Using AI to Detect Lung Cancer Risks With Dr. Lecia Sequist
Dr. Lecia Sequist is the Program Director of the Cancer Early Detection & Diagnostics Clinic at Mass General Cancer Center. For nearly 20 years, she’s specialized in lung cancer.
Observing first-hand the obstacles involved in current screenings of lung cancer, Dr. Sequist made a career switch to the research of early lung cancer detection. This led her to meet MIT professor, Regina Barzilay. Together, they created Sybil – an open-source AI tool that uses pattern recognition to predict one’s risk of lung cancer.
Dr. Sequist shares the benefits of AI in preventative medicine, how AI works to assess cancer risks, the logistics of using AI, and the importance of getting screened for lung cancer.
If we can take a step back in time and try to identify those patients who are at the highest risk before cancer is visible, and we monitor those patients closely, we have a better chance of being able to pick up the cancer when it first appears and treat it and get rid of it at its earliest stages.
Dr. Lecia Sequist
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Introduction
Tell us about yourself
My name is Lecia Sequist and I am an oncologist. My clinical area is lung cancer and I work at Massachusetts General Hospital and Harvard Medical School in Boston.
I’ve been a lung cancer-focused oncologist for almost 20 years now. At the beginning of my career, I did a lot of drug development and clinical trials looking for better ways to treat our patients with advanced lung cancer. It’s been an exciting era in oncology when there’s been more targeted therapies and just a lot more different approaches for treating patients with cancer.
Obstacles in early lung cancer detection
After several years of working in that vein and especially taking care of patients, unfortunately losing a lot of patients to lung cancer, I really wanted to try and focus on early detection. Our best chance of curing lung cancer, like most cancers, is if we can find it early before it has spread and it can be surgically removed.
We have a very hard time finding lung cancer at early stages. It usually doesn’t have symptoms or the symptoms are very mild, like a cough, which could be anything. It could be allergies, an infection, or post-nasal drip. It is really hard for both patients and physicians to detect lung cancer at the earliest stages.
»MORE: The Doctor Fighting for Early Lung Cancer Screening
Our best chance of curing lung cancer, like most cancers, is if we can find it early before it has spread.
What work do you do now?
We need better technologies and better methods, and that’s what I started focusing my research on about 5 years ago. I have really enjoyed the ability to meet lots of new people. Early detection is a very multidisciplinary field. You have different types of medical people working in that field. You’ve got radiologists, surgeons, and pulmonologists. There are also a lot of other people outside of traditional medical fields that are interested in early detection like engineers or diagnostics companies. It’s a really exciting space.
I’ve enjoyed that switch in my career. That switch in my focus was what got me in the same room with an engineer from MIT named Regina Barzilay. She’s a professor at MIT in computer science and electrical engineering, and really thinks about the process of cancer diagnostics in a different way than a lot of clinicians think about it. We got thinking and talking and built a collaboration and designed this model called Sybil that we’re going to talk about today.
The Benefits of AI in Medicine
Describe Sybil
Sybil is the name of our model. It’s named after the ancient prophetesses who were Sybil, so it doesn’t stand for something. A lot of people wonder if it’s an anagram that stands for something, but it’s the name of a mythological group of women who were able to see the future. We picked that name because that’s what our algorithm is trying to do.
It’s basically using smarter tools and computer powers to do tasks that humans can’t do or take a really long time to do.
What are the benefits of AI in medicine?
There’s lots and lots of artificial intelligence or AI tools that are coming out, whether it’s in health care or in other aspects of our lives. I think, in a lot of people’s minds, it’s all lumped together. It’s just AI, but one thing that I’ve learned is that AI is such a general term. It could mean almost anything. It’s basically using smarter tools and computer powers to do tasks that humans can’t do or take a really long time to do. The computer can help you do it faster.
We’ve all benefited in our daily lives from having computers help us do things, whether it’s searching for information on the Internet or navigating to figure out how to get to someone’s house. It’s that type of assistance that we’re looking for in medicine to help doctors and other healthcare providers do their jobs easier, quicker, and smarter. Not necessarily take the place of clinicians, but a tool to help us do our jobs better.
How does using AI differ from other cancer screenings?
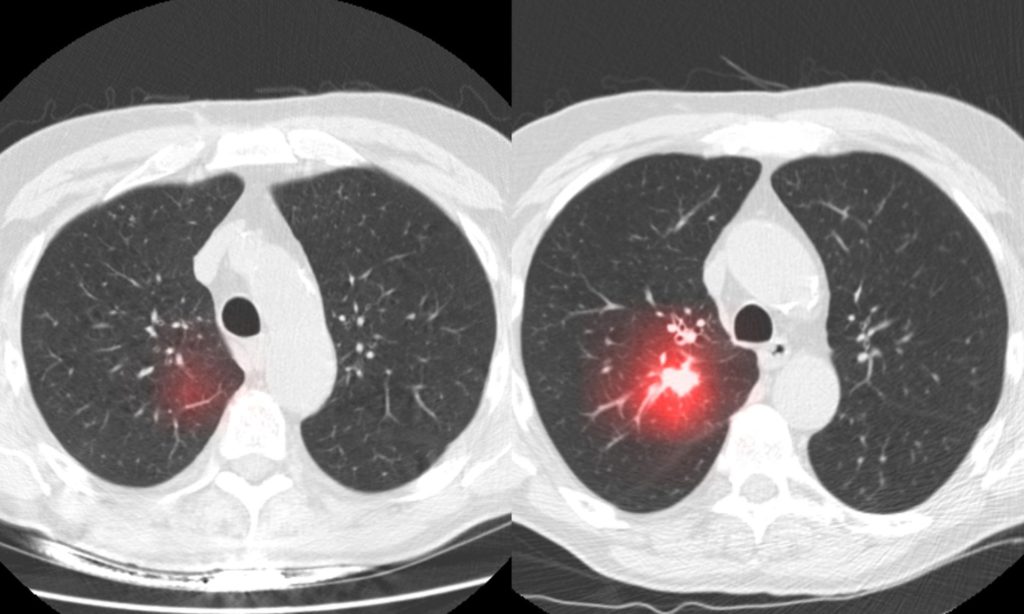
What Sybil and some other tools similar to it are trying to do is not necessarily use those images to tell you what’s happening today with the patient, but to look to the future and say, what is this patient at risk for?
When it comes to radiology – any kind of imaging, whether it’s an x-ray, a mammogram, or whether it’s a three-dimensional image, like a CAT scan or an MRI – in medicine, we have traditionally used radiology imaging to tell us what’s happening with a patient right now. Is there a mass? Is there a tumor? Is there a trauma? Is there a broken bone? Is there COVID right now? Is there a stroke? We always used it to tell us what was going on with the patient at that moment.
What Sybil and some other tools similar to it are trying to do is not necessarily use those images to tell you what’s happening today with the patient, but to look to the future and say, what is this patient at risk for? That’s what’s really different about the research we published is that we’re using a CAT scan that’s taken today on a patient, but we’re not necessarily looking for a cancer that’s present or visible on that scan. What we’re looking for is a background pattern of risk that is imaged with a CAT scan to tell us if this patient is in a high-risk category or a low-risk category and that’s just by pattern recognition.
Difficulties in current lung cancer screenings
It is possible that the model could also overestimate someone’s risk because of some kind of fake out. That’s why none of these things are set in stone. It’s a risk, it’s not a diagnosis.
That’s one of the main downsides with lung cancer screening right now is that our lungs are very busy places. A lot of stuff comes in and out with every breath. You get soot in your lungs, you get viruses in your lungs, you get all kinds of stuff that can cause visual abnormalities in the lungs. Either you breathe it in or your body’s reacting to what you breathe in. That’s what causes a lot of confusion for doctors today when we’re looking at CAT scans and trying to see if there is an early tumor there. We get faked out all the time by a viral infection or some other type of inflammation or a little piece of mucus that’s in our lungs. That’s why I think actually looking at future risk is helpful because it helps us cut through some of the noise that might be visible in a busy place like the lungs and really look at future risk.
It is possible that the model could also overestimate someone’s risk because of some kind of fake out. That’s why none of these things are set in stone. It’s a risk, it’s not a diagnosis. If Person A has a 70% chance of lung cancer in the future based on Sybil and Person B has only a 1% risk, it doesn’t guarantee that Person A is going to get lung cancer or that Person B couldn’t. It just tries to risk stratify that someone’s at higher risk than someone else and you might treat them differently. If you were taking care of them, you might watch their lungs more carefully or try to modulate that risk if you could.
How AI Detects Lung Cancer Risks
Using pattern recognition to predict future outcomes
A lot of us are very familiar with AI, even if we don’t know it’s called AI. When we’re searching on the Internet, whatever search engine we use, they all have AI algorithms so that if you type in just one word out of a four-word thing, the computer seems to magically fill in the other words for you. Sometimes you wonder, how did it know that’s what I was going to type in? But it’s pattern recognition and predicting the future of what you’re going to type based on information that it knows from thousands of other people who have typed similar things, or have your demographics, or have run similar searches to what you’ve read in the past. It knows what you might search for in the future. That’s kind of what we’re doing here.
We’ve trained Sybil with thousands and thousands of CAT scans of patients’ chests and lungs and we’ve told the model, this person ended up getting cancer, 4 years later, this person never ended up getting cancer, or this person got cancer 6 months later. The computer has learned to recognize the patterns, not in the same way that a human looks at a CAT scan.
When a human radiologist looks at a CAT scan, they have a very systematic way of looking at it. They look at the right lung and they look at the left lung, they look at the lymph nodes, the heart, and the bones so that they don’t miss anything, but it’s all anatomy-based. Our eyes and our brains can’t necessarily see the type of underlying patterns in the data that a computer can pick out. It’s just not the way we’ve been trained or the way that we interpret visual images.
What Sybil is doing is using all of the information contained in the digital image, and it’s looking for pattern recognition where it’s been trained to see cancer or to see the patterns that are affiliated with cancer before cancer develops. Sybil can say these scans are high-risk and these other patients are low-risk for developing lung cancer.
We’ve trained Sybil with thousands and thousands of CAT scans of patients’ chests and lungs…The computer has learned to recognize the patterns, not in the same way that a human looks at a CAT scan.
How does preventative medicine reduce one’s risk of diseases?
It’s not giving a diagnosis but it’s risk-stratifying people. That’s what preventive medicine is all about. We know that high blood pressure is a risk factor for having heart attacks, so we screen people in their primary care doctor’s office for high blood pressure. If they have high blood pressure, we try and lower it with medicines or we recommend things like exercise or weight loss to decrease that person’s risk of a future health problem.
A lot of preventive medicine has to do with risk reduction. How can we decrease your risk for certain diseases that may happen in the future? With a lot of diseases though, we don’t necessarily know what to screen for. The same is true with cancer.
Cancer screening has, for the most part, been about whether we can see cancer. When you get a mammogram done on your breast, they’re looking for a cancer that’s visible. When you get a chest CT for lung cancer screening, same thing. We’re looking for a visible cancer. If we can take a step back in time and try to identify those patients who are at the highest risk before cancer is visible, and we monitor those patients closely, we have a better chance of being able to pick up the cancer when it first appears and treat it and get rid of it at its earliest stages. That’s what we’re doing clinical trials now to determine.
The importance of getting screened for lung cancer
Lung cancer screening is available, not necessarily with the Sybil AI tool, but with standard CAT scans. It’s available today. Most people who could qualify are not taking advantage of it for a lot of complicated reasons. In order to qualify currently, you have to be at least 50 years old and you have to have smoked cigarettes in the past or a decent amount. The threshold is fairly high for tobacco history. That’s required to even get your foot in the door for screening.
Sadly, in the US, although there are over 10 million people who are eligible for lung cancer screening, only 5 to 10% of them are actually getting it for a variety of reasons that have to do with hospitals offering it, to doctors ordering it, to patients knowing about it or wanting it. It’s a complicated issue, but we’re hardly screening anybody for lung cancer, unfortunately.
At the same time, the disease is changing. What I see in my clinic as an oncologist, seeing people who are already diagnosed with lung cancer, we see people all the time who would not have qualified for lung cancer screening even if they wanted to get it. They’re younger than 50, they’ve smoked a lower amount than the threshold or even never-smokers are getting lung cancer now at an increasingly common rate. We think this has to do with air pollution and other types of environmental exposures, but lung cancer and people who’ve never smoked are on the rise quickly.
In the US, although there are over 10 million people who are eligible for lung cancer screening, only 5 to 10% of them are actually getting it.
We have to change who we’re letting in the door for lung cancer screening. We have to throw those doors open wide. At the same time, it doesn’t make sense to screen every living person for lung cancer because that’s just way too many CAT scans. There are costs and risks associated with screening people who are not at high risk. We have to develop tools to figure out who is at risk and should be screened and who’s not and maybe doesn’t need screening. That’s where we hope Sybil can really fit in. We’re doing clinical trials to prove that now. We’re running a series of trials along with collaborators around the world to figure out how can Sybil help real patients.
Logistics of Using AI For Cancer Risk Detection
Is Sybil currently in use?
Sybil is run off of a CAT scan, so it’s not a separate procedure. Basically, the radiology department would take the CAT scan and Sybil is just another set of eyes to look at it.
It’s not something that’s covered by insurance right now, but it’s not something that I would recommend for the general public right now either. We’re doing clinical trials to figure out how best to use it and what kind of information is actionable or not actionable. It’s still in the experimental phase.
Are there costs associated with creating and running Sybil?
I think the question of cost or who’s going to pay for it very much depends on how the tool is developed. There are some computer AI tools that are being developed by companies who, just like drug companies that develop new drugs, have to recoup the cost of the development by charging for their algorithm.
Our algorithm actually is open source. It was developed from an academic collaboration between MIT and Mass General Hospital. Anyone can use it essentially for free. There’s not a cost associated with it right now. We hope that encourages investigators from around the world to use it and study it on their own so that we can all move forward together.
Anyone can use it essentially for free…We hope that encourages investigators from around the world to use it and study it on their own so that we can all move forward together.
How far out does Sybil look to predict lung cancer risks?
We had our research focused around up to a 6-year time horizon. That was in large part because of the big data set that we used to train the model, that was how far their follow-up went. With any kind of future predictive test, the farther out you get, you lose some accuracy. But right now, we’ve designed it to look 6 years out in the future and tell us what is this person’s risk of lung cancer.
»MORE: Lung Cancer Patient Stories
Does bias play a role in Sybil’s predictions?
With any computer algorithm, you have to be wary of bias. If you had a computer algorithm that was going to predict who could drive a car, and you only taught it how to look at 8-year-old children. Well, 8-year-old children don’t know how to drive a car yet, hopefully, or they don’t have a license at least. If you’re looking at the wrong population, you’re not going to be able to predict the outcomes.
That’s really important to our research team as well, that we make sure that this is an algorithm that could be used globally and on people of different ages, sexes, and races. We’ve looked at it in a large group of people, but still, it’s not inclusive of all diversity worldwide. That is one of the main things we’re working on right now with our collaborators, is to try to get populations that are representative of different parts of the world and different demographics and look at, does the algorithm translate just as well or are adjustments needed to retrain it to include a certain type of person? It’s really important with any algorithm that you think about those sources of bias.
That’s really important to our research team as well, that we make sure that this is an algorithm that could be used globally and on people of different ages, sexes, and races.
The Future of AI in Cancer Risk Detection
When will Sybil be available for use?
It is available to people now, so it’s open source, but would I recommend that they use it to take care of patients yet? No, because I think we need more publications saying that this is how it was used in patient care and this is what it was good at. This is what it wasn’t able to do. With any tool that a health care provider is using, you have to know what it can do and what it can’t do so that you don’t use the tool inappropriately.
I think within a couple of years we’ll have reports from these various clinical trials that showed what it could do, what it couldn’t do, what its strengths were, and what its weaknesses were. That’s when doctors can start to implement it as a tool that they would use to take care of a patient in front of them.
Could Sybil be used to detect the risk for other types of cancers?
Right now, it’s only been designed to look at patterns associated with lung cancer. But that’s a really good question. Can we do similar things with other imaging or even the same imaging of a chest CT? I think that using radiology scans, which are very detailed and contain a lot of fine imagery detail about the inside of a person’s body, it’s a whole new field of how can we best use those images to improve someone’s health. There’s a big wide open universe of ideas that could go into these types of algorithms.
Do you have any advice for someone interested in lung cancer prevention?
Lung cancer screening is a very powerful tool. It’s able to save lives by finding cancer early.
Even though Sybil isn’t quite ready to be rolled out and is still being studied in the experimental phase of its development, lung cancer screening is available, and I mentioned some of the problems. It’s not being ordered on everybody or you have to be 50 and you have to have smoked the equivalent of at least one pack a day for 20 years to get lung cancer screening now. That is a lot of people who fit into those categories. So if you’re watching and you, someone you love, or a friend is a smoker or used to smoke tobacco, please tell them that lung cancer screening is out there. Tell them that they should talk to their doctor about whether they qualify for it, and if they qualify, they should definitely go.
Lung cancer screening is a very powerful tool. It’s able to save lives by finding cancer early. Lung cancer is on the rise, so it’s really important to get screened if you’re eligible. My goal in the future is to open the doors wider so more people can be eligible.





