Barbara’s Stage 3 Colon Cancer Story
Barbara shares her stage 3 colon cancer story, which began when she was just 42 years old. She details undergoing surgery to remove her colon (colectomy), how she got through recovery, and her 2 treatments with chemotherapy.
In her story below, Barbara also highlights navigating life after her colon cancer diagnosis, including how she advocated for herself as a patient, how she was able to ask for the right support, managing through scanxiety, and transitioning into survivorship.

- Name: Barbara M.
- Diagnosis: Colon cancer
- Age at DX: 42
- Staging: 3
- 1st Symptoms:
- Stomach discomfort
- Hard to eat
- Family history wasn’t flagged. When it was, sent immediately for colonoscopy
- Treatments:
- Colectomy (surgical removal of colon)
- Chemo
- FOLFOX
- 12 rounds of infusions: 6 months, every 2 weeks
- CAPOX
- FOLFOX
- Diagnosis
- What were the your symptoms?
- You had to advocate for yourself to get diagnosed
- You encourage others to push for testing
- Laundry list symptoms leading up to the colonoscopy
- How long does it take to book the colonoscopy?
- How long does it take to get colonoscopy results?
- Describe the moment you got the cancer diagnosis
- When did you go to the hospital after the diagnosis?
- How did you process the diagnosis?
- How did you share the news of your diagnosis?
- Message to patients, especially women: conserve your energy
- Colonoscopy & Colectomy (Surgery)
- Surgery Recovery & Cancer Staging
- How is the recovery from the surgery (colectomy)?
- How is the physical recovery in the hospital?
- How do you go back to eating solids?
- How long does it take to get the results back on the cancer stage?
- How do you process the cancer stage news?
- Describe your treatment plan
- How do you tell your kids you have cancer?
- There’s no “right” way of sharing a cancer diagnosis
- Did you get a port or PICC line?
- Chemotherapy & Side Effects
- Mental & Emotional Impacts of Cancer
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Yes, there’s a lot of things that are out of your control, but there are things that are in your control. Do your best to make good choices.
It’s an 80-20. 80% of the time, choose positivity; choose good stuff; choose smoothies, supplements, and detoxifiers; choose to surround yourself with people with positive attitude, optimism, hope, love, laughter, light.
Those are in your control.
Barbara M.

Diagnosis
What were the your symptoms?
Slowly over time, I found it very hard to eat. I’m always hungry. I always like a good meal. But I found it really hard to process food.
Things were just sitting in my gut. It was starting to get really really uncomfortable.
Then I just started to take out wheat and dairy and puree my foods, getting a real sense of, “This is not right.” We all have intuition, and my intuition was like, “This ain’t going well, Babs.”
You had to advocate for yourself to get diagnosed
The reason why I don’t mind sharing my story about being a colon cancer survivor is I was dismissed over and over again. I am 5’2″ and the right BMI. I do triathlons, I run, I walk to the office, and I do not present as somebody who could possibly have colon cancer.
We have this preconceived notion — which was right in another generation. It no longer is applicable. But in the generation I grew up, colon cancer was something that was more in the older male, overweight, poor lifestyle very prevalent in that demographic, per se. A young female who ate right and exercised? I really just didn’t fall into that category.
Unfortunately, because of people’s bias or doctors’ bias, I was very much dismissed. It was IBS. Take out dairy. Take out wheat. Try to drink more fluids. You have hemorrhoids.
I was dismissed with anything, except for, ‘Why don’t we explore deeper.’ It was really frustrating.
What happened for me was I actually went to several doctors. I went and pulled my reports after this whole experience. I had written down to my primary care doctor that my father had colon cancer, and it wasn’t flagged.
It was really sad because then I went to an alternative doctor, because I decided I needed some “voodoo,” go off the beaten path. Give me some supplements. Somebody help me. She looked at me, and she goes, “You’re 42, and your father had colon cancer.”
She’s like, ‘You needed a colonoscopy 2 years ago.’
She pulls out her pad and pen and writes me a script for a colonoscopy. Fortunately, it was then at 42 years old that from the colonoscopy, I was diagnosed.
»MORE: How to be a self-advocate as a patient
You encourage others to push for testing
When I would go in to see these doctors, they’d be like, “You’re fine.” I was like, “Great, I’m fine.” I was very quick to take that answer. I was not very assertive or very confident in my own self diagnosis.
I don’t think I knew anybody with colon cancer except my father, who was labeled with colon cancer, but was actually colon cancer, stage 0. They found a mass that didn’t show any cancer cells, and it was more of a tumor in his intestines that they removed, the same way they removed mine.
I share because some people might be like me, they might identify with what I’m saying, and this might resonate with them. As soon as she told me I was okay, I was like, “Oh, I’m okay. The doctor told me I’m okay. I went. I checked. I’m clearly okay.”
A little bit of that is on me, because I was like, “Well, great. They said I was good,” even though intrinsically I was like, “Yeah, no, this is not good.”
Laundry list symptoms leading up to the colonoscopy
Summary: Lethargy, easily tired
I started to become more and more lethargic, and my energy levels started to decline. Again, I’m to blame in this capacity. I blamed it on 3 kids. My youngest was 4 years old. She didn’t enjoy sleeping; sleeping was not her jam.
I was struggling in my marriage and balancing everything. It was a complicated time. Actually, it was just life. It was a chapter in my life. Being tired could have been chopped up to anything.
In retrospect, I ran the New York City Marathon. The kids were really young. 2005. Then I ran the marathon 5 years later in 2009, and I remember in ‘09 I could not get the wind in my sails.
Anybody who’s an exerciser that’s listening to this, you know that when you first start working out, it’s brutal. You’re like, “I am so winded, and my lungs hurt, and my heart hurts, and my toenails hurt. Everything hurts.”
You start working out, and every piece of your body all of a sudden is speaking a language that you didn’t even know. It’s tough.
But once you start building muscle and muscle memory and you get more conditioned, all of a sudden, that 3-mile run becomes very easy. You’re like, “Okay, I’m gonna go out and run 3 miles.”
I have to tell you, throughout that entire training period, I kept waiting for that ease of, “I should be able to run 5 miles. I should be able to run 10 miles.” I had been training. Never once did I hit that. Every run was so hard.
I was training for a marathon, but I’m really just speaking to that baseline. I never hit that baseline. I couldn’t build that when my body was fighting cancer.
We’re tired. We’re parenting. We’re juggling aging parents. We’re juggling jobs. We’re juggling, you know, infertility. I don’t know. Everyone is juggling.
Please understand you are juggling things, but tune into your body. Even though you are juggling a million things, we all know our baseline or energy baseline. We just know our baseline, and now I’m back to that baseline — not that I’m running any marathons anytime soon. I actually lost the will to do that.

How long does it take to book the colonoscopy?
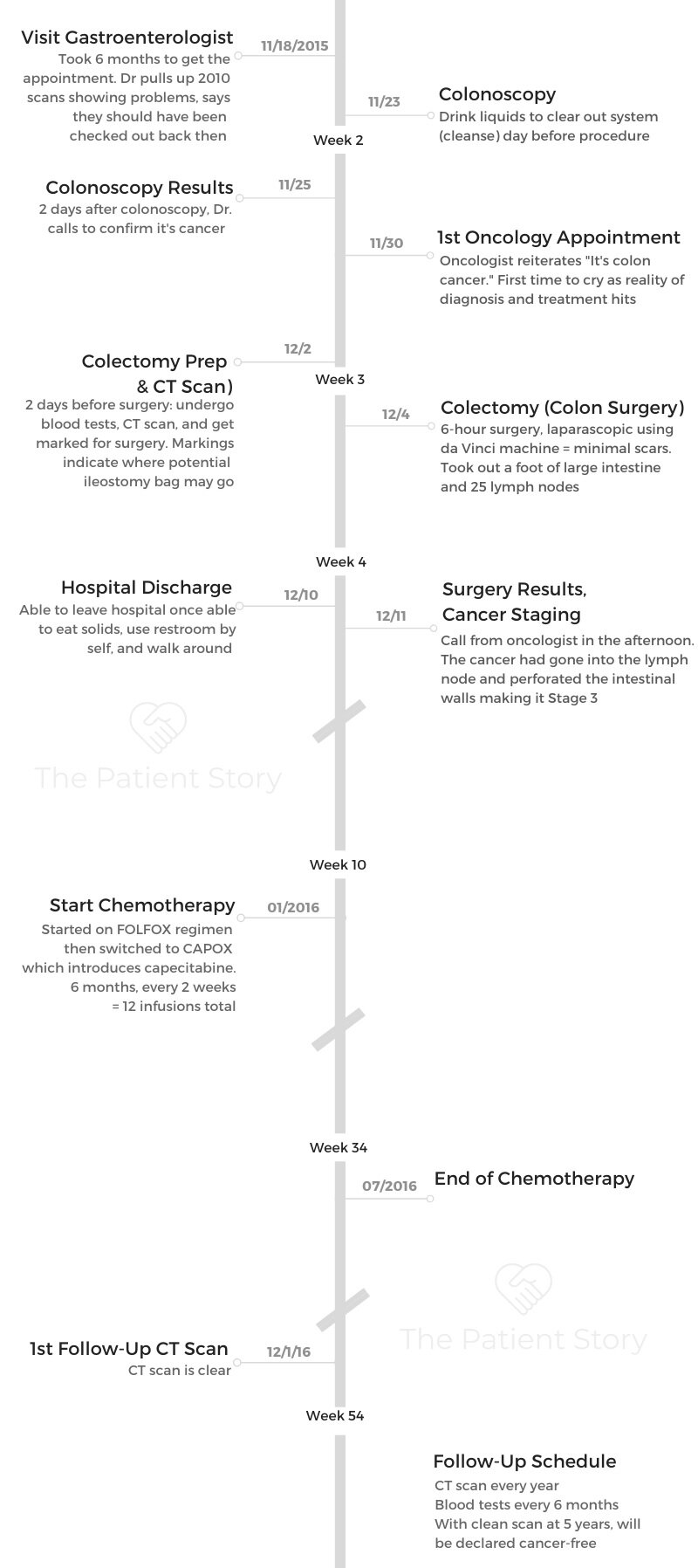
What was crazy about that was a couple things. I couldn’t get an appointment for 6 months. They called me the week before this appointment. You have to meet the gastroenterologist first, and then they scheduled the colonoscopy. It can be a really long time, and for some reason, gastroenterologists are really popular doctors.
I struggled to even get that appointment. Then the week before, they’re like, “Are you sure?” Almost as if enough time had gone by. Did my situation work itself out?
I remember saying, “Yes, I’d love to cancel. I don’t really want to talk about this. I am in the middle of a divorce now.” I remember being curmudgeon-y. I could feel energetically I was like, “Of course I don’t want to show up.” But yeah, I’m coming in because a higher power was like, “Babs, you’re going in!”
I show up, and she pulls a scan that I had from 2010. What happened then was I was having such severe stomach pains that I actually passed out in front of my children and was taken by ambulance to the emergency room. They did some scans. The scans showed that I wasn’t processing food correctly.
Then I’m in the gastroenterologist office in November of 2015. She pulls the scan.
She goes, ‘You shouldn’t have been discharged. Something’s wrong, and I want you in for a colonoscopy tomorrow.’
I was like, “Tomorrow? I have 3 kids and 3 places. I’m in the middle of a disastrous marriage. I have pickups.” I had a tennis thing in Florida that weekend, and I was like, “Hard pass. You need to prep, and I’m not prepped.”
That was a Wednesday, and that Monday, I booked the colonoscopy.
How long does it take to get colonoscopy results?
It went from zero to cuckoo in a really short amount of time. I had the colonoscopy on Monday. She was like, “Something’s there. We tattooed it. We’re gonna send it off for pathology. You’ll get the results in a couple days.”
Describe the moment you got the cancer diagnosis
She called me that Wednesday, 2 days later, and I’m at the pickup line. I’m picking up my middle child at the time, who was in fourth grade, and I’m thinking of him and his 72 friends, because this is what I do. I am like the Pied Piper — all the kids in my car, everybody to my house, snacks are on the table.
She calls me and asks if I can talk. I was like, “Of course.” Because I’m a mother, I multitask. I would never know how to just sit and have a conversation with anybody.

She’s like, ‘The pathology came back, and it’s cancer.’ I was like, ‘Okay, can you hold on?’
I’m screaming out the window for the kids. My car’s over here, and the boys are piling in. She keeps talking, and I’m so in shock that by the time I drove home, which was a mile and a half away from my kids’ elementary school, I decided I did not have cancer and it was pre-cancerous. I was cancer-free, and my husband, their father, at the time, called into my office.
I was like, “The gastroenterologist called, and she thinks it’s a little cancer-y.” He said, “Oh, so it’s not that serious.” I said, “No, no, it’s not serious. We’re just gonna have to remove it with surgery, and it’s not a big deal.”
When I tell you the stress I was under was too much that I was like, ‘I can’t have cancer right now because I just can’t. My kids are too young. I’m too healthy, and my marriage is a piece of garbage. So I’m going to say that cancer — we don’t have time for that. I’m gonna take a pass.’
When did you go to the hospital after the diagnosis?
That was Wednesday. That Monday, I’m at Sloan Kettering Hospital, and the doctor is sitting there. They call me in, and I’m still telling everybody, “It’s a little cancer-y. I just have to have a little surgery. It’s not anything serious.”
I’m sitting with the doctor, and he’s asking me about my bathroom habits and all this stuff. I put up my hand. Their father at the time was with me. I was like, “Can you just leave? I don’t really want to talk about this in front of him.”
He leaves, and the doctor looks at me. He’s like, ‘You know why you’re at Sloan Kettering?”
I was like, ‘I did. I have to have surgery to remove something that’s not supposed to be there.’
He’s like, ‘Honey, you’ve got colon cancer, and you’ve got a long road ahead of you.’
I was like, “Oh.” It was the first time I actually heard it. I started crying. I texted the husband, “I’ve got cancer. You’ve got to come back in here.”
How did you process the diagnosis?
I’ll never forget, because he just looked at me. It’s like, “Do you realize you’re at Sloan Kettering?” I was so out to lunch. I wish there was a video camera on me. I must have looked like the biggest space cadet suburban mom that you can think of.
I call myself a delusional optimist because I just think everything’s gonna work out, and things are gonna be great. I just really like being my positive self.
It was a hard pill to swallow of what I already am dealing with: a bad situation with the marriage. I just really didn’t want to. I just couldn’t. I was like, “This is a little too much for me. I’m gonna take a pass. Is there something else on the menu? I’ll check it out.”
My emotions were all over the board. It’s like life interrupted. It was really shocking and scary. I really wanted to talk to somebody who had colon cancer, and I didn’t have access to a single person.
What you’ve got to understand is my dad had what they labeled as colon cancer, but they were like, “Oh, we’ll remove it in a month.” It was the label of it just was a tumor. It wasn’t like I could call him and be like, “What lies ahead?” We obviously had different pathologies.
How did you share the news of your diagnosis?
Emotionally, I was really all over the place, and I knew everybody was waiting. I was slowly texting people. I am a phone person. I’m really friendly, but sometimes what you need to communicate needs to be in your wheelhouse. I have to call everyone, and I have to [do all these things].
There’s no right or wrong. It is your diagnosis, and it is your experience. For me, I did not feel like dealing with the emotional wreckage on the other side of a phone or making a series of phone calls.
I basically texted a handful of people that I felt were more like the gatekeepers and let them disseminate the information. I had a lot of control over that because I was like, “This is really not for the public. This is not a Facebook post. I know you guys know I’m going through a lot, and I know you’re waiting for this appointment. This is the diagnosis.”
The reason I share that is I understand your audience is going to be maybe caregivers or people just entering into the phase of getting a diagnosis. You need to know that the way other people perceive it is not your problem. You do as you need to do, and I needed to just communicate through texts.
I didn’t want to talk on the phone. I didn’t want any FaceTime. I don’t want any public posts on Facebook and Instagram of like, “Pray for me.”
I had to do it my way, and my way was through a text. My parents got a text message. I wasn’t in the mood. I was in shock. I was scared. I was annoyed.
You know, I found that feeling a lot. I was very annoyed. This is annoying. I have things to do. I have the Christmas concert coming up for my daughter and my sons. I had Hanukkah.
I was like, “How rude. Cancer is the rudest thing. Just comes whenever it wants. It just shows up on your front step. Did you call ahead? No. Nothing, not even to save the date. Are you kidding? It’s so rude.”
»MORE: Breaking the news of a diagnosis to loved ones
Message to patients, especially women: conserve your energy
I find women were like, “I don’t want to hurt their feelings, so I better call them.”
Oh, stop it. You don’t feel like calling anybody? You just got permission from Babs over here to tell you you don’t have to call nobody. I did it my way.
Who is that? Is that Frank Sinatra? I did it my way. I was like, ‘You don’t want a text message, and that was rude? Okay, good. I’m rude. So is cancer.’
I’m fortunate I had that much sensibility, because I’m usually so sensitive about, “Are they going to be upset if I just don’t call them?” Fortunately, that moment, I was like, “You know, they’re going to go out and have to deal with their own mishegoss” — that’s a Jewish word for their own craziness.
At the time, I was with the surgeon, and I didn’t get to be in oncology until after the pathology, when they removed the intestines.
Colonoscopy & Colectomy (Surgery)
What’s the colonoscopy like?
They can’t do the pathology from that point, but they can identify a polyp that has already progressed past a stage that they can remove it. I don’t know what that looks like. They sent me a picture. I was like, “I don’t know. It looks good to me.”
It’s so funny. They give you your pathology pictures or your colonoscopy pictures. The colonoscopy is a pain in the neck. It’s just an inconvenience the day before because you don’t eat, and some people do pills or some liquid drinks. Everybody’s got their own cleansing process.
People overdramatize it. The colonoscopy is just you clearing out your system. It’s not that big of a deal. You’re going to feel cute and skinny the next day. People just overdramatize everything, and then you show up for your colonoscopy. You go to sleep. It’s overdramatized because people want more of a story, but I am so black and white.
I don’t want to scare people. “I’m scared about a colonoscopy. I’m scared about the prep.” There’s no service in me dramatizing a day where you just drink liquids. It’s good for your body; it’s good for yourself. It’s good for your organs to flush your organs out with liquids and to really purge your body of toxins for the day. Fasting and cleansing is a really healthy way to live.
I recommend it as something to do every 6 months. Just take a day off from overwhelming your system. It’s definitely more in my wheelhouse to dial it into a space. It’s really not a big deal.

I had somebody text me once when I was in the middle of chemo, and they’re like, “I’m really afraid of the colonoscopy.” I was like, “I don’t know what to say.”
I remember just being really honest, saying, “You do realize I have to go sit in the hospital for 7, 8 hours, and then I have to go spend the night in a New York hotel, throwing up and being away from my 3 kids, being unable to drive a car.” A colonoscopy to me is so entry level. It’s like a finger prick for some sort of blood test.
It’s not that it doesn’t warrant the attention. It’s getting in a negative space.

How do you handle the waiting time before the surgery and knowing your cancer stage?
It was mid-November. I got to have Thanksgiving with my family. By that time, I knew I [was getting] the surgery December 4. There wasn’t much time in between colonoscopy and surgery. There was Thanksgiving in there. That’s what I remember, because we had gone in to see the Thanksgiving Day Parade.
A good friend of mine played for the New York Giants, and he was in town. It was a really exciting time, but there was a wet towel over all of us because there’s a lot of unknowns. It was really just the unknown. That is really a hard space.
Once you have your diagnosis, it’s a little bit easier dealing with facts, not fear. When you don’t have the facts because you’re in the space of, “I haven’t gotten my surgery yet. I don’t know the pathology. We don’t know the stage.”
I didn’t know if I was getting chemo. That was actually the hardest psychologically because I was like a ping-pong ball. A yo-yo. I vacillated between, ‘This is just going to be a surgery. I’m just going to bang it out like my dad. I’m going to be back in the swing of things, and I’m going to be skiing in mid-January.’ That was one that was Barbara, delusional optimist.
And then “Doom and Gloom Barbara” was, “I should write my obituary right now and get my affairs in order.” It’s like there’s no middle ground in the space of “I don’t know.” The space of “I don’t know” is really polarizing, traumatizing. It ages you.
Everybody’s going through it with you, but it all manifests differently. Your family’s going to act weird. You’re going to act all sorts of — you’re going to be cuckoo. That, to me, is a really tough space.
»MORE: Patients describe dealing with scanxiety and waiting for results
Describe the lead up to the surgery (colectomy)
Leading up to the surgery, I didn’t have a lot of people to talk to. I will say that my dad had had the same surgery but a different surgeon, and his process was different. I had the da Vinci machine. Mine was laparoscopically done, so I had like 5 incisions on my abdomen that were very minimal.
I would be happy to share if anybody is [reading] that is gearing up for this; I will FaceTime you and show you what the results are. Because if you saw me, the scars are so minimal. You would never know that I literally was gutted, and so I’m really really grateful for that.
I didn’t have a lot of people to talk to, so I just had unanswered questions. I couldn’t find anyone, so I just had to surrender to all this unknown.
I was sad because I had a lot of delusions about the surgery. It was coming up on Hanukkah. I’m Jewish; my husband is Catholic. We celebrate all the good stuff. Hanukkah was that week, and I brought in chocolate dreidels into the hospital, these giant chocolate dreidels. I thought as soon as I had the surgery, my kids would come in and visit me in the hospital. We can do dreidels, and we can have a good time. I mean, talk about delusional optimism! That’s like me in a nutshell.
Pre-surgery, I just didn’t have a lot of information. My dad was apprehensive to share his experience. He’s like, “Look, I’m fine now, and yours is going to be different surgery.” I guess I didn’t know what questions to ask.
2 days before surgery, you go into the hospital, and you do a series of blood tests and all this stuff. You’re on different floors, and I don’t know where I was. I was all over the place, all over Sloan Kettering for this, for that.
It’s an all-day. It’s so exhausting. Then at the last stage, they mark you for surgeries. You lift up your shirt, and they’re putting this black sharpie that isn’t going to wash off.
She’s like, ‘Where do you wear your belt?’ Then she draws this big black circle underneath my belt line. I was like, ‘What’s that?’ She’s like, ‘There could be complications.’ I don’t remember exactly what she said, but what [I think she was saying] was I could have a bag attached to me for my waste. It’s called an ileostomy bag.
I had those markings 2 days before my surgery, because then the next day after the marking day was a starvation day. You don’t eat that day either. On colon cancer, you’re gonna get really used to not eating.
They have to clean out your system, so that whole day, you’re drinking fluids. I don’t remember there being a preparation or anything, but I could be wrong.
Processing the news of the ileostomy bag
All I heard was a shitbag. To me, I was like, “You’re marking me. You’re literally marking me right now for a bag of poop. My marriage is done. I’ve just been diagnosed with cancer. I have 3 kids. My kids are 4, 10, and 12. And now somebody is marking me for a poop bag. I can’t. I cannot. I cannot. I cannot believe this.”
I was like, “What do you mean? I don’t understand. Am I gonna wake up with a bag attached to me? Does this bag go back? How does this bag work?”
That one was a doozy. I’m not gonna lie. I was very frightened. I need to be truly honest. I’m probably a little more on the vain side. I try to take care of myself. I was about ready to become a single woman and start dating, and I was like, “That’s gonna be something to talk about on a first date. ‘By the way, I have 3 kids and a poop bag.'” So yeah, I wasn’t excited.
That was a tough one. I just hope I’m not offending anybody with how I internalized that. It could happen to anybody. There are a lot of people out there handling that byproduct of colon cancer very, very well.
Describe what you remember from right before and after surgery
I remember walking into the surgery. They have you walk in because you feel more [hospitalized] when you’re rolling in, but by walking in, you walk in with superpowers, which I appreciate.
Then you land in this bed. When you walk into the surgery unit at Sloan Kettering, it is like out of a movie. There’s these huge televisions and state-of-the-art technology that was in this space. I was blown away. It looks nothing like an emergency room or hospital room. I had never been in a surgery center like that. It was really impressive.
I felt like I was in good hands. You lay down. They say, ‘Count to 10,’ and they’re talking to you. The next thing you know, you don’t know anything.
The surgery was 6 hours. Mine was laparoscopic. They have 5 incisions. They took out a foot of my large intestine and 25 lymph nodes, and then they put the intestines back together.

Surgery Recovery & Cancer Staging
How is the recovery from the surgery (colectomy)?
It’s a mystery I have zero interest in discovering. I guess they just [put] my intestines back together. They sent that off to pathology. When I came to, I do remember my husband being there and the surgeon.
I don’t particularly remember, but you’re in a fog. You get to eat an ice chip an hour. You go from the day before not eating, and then an ice chip an hour.
I can’t remember if they tried to get me out of the bed that day or that following day. The whole day of surgery is really a wash.
I remember waking up like I was in the best mood. All I cared about was did I have a bag? I was very loving. I loved everyone. I loved the nurses, and I loved the doctors. I was high; I was in La La Land. The pain and the reality did not kick in until the next day. I was hungry.
How is the physical recovery in the hospital?
I was there for what felt like forever. Then the next day, I was really hungry. They’re like, “You get to eat an ice chip an hour.” I had access to my own pain meds through this thing that you click with your finger.
I wanted nothing to do with the pain in my abdomen. I was extremely distended because they blow up your intestines with air — I could be completely wrong. Maybe it’s water or fluid. They blow you up like a Macy’s Day Balloon for a parade. There I am starving, and I look like I’m 19 months pregnant.
I literally look like the worst version of myself. I’m like, “Okay, great.” You’re all blown up, you’re all puffy, and they have you get out of bed. I was on so much pain medicine. I’ve never actually cried from pain, and I cried from pain. This comes from a woman.
I’m apprehensive because somebody’s gonna have to go into this, but maybe go in with open eyes. I delivered 2 out of my 3 kids naturally. The pain from this doesn’t hold a match. This was really painful.
This woman comes in as a physical therapist, and she’s like 83 pounds. It’s like the blind leading the blind. I don’t know how she lifts other people out of a bed, but she did a great job. She got me out of the bed, but I’m sitting there the whole time. I’m like, “You can’t lift me. I can probably lift you.” She was really nice and really sweet.
From there, it was walking. They’re very big on walking.
My first walk took an hour to get around the floor, and it was really painful. I believe I was in the hospital for something between 5 and 6 days. I’m almost positive 6.
They eventually move you off of morphine to oral Advil or Tylenol. I wasn’t eating much. The reason they try to get you off of morphine is because it’s like putting your whole body to sleep, so they want to get the muscles moving in the digestive tract.
How do you go back to eating solids?
I had to show that I could handle food. On the last day, you get to order a meal. You go from ice chips in an hour on the first day. You haven’t eaten for 3 days, then you go to ice chips an hour.
Then the next day is liquid broth, some miso soup or something. Then you migrate up to maybe a bowl of mush. By the way, you’re still 700 pounds, because they’ve blown you up, and it’s the most annoying thing.
You’re starving to death, yet you weigh 7000 pounds, so it really sucks. On the last day, they hand me a menu. It might as well have been from a ballpark, like I had gone to Yankee Stadium. It had a quesadilla; it had a hamburger. It had a list of real food.
I’m a healthy eater. I was like, “Well, I wouldn’t eat a quesadilla. That’s like a party. That’s like I’m celebrating or something.” But it was this real heavy, obnoxious food, and I found that really a little off-putting.
My body just went from as pure as it can be, and now I’m going to throw down a quesadilla and some French fries. Okay.
That’s just modern medicine right now. I don’t know that nutrition has really caught up with modern medicine. I felt if I had been in charge of nutrition and wellness there, it would have been like, “Which of these 6 smoothies are you gonna have?” It would have been filled with ground flaxseed or vitamin C, vitamin D.
That was bizarre. That was the day they let me go home. I was moving very slowly then. I was in so much pain that I couldn’t have my kids come into the city. That was a bummer.
How long does it take to get the results back on the cancer stage?
It was 7 days after, because I got the results on December 11. They didn’t call me until 3:30 in the afternoon. I knew I was getting a call that day. Again, you’re a ping pong ball. You go from cuckoo to cuckoo, you’re fine to you’re dying.
I was at home by then. I remember thinking, “If they don’t call me today, do they go home for the weekend?”
They called and said, “The good news is you won’t lose your hair.” I kind of knew it was going to nosedive from there. They said it has gone into the lymph nodes. It had perforated the intestinal walls. It was stage 3.
How do you process the cancer stage news?
It was the first time I really cried hard. I wouldn’t say I cried hard until that point, because I think I just have a way of believing in and staying an optimist. It’s my nature. I’m a very positive person. It was the first time my balloon was really deflated.
I couldn’t handle the rest. I actually handed the phone to my was-band. He was upstairs, and I said, “You’d better come down. These are the results I wasn’t hoping for.”
Fortunately it wasn’t a stage 4, but it was a stage 3. It had perforated the intestinal wall, which meant it was headed out to the mothership. Because it had already entered a lymph node, it’s not a great sign.
Describe your treatment plan
My doctor said colon cancer is highly curable with 6 months of chemo. I couldn’t stop crying over that. I was like, ‘I don’t have the time for that.’
Your life gets hijacked. It’s a real punch in the gut. That was a doozie. That call really sucked. We decided very quickly it was time to tell the kids.
How do you tell your kids you have cancer?
We didn’t tell my daughter; she was 4. My boys we told independent of each other. First we told my 12-year-old. Then we told my 10-year-old. That sucked.
There’s no right or wrong. I’m not a secret keeper. I didn’t think the kids needed to know if the surgery had gone in another direction.
It would have just been for medical history purposes at some point — that they knew their medical history.
But up until that point, we just were like, ‘Listen, it’s just surgery.’ We kept it very age-appropriate.
As soon as I knew I had chemo, I just couldn’t not tell them because it was going to require everyone’s understanding of this “new normal.” Mommy wasn’t going to be at pick-ups and drop-off some days, and she wasn’t going to be able to do her usual Mommy things. I just needed everybody on board.
It changed the chemistry of my home. I think it changed the fabric of my children’s childhood forever. Cancer’s a very deep word. It’s very scary. All of a sudden, it’s like everyone is dying of cancer. Cancer is a scary word.

I think their innocence was robbed that day. Life just all of a sudden became very real. We had Googled, “How do you tell your kids you have cancer?” I did get some great advice on the internet.
It was make sure the kids know it’s not contagious, that they didn’t do anything wrong. They had nothing to do with it. Speak in very factual terms, but be very optimistic, very factual.
My kids know how strong I am, but I saw them change. It was tough. My daughter knew I couldn’t pick her up after my surgery, but she was 4. She knows now.
She’s seen the scars, but I think it’s important because I don’t want her to wake up one day all of a sudden and be like, “Mom, you had cancer? Is it going to come back?”
»MORE: Parents describe how they handled cancer with their kids
There’s no “right” way of sharing a cancer diagnosis
I just like being transparent. It works better for my personality, and I don’t think I have anything to be ashamed of. I know another woman in my same town that had the same diagnosis.
Everyone was on lockdown not to tell her kids. She had 4 kids, and I was like, “That looks a lot harder. That looks like a lot more work.”
But it’s not up for judgment. You want to send people a text? You want to announce it on Facebook? You do you. That wasn’t my speed at the time. I was very private about it for a very long time.
Until Colon Cancer Awareness Month, which is in March, when I felt a call to service. Okay, this is what colon cancer looks like. This is the face of colon cancer now, folks.
Did you get a port or PICC line?
I refused a port. I just always went in through the arms. I almost shifted gears in the middle of it. Getting the infusions through the arms — man, my left arm, I still [have] PTSD from it. One nurse just couldn’t find the vein! But yeah, I didn’t have a port.
You do you. I just think for me, I didn’t want the scar. I wanted to do it and be done. I didn’t want the port scar.
»MORE: Read patient PICC line experiences

Chemotherapy & Side Effects
Describe the chemotherapy regimen for your colon cancer?
I was on oxaliplatin, which was my infusion. I started on one regimen, FOLFOX, then went to capecitabine. This was a while ago, and chemo does a number on your brain. I believe I went every 2 weeks for my infusions. I had 12 rounds of infusions — 6 months, every 2 weeks. I would only go in for one infusion for several hours.
To say I was sick would be an understatement. I would get violently ill. Then I chose to do the oral chemo, along with the oxaliplatin. You do 2 chemos when you’re on colon cancer. I traded out my FOLFOX for CAPOX, which is capecitabine.
I had to do 7 days of an oral pill, and they were horrible. Everything was horrible. I hated chemo. I thought I had delusional expectations. I had seen people who had lost their hair in other treatments do yoga, SoulCycle, and I couldn’t even drive a car.
What are the chemotherapy side effects?
Summary: neuropathy in fingers, aversion to drinking cold liquids, chemo brain/fog, intense nausea
Neuropathy in my fingers. You had this thing with shards of glass when you drink something. It’s the worst. You drink something, and then you feel the shards of glass. It’s the worst. I actually don’t drink cold water anymore. I don’t like cold anything.
I remember I tried going for a walk with my friend, and it was 2 days after my chemo treatments. I could feel like there was something in my body, almost like the neuropathy you have in your fingers, but it was all through my thighs, legs, my whole body. It was like the poison was going everywhere. My body felt so gross.
Toward the end, I couldn’t string 2 thoughts together. I couldn’t drive a car. I couldn’t focus after my infusion.
I remember once trying to pick up medicine at a supermarket or drug store, and I’m like, “Woo, let me put on my lip gloss.” I was driving and was so unfocused. I thought, “You know what, I don’t belong on the road.” I really struggled with my bearings and my thoughts.
The nausea was blinding. We did the ginger tea concoctions, I tried acupuncture, and I tried massage. I couldn’t do anything. Nothing worked for me. The only time I felt that it could abate it for a little was walking. I think that was more of a distraction than a real anything.
What helps fight the chemo side effects?
I could walk. I did a lot of walking through my chemo. There’s no bad weather, only bad clothing. I walked in the snow. It was my healing. It was my therapy. It was my everything.
Everybody would ask me, “Can we drop a casserole off? What can we do?” I said, “If you want to help me, I walk twice a day.” People would come over once after drop-off and another time in the afternoon, and I’d go through these long walks. I got a Fitbit. I did a ton of stuff.
It was the only time that I felt like I was playing an active role in my recovery. It helped me in my mind.
I’m not saying this is true, but I think in my mind I felt like I was helping metabolize the chemo in my body and move it along. I just felt like I was playing an active role in the process.
My chemo was January through almost July, because I started my chemo late in January. I didn’t like the first place I went. Then I went back to New York.
[It was] 6 months of chemo. Brutal. I hated it. Well, divorce is the worst thing. Chemo is second! For the nausea, Zofran, nothing worked.
What helps move you forward each day?
I watched a lot of HGTV. By the way, now that I’m not in chemo, I don’t watch at all, and I could care less about the Property Brothers and what they did. But during that time, I was obsessed with Property Brothers and Tarek and Christina. I watched that channel all the time.
Once chemo was over, I didn’t remember the station it’s on TV. I couldn’t read. People were dropping off books, and I have to tell you, that was a shock to me when I couldn’t read a book. I couldn’t focus enough.
I couldn’t watch movies. Movies required a lot of attention. I didn’t have an attention span for movies, but I could watch short shows. It was bizarre. I didn’t read magazines or books. It was these short little makeover shows. I wasn’t myself.
What is the follow-up schedule?
Every 6 months I have a blood test. Every year I have a scan.
Mental & Emotional Impacts of Cancer
How can you ask people for support and for help?
I was really fortunate. My parents live very close, and they’re very hearty as well, so they were very involved. My friends were very quick to drive my kids to different places. In the middle of my chemo, I had my car stolen.
One day I went out, and my husband was driving. Both the cars were stolen. I was like, “That’s fun. At least they didn’t come in my house!” Again, I can spin anything. I literally had the best attitude. I ain’t feeling sorry for myself! I feel sorry for that person who thinks this is how you earn a luxury vehicle.
I was really fortunate I had a lot of help. I had a lot of people volunteering. Reaching out to your church, your temple, your groups of friends, and saying, “Listen, these are my infusion days. This is what I might need. Could somebody grab my kids? Could somebody get the groceries?” My neighbor randomly dropped off groceries, and I loved that.
My parents did something really good that went on for a very long time. On Tuesdays, they would go grocery shopping because they’re seniors, and they were very excited about their senior discount. I gave them my credit card, and they went shopping.
I don’t know what the cashier was thinking, like these 2 seniors buying food. I’m a family of 5, and we’re growing humans, so we got into a really good rhythm.

I would say accept your limitations. If somebody wants to come over and do your laundry, let them, because it helps them feel better. They’re scared.
I just did very little, and I didn’t have the bandwidth to do a lot. I was really sick. I did not do well in chemo. I was not at yoga. I signed up for a tennis drill. Again, my delusional optimism. I was like, “Well, I think I can do tennis. Do my infusions, and 3 days later, be at tennis.”
There’s no poster child, and everybody handles it differently.
»MORE: What kind of support cancer patients say helped the most
How do you handle “scanxiety“?
I went into that post-treatment scan really optimistic. I’m on year 4, and I’m no longer that person, unfortunately. Those scans create a lot of anxiety for me. I’ve lost the ability to be my delusional optimist. I have a tough time with the scans.
As delusionally optimistic as I am, those scans throw me off my center every year. I get worse, progressively worse, so God only knows what next December is going to look like.
They say if you make it to year 3 and no markers of cancer, you have a higher probability of it not coming back, so that’s positive.
I would like to try to be as positive as possible, but the truth is I landed a stage 3 cancer diagnosis after a scan and after a pathology report, so I don’t always have access to that [optimism] anymore.
»MORE: Dealing with scanxiety and waiting for results
How is survivorship after cancer?
It is a work in progress. What I really like to share is you can’t control that. You can only control what you can control, so I try to eat right. I try to exercise. I try to really live out loud. I really try to do things.
I went skiing in St. Moritz this year. I’ve taken career risks. I’ve launched a podcast. I’ve gone on television with the Today Show, different programs.
I really know that I can’t control what happens later, like my 5-year scan in December, but I can control the in between.
I think it’s safer and healthier to be like, “Let me just do what I can today to make sure I’m living this great life and being happy, fulfilled, being with my kids. Trying new things and not waiting. Not waiting.”

It’s all about the dash. It’s all about your date of birth (1973 for this lady) and the dash, and then where it ends. You really only control the dash, so what are you doing between now and then?
I just try to live a very positive life. Stay away from things that aren’t serving me and from people that aren’t good for me. Go for it. Book the trip. Spend the air miles. Get out of your own way. Try the new career. Leave a crappy relationship. Throw out what’s not working for you. Invite in new opportunity.
Living in fear of a bad diagnosis — you’ve got to find a good place for that. For me, it’s more motivation of, “I can only do the dash, and the dash is in my power. I’m going to make it a good dash.”
What’s your message to patients and caregivers now?
Keep the feet moving forward. I think being positive, being optimistic, and taking control of what you can is super important. You control your thoughts and what you think about. Try to stay positive, because your thoughts dictate your actions, and your actions really do dictate your future.
In feeding your mind and body with positivity and healthy nutrients, whether it’s health thoughts or healthy food, it allows you to be in the driver’s seat much more than anything else.
There’s a lot of things that are out of your control, but there are things that are in your control. Do your best to make good choices.
It’s an 80-20. 80% of the time, choose positivity; choose good stuff; choose smoothies, supplements, and detoxifiers; choose to surround yourself with people with positive attitude, optimism, hope, love, laughter, light. Those are in your control.
Watch things that are positive and uplifting. Feed your brain. Feed your cells the good stuff. It’s going to make a really big impact on you. Choose to go for a walk. Walking releases endorphins, and endorphins are a mood-enhancer. Your mood, having it positive affects everything, and you look better.
I looked better because I walked. Fresh air, sunshine, vitamin D. All of it is immune-building, so that’s in your control. If you can, I’m not saying everybody can, try to choose the good stuff.
You found silver linings
I hope everyone that’s listening understands there’s light at the end of the tunnel. There’s a lot of silver linings in these experiences. I have a lot of respect for my experience and people that have gone through it.
I hope everybody gets to the other side, because I think your story could help somebody else. That’s what we’re here to do — align with humanity and share collective struggles and experiences to help each other.

Inspired by Barbara's story?
Share your story, too!
Colon Cancer Stories
Jackson A., Colon Cancer, Stage 3
Symptom: Sharp abdominal pain
Treatment: Surgery (emergency transverse colectomy)
Jay W., Colon Cancer, Stage 4
Symptom: Occasional presence of blood in stool
Treatments: Chemotherapy, surgery (installation of port and liver infusion pump, colectomy, hepatectomy, liver ablation, removal of liver infusion pump)
Kelly C., Colon Cancer, Stage 4
Symptoms: Constipation, bloating, severe abdominal pain
Treatments: Surgeries (colectomy, colostomy, hepatectomy), chemotherapy
Marc Anthony S., Lynch Syndrome and Colon Cancer, Stage 2A
Symptoms: Blood in stool, severe constipation, persistent exhaustion, constantly feeling cold
Treatment: Surgeries (sigmoid colectomy, lymphadenectomy)
Crystal W., Colon Cancer
Symptoms: Blood in stool, intermittent severe lower abdominal pain, urinary tract infection (UTI) with strong odor, fistula
Treatments: Surgeries (cystectomy, oophorectomy, and hysterectomy), chemotherapy
Albita G., Colon Cancer, Stage 4
Symptoms: Blood in stool, pain during defecation, constant constipation, steady weight gain in the midsection despite exercising
Treatments: Surgeries (colectomy, hepatectomy, hysterectomy), chemotherapy, radiation