecurity.
I think people really don’t understand how hard it is. It’s hard enough being in this country, being black, and being a woman. And when you’re diagnosed at a younger age and you have all of these issues and you’re still trying to have a career, you also need to pay all the bills and be prepared for other medical emergencies and always have insurance. And the fact that insurance is tied to employment.
I can’t really go and pursue the creative stuff as much as I want to because, having to do everything myself, it’s a lot.
I’m normally smiling but it’s through my writing that people really got to know me, and that’s where I was able to get some of this out. I’m still here but I really wish I had my quality of life.
What do you want to tell people on their own cancer journeys?
A lot of us post-cancer have a lot of issues because that’s when we start to learn about the long-term side effects of all the toxic treatments and multiple surgeries…It’s exhausting so make sure to give yourself breaks.

Trust yourself and always remind them that [the doctors] are not the only ones making all the decisions. They can make suggestions for you, but it’s up to you to decide, is that the way I want to go? Ask them, “Is this what you would recommend for your sister, your mother, your daughter, your cousin?”
If you feel more comfortable with the nurse, it is your right to say, “Can I have your nurse come in while you’re talking?” Or speak with them after. If a doctor’s feelings are hurt, that’s their ego talking. Because at the end of the day, you need to be armed with the information about your specific case so you can make informed decisions. It’s about making informed decisions together. It is a partnership with your medical providers.
A lot of us post-cancer have a lot of issues because that’s when we start to learn about the long-term side effects of all the toxic treatments and multiple surgeries. Now you have new health issues. It’s exhausting so make sure to give yourself breaks. Your quality of life matters. I often say, cancer cannot take away the essence of you. God, I’m really crying here. It can’t take away the essence of you.
What has helped you along your cancer journey?
Though I still feel frozen financially and get scared because it all falls on me, I’ve been dating Atlanta, Georgia for 2 years. I do go to certain things when I can stand or I can walk. I do have an awesome pink cane on the days I’m feeling potentially wobbly, but I am doing things that may not be the thing that truly brings me all the joy, but I’m still able to find it. I just wrote a blog titled Finding Pockets of Joy. I wish there could be more, but I am finding that and that’s how I can actually have a genuine smile and feel like I am somewhat living.

I’m still enjoying the things around me and finding others as a support system like my friends in the cancer space who I’ve met in person or who have been virtual. It’s amazing, the community and the connection, but also there’s racism in that too, and how hard that can be sometimes. There’s just a lot that weighs on a person like me but you can push through it.
Extend yourself grace. It’s okay to take a break. It’s not being selfish. It’s okay to take some PTO. I shut down. I do not answer emails when I take PTO, that is my time. You’ve got to actually make yourself the priority because, without your health, you got nothing.
For the single people, the truly single people who don’t have kids, it can be hard to find others. Protect yourself. When it’s time for Mother’s Day or Father’s Day, recognize that there is PTSD that goes with cancer. Sometimes I can’t handle going through the children’s section at Target. You’re going to realize there are certain triggers for you. Once you learn what those triggers are, you can avoid them.
More importantly, find a therapist or a psychiatrist or someone to talk to about this who is objective. My therapist specializes in cancer and chronic pain. I know it can be hard to find people that you fit with and that’s the same with therapists. He had to audition for the coveted role of Megan-Claire’s therapist and he won it. You’re worth it and it’s too much to go through by yourself. Your family, as much as you love them and they love you, will not fully understand why you’re still struggling when it’s months and years post-cancer. So it really is important to find someone to help you process this and it is ongoing.
»MORE: Cancer and Mental Health

More Breast Cancer Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Symptom: Lump found during self breast exam
Treatments: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Symptoms: None; caught by delayed mammogram
Treatments: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Symptom: Lump in right breast
Treatments: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Symptom: Lump found on breast
Treatments: Lumpectomy, AC/T chemotherapy, radiation, hormone therapy (Lupron & Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Symptom: Lump in breast
Treatments: Chemotherapy, double mastectomy, hysterectomy