Stacy’s Myelofibrosis Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

Stacy shares the subtle symptoms she experienced that eventually led to her diagnosis of myelofibrosis, a rare type of bone marrow cancer.
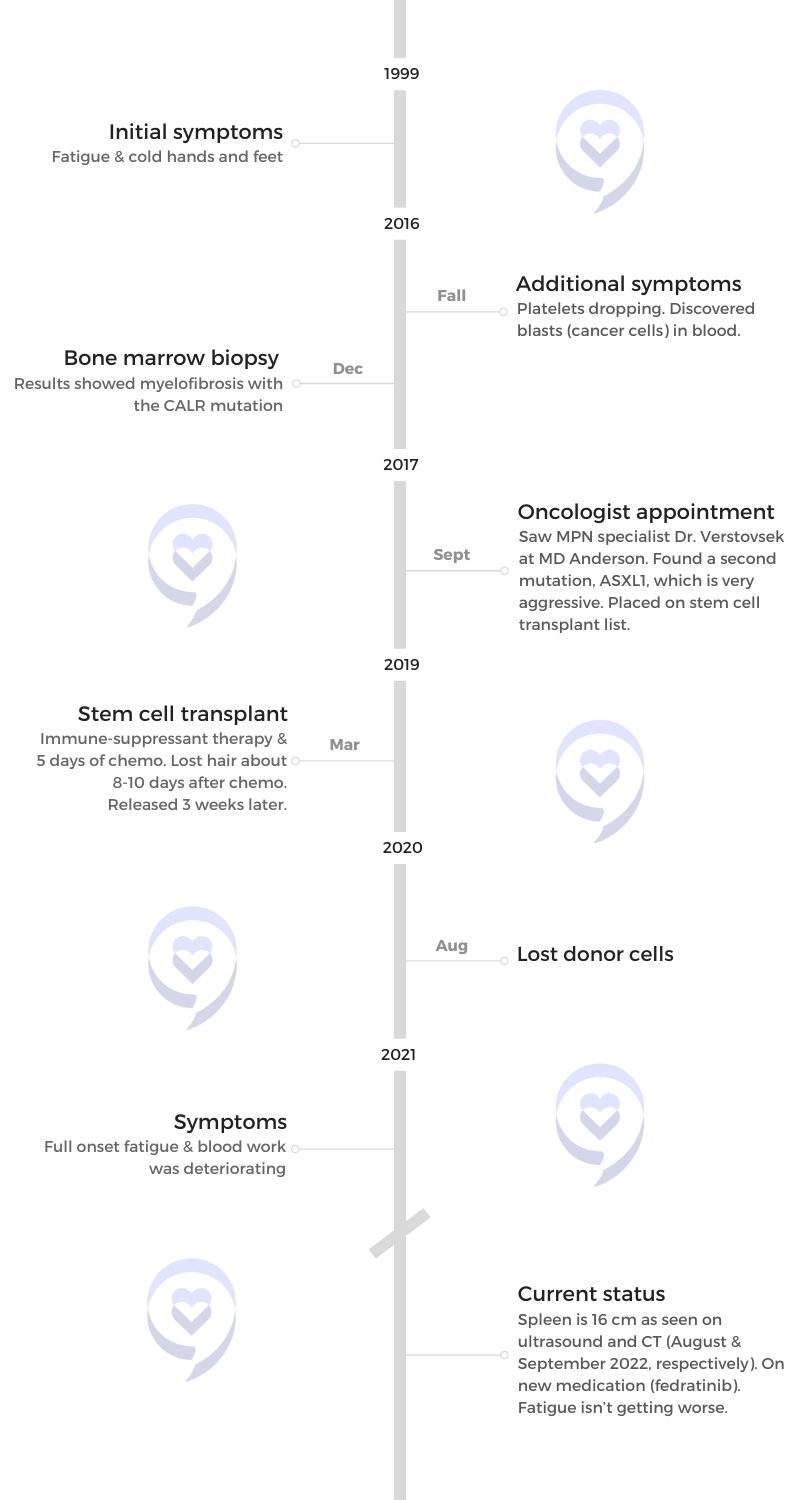
In 1999, Stacy was initially diagnosed with essential thrombocythemia (ET), a disorder that causes the overproduction of platelets. She initially went in to see her doctor because of what she thought were thyroid issues until her blood work showed a platelet count that was off the charts.
After being referred to an oncologist and getting a bone marrow biopsy, she was told she had a bone marrow disorder. Despite not having any symptoms, she was put on medication and continued seeing an oncologist for the next two decades.
During one of her annual checks, her new oncologist found blasts in her blood. The biopsy results subsequently showed myelofibrosis with a non-aggressive mutation.
Shortly after, she consulted with renowned MPN specialist Dr. Serge Verstovsek and found out that she had another mutation. This one was more aggressive so she was put on the stem cell transplant list immediately.
She talks about going through the uncertainty of initial diagnoses when it comes to myeloproliferative neoplasms, going through stem cell transplant, managing an enlarged spleen, and the questions she faced with treatment decision-making.
In addition to Stacy’s narrative, The Patient Story offers a diverse collection of myeloproliferative neoplasm (MPN) stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Stacy S.
- Diagnosis:
- Mutations:
- CALR
- ASXL1
- Initial Symptoms:
- Fatigue
- Cold hands & feet
- Treatments:
- Agrylin (blood thinner; for thrombocythemia)
- Ruxolitinib (JAKAFI)
- Fedratinib (INREBIC)
- Stem cell transplant
Introduction
I grew up with five brothers. I’m the only girl and the youngest.
I live in Tomball, a suburb of Houston, Texas. I love sports. If Houston has a sports team, I root for them.
I did community theater for about 25 years. It wasn’t the applause that I loved. What did it for me is when you hear people laugh or in a drama, when you hear that silence when something is really, really tense. It’s been tough to let that go, but I don’t have the energy anymore.
I’ve channeled it into something new. I’ve been writing and directing little skits for Vacation Bible School at church. It’s been a whole different world for me.

I had thrombocythemia. They gave me medication. It was great for 17 years. Then they noticed some immature cells and my platelets dropping. That’s when they found the myelofibrosis.

Pre-diagnosis
Initial symptoms
In September 1999, I thought there was something wrong with my thyroid because I had some fatigue. I was tired. My hands and feet were cold, but I don’t know what caused that.
They did a blood test. My platelets were through the roof that they couldn’t even read and had to send out. It was 1,400,000.
When they did a bone marrow biopsy, that’s when they found that I had thrombocythemia. They gave me medication. It was great for 17 years. Then they noticed some immature cells and my platelets dropping. That’s when they found the myelofibrosis.
At work, my lunch hour was always my time to work out. I would do the elliptical and strength and/or core. I would start out on the elliptical and instead of being able to add more resistance or go faster, I get out of breath faster and can’t do more. I’ve got to do less or take away resistance. All I could think of was, Is it because I’m getting older? That was my excuse for it.
That happened in April 2016.
Diagnosis
When the results came back, I said, “Let’s do them again. I want to make sure. Let’s do them again before we do a biopsy.” We did them again. I got scheduled for a biopsy and that’s when they found out that it was myelofibrosis.
In 1999, thrombocythemia was considered a bone marrow disorder. It shifted in 2006. My oncologist never told me. I always went for my annual CBC and everything looks great.
When I went in after my biopsy and my oncologist said, “You’ve always had cancer,” that’s when I looked it up online. In 2006, they upgraded it to describe it as cancer.
I thought thrombocythemia could turn into acute myeloid leukemia. That’s what the little sheet of paper he gave me said. I never heard about myelofibrosis or polycythemia vera.

The second bone marrow biopsy was a nightmare… The painkiller they gave me wasn’t working.
Testing
I had a biopsy. The first one was great. I had twilight in 1999 so I felt nothing.
The second one was a nightmare. Since myelofibrosis is scarring of your marrow, it’s harder to get that sample. I was at the table for about 40 minutes. They kept on trying and couldn’t get a sample so I sat there for another 30 minutes. They brought a second team and they kept on trying until they got a semi-sample.
I found out that morphine doesn’t work on me. The painkiller they gave me wasn’t working so it was hellacious.
Processing the Diagnosis
They said, “You’ve got one mutation, but it’s not very aggressive.” It was the CALR, which was the “good” mutation. If you have myelofibrosis, this is the one you want. The prognosis was 15 to 20 years. I thought, Hey, I’m cool with that. That gave me until I was 70 so I was happy with that.

I’m living each day like I might not have tomorrow, but I’m going to make plans for next month. I’m going to make plans for next year. I’m buying Christmas presents. I’m living like I usually do. I’m not going to focus too much on that because it’s not up to me anyway.

Treatment
Medications
I took Jakafi for about six months, but my platelets were crashing and my spleen was still getting bigger so I got off it.
Then I did thalidomide and that was tremendous. It was great. That helped me a lot. It pushed my numbers up.
But in April 2017, I said, “I’ve got a little numbness in my right foot. Is that neuropathy?” My oncologist said, “No, no, no. If you don’t have it in your left foot and just your right, then it’s fine. It would be in both feet.”
August came around and I said, “I’ve got numbness in both feet now.” I had already stopped taking it. I really wish I stopped taking it in April because whenever I got chemo, that’s when it worked its way all the way up to my knees.
I started to go to MD Anderson to the world-renowned myelofibrosis doctor Dr. Verstovsek. He did a few more blood tests and got some of the samples from my biopsy. He said, “Yes, you do have the CALR, but we found a second mutation. We found the ASLX1, which is one of the more aggressive ones so we suggest you do the stem cell transplant because you’ve now got 2 to 5 years.”
I’m on a Facebook page where many people have been told that they have 2 to 5 years and they’re saying, “Yeah, but I’m on my year 10,” “I’m on my year 15,” so it’s okay.
I’m living each day like I might not have tomorrow, but I’m going to make plans for next month. I’m going to make plans for next year. I’m buying Christmas presents. I’m living like I usually do. I’m not going to focus too much on that because it’s not up to me anyway.

‘We suggest you do the stem cell transplant because you’ve now got 2 to 5 years.’

Stem Cell Transplant
The stem cell transplant was in March 2019.
Before the stem cell transplant, you go through a boatload of tests, like a bone marrow biopsy. Your family goes through training on what to expect. For the first 100 days, you have to be prepared to be within an hour of the hospital and then expect to say about a month in the hospital.
You check in and they put in a port for them to give you medicine, do blood draws every day, and also give you your chemo.
Side Effects
The other thing worse than the chemo was the immunosuppressive treatment. That’s the worst thing I’ve ever been through in my life. It was basically to crash your immune system.
I’ve never had the flu, but I’m guessing this was like getting the flu times three. You get a fever. I’ve only had probably five fevers in my life. My fever spiked to about 102°F or 103°F. I remember seeing my hands shaking. My body was shaking.
I learned to meditate so I started to meditate and I could calm it for like 6 or 7 seconds then it would start up again. The bone pain in my legs was so excruciating. I had to get out of bed and walk around. They gave me three doses of either Percocet or Darvocet. After about 3 or 4 hours, it finally went away.
I had a little nausea from the chemo. The anti-nausea medications that they gave me didn’t help. The first day, I was sick and had nausea and diarrhea. Then the next day, it was like my body got used to it and I was fine. They switched to the next one and then I was sick and then my body got used to it.
After chemo, I got mouth sores. A lot of people had it much worse than I did because they were always checking if I had it down my throat so I was very lucky in that capacity, but I did have bad mouth sores.
They gave Biotène, but that didn’t help. I would try and numb my mouth with ice and that helped.
After, you wait for your numbers to get better. They waited for the leukocytes to get up to a certain number. I think 19 was the magic number to release you.
I had a little bit of graft versus host disease. Again, not as bad as most people. My skin itched terribly. I didn’t have any rashes, but my skin felt like I had ants crawling over me all the time. The magic thing was putting coconut oil on my skin, especially right after a shower when the pores are open. It felt so good.

The other thing worse than the chemo was the immunosuppressive treatment. That’s the worst thing I’ve ever been through in my life.

Recovering from Stem Cell Transplant
I stayed at my mom’s for the first week and then I moved to stay with my brother and sister-in-law.
When the stem cells didn’t graft, they kept on saying, “We’ll keep on checking your blood counts.” My blood counts kept on looking really good for a year or two, except my white blood count because they’ve always been pretty high. They said, “Okay, keep on doing what you’re doing.”
It wasn’t until 2023 that my LDH went through the roof, which is what shows how much scarring is in your bone marrow. You’re supposed to be around 150 and mine’s about over 2,000.
I’m on medication because I have neuropathy up to my knees. I got Addison’s disease so I’m on steroids. I also get migraines so I’m on medication for that.
I’m still on several medications from the stem cell transplant. I take medication right when I wake up, when I go to bed, and twice during the day. I also take supplements.
Post-Stem Cell Transplant
I stopped having transfusions. My last transfusion was in January 2020.
Then I started to lose the stem cells in August 2020.
They said that they wanted to do another stem cell transplant, but I said no. I wasn’t going to do it again, mainly because I’m still living with the side effects from the chemotherapy that I got. The neuropathy and Addison’s disease haven’t gotten better.
Addison’s attacks your adrenal glands and your adrenal glands work in conjunction with your muscles. I have pain in my muscles all the time. Now I have low sodium, low magnesium, and high potassium. At nighttime, I wake up with really bad cramps in my feet, ankles, and shins.
Even if the next stem cell transplant were successful, I would be worried about what would be left over in my body afterward.

They wanted to do another stem cell transplant, but I said no. I wasn’t going to do it again

Fatigue
I would like to take a nap every single day. There are so many stages of fatigue. Fatigue stage 1 would be when your hemoglobin is at 10 and when it hits 9, you’re dragging, but you can still do stuff.
Then when it hits 7 or 8, which is where I am now, getting out of the chair and going to cook something requires focus. When I drag my sprinkler out, I’m so worn out and breathing heavily that I slump in a chair and think, I have to go to the bathroom. Okay, I’ll do that in about 15 or 20 minutes when I can do that.
I’m not married. I don’t have kids so I’m taking care of myself. It would be really difficult for me to take care of myself if even more of my body is affected by the chemo. Even though the cancer is gone, there would be other things going on. Right now, I can at least get around and take care of myself.
Enlarged Spleen
The normal size is around 11. It shoves up against your stomach and it can make you feel fuller faster. My spleen in December 2016 was 16.5 cm. By the time I had the stem cell transplant, it had gotten up to 22 cm. But now it’s halted at 16. I had a CAT scan in 2022 and it was 16.5.
My oncologist feels my side every single time I go in, which is every two months. He says, “Yeah, it still feels like it’s about that.”
We are planning on having another CT scan before the end of 2023, but it doesn’t seem like it’s getting any bigger.
Fedratinib’s been great. It’s keeping my spleen where it should be. It’s still affecting my hemoglobin so we’ve been waiting for the other one. I heard that it doesn’t affect your hemoglobin as much so that’s what I’m looking for. But it does help with fatigue and helps keep your spleen where it should be.
Fedratinib’s been great. It’s keeping my spleen where it should be.
I asked my oncologist about that a year ago. I mentioned it to him because I got it from the MPN newsletter that I get. I said, “Did you hear about this?” They were talking about a March release from the FDA, then it was pushed to June, and then it was pushed to the fall.
He said, “I’m going to get you on it the second that it gets released,” so we’re definitely on the same page there.
It seems like there’s more awareness of it because there’s people talking about it now. People are getting more into research.
Words of Advice
I could not have gotten through it without my family, my friends, and my church community. There’s no way. When I thought about the transplant, I didn’t worry about the chemo, losing my hair, or being in the hospital.
I dreaded going to the hospital 2 to 3 times a week and having to depend on somebody else to drive me. I lost sleep over that because I did not want to have to put people out like that. It bothered me so much thinking about it.
Accept the help and give help whenever you can and however you can.
My family, my friends, and my community were so giving to do that for me. I can’t thank them enough. I learned humility. It’s the greatest gift I’ve ever, ever, ever received and I’ll never be able to pay them back.
There are people that have such good hearts. Accept the help and give help whenever you can and however you can, even if it’s just to call somebody up and say, “Hey, how are you doing?”
When I wake up every morning, the first thing that I do now before even getting out of bed is meditate on Scripture. Before it was, “No, I’m going to stay in bed. I’m going to sleep ten more minutes.” It’s not my day. It’s His day.


Inspired by Stacy's story?
Share your story, too!
More Myelofibrosis Stories
How to Support Someone with Cancer: Karina & Jesse's Myelofibrosis Story
“I underwent a lot of sadness, hardship, and difficulty, and all that entails. But I pressed forward in hope for sure. There was a lot of hope that just kept me going all those years.”
Demetria J., Essential Thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Extreme fatigue, stomach pain (later identified as due to an enlarged spleen), dizziness, shortness of breath
Treatments: Spleen-shrinking medication, regular blood transfusions, bone marrow transplant
Neal H., Prefibrotic Myelofibrosis
Symptoms: Night sweats, severe itching, abdominal pain, bone pain
Treatment: Tumor necrosis factor blocker, chemotherapy, targeted therapy, testosterone replacement therapy
Andrea S., essential thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Fatigue, anemia
Treatments: Targeted therapy (JAK inhibitor), blood transfusions, allogeneic stem cell transplant