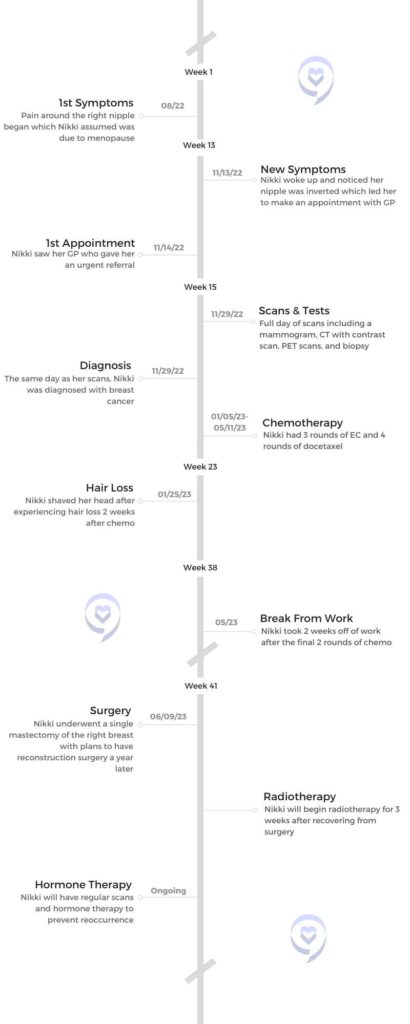
Nikki’s Stage 3 HER2+ Inflammatory Breast Cancer Story
Trouble breastfeeding her newborn son led Nikki’s doctor to investigate previous health concerns, where she discovered a stage 3 tumor in her lymph nodes and bowel.
Years passed after overcoming bowel cancer and new symptoms arose that Nikki assumed were symptoms of menopause until she awoke one morning with an inverted nipple. This led to a secondary diagnosis of HER2+ inflammatory breast cancer.
Nikki shares her double cancer story shortly before undergoing single mastectomy surgery and reveals her side effects from chemo, how she advocates for herself as a patient, the effects cancer has had on her marriage, and how she explained her diagnosis to her 7-year-old.

- Name: Nikki M.
- Diagnosis (DX):
- Bowel Cancer
- Inflammatory Breast Cancer
- Invasive Ductal Carcinoma
- HER2+
- Staging: 3
- Symptoms:
- Centralized pain around the nipple
- Inverted nipple
- Swollen breast
- Differences in nipple color
- Warm-feeling breast
- Age at DX: 47
- Treatment:
- Chemotherapy
- Red Devil for 3 rounds
- Docetaxel for 4 rounds
- Epirubicin and Cyclophosphamide
- Surgery
- Single mastectomy
- Radiotherapy
- Chemotherapy
Try and find joy, as daft as it sounds, because it’s not going to harm you and it might help…When it comes to laughter and joy, I try to find a little bit every day.
Nikki M.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Symptoms & Diagnosis
- Tell us about yourself
- What led to your cancer diagnosis?
- How did you react to your cancer diagnosis?
- Years later, new symptoms arose
- What did you think was causing your symptoms?
- What made you see a doctor?
- Getting a secondary cancer diagnosis
- Experiencing guilt for not going to the doctor sooner
- Did you get yearly mammograms?
- Expanding what we know about breast cancer
- Advocating for inflammatory breast cancer
- Describe being told about your secondary cancer diagnosis
- Quality of Life
- Sharing a cancer diagnosis with family and children
- How has your husband adjusted to your cancer diagnosis?
- What happened after you were diagnosed with breast cancer?
- What cancer treatments were you on?
- What’s your doctor’s outlook on the surgery?
- How did doctors respond to you feeling guilty about not being seen sooner?
- Chemotherapy & Side Effects
- Being A Patient Advocate
- Reflections
Symptoms & Diagnosis
Tell us about yourself
I’m Nikki and I’m a mum of 2. I’ve got a little boy who’s 7 and a daughter who’s in her 20s, so massive age gap. I’m also a teacher, which is a job that I love. My hobbies tend to revolve around the outdoors, so lots of walking and exploring the countryside. I live in Norfolk, which is beautiful. I also love to garden, cook, and read as well.
What led to your cancer diagnosis?
In a way, this treasured son actually saved my life because if I hadn’t been trying to breastfeed him, the doctor wouldn’t have done the investigations.
The very beginning was 2016. I was breastfeeding my son and he was a son that I’d waited a decade for. We were told we couldn’t have children. When he arrived, he was a miracle baby. My daughter used to joke, it was like the coming of John the Baptist. He was a much-treasured, wanted baby and I wanted to do everything right.

I was trying to breastfeed him and he wasn’t putting on weight. I went to the doctor and asked her if I could have some help to increase my supply. She looked at my medical records and said to me, “I’m willing to help you, Nikki, but I’ve looked at your medical records and there are lots of bowel complaints, IBS, and stomach issues. Will you let me investigate further?”
I’d been going to the doctor for years and was told I had IBS, to improve my diet and it would solve itself and it never had. That GP saved my life because she uncovered that I had a stage 3 tumor that was in my lymph nodes and my small bowel. It was a neuroendocrine tumor, which is incredibly rare. I think it’s 1 to 2% of cancers and it’s often mistaken for IBS. Although it’s very slow growing – my tumor was the laziest tumor in the world – they think that it had been there for years and we just ignored it or had been told it was something else.
In a way, this treasured son actually saved my life because if I hadn’t been trying to breastfeed him, the doctor wouldn’t have done the investigations.
I look at that now and think it was a baby cancer because all I needed was keyhole surgery.
How did you react to your cancer diagnosis?
It was scary, particularly in those first few weeks after you get your initial diagnosis where you don’t know how far the cancer has spread. It was scary and it was emotional, particularly because I was diagnosed on my son’s first birthday, which was heartbreaking. I was really angry at the world for a very long time in terms of what I’ve gone through.
Since it was a baby cancer, because of keyhole surgery, it was gone and I’ve been free of that cancer now since 2017 and I have yearly checks.
Years later, new symptoms arose
You would think that would make me more likely to go to the doctor. But in August of 2022, I started to develop a pain in my right breast that went around mainly the nipple. You’re always told cancer doesn’t hurt so I ignored it. I feel really silly that I ignored it, particularly because in my family there was a lot of breast cancer. If you go back 2 generations, that’s how most of the women in my family sadly have passed away or they’ve had it, and it’s been a factor later in life.
What did you think was causing your symptoms?

I spent that summer holiday moaning about the fact that my boob hurt and my husband, probably to shut me up, Googled and said to me, “It’s just a menopause symptom.” That’s what I wrote it off as because I had it in my head, there’s no lump and there’s pain. That can’t be cancer.

This pain continued through the holiday and got really sharp. Again, I thought maybe it was an ill-fitting bra. Your boobs do hurt when it’s coming up to your period or just after. I found lots of excuses to ignore it and I feel really silly.
What made you see a doctor?
I woke up and my nipple was completely inverted and I had a panic.
Towards the end of November, that’s how long I left it, I woke up and my nipple was completely inverted and I had a panic. I was supposed to be doing something big at work and I emailed work this morning and said, “This has happened. I’m not coming to work. I’m going to the doctor.”
I went to the doctor and she said the same as me, there’s no lump. She said, “All I can see is the nipple inversion and that could be a cyst or something. I really don’t think this is cancer, but I can see how worried you are so I’m going to do an urgent referral.” I went home and felt a little bit silly, but I was also convinced that it was cancer.
Getting a secondary cancer diagnosis
Within 2 weeks into mid-December, I had a whole-day appointment at the hospital. The type of cancer I have is inflammatory breast cancer, so it does come with pain. It often comes without a lump. Usually, you also have lots of red rash on your boob and I didn’t have any of that. My only symptom to this day has been the inverted nipple and the pain.
I had a mammogram, but that doesn’t pick up my sort of cancer which is why the risk is so high with my sort of cancer. I had to have a CT contrast scan and I had a biopsy as well. The doctor who did the biopsy said, “Do you want to know? I don’t like knowing things that you don’t know because it’s your body. It’s cancer.”
We didn’t know it was inflammatory, although I think he did know because another symptom is that you get almost what looks like cellulite, that kind of texture on your boob. I’m a plus-size woman of 47. I have cellulite in other places on my body, so I didn’t think anything of it but he pointed that out to me. He said to me, “I can’t be 100% certain, but looking at what we’re taking out of the biopsy I want you to know that I think it’s cancer.”
The doctor who did the biopsy said, “Do you want to know? I don’t like knowing things that you don’t know because it’s your body. It’s cancer.”

Experiencing guilt for not going to the doctor sooner
My whole world fell apart because I was scared, but also haunted by guilt. After your initial diagnosis, you have a few weeks where you don’t know how far it spread. I had read enough and thought that it was inflammatory breast cancer before anybody told me and I knew that it was super aggressive. I knew that most women who had it had cancer somewhere else. I knew that the survival rates were scary. You shouldn’t Google them, but of course, I had.
The guilt that by ignoring something, I could possibly leave my children and husband without a mother and a wife. I was also thinking to myself, “How stupid are you that you’ve had cancer? You should be better at this. You should have followed it up.”
I have been incredibly lucky in that it has not spread anywhere else. Whenever I’ve shared these feelings with the cancer team, they have said to me that my symptoms were so slight that I did really well to get it picked up because I was so insistent. But my whole world just fell apart that day.
Did you get yearly mammograms?

I’m too young in the UK to get a yearly mammogram. So no, I hadn’t. I will now. But I’m too young, which again, is something that annoys me.
We know our bodies and I knew back in August that there was something wrong and I should have pursued that straight away.
Expanding what we know about breast cancer
Although looking for lumps is important, we need to get rid of that narrative of lumps and no pain [means cancer], and then going to our doctors and being quite insistent because again, it’s my second rare cancer.
When I looked up inflammatory breast cancer and saw it was 1% or 2% of people, I thought to myself, “I can’t have another rare cancer.” It’s like I’m winning the cancer lottery. Cancers that are rare, someone has to get them. I have checked and they’re saying that there’s no link between the 2 [cancers I’ve had]. I’m just incredibly lucky.
Although looking for lumps is important, we need to get rid of that narrative of lumps and no pain [means cancer].

Advocating for inflammatory breast cancer
Unfortunately, we have to educate ourselves because when we meet a GP or even an oncologist who doesn’t specialize in inflammatory cancer, we have to advocate for ourselves more than we should. I do that in my appointments where you have to act really fast with this cancer because it’s aggressive.
When I’ve had to wait longer for chemo than I wanted, I did question that. When I worried that my gap between surgery and radiotherapy is going to be longer than it should be, I questioned that and raised it as a concern. We, unfortunately, have to educate ourselves.
There is an Inflammatory Breast Cancer Network that has really good information. That’s really helped me understand my treatment journey because sometimes oncologists talk in jargon and I come away thinking I’m quite intelligent. But sometimes I come away and I say to my husband, “Not quite sure what she said,” so I check and then I understand.
We have to educate ourselves because when we meet a GP or even an oncologist who doesn’t specialize in inflammatory cancer, we have to advocate for ourselves more than we should.
Describe being told about your secondary cancer diagnosis
I was with my husband when they told me. There was the surgeon who was doing the biopsy and a nurse. I think the nurse picked up that I’m not really into physical affection from strangers. If people hug me, I’m like, “Oh, God, get off me.” As the doctor told me that it was cancer, she said to me, “Do you mind if I hold your hand?” She gently stroked my hand and I had tears rolling down my face, but she knew that I wouldn’t want her to wipe the tears away.
That was me processing it in the room and my mind just went to really dark places. I told my husband immediately because he was in the hospital with me.
Quality of Life
Sharing a cancer diagnosis with family and children
[My husband] let immediate family know because telling people was the thing that I found hardest. As selfish as it sounds, I don’t want to have to deal with your reaction because I’ve got it all going on in my head. When you tell someone, you have to deal with their reaction, and I totally understand that. But for the first few months, I couldn’t tell people. At work, I just sent a very flat email.



With my son, we took some advice because I didn’t know how to tell him. He’s 7. He was 6 back then and he’s not a particularly mature age 6. My nurse gave me a book that’s called “Mommy Has a Bubble in Her Boob,” and that’s how we explained it to him. We said that Mommy’s got a bubble in her boob and it’s making her very tired. It’s going to make her hair fall out because that’s the thing they notice. I was going to be tired for a while, but then I’ll be okay.
We let his school know that it was aggressive, that it was unsettling the family, that we were going to be struggling with homework and that just us functioning as a family was enough. We couldn’t do all the other stuff. But he seems to have handled that quite well.
We haven’t used the “cancer” word in front of him because he doesn’t understand the word. He could go into his school and say it to an older child and they would say – not being unpleasant – “Is your mummy going to die?” I’m not going to die, so he doesn’t need to hear that.
»MORE: How to Talk to Kids About Cancer
How has your husband adjusted to your cancer diagnosis?
We need to get better at supporting the partners of people who have cancer.

He’s been wonderful, but he’s found it really hard. He had quite a formidable wife who had a very full life, lots of hobbies, and was very into her career. He’s watched a lot of that spirit drain out of me. I was also very independent and I’ve become dependent and I don’t like that.
He doesn’t begrudge helping me, but I think he doesn’t like that because that wasn’t the kind of wife that he married. So we found it hard. I think there’s this sort of fairy tale that illness brings couples closer together. I’m not quite sure that’s true. It’s tested our marriage and we will survive because we love each other a lot, but we’ve had to renegotiate our relationship like lots of couples had to in COVID.
We also found COVID difficult because we had to renegotiate how we lived our lives. We’re probably a little bit stuck in the mud. So it’s been really hard.
Also, nobody asks after the partner. They do ask after my children. They do ask after me. Nobody asks how he’s doing. He’s working full-time. On my bad days, he’s cooking all my meals, tidying up, and doing more for our son. He’s stuck with me if I’m crying in the night and then getting up in the morning and doing a full day’s work. It’s been really hard. We need to get better at supporting the partners of people who have cancer.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
What happened after you were diagnosed with breast cancer?
I was sent to another specialist who was really guarded and he wouldn’t answer many questions. I said to him straight away, “I’ve Googled. This is inflammatory breast cancer, isn’t it?” He said, “We can’t say that until we have all the information.” I respect that, but at the time I found that really frustrating.
Then they collect information from all the scans, and I had a letter within a few days that confirmed that it was inflammatory, hormone positive, in my lymph nodes, grade 2, and they laid out what my treatment plan would be.
I was told that because it’s aggressive they have to get it as small as they can before they do surgery. So I don’t have a single lump. The cancer is diffused through my breast. That makes it harder to treat when it’s harder to see. It can be really tiny.
What cancer treatments were you on?

Initially, they said 6 rounds of chemotherapy. I had what is known as the Red Devil for 3 rounds. I didn’t find that that bad. Then I’ve had 4 rounds of docetaxel, which I found really hard. Then I will have roughly about 3 to 4 weeks off to recover from chemo. I’ve got a surgery date of the 9th of June and I’m going because I’ve had such a good reaction to chemo.
They gave me a seventh dose because, although I’m currently no evidence of disease, the cancer is so tiny that it is likely to be there. They said because we know it’s battling the cancer, we might as well do it again. So I’ve had 7 rounds of chemo and then I have recovery time. Then I’ll have a single mastectomy.
I won’t have a reconstruction for at least a year because the surgery can make the cancer angry. They want to make sure before they do anything else that it’s cancer free. You don’t want to rebuild the breast and then find the cancer is in there.
After surgery, I’ll have recovery time. Hopefully, within about a month I will then have radiotherapy, which will be every day for 3 weeks and then I will be on hormone therapy for years after.
What’s your doctor’s outlook on the surgery?
They’ve said to me they’re really confident that the cancer is going to go, so a lot of what we’re doing now is making sure it doesn’t come back because it’s got a high remission rate. I am incredibly lucky because, as I said, for most women, it’s gone somewhere else. I’ve had 2, maybe 3 PET scans, and there’s no sign of cancer anywhere else in my body. It can spread in weeks and go elsewhere in the body. That’s how aggressive it is.

How did doctors respond to you feeling guilty about not being seen sooner?
They were very careful with me because they knew that I had all these feelings about not going to the doctor when I should have. Once they knew that [cancer hadn’t spread], then they said how lucky I was.
Chemotherapy & Side Effects
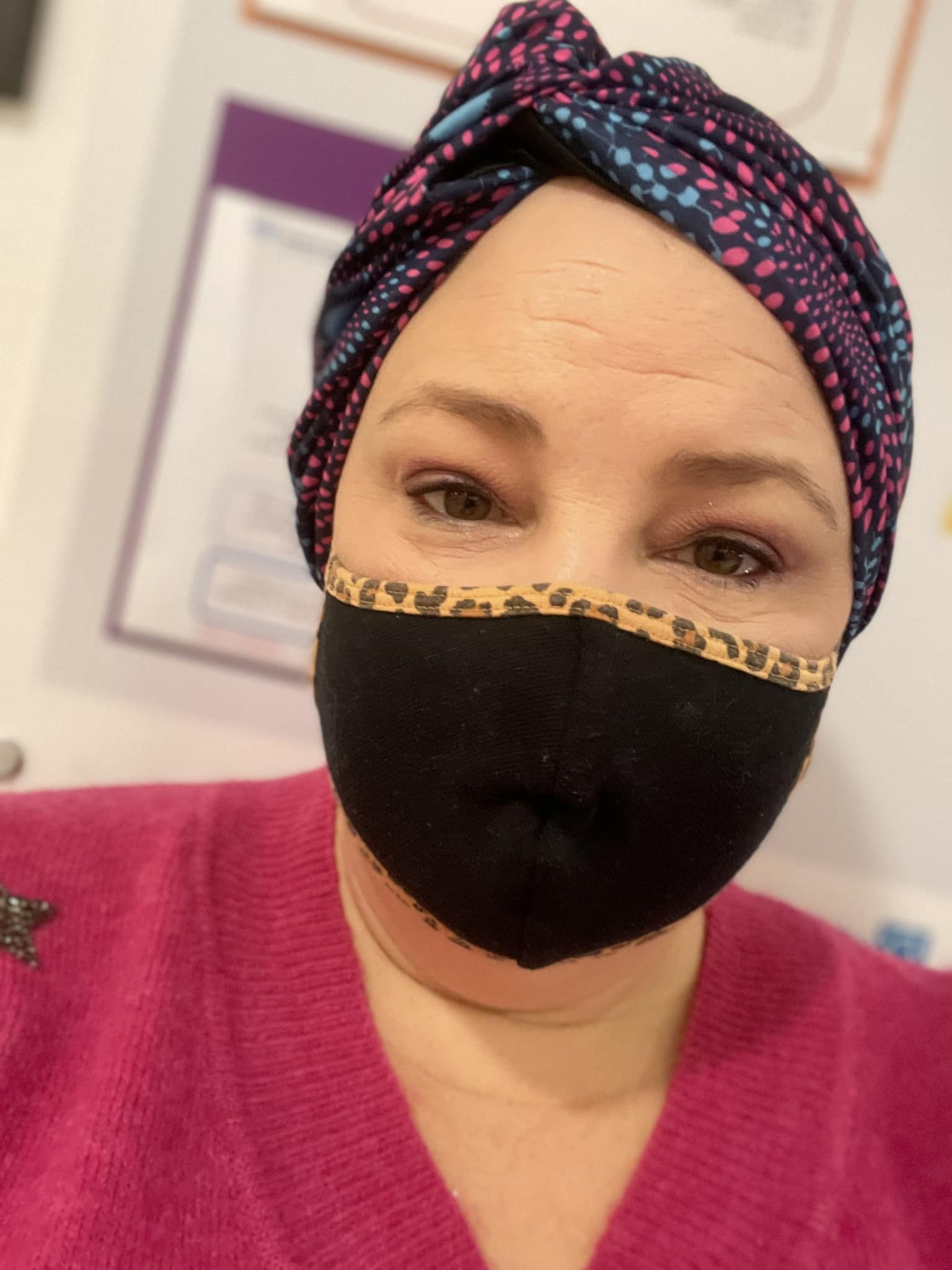
Describe hair loss after chemo
With EC, I completely lost my hair after the second treatment. I think it started to go within 2 weeks of me having the first chemo.
I’m quite vain. I had silvery gray hair that I was incredibly proud of because I thought it was a bit of a feminist statement. I stopped brushing my hair and my husband used to laugh. Everywhere I went, I left hair behind me. I said, “Look, I’m keeping a hold of my hair.” I wasn’t. I just wasn’t brushing my hair so none of it was coming out.
I went to the hairdresser for a chemo cut and she cried. I didn’t cry. She did because so much came out in the sink. I then took control and shaved it and that made a massive difference because my head was sore.



It’s really distressing to lose your [hair]. I’d have a bath and it would all be in the sink. It was just horrible. So that would be a recommendation from me, to shave it. Even if you do what I did, where you get a really short chemo cut and then you shave it 2 weeks later. I don’t think I could have gone from quite long hair to shaved.
In terms of my eyebrows, I didn’t lose them until I started docetaxel and I thought I was going to keep them, but docetaxel saw the back of those.
How did you feel after chemo?
With EC, it was mostly nausea and tiredness but not much else. Docetaxel, that’s a completely other beast.
I’ve had what they call hand and foot syndrome. I’m on top of it now because I’m taking a steroid cream, but basically, your hands peel and blister as well as your feet and get really sore. There was a time when my feet were covered in blood blisters. It made me not want to walk and then you walk funny. You walk on the side of your feet and then that blisters the side of your feet. I wish I’d told the oncologist about that sooner because they gave me hydrocortisone cream which sorted my hands.

My feet haven’t been too bad this round. I kept on top of that though. My husband bought me a foot spa so I would ease the pain in my feet. I had foot creams and balms that softened my feet. If I did that every day, I could just about keep on top of it. But when you’re tired, it’s quite hard to keep up that sort of routine.
Do you still have your nails after chemo?

I haven’t lost my nails. I’ve still got them. My top tip that my oncologist told me was to paint my nails a dark color, so I haven’t lost any. I’ve done the same with my toenails. as well. It makes you look and feel better when they look nice. My nails are very sore at the moment. I’m hoping I’m going to keep them, but I am a little bit worried.
How do you cope with pain?
I have really bad pain in my bones and part of that is to do with the injections I have to boost my neutrophils because your immune system takes a real dive after chemo. I take an antihistamine, which is Claritin every day. That helps.
I also take codeine. I try only to take it in the evening because it makes me sleepy and drowsy and it also makes me feel a bit nauseous and the chemo makes me nauseous. I have learned that there will be 3 or 4 days where I have to be ahead of the pain and I take the codeine 4 times a day. For the rest of the difficult bit of the cycle, I try to take it before bed because it helps me sleep.
Describe how chemo changed your sense of taste
I have the most awful taste in my mouth all the time. I brush my teeth obsessively because my teeth feel odd. You can get Difflam, a special mouthwash that prevents mouth ulcers, but the corners of my mouth crack. If I have a sandwich, I have to make the sandwich really flat because I can’t open my mouth very wide to eat it.
I have lots of boiled sweets just to take. It’s like a metallic taste, a bit like morning sickness, but I’m not going to get a nice baby. Sometimes I have mint ones, but any kind of boiled, fruity, sweet, or mint sweet – it doesn’t really matter. You just want something that takes the taste away.


You probably want to avoid things like lemon sherbet or anything that could be a bit abrasive in your mouth. I made that mistake once. I’ve been told that pineapple can be quite good for your mouth as well. We have a drawer full of ice lollies for when my mouth feels a bit sore or to get rid of the taste.
What other side effects did you experience from chemo?
My sleep patterns have been ruined by steroids and pain at night…I have such a long list…I also have, constant pins and needles in my hands and feet. I think that’s to do with the hand and foot syndrome. When your feet are really cold and they hurt, that’s what it feels like. I have an electric blanket that I put at the bottom of my bed. I think that helps a little bit.
I’m losing my fingerprints. My mum Googled today and apparently, they will come back. But the tips of my fingers are really smooth and I can see that my fingerprints are going and then a pain in the joints of my fingers as well.

My energy levels are really low. There were days I struggle to get out of bed and get dressed. There are days when I can’t walk more than 100 yards.
»MORE: Cancer Treatment Side Effects
My temperature is all over the place. I think that’s menopause. Because my cancer’s hormonal, they were worried about it jumping to my ovaries so I’ve been plunged into early menopause. I’ve got really bad hot flashes. If I do anything, my temperature goes up and I’m supposed to go into hospital if my temperature goes up. I’ve learned to just wait before I take the temperature. That keeps me awake at night and adds to that tiredness…It’s a long list.
Another one is my eyes water constantly. I can see them doing it now. People are always saying to me, “Are you crying?” I’m like, “No, it’s just my eyes water.” I think that’s because my eyelashes have gone and so things get in your eyes. I don’t think my eyesight has been affected, but my eyesight looks quite blurred because it’s always a little watery.
Being A Patient Advocate

Speaking up means that, you’ve done all that you can…I learned from not going to the doctor when I should have that I regretted not speaking up. That inspired me to speak up and ask questions.
Describe how self-research helped you advocate for yourself
I like to read and research, so I did lots of research. I write things down before I go in because I’m likely to forget them. I try to take my husband to my appointments with me because he will remind me, or if I’m not feeling very brave, he will say, “Nikki, there was a question you wanted to ask. Why don’t you ask it?” Because sometimes you do feel overawed by doctors.
On Facebook, there’s an Inflammatory Breast Cancer Network that I think is mostly women in the UK. They have representatives from the inflammatory breast cancer charity, so being able to ask them questions has been useful.
Also if something worries me, I go on there and search for what it is. Sometimes just seeing that other women are having the same symptoms as me makes me feel a bit braver to then say, “Actually, I’m really struggling with this. Can I have some help?”
For example, when there was a delay with my chemo, I said, “Is there an unreasonable delay?” They said, “Yes, there is” and linked me to research papers or articles. I could then go back to the oncologist and say, “I’ve looked this up and I’ve read this. This isn’t just a quick Google, and I think I should be having chemo quicker.” I’ve done the same with radiotherapy as well – I’ve let them know that I have researched this.
»MORE: How To Be A Self-Advocate As A Cancer Patient
I do want to say that no one’s deliberately delaying treatment, but because my cancer is very different from other breast cancers, I think you do have to keep reminding people of that.
Why did doctors delay your chemo treatments?
Partly because of the time of year. I had my proper diagnosis in mid-December, and then we went into Christmas. I was unlucky at the time of year. People were going on holiday and the NHS in England is struggling so that has been an issue. The care I’ve had I can’t criticize at all, but I have had to wait for that initial chemo longer than I would have wished.
The importance of advocating for yourself

It did make me feel like I’ve spoken up. I wouldn’t have liked to have waited and then be at home thinking, “You haven’t spoken up again, Nikki.” Speaking up means that, you’ve done all that you can. I learned from not going to the doctor when I should have that I regretted not speaking up. That inspired me to speak up and ask questions. Having a little notebook and writing the questions down is a good thing to do when you go to the doctor anyway, particularly for this.
Reflections
How has humor helped you?
I have a small group of female friends that I’m more open with than my husband because we can do dark humor. My husband struggles a little bit with the dark humor. That has been really valuable, being able to make “cancer’s getting on my tits” kind of jokes or, laughing at “something else has fallen off my body.” That kind of humor has been really good. Female friends, close friends, are really important.
Continuing to work through cancer

Listen to your body and do what works for you, not what you’re told to do. For example, I’ve kept working through most of my treatment which my husband hasn’t really agreed with, but that helps me remain mentally strong. I think we know ourselves and we can, within reason, navigate a path that works for us.
What works for one person doesn’t work for another person because their cancer will be different or their job, or their lifestyle. I’ve possibly done things in quite an unorthodox way, but I wanted to prioritize my mental health as well as my physical health. I think now that I’m almost at the end of my chemo journey, I made the right decision.
Checking breasts more thoroughly
We need to take pain seriously…If our body hurts, there’s a reason for it.
Even looking for a lump, I don’t think we really know how to do it. My oncologist said to me, “Did you check your breasts, Nikki?” I said yes because I did. She showed me how to do it and said, “Was that what you did?” I said yes, thinking no. It’s a lot more of a thorough process than we’re [told to] do.
She said to me, do it both lying down and sitting up, whereas often we’re told to do it in the shower. We don’t lie down in the shower, so I think we need to be more relaxed around our bodies and look at our bodies. Then you will notice the changes. Even my change, which was little, I did notice it.

Also, we need to take pain seriously. I think women because we give birth and it hurts underplay pain and we just take a painkiller and say, “Oh, it’ll go away.” If our body hurts, there’s a reason for it. Not just feeling for lumps, but properly looking at your boobs.
The other thing that can happen is your boob can swell. It can also feel quite heavy and warm. Looking back, mine did. Again, I just thought that was a period or menopause [symptom] but that was happening as well. [We need] more education about non-typical breast cancers because they’re more deadly at the moment.
What did your breast pain feel like?
Anything that doesn’t look quite right we need to take seriously.
Sharp, piercing pain. A little bit like when you’re breastfeeding wrong is exactly what it felt like.
It was very focused around the nipple. I had times when my whole boob felt a little bit achy and that might be the menopause, period kind of feeling. If it’s a pain that’s focused on the nipple, that is one that I would take very seriously.
The other thing that can happen is your nipple can change color and mine had slightly. Because I didn’t pay much attention, I hadn’t noticed that. Again, when the oncologist did a physical exam, she said to me, “Can you see that one is a slightly different color, Nikki?” Anything that doesn’t look quite right we need to take seriously.



How do you deal with scanxiety?
Scanxiety is awful. I know you’re told not to Google, but we’re human and you do. Remember that the advancements in cancer over the past 3 to 5 years have been huge, particularly with inflammatory breast cancer. If you’re looking at something that’s more than 3 to 5 years old, close it.
Go to reputable sites like Macmillan or the Inflammatory Breast Cancer Network, because we are going to look for that information. That’s how I cope with scanxiety and I try to plan some nice things.
Remember that the advancements in cancer over the past 3 to 5 years have been huge, particularly with inflammatory breast cancer. If you’re looking at something that’s more than 3 to 5 years old, close it.
Surgery worries me. It’s a big surgery that I’m having and also I’m having a bit of my body removed that I’m quite attached to, and I don’t think I’ve quite dealt with that yet. I have booked some counseling because I think I’m in denial about how hard that’s going to be. Having someone to talk to who is someone I don’t know that I can be really honest with, I think is going to help me process that a little bit.
What is your top advice to someone on a cancer journey?
Try and find joy, as daft as it sounds, because it’s not going to harm you and it might help. I’m not a woo-woo person at all, but when it comes to laughter and joy, I try to find a little bit every day.
I often sleep in the hammock, in my garden, in the sunshine, and that’s better than sleeping in my bed because I can hear the birdsong and I get some fresh air.
I try every day to save a little bit of energy to do something nice with my son. We do lots of arts and crafts and baking. Baking with a 7-year-old, something is going to go wrong and it’s funny. Or making time to chat with friends and laugh and do inappropriate humor. Doing fun stuff so you’re not just an ill person I think is really, important.


Try and find joy, as daft as it sounds, because it’s not going to harm you and it might help…When it comes to laughter and joy, I try to find a little bit every day.
More Breast Cancer Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Symptom: Lump found during self breast exam
Treatments: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Symptoms: None; caught by delayed mammogram
Treatments: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Symptom: Lump in right breast
Treatments: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Symptom: Lump found on breast
Treatments: Lumpectomy, AC/T chemotherapy, radiation, hormone therapy (Lupron & Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Symptom: Lump in breast
Treatments: Chemotherapy, double mastectomy, hysterectomy





