Stage 4 Cardia Cancer Transformed Luwen’s Life and Perspective
Cardia cancer, a rare and aggressive cancer at the junction of the stomach and esophagus, fundamentally changed Luwen’s day-to-day life, career aspirations, and connection to her body and community. Diagnosed in Paris in December 2024 after months of misattributed symptoms, her experience reveals the often-overlooked complexity and adversity surrounding late-stage cancer diagnosis.
Interviewed by: Keshia Rice
Edited by: Chris Sanchez
Immediately preceding her diagnosis, Luwen balanced the challenge of beginning her career in theater with daunting physical symptoms, including persistent back pain, chest burning, and a profound sense of unease. As her symptoms intensified, she underwent multiple consultations and procedures. The French healthcare system posed its own hurdles, involving both public and private pathways, and required out-of-pocket payments until her diagnosis of cardia cancer, a kind of stomach cancer, categorized her illness as a long-term condition eligible for government coverage.

The emotional toll of stage 4 cardia cancer was magnified by isolation, as Luwen navigated both the diagnostic process and her mother’s concurrent battle with breast cancer, while extended family remained abroad. Self-advocacy proved essential; despite repeated dismissals from medical professionals and friends attributing her symptoms to stress, she persisted, ultimately insisting on crucial tests that revealed the true nature of her illness.
Treatment transformed every aspect of Luwen’s life. Eight months of chemotherapy and immunotherapy followed by a major surgical resection altered her physical relationship with food and her body, requiring new dietary habits and a lasting regimen of medication. The physical challenges were matched by emotional transformation; what mattered shifted from professional achievement to peace and well-being.
For others living through stage 4 cardia cancer, Luwen’s story offers important lessons: trust in oneself as the expert of one’s body, the necessity of persistence within medical systems, and the possibility of redefining one’s priorities after illness. Her experience is a testament to the power of self-advocacy and adaptability, and to the meaningful changes that can result from even the most difficult diagnoses.
Watch Luwen’s video above and read through her edited interview transcript below. Both will provide insights into why and how:
- Advocacy matters: being persistent to get the correct diagnosis is vital, especially when symptoms are minimized
- You are the real expert on symptoms; trust yourself when you know something’s wrong
- Major illness like cancer often forces patients to reconsider what matters most in life
- Support networks such as family, friends, and therapists, help patients endure treatment and uncertainty
- Transformation is possible: Luwen’s priorities shifted toward peace, self-care, and authentic living
- Name: Luwen S.
- Diagnosis:
- Cardia Cancer
- Age at Diagnosis:
- 25
- Staging:
- Stage 4
- Symptoms:
- Backaches
- Heartburn and acid reflux resulting in vomiting bile
- Fainting spell after eating
- Fatigue
- Inability to swallow
- Treatments:
- Chemotherapy
- Immunotherapy
- Surgeries: esophagectomy, partial gastrectomy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Luwen
- My initial symptoms
- Navigating the French healthcare system
- I processed everything while I was alone
- My body broke down, and I doubted myself
- My persistence led to second opinions and the key endoscopy
- My treatment experience
- I had surgery, and how I recovered from it
- Moving forward, and my new priorities
- How I coped with the hardest moments
- Lessons for young cancer patients
- Healing, recovery, and looking forward
- My final reflections
My name is Luwen
I was diagnosed in December 2024 with stage 4 cardia cancer. The cardia is basically the junction between the esophagus and the stomach. I was diagnosed in Paris, and I live in Paris.
I had just finished university and was getting my first job in theater. I’ve always had an interest in theater, and I was really happy because I was working on this big production. I remember it because my cancer basically started to grow at the same time that I got my job. So, during the summer of 2024, I was very stressed. I was trying to find a job after my internship and couldn’t find one. As I interviewed for many positions and eventually got the job I wanted, my symptoms worsened.
Alongside this, my family lived in China, and my mother was diagnosed with breast cancer in November, a month before my own diagnosis. I did a lot of back-and-forth travel between China and France, while my grandparents lived in America, so I was used to traveling. But, yeah, that was pretty much my life before I got cancer.
My initial symptoms
It was really strange because I started with back pain. Basically, I had metastasis along the spine, and those were my first symptoms in the summer of 2024. It started in June. I remember this because I was at a Buddhist retreat, sitting cross-legged all day for a week, so I thought it was the retreat that had caused the pain. I started to take ibuprofen and paracetamol, hoping to ease the pain, but it didn’t help.
In August, I developed chest burn, which I didn’t know was acid reflux at the time, and which I later learned to name. That was my mistake: I called it acid reflux, so the doctors just stuck with that diagnosis, saying there was nothing else wrong. I was misdiagnosed for six months, going from doctor to doctor, always being told I had nothing. All the while, my back pain and chest burn continued to worsen.
I remember once in September, it was the first real alarm in my head. I woke from a dream where I was on a sterilized hospital table, doctors trying to get something out of my stomach, and they couldn’t. I woke up to realize the pain wasn’t a dream; it was very real. That’s when I realized I really needed to see a gastroenterologist, but the first one I saw was really bad and misdiagnosed me.
Navigating the French healthcare system
In France, you typically have a primary physician. I saw mine at the end of August, after I’d started my new job and when my symptoms had worsened. One night, I had a really bad hunger pain in my stomach, and I knew that eating would ease it. So, I went to eat, then fainted, which had never happened to me before. I was lucky I didn’t hurt myself.
After that, I saw my primary care doctor, who said I needed a physiotherapist for my back, and that the chest burn (acid reflux) could wait until November for a gastroenterologist appointment. So, I started physiotherapy, which didn’t help. In September, after continuing to wake in pain, I realized I couldn’t wait any longer.
France has an app for scheduling doctor appointments, but it’s hard to know which doctors are good; you have to check reviews online or hear about them through friends. No one around me knew a reputable gastroenterologist, so I chose from the limited, less-recommended options available on short notice. Appointments with specialists are particularly hard to get.
There’s public healthcare, where you don’t pay out of pocket, and private practitioners, who set their own rates. I paid my private gastroenterologist €80 per visit, three times total during this process. I also returned to my primary care doctor about ten times in three or four months, but he couldn’t figure out what was wrong. I underwent many scans and imaging, some of which I had to pay for, depending on whether it was public or private healthcare.
I was really lucky that after my diagnosis, everything switched to 100% public healthcare. I didn’t have to pay for my treatment. But during the diagnosis period, I spent about €2,000 to €3,000 on doctors and scans. In France, once you’re categorized as having a long-term disease, anything related to it is covered by the government. So, after diagnosis, cancer care was paid for.
I processed everything while I was alone
You have to keep in mind that I was alone in Paris. My parents were in China, and my grandparents were in America.
I was navigating all of this by myself, getting more stressed with my job, when I got the news that my mother was also sick. It was a lot to process alone.
It was weird, trying to get an answer while everyone around me kept saying, “You’re insane, you’re making this up, it’s just stress.” I heard that so many times that eventually, I began to believe it myself, despite knowing deep down it was more than stress.
I even started doubting my own symptoms because of all the repeated dismissals from those around me.
My body broke down, and I doubted myself
At work, my boss was running a show and an exhibition, and I was supposed to go to Marseille for two weeks for my job. I stayed for just two days before my body gave out.
I had driven myself to the breaking point. Everything happened so quickly that, only in January, right before starting treatment and after returning from Christmas holidays, did I realize just how hard this all had been to take on alone.
I don’t think I trust the health system. Even though I am cured, thankfully, it’s hard for me to see a doctor and believe they are telling me the whole truth or getting to the root cause. In my case, my gastroenterologist just treated the symptoms (acid reflux) with omeprazole, which masked the symptoms and delayed realizing the underlying (cancer) problem.
My persistence led to second opinions and the key endoscopy
When my body finally broke down, I was sent back to Paris and put on sick leave. That week, I saw about four gastroenterologists, but for some reason, none wanted to give me an endoscopy. I had known since October that I needed one, but I wasn’t taken seriously.
I finally texted a friend, who knew a really good private gastroenterologist. I emailed him all my symptoms on a Sunday night and was lucky; he let me come in the next day. I decided I wouldn’t leave without an endoscopy scheduled. I had to exaggerate my symptoms, saying I couldn’t swallow water or eat (even though I could still drink), just to be taken seriously.
At my endoscopy, the doctor said, “Don’t worry, it’s probably nothing; we’ll just give you more omeprazole.” I insisted that omeprazole hadn’t helped me. He told me he’d call after the procedure to say everything was fine, but when I woke up, he was there in person. He said, “Do you have a minute? I have bad news for you.”
Later, he returned to my room and told me, “You have a lesion; it also has an ulcer, and it might be cancerous.” That was the first time I heard the word cancer regarding myself. I felt so relieved: “Oh my God, I’m not crazy. I’m not making things up.”
From there, everything moved very quickly. Doctors aren’t technically allowed to tell you outright that you have cancer, so he just said, “It might be cancerous.” But he made sure all tests happened within a week, which is rare for the French system. My endoscopy was on December 5th; my first meeting with my oncologist was on December 16th. The weekend before that, my friend from the UK came to stay with me because I was so stressed.
When I was finally able to process information, I realized how serious this was: scans, blood tests, a glowing spot in my stomach. I didn’t even know what cardia was until I looked it up. Everything fell into place piece by piece.
My treatment experience
It got quite bad before I began treatment. I was in constant pain, couldn’t eat or drink, and was losing weight week by week. I don’t like to say I stared death in the face, but it did feel close. During this time, after my diagnosis and before starting treatment, I returned to China to be with my mother, who had just started her own breast cancer treatment.
Having my mother go through chemo ahead of me meant I had someone who understood each step. I knew how to pack a chemo bag, what to expect, and how symptoms might develop. I was relieved to learn I wouldn’t lose my hair.
My first chemo was the worst. I was so sick I could barely get out of bed; I was overcome with nausea. Fortunately, my body responded well to immunotherapy. By the second chemo, I could almost eat normally again. By the third, I had regained some strength; by the fourth, scans showed the metastasis in my spine was completely gone. I had chemo and immunotherapy for eight months, and the cancer was gone in six months.
I had surgery, and how I recovered from it
After eight months of chemo, I was cancer-free, but we weren’t sure it was totally gone. Surgery (esophagectomy) was needed to remove the cardia and ensure there were negative margins. This meant removing most of my esophagus and a third of my stomach.
Now, my stomach is higher, and I don’t have an esophagus. Food falls directly into my stomach and then into my intestines.
Learning how to eat after that is difficult. I had surgery on September 8th, and as of now, I’m still recovering. I’ve lost about 10 kilos (~22 lbs). Eating requires extra care; monitoring oil, sugar, and food quantities to avoid dumping syndrome, which causes stomach pain, nausea, and diarrhea when food moves too fast into the small intestine.
Despite losing weight and always having had a sweet tooth, I have to be careful now. The way my body processes food has changed, requiring lifelong meds for acid reflux. It’s challenging, but it pushes me to adopt healthier habits. My life, needs, and desires have all changed.
Moving forward, and my new priorities
Cancer has taken away a lot, but weirdly, it has given me a lot too.
I used to work as a theater producer, but lost the desire to continue due to the stress and ego management. What I want now is to be happy, peaceful, and healthy. It’s no longer about pleasing others; it’s about making myself feel good and putting myself first.
I am not on maintenance therapy; all treatment ended before my surgery. Now, I just get regular scans every three months, then every five, then yearly.
It is behind me in the sense that I don’t want to think about it, but surveillance and the reality of stage 4 cancer mean you never quite feel “cured.”
My biggest fear today is that what comes back could be worse: pancreatic, stomach, or lung cancer. The word “cancer” will always be a part of my life now.
How I coped with the hardest moments
During treatment, I often lost my mind. My mother came back to France to care for me while she was ill, and I cared for her too. Once, she had a kidney failure episode, and I rushed her to the emergency room; if I’d been 20 minutes later, she could have died. That was on Mother’s Day.
What got me through was calling my best friend to cry and having therapy. I was surrounded by personal and healthcare therapists.
Ultimately, it was the mentality of, “I don’t get a choice; I just have to keep going. You can cry all you want, but you have to do the next round of chemo.”
I was lucky that my treatment worked, which made it a little easier to endure.
Lessons for young cancer patients
I was 25 when diagnosed. Having cancer at a young age is often dismissed; people expect youth and health to go together. Being young and female, women’s pain is often minimized, so I had to exaggerate symptoms to be taken seriously. My oncologist told me, “You’re lucky; apart from the cancer, you are otherwise very healthy because you are young.”
Most patients I saw during chemo were in their forties or older. But statistics show more young people getting cancer, even if it’s still rare. The main thing I would tell other young people: you know your body best. If you know something is wrong, trust yourself.
Cancer taught me how to advocate for myself, how to say, “No, you are wrong; I am in pain.” If a doctor doesn’t listen, see someone else until you get an answer that satisfies you.
I didn’t really connect with any other young people with cancer at the same time. I mostly navigated it by myself, though I had friends, family, and a lot of therapists in my life. Illness sheds false friendships, but it also brings new, real ones closer.
Healing, recovery, and looking forward
Words like “recovery” and “healing” have new meaning for me now; they exist where before they didn’t.
When you’re young, you’re focused on chasing the next thing; when you fall off that hamster wheel, you realize you must learn a new way forward, and it isn’t just about health. It’s about building a life again after illness.
I hope I get to do the job I want; publishing and writing, maybe publishing a book someday. I pay more attention now to health, food, and exercise. It’s scary to start over, but exciting. There are so many new opportunities and people to meet.
Statistics were not on my side. My oncologist told me that if immunotherapy hadn’t been available, I would have had only 4-6 months to live. That made me realize how far medicine has come. I really did beat the odds.
Still, I feel I’m on borrowed time and need to enjoy it fully while I have it.
My final reflections
I survived; long story short, I survived. It was not easy, and I’m very tired.
I tell my best friend that if cancer does return, I’m not sure I want to fight it again, but we’ll see when we get there.
Hopefully, I will never have cancer again.

Inspired by Luwen's story?
Share your story, too!
Related Cancer Stories
Melissa W., Stomach Cancer (Gastric Adenocarcinoma), Stage 4B (Metastatic)
Symptoms: Feeling like something was in her throat, occasional nausea, acid reflux, occasional feeling of having boiling water in her stomach, soreness in the bottom of her ribcage
Treatments: Chemotherapy, immunotherapy
...
Dawn C., Stomach Cancer (Gastric Adenocarcinoma, Hereditary Diffuse Gastric Cancer), CDH1+, Stage 4 (Metastatic)
Symptoms: Persistent bloating, feeling of discomfort in the stomach area, weight loss, dehydration, feeling very full leading to vomiting, high blood pressure
Treatments: Chemotherapy (HIPEC, including through a clinical trial), surgeries (gastrectomy, splenectomy, cholecystectomy, oophorectomy, appendectomy, omentectomy, peritonectomy, lymphadenectomy), immunotherapy
...
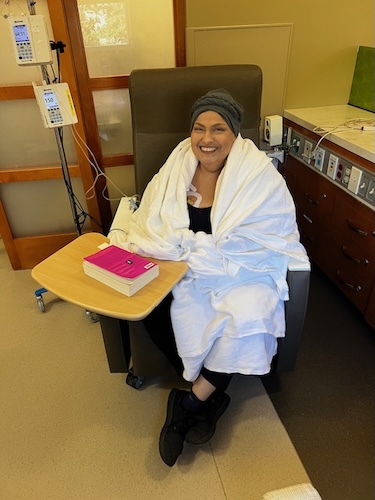
Niccole B., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Stomach pain after having alcoholic drinks, eating less, slight weight loss, acid reflux, vomiting, getting full fast
Treatments: Chemotherapy (hyperthermic intraperitoneal chemotherapy or HIPEC, open HIPEC with cytoreductive surgery), surgeries (partial gastrectomy, cholecystectomy, splenectomy, partial colectomy, partial hepatectomy), radiation therapy (targeted radiation therapy), immunotherapy, targeted therapy (PARP inhibitor)
...
Frank B., Stomach Cancer (EBV-Positive Gastric Adenocarcinoma), Stage 4 (Metastatic)
Symptoms: Weight loss, night sweats, fatigue, swelling in one testicle, urinary tract infection, back pain
Treatments: Chemotherapy, immunotherapy
...
Luwen S., Cardia Cancer, Stage 4 (Metastatic)
Symptoms: Backaches, heartburn and acid reflux resulting in vomiting bile, fainting spell after eating, fatigue, inability to swallow
Treatments: Chemotherapy, immunotherapy, surgeries (esophagectomy, partial gastrectomy)
...
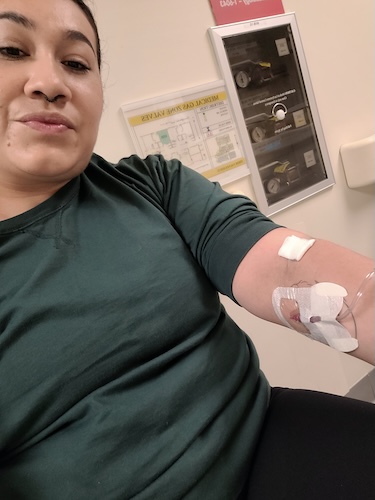
Arelly R., Stomach Cancer (Gastric Adenocarcinoma), Stage 4 (Metastatic)
Symptoms: Nausea, blood in stool, side pain, extreme fatigue, excessive burping
Treatments: Surgeries (gastrectomy, port placement), chemotherapy, immunotherapy, targeted therapy (antibody-drug conjugate)
...