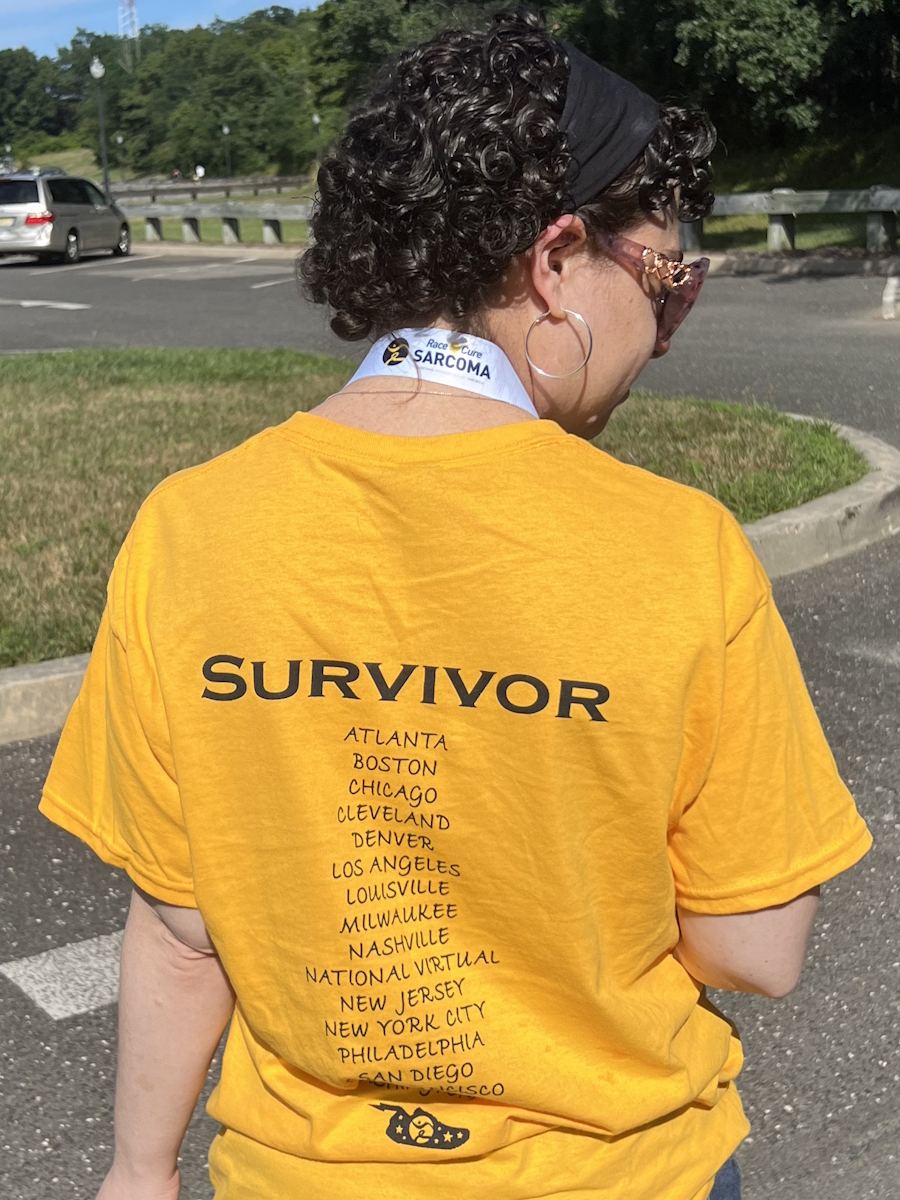
The Nickel-Sized “Bruise” That Changed My Life: Sophie’s Stage 2 Ewing Sarcoma Story
Sophie’s story begins with a strange, round robin’s-egg–blue spot on her upper arm that didn’t hurt, fade, or otherwise behave like a normal bruise. Pushing for answers led to a diagnosis of soft-tissue Ewing sarcoma, a rare kind of cancer, at age 31. Initially, a doctor thought it was nothing serious. But Sophie trusted her gut and insisted on further checks. Her persistence led to an ultrasound, a surgery, and eventually the devastating phone call: it was cancer. She had never even heard of Ewing sarcoma before that day.
Interviewed by: Nikki Murphy
Edited by: Chris Sanchez
Sophie’s experience emphasizes the importance of self-advocacy, particularly for adolescents and young adults. She quickly learned that waiting months to be rechecked wasn’t an option. Pushing for answers, she navigated multiple appointments, imaging scans, and pathology reviews until she received a clear diagnosis. Along the way, she also discovered the emotional toll of rare cancers like Ewing sarcoma, namely fear, uncertainty, isolation, and how it can feel when life halts while friends and peers continue moving forward with weddings, new jobs, and other milestones.

Sophie’s treatment involved 14 cycles of chemotherapy over 10 months, split between inpatient and outpatient sessions, plus a second surgery to secure clean margins after the first removal proved insufficient. Uncomfortable side effects like fatigue, nausea, food aversions, and hair loss became part of her new reality. But she found ways to manage the cycles and focus on what she could control. She realized that mental health was as important as physical health, and leaned on family and close friends who stayed present through the hardest days.
She now has no evidence of disease (NED), and continues regular scans and bloodwork to monitor her health. Sophie hopes her story encourages others to listen to their bodies, speak up if something doesn’t feel right, and seek specialists for rare cancers like Ewing sarcoma. She also wants to shine a light on the psychological impact of cancer in young adults: how it reshapes expectations, identity, and hope, and stresses that research into rare cancers must continue to grow.
Watch Sophie’s video and check out the transcript of her interview. You’ll find out more about:
- The little round blue “bruise” that turned out to be something far more serious
- How one young woman pushed for answers when doctors said to wait six months
- How Sophie’s story evolved from a casual doctor’s visit to a life-changing cancer diagnosis in just weeks
- The emotional toll of facing mortality at 31 while friends moved forward with life milestones
- Hard-won lessons on self-advocacy, resilience, and finding strength in the face of Ewing sarcoma
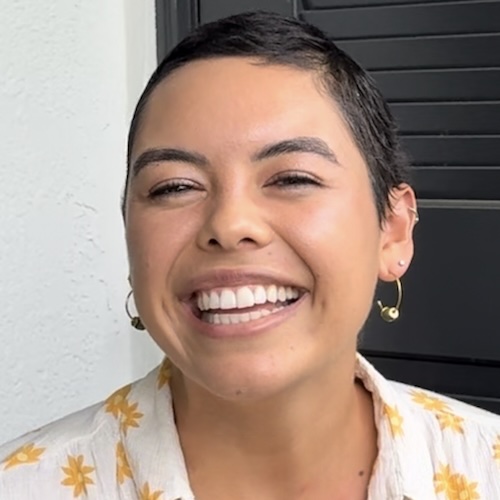
- Name: Sophie F.
- Diagnosis:
- Ewing Sarcoma
- Age at Diagnosis:
- 31
- Staging:
- Stage 2
- Symptom:
- Appearance of a nickel-sized, blue, and solid but soft and spongy mark on upper left arm
- Treatments:
- Surgeries: cyst excision surgery and wide excision surgery
- Chemotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
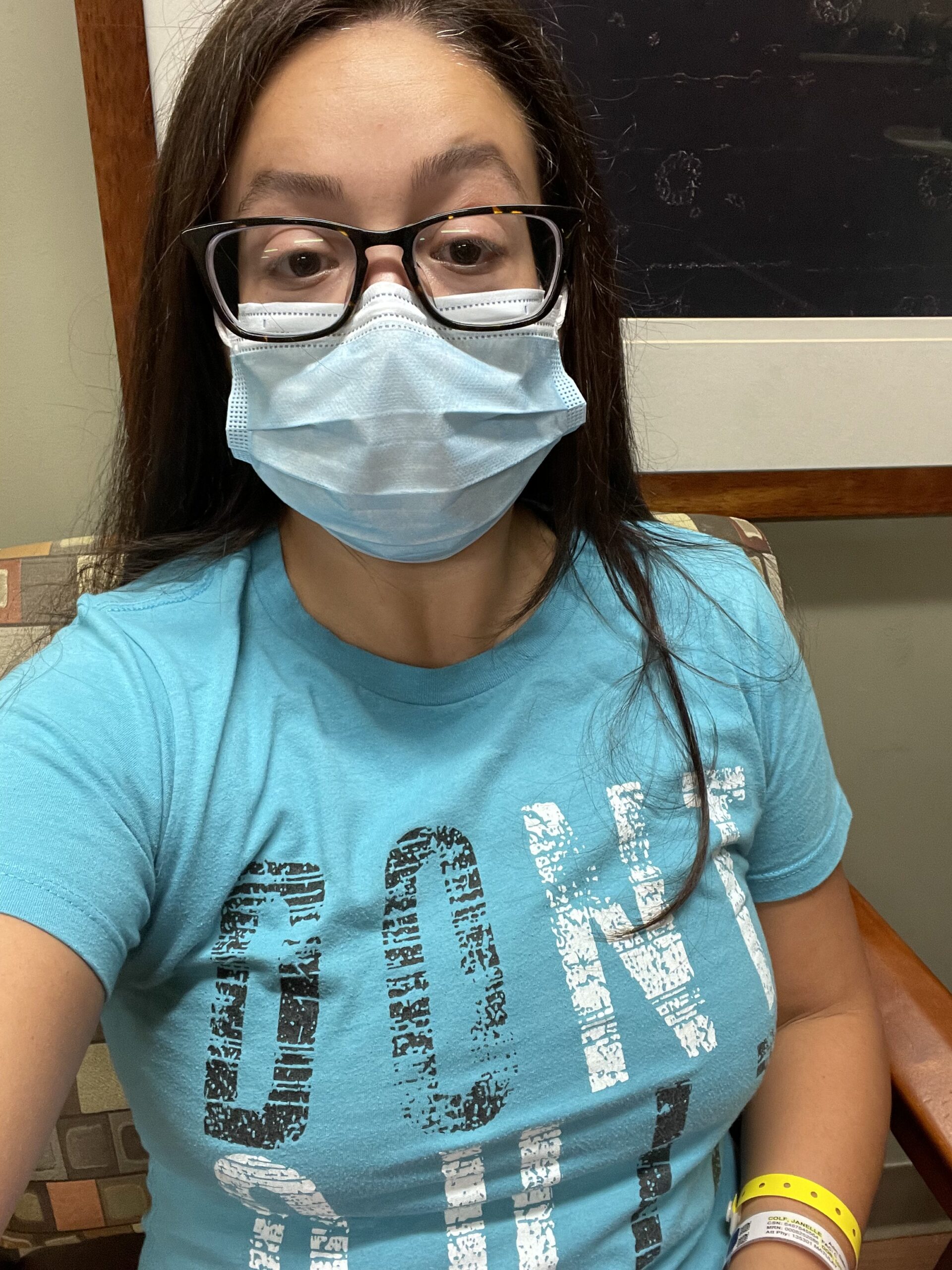
My name is Sophie
I was diagnosed with Ewing sarcoma, soft tissue, in 2022.
I only had one symptom
One day back in fall 2021, I was looking in the mirror and caught a glimpse of the side of my left upper arm, and it looked like there was a bruise there. But it was weird-looking, just slightly different. It was not faded and didn’t have that kind of blue-yellow color. It was pure blue, almost like robin’s-egg blue. And it was perfectly symmetrical, perfectly round, and the size of a nickel. It wasn’t sore to the touch, it didn’t hurt at all. It wasn’t raised. When I touched it, I could move it back and forth under the skin. It was moving as a solid, if that makes sense.
Within a week or two of noticing this strange bruise, I went to the doctor, because a bruise typically goes away pretty quickly and also hurts. I knock into stuff at the time, but this was significant enough that I should have remembered what I did that caused it.
The doctor I saw, who wasn’t my PCP but who was in the practice, barely examined it. I don’t even know if she touched it. She looked at it and basically said, “It looks fine, you’re young and healthy, and you have no other symptoms, so maybe it is a bruise. Or a hematoma, or a fatty deposit. But I’m not really worried about it. If in six months, it’s still there, you can come back.”
So I went home. But it didn’t sit right with me that she barely checked it out. More importantly, it didn’t make sense with what I was seeing and feeling. So, within two weeks after that visit, I called the doctor’s office back and said, “Look, I need to get back in sooner than six months. I’m not comfortable with someone not taking a closer look at this.” But I was told that there were no slots available for six months.
I finally saw my primary care doctor
She thought it was weird that the mark hadn’t gone away already. She suggested getting an ultrasound to get more information. So I went to get one. That took a couple of weeks.
The ultrasound results were those of an abnormal cyst. So it looked like a cyst, like a fluid-filled sac. But what was abnormal about it was that it had blood flow, which cysts usually don’t have. So I asked her what that meant, and she said kind of could mean a variety of things. She said, “I’m still not concerned, but we have a couple of options moving forward. We can watch it for a few months, you can do an MRI to get more information, or you can just have surgery to get it removed.” At this point, it had been four months since I first noticed it. So I went, “I just want surgery.”
I didn’t know anything about the steps you’re supposed to take if it’s something suspicious, because I had not dealt with that before. And she never said, “I think this might be cancer.”
The day of surgery
Finally, in February 2022, I went and got it removed by a regular surgeon. She wasn’t worried about it after the surgery. She called and said, “It went well. It was mostly just blood in the cyst. And it didn’t look weird. I’m not concerned about it or anything, but I’m sending it to pathology as part of the process.” I thought it was no big deal since I felt fine and it was just a small incision.
But a week later, she called again and said, “I’m really sorry. I was wrong. It’s actually cancer. We don’t know what type of cancer it is yet. We’ve sent it to pathology here in Syracuse. And they’re not coming up with a definitive diagnosis. It could be anything from blood cancer to skin cancer to Ewing sarcoma, which is our best guess.” I’d never heard of Ewing sarcoma before. She added, “Don’t look that up, don’t freak yourself out. We’re sending it to Memorial Sloan Kettering in New York City, and they’ll run their pathology.”
But knowing that it was cancer, I got set up with an oncologist and a surgeon and everything. It was three weeks before I got my official diagnosis on March 1, 2022, and they turned out to be correct. It was Ewing sarcoma.
How I reacted to my diagnosis
I was shocked, for sure. I was terrified and distraught. I think that phone call where she told me I had cancer was the most scared I’ve been throughout the entire experience. Not only was I hearing those words when I just turned 31, but they didn’t even know what it was specifically.
I was with my friend when I got the phone call. It was on a regular weekday afternoon. I immediately called my parents, and they came over, and my friend left. It traumatized her, too, understandably. I cried for a good while. More than anything, I was just terrified not just of cancer but because I was imagining all the things that it could be and what that could mean for me. There wasn’t any information yet about how aggressive it was, if it was localized, or even what category it fell under. So, yeah, the initial reaction wasn’t great.
My treatment plan
So the treatment plan was typical for Ewing’s sarcoma. It was very specific and targeted. It covered five chemotherapy drugs over the course of eight months to a year, depending on how the patient’s body reacts.
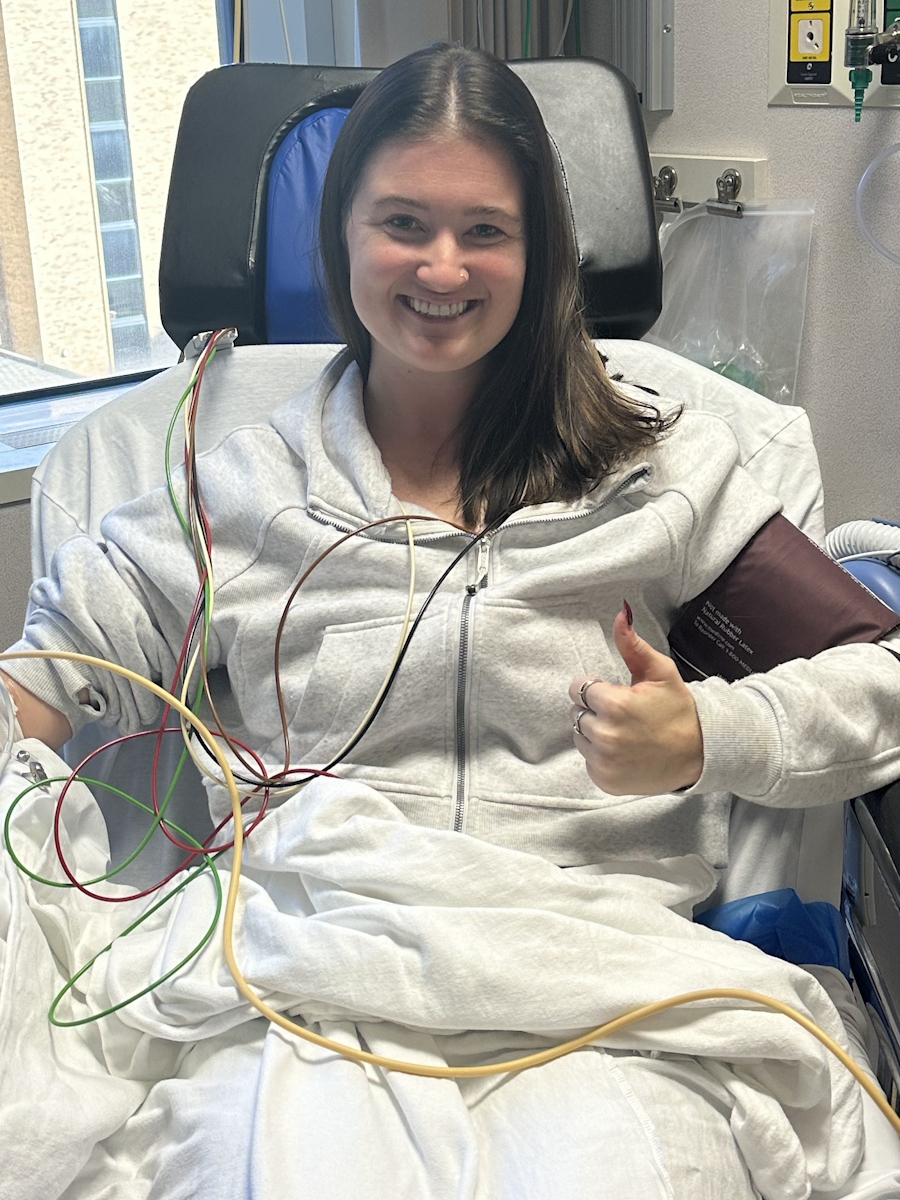
So for me, it was 14 cycles total, seven of which were inpatient and seven outpatient. The outpatient was typical chemo, where you go to an infusion room and you get an IV with chemo along with other people. The inpatient ones required me to stay at the hospital for a week at a time and get two or three drugs a day for five days in a row. I would have two days of the outpatient chemo, and then, two weeks afterward, five days of the inpatient chemo, and then two weeks later, and moving forward, that had to be spread out a little bit more because my body started taking longer to recover. In total, it ended up taking me about ten months.
Also, with Ewing’s, if it’s operable, you do surgery. Mine was, because it was in the soft tissue. Typically, this is done about halfway through, after, say, the first six cycles of chemo and before the remaining cycles. For me, when I had the initial cyst removal, they didn’t get clean margins because they weren’t operating as if it were cancer, just a cyst, so they didn’t take a lot of the area around the cyst. I needed to have that second surgery, wide excision surgery, in the midst of my chemo. And that was basically to take an extra inch around where the original tumor had been to get clean margins.
The side effects I experienced
The chemo was very challenging because I had a whole host of side effects. The main one was extreme fatigue. I would be insanely exhausted after chemo. After outpatient chemo, I would usually have two or three days when I would crash and then just be down for five or six days. When I was in inpatient chemo, it would be five days in a row. Maybe the first or second day wouldn’t be so bad. But by the third day, I would be spent. And that would last for up to a week after I got home. I would sleep about 12 to 14 hours a day and still be exhausted. I would get up to try to force some food down and then go back to sleep.
Other side effects I faced were nausea and lack of appetite. I only actually vomited once during my entire treatment, but that said, I still did get severely nauseated. I also had zero appetite and really did not want to eat. I actually had a food aversion; it would really gross me out to see food. And I also lost all my hair on my entire body. I usually don’t think about that side effect because it was expected. I knew it was going to happen. Still, though, it was not an easy thing to go through. I had other side effects too, like mouth sores once in a while, and some gland pain.
Once I spaced out my treatments, which took place after the third or fourth round, a lot of these side effects actually eased up. And I never needed to go back to the ER. I learned how to manage the various cycles and their side effects. It got a little bit easier for me after that.
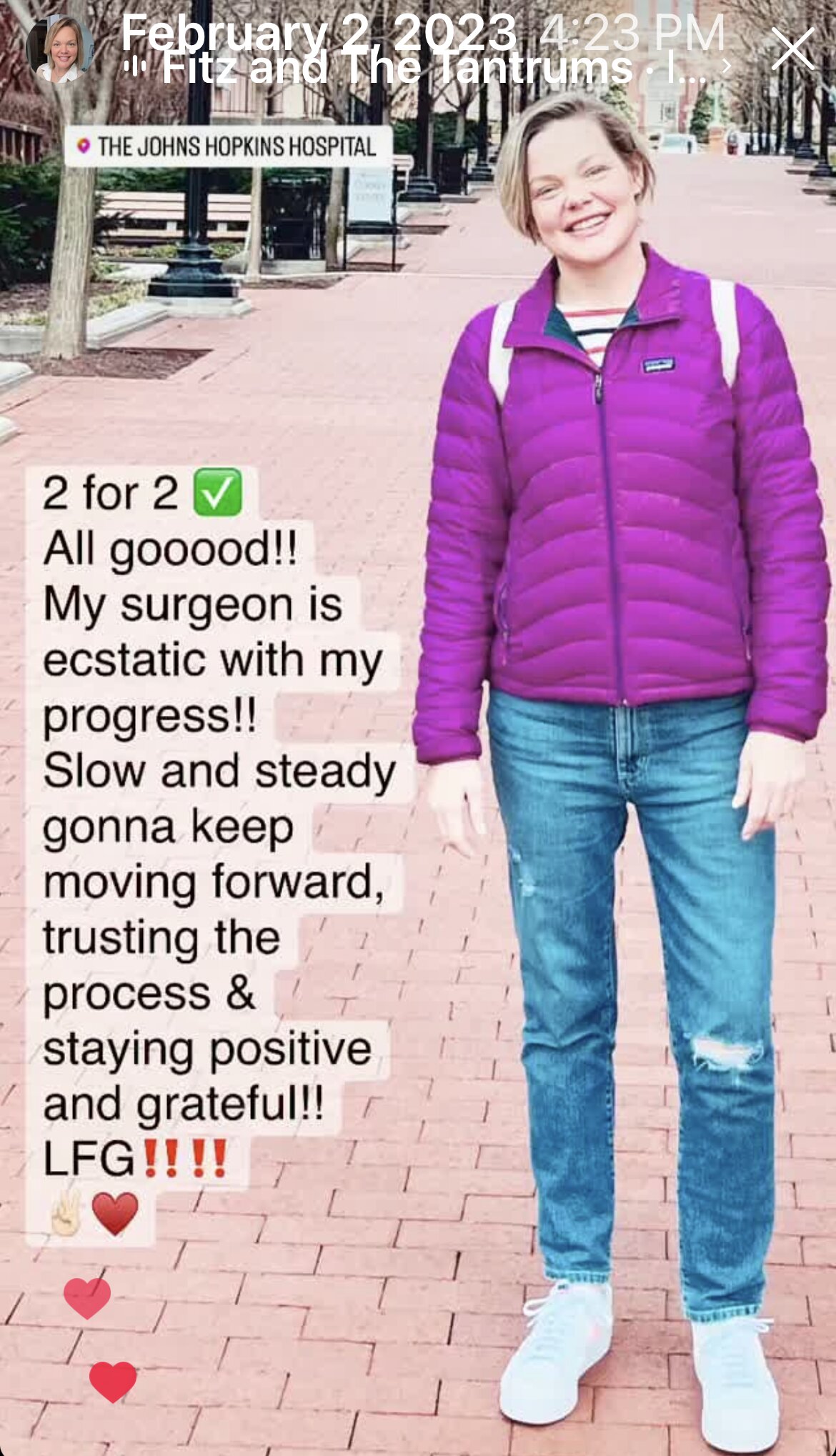
I currently have no evidence of disease
I was told that for patients who have Ewing’s and maybe all other sarcomas, they don’t use the phrases “in remission” or “cancer-free.” They use NED, “no evidence of disease” or “no evidence of active disease.” I was actually considered NED after my second surgery, about six months before the end of my treatment, because the evidence of disease was the positive margins I had after the initial cyst removal surgery. So once they got clean margins, it was technically dead. My NED anniversary is in July.
But I still had to do the rest of the chemo even though I was declared NED. That’s the protocol for Ewing’s sarcoma. And every three months for the first two years afterward, I would get scans, like a scan of my arm where I had the cancer and a scan of my chest, too, because if the cancer comes back or metastasizes, those are the most likely places it will go — my arm where the original one showed up, or my lungs. So, scans every three months aside from bloodwork to see if my body is recovering the way it’s expected to or if there’s anything new and weird that they need to investigate.
The hardest part of my diagnosis
There are so many things that were hard, some of which continue to be hard. I don’t want to downplay how tough chemo was, for example. I mean, it was like a living hell a lot of the time. But even harder than that was the psychological and emotional toll that cancer took and continues to take.
Any time you’re told that you have cancer, it’s absolutely awful and life-changing, and not the way you want it to be. But I think finding out and being told at a relatively young age was just that much harder. I was in the prime of my life. People around me were getting engaged, getting married, having kids, buying houses. And I was stuck in time. It felt like everyone else was advancing, while I was standing still — or fighting for my life — and finding out whether or not I was going to die. It really messed with my perception of my own life. What I thought my life was going to be, what I expected for myself, my assumptions, like I had assumed I would be healthy until I was old.
My mom is actually a breast cancer survivor; ten years this month. She was 60 when she was diagnosed. So I did have experience with these things, but she was 60 and I was half her age when mine was diagnosed. I never saw it coming. That was really challenging. That was the hardest part, when I had to face my own mortality at a young age, when my peers didn’t need to. It was just a given for them, like they were healthy and would live long lives. And that’s how it used to be for me, too, but it was taken away all of a sudden. That was not easy at all.
In terms of who I am now versus who I used to be, it’s sort of the same. I used to be innocent about my expectations for my life and my hopes and dreams, and how I wanted my life to look. It’s different now.
What I want others to know
I have one piece of advice, but it has two parts.
One would be a logistical answer: advocate for yourself. Don’t take no for an answer if you think something is weird or wrong, even if you have health anxiety, even if you’re anxious to begin with. Push away, because you never know, and it’s better to be safe than sorry. It’s better to have something looked at and then find out it’s nothing rather than having someone brush you off or not have it checked at all and then find out it’s something serious and even potentially at a later stage. Push for answers, push for yourself, take care of yourself. Make sure that people are listening to you. Get a second opinion, especially if you are diagnosed with cancer, ideally somewhere where there’s a specialist. There was no sarcoma specialist at my local hospital, and I had to go for a second opinion at MSK to get the peace of mind that I was getting the right treatment.
The second is not logistical: cancer is tough, but you’re tougher. There are a lot of platitudes like that, but you really are stronger than you think you are. I used to be really squeamish and scared of blood and needles and doctors’ offices. And one of my first thoughts was, “How am I going to get through this? I don’t thrive in this environment. I’m scared of it. I hate being sick. What if I can’t do this?” And the answer is, you just have to. And so you will. You can do many more things than you think you’re capable of, simply because that’s the situation you find yourself in. And it’s what’s in front of you. Just take it one step and one day at a time. Look at what you need to do to move from one place to another. And eventually you’ll be in it, and hopefully you’ll be done with treatment and living a cancer-free life. Make sure you lean on your supports. Find the people in your life who are going to stay and who are going to help you. They’ll help you get through anything.

Inspired by Sophie's story?
Share your story, too!
More Ewing Sarcoma Stories
Ariane B., Ewing Sarcoma (Bone)
Symptoms: Aching in arm, lump in forearm
Treatments: Chemotherapy (14 rounds), surgery (of radius), radiation (36 sessions)
...
Brandi B., Ewing Sarcoma (Soft Tissue), Stage 1B
Symptoms: Extreme fatigue, lump in pelvic area
Treatments: 17 cycles of chemotherapy in-patient at hospital with (leg-sparing) surgery in between
...
Sophie F., Ewing Sarcoma (Soft Tissue), Stage 2
Symptoms: Appearance of a nickel-sized, blue, and solid but soft and spongy mark on upper left arm
Treatments: Surgeries (cyst excision surgery, wide excision surgery), chemotherapy
...