Lindsay’s LAMN Appendix Cancer Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

Lindsay was diagnosed with a very rare appendix cancer called LAMN or low-grade appendiceal mucinous neoplasm. She found out that she had LAMN appendix cancer after discovering an ovarian cyst.
As she was training for a marathon, she noticed that she had an increasing urge to urinate and was going to the bathroom more often.
She had a history of really bad periods, including bad cramping and terrible bloating. Multiple doctors kept telling her to go on the pill or have an IUD inserted. Before she could get an IUD, her doctor wanted her to have an ultrasound done. Results showed what looked like a complex ovarian cyst.
While undergoing surgery to remove the cyst, her gynecologic oncologist recognized that something was going on with her appendix and abdominal cavity. She was familiar with appendix cancer and immediately knew what to remove, what to biopsy, what pathology to request, and what the next steps were.
Appendix cancer is often misdiagnosed as ovarian cancer or overlooked as a gynecological issue so she was lucky that she went to a gynecologic oncologist who was familiar with it.
In addition to Lindsay’s narrative, The Patient Story offers a diverse collection of patient stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Name: Lindsay B.
- Diagnosis:
- LAMN (low-grade appendiceal mucinous neoplasm)
- Initial Symptoms:
- Increasing urge to urinate
- Treatment:
- Cytoreductive surgery (CRS)
- Hyperthermic Intraperitoneal Chemotherapy (HIPEC)

Introduction
I live in New York City.
I’m from Manhattan. I live on the Upper West Side with my dog Charlie, who I adopted in 2020.
I love running. I’m really into Peloton. I love to travel. I equally love the beach and the mountains so I can never choose between one or the other.
I love trying new foods and new restaurants. Natural wines have been a new thing that I’ve been exploring. I love listening to live music and going to concerts.


Pre-diagnosis
Initial symptoms
I’ve always had really bad periods, including bad cramping and terrible bloating. In the last few years leading up to my diagnosis, I noticed that it was getting worse.
I had been speaking to multiple doctors to try and figure out what was going on with my period and what I thought was endometriosis. They kept telling me, “Take birth control or go on an IUD,” but I wanted to get down to the root of it.
I was actually at my healthiest. I was training for my fourth marathon when all of this started. I noticed I was going to the bathroom more often. I’d drink water and 10 minutes later, I immediately had to pee. I couldn’t hold anything.
Discovering an ovarian cyst
It turned out that I had an ovarian cyst. The only reason we found out was because my gynecologist told me I needed to get an IUD so I would need to have an ultrasound to make sure that everything was all right down there. Thank goodness because, if not, we would have never found this.
I got the ultrasound and it showed what looked like a complex cyst so they wanted me to get an MRI. This was the weekend of the marathon. The marathon was on a Sunday. I had my MRI appointment on Friday morning.
The biggest thing I was worried about at the time was that the contrast they were giving me was going to mess up my nutrition and my hydration plan.
I was ready to run this marathon. I had a goal time. I wasn’t just running it to complete it so I was feeling really good.
The cyst itself wasn’t painful. It was really mostly around the time of my period that it would get really painful.
When we were in the office pre-COVID, there were days that I’d be sitting at my desk thinking I’d have to leave early because of such bad period cramps. But it was coming from the smaller-sized cyst at that time.
Nearing my surgery, I started to feel where it was and it did get uncomfortable, but it wasn’t very painful. It was more just this bloated discomfort.




Ovarian cystectomy
A couple of days after the marathon, I got a call from my doctor saying that the cyst was huge and very complex with all of these bumps. It needed to be removed then he referred me to an oncologist. I thought, I don’t need to go to an oncologist. Everyone gets cysts.
No one really thought that a cyst was going to lead to cancer because I was so “young” and feeling healthy. I ended up going to an oncologist who removed it.
Thank goodness I did because, during surgery, she recognized that something was going on with my appendix and my abdominal cavity. Because she was familiar with appendix cancer, she immediately knew what to remove, what to biopsy, what pathology to request, and what the next steps were.
Feeling that something was wrong
I’ve been running with the same running group for at least 10 years and I’m very close with the coach. During training, we did a half marathon. It was the same 4 1/2-mile loop over and over. There were two porta-potties halfway through each loop and every time I passed the same porta-potty, I had to stop and pee.
I’ve run 15 or 20 half marathons. I’ve never once had to stop to go to the bathroom. I told my coach, “My pace was great, but my time is all messed up because for the first time ever I had to stop to pee every time I hit that same bathroom.” He joked, “Finally, after all these years, you followed the right hydration plan and hydrated properly; that’s why you had to go pee.”
It turned out the cyst was the size of a grapefruit or a softball, they said. I’m very petite so it was pushing against my bladder and that’s why I was constantly having to go to the bathroom.
I knew something was up with my body. I was feeling really bloated. It wasn’t weight gain because I was in the best shape of my life at that point. I knew something was up, but I just didn’t know what it was.
Gynecological issues get downplayed. Take a pain reliever, take a leave, or take birth control but that’s not really fixing it. It’s just putting a Band-Aid on it. I got frustrated after all these years and really wanted to get to the bottom of it.


What if it’s cancer?
It’s ironic because I ran the marathon with the American Cancer Society. We had a team pasta dinner the Saturday night before the marathon. At dinner, a member of the team told her story.
She said, “At this time last year, I was sitting right where you were. I was trained for the marathon, ran the marathon, then a week later, I found a lump in my breast, and it turned out to be pre-cancer.”
I got up to go to the bathroom with my mom and said, “It’s kind of freaking me out because what if that’s me? What if I have cancer?” It was the first time that I ever really thought of that.
I’ve had an abnormal amount of friends and family over the years who have had cancer. It never once crossed my mind that what I was going through could have been cancer, which was very naive of me.



Biopsy
My primary care doctor referred me to a gynecologic oncologist. I met with a couple of other doctors, but I ended up loving this woman and having the surgery with her.
They removed the cyst through laparoscopic surgery. While she was inside, she noticed that my appendix was huge and had a tumor on it and that my abdominal cavity was filled with what looked like mucus.
She kept calling it a jelly-like substance. She had a hunch of what it could be, but she didn’t really get into detail. She said, “Let’s run pathology on it then we’ll figure it out. Let’s not worry about it.”


At that point, she removed my appendix, she removed as much as she could of the funky (as she called it), jelly-like substance. The cyst was so big that it had completely taken over my ovaries so she removed the right ovary as well and ran pathology on it.
I knew something was wrong because I had an appointment the following week with her PA as a follow-up to the surgery. It wasn’t an easy surgery because it was a lot to recover from, but they do these all the time. I didn’t need to see her again. They were going to look at these four holes, tell me that I was healing fine, and move on.
The oncologist called me the night before my appointment and said, “Can we change your appointment time? I want to see you because I want to talk to you about the pathology reports.” That’s when I knew something was wrong. That’s when it hit me.
I actually called my parents separately because I thought maybe she told them something that they didn’t tell me because she spoke to them immediately while I was in recovery. I thought maybe they were trying to hide something from me so I wouldn’t worry.
I called them both and said, “What did Dr. Villella tell you? Because now she wants to talk in person and she said that it’s exactly what she thought it was going to be.”
The reason I say I’m lucky and I’m glad that I went to her is that so many oncologists don’t know what appendix cancer is. Even if you’re not an oncologist, so many people just have their appendix removed.
She recognized that this could be coming. They did biopsies for ovarian cancer and everything else, but she knew to include appendix cancer.





Diagnosis
Getting the official diagnosis
My parents came with me to the appointment. I sat on a table and she put her hand on my knee and said, “You’re going to be okay, but this is going to be a difficult, difficult couple of months for you.”
Then she explained that it is this extremely rare appendix cancer, that it’s the best of them, that there are several different kinds, and that if I was going to get diagnosed with appendix cancer, this is the least invasive.
It’s all a blur, but the biggest takeaway I got was that it cannot spread the way other cancers spread so I don’t have to worry about this becoming breast cancer or lung cancer. It’s going to be very contained.
I was going to need another major, major surgery that sounded completely barbaric and foreign to me, something I’d never heard of. I would not need systemic chemo, but it would be another type of chemo treatment.
My parents cried. I was too in shock to cry.
The doctor printed out some medical journal articles and highlighted certain things. I was so thankful that she did. She said, “I think that you are smart enough that you could read through this and will understand a little bit more about LAMN. I wouldn’t have printed this or gone this deep into it for most patients, but I think that this would be useful for you.”
She even gave me printouts of photos that they took inside and showed me where the mucin was on my organs, what it looked like, and how much was there. I understood that part of it and that’s pretty much all I left with.


Reaction to the diagnosis
It was a shock. I remember it so well. It was in December. My mom stayed over that night. We tried to watch all these Christmas specials to take our minds off of it, but it was very overwhelming.
It’s horrible enough to be told you have cancer, but to be told you have a type of cancer that you’ve never even heard of before is just next level.
No one ever expects to hear, “You have cancer,” but to hear you have a type of cancer that you didn’t even know existed is another blow. It’s like getting hit in the gut and then getting punched even harder.
There’s no research on it, which was why she gave me printouts because she said it’s going to be hard to find data to help make treatment decisions. She recommended an oncologist that she worked with before, but she encouraged me to meet with as many other specialists.


She said, “Find as many people as you can that have heard of appendix cancer. Meet with them and hear what they have to say. You don’t have to have your next surgery with me and with this other guy. You could do it wherever you’re most comfortable, but find out what you can and come back and report it to me. I want to hear what you find out because this is fascinating.”
I think she actually said something like doctors are going to want to meet with you because they’re going to be so fascinated to meet someone that has appendix cancer because they probably never have or will.
Not having much research data available
It was really, really frustrating, especially when it came to the treatment, the fertility part of treatment, and certain decisions that had to be made with my treatment plan.
It wasn’t black and white. There’s not enough research that says if you do this, you will have this outcome or if you have this treatment, you will not be able to have children.
There are just so many pieces to it. I was extremely overwhelmed, but I was in major fight-or-flight mode, which I’m sure everyone gets into when they have a diagnosis like this.


Meeting with specialists
I met with a couple of top specialists in the city. I’m so thankful that I live in a city where I have access to these doctors and that you can meet virtually so I didn’t have to take a lot of time off from work. I would hop on a call with a doctor and get back to work.
I made it a point to meet with as many doctors as I could until I could fully understand what the treatment plan was and actually retell it to someone. Until I was able to explain fully what was getting done, I was not ready to make any decisions.
I was completely overwhelmed; that was the biggest feeling. I wasn’t sad or angry. It was just overwhelming how I had so much to do and no idea where to start.
I ended up sticking with the GYN oncologist who did my surgery at Lenox Hill. There’s a GI oncologist who she works with who has done this type of procedure before. I ended up moving forward with them.
I met with two other GI specialists. One is at Sloan-Kettering. He’s done incredible research for appendix cancer and he’s very well known in the appendix cancer world, but it just was not a fit for me.
Then I met with this other doctor at Mount Sinai who is very well-experienced in HIPEC. He was recommended by a friend of mine. Her husband went to him and he was really nice and answered all these questions.
At the end of the day, I felt like there was more of a team effort with the doctors at Lenox Hill in terms of discussing the plan. Other doctors were saying, “We should remove this, we should remove that while we’re inside. We should also get rid of your cervix. I’ve removed ovaries before. Once you’ve removed that, you can remove anything in a reproductive system.” It was not what you wanted to hear.
I ended up sticking with the original team, knowing that the GYN oncologist who discovered it would be part of the surgery. She’s already been inside me. She knows what to look for. She knows what’s there. She found it so that was where I was most comfortable. I’m so glad I went with them. They were fantastic.




Treatment
Discussing the treatment plan
Across the board, they all said that I would need cytoreductive surgery (CRS) and HIPEC, which is a heated chemotherapy bath in your abdominal cavity.
With cytoreductive surgery, they cut you open from your chest plate all the way down to your pelvic bone. The first part of the surgery is to remove any visible tumors, which are in the form of mucin, that jelly-like, funky substance. They go in and scrape out as much as they can. But mucin, because of its consistency, can get stuck to certain organs.
I was told that I would have my left ovary removed for sure because it was covered in mucin. They also recommended to remove my uterus and do a full hysterectomy.
A lot of doctors also recommend doing a bowel resection because the appendix is connected to the end of your bowel. They want to make sure that they get any cells that could have left the appendix and got in your colon or bowels.
My team at Lenox Hill said, “We will do what we have to do. We don’t remove organs just to remove organs. If we cannot clean off your uterus, we have to remove your uterus. But if we can salvage it, we will salvage it for you.” The other doctors did not say that. They immediately said we should get rid of this, this, and this.
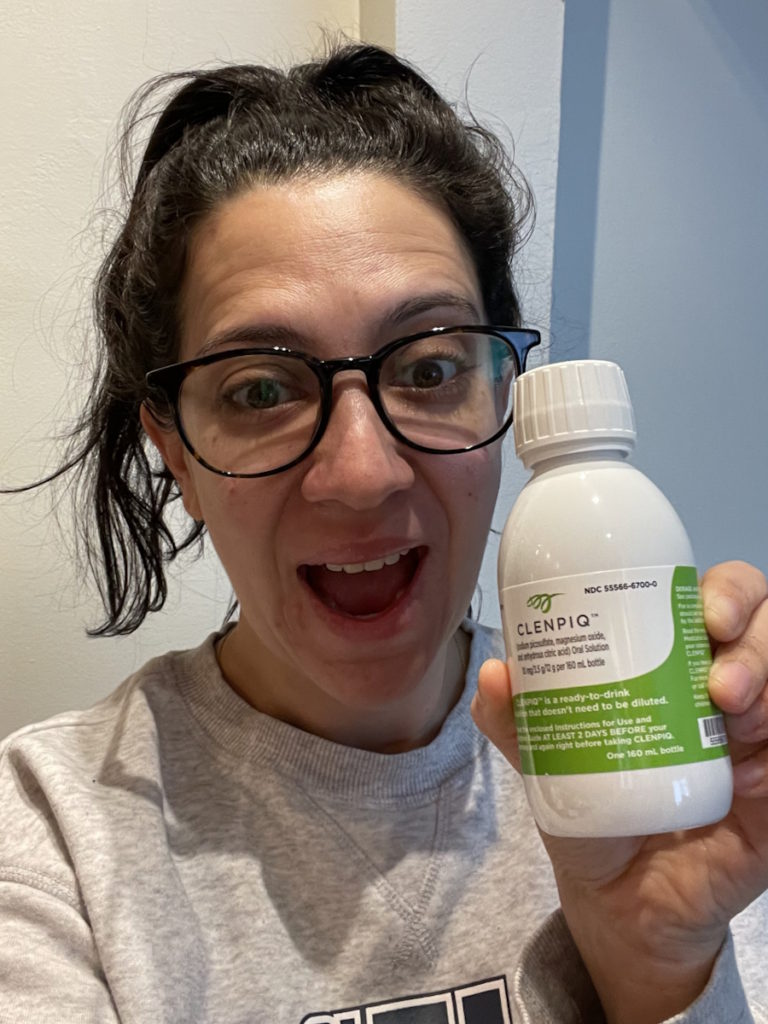
Cytoreductive surgery (CRS)
I woke up from surgery thinking I was going to have no uterus and left ovary. They were able to clean all of the mucin off and save my left ovary. It does not work though. I’m in menopause after surgery, but it’s still there.
Cytoreductive surgery involves going in and removing what they can remove and that could include organs. It’s very common to have your spleen removed. I also had a piece of my omentum removed, which is like a sheet over your abdominal cavity. I think a part of my liver was also removed and a lot of mucin.


Hyperthermic intraperitoneal chemotherapy (HIPEC)
After everything visible is removed, they temporarily close up your abdominal cavity and pump you with a very hot chemotherapy bath. They rotate your body for 90 minutes to make sure that that chemo gets into every crevice of your abdominal cavity to kill anything left.
Now, that doesn’t work for every type of appendix cancer, but for my type, it does. With certain types of appendix cancer, it’s not mucin but a different type of tumor. It’s hard and won’t break it up.
When I first heard about it, I thought it sounded very barbaric. They’re going to cut me in half and remove stuff from inside my guts with your hands and then “shaking.” A doctor I know who’s a specialist jokes and calls it shake and bake.
Find a specialist who is well-versed in this because it’s not a common treatment. It’s more common in Europe and I believe they do it for ovarian cancers. There’s a trial for HIPEC in a certain type of colon cancer. A lot of people do feel strongly for and against it, but I am a big supporter.


Recovery from surgery
Recovery was awful. Everybody warned me that it was going to be bad. But until you actually go through it, you can’t understand how bad.
My doctors and people in my support group who’ve gone through it said, “You’re not going to feel like yourself for at least 3 to 6 months. It’s going to take a full year for you to fully recover.” It’s hard to understand without going through it.
Now that I’ve gone through it, I say that to other people. New patients don’t understand it.
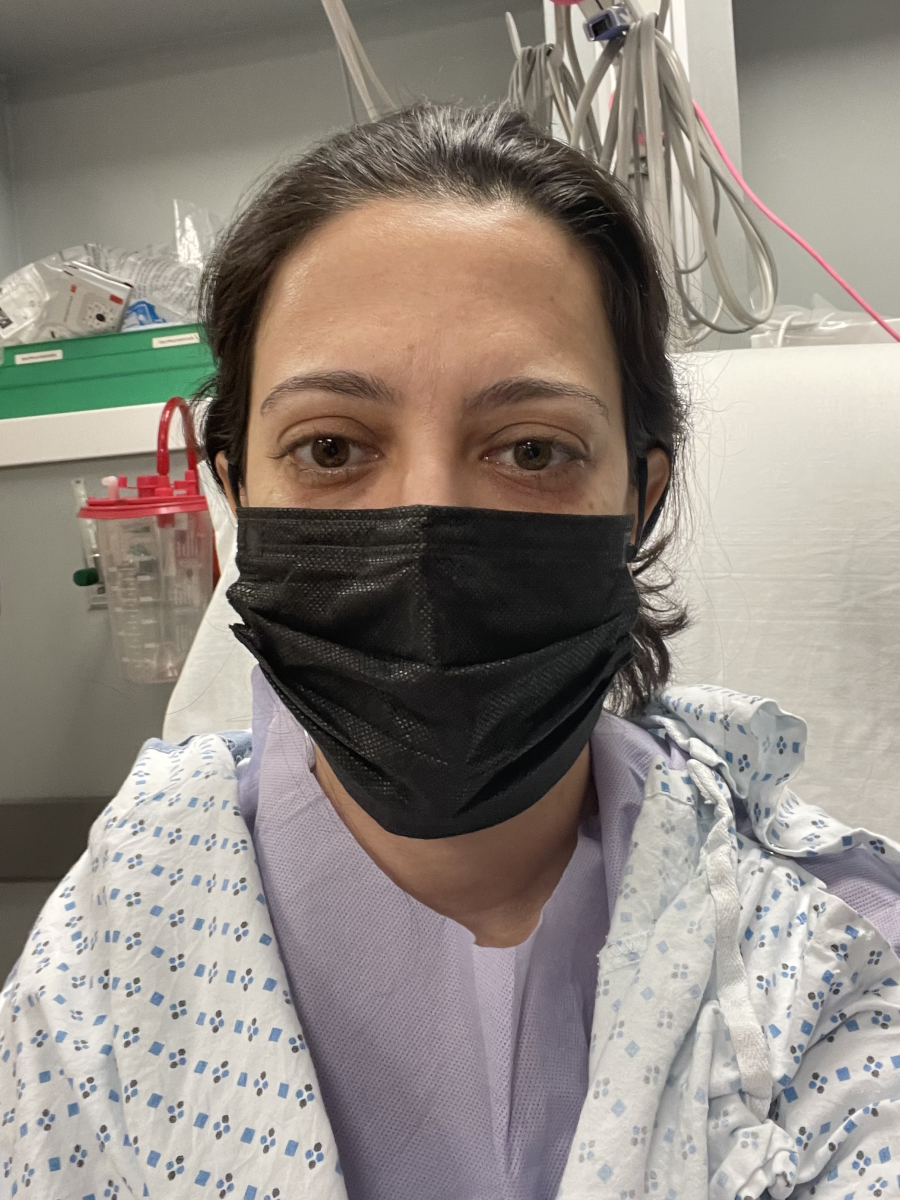
I was in the hospital for a week and had 52 staples across my abdomen. My mom had to move in with me for a couple of weeks because I couldn’t do anything on my own. I couldn’t shower without holding on to someone.
I would have to decide if I wanted to take a walk or shower. My energy levels were so low that I couldn’t do both. There were days that I would just walk up and down my hallway. It was too much for me to go all the way downstairs and walk to the corner and back so it was complete exhaustion, really bad pain.


I lost my appetite. I lost about 10 or 15 lbs. They eventually came back, which is how I knew that I was finally starting to recover. But zero appetite and hair loss, which they didn’t warn me about. I didn’t lose all my hair, but I would say at least 50 to 75% of my hair fell out. It was really thin. It’s traumatic when that happens. I think anyone would say that.
I was depressed. I went on Zoloft (sertraline) because I got to a point where I just had no motivation to do anything. I felt like the world was passing me by. I was sleeping on my couch all day long and didn’t feel like I was getting better.
It was painful. I slept on my couch for a few weeks because it was too painful to get in and out of bed. My couch was more comfortable.
I remember being in the hospital one day, looking up at the very sterile, ugly white walls, and that was when it hit me that I was a cancer patient. I was also very hyped up on pain meds. Even though I’m not your standard cancer patient who’s getting chemo and this and that, this is real.
I can’t get out of bed without someone helping me. I cried when I came home. I’m not a crier but I was crying nonstop because I went from being super independent to needing my mom to move in with me.
About a month after the surgery, I finally went back to work. I was working from home so I was able to adjust. My birthday was in June and that was my 40th. I remember hitting this wall of depression where I was thinking, I am not where I thought I would be at 40.
I could barely walk around the block. All of my friends are out celebrating their big 40th. We should be going on trips and this and that. I was just processing that I have cancer. This is going to take a lot longer to recover from. Thank goodness I didn’t have any complications, but it still was just a painful couple of months.
My oncologist said, “I think you should see a specialist like a psych-oncologist to talk through this stuff.” I did and he was very helpful in understanding what was going on
It was also a hormonal issue as well. I was going through surgical menopause and we couldn’t get the hormones right so I think all of it was messing with my head.





I’m over a year out and it’s still not easy because I always thought that I’ll just go back to normal. But it finally has hit me: there is no normal to go back to and it’s not necessarily a bad thing.
I absolutely love my life. I feel so blessed. So many of my friends really showed up for me. I reconnected with old friends. We didn’t have any falling out; we just drifted apart. When they heard what happened to me, they said, “What’s going on? I’m going to be here for you,” and they were. It was really incredible to reconnect with these people.
I’ve found this passion to advocate for women, to listen to your body, and for rare cancers.
I still sit here over a year later thinking, This sucks. I have to worry about scans every six months. I have another surgery because I have an incisional hernia, which is a remnant from my last surgery and that’s going to set me back another 6 to 8 weeks before I can get back to things.
I’m still processing it. What is this new normal and how do I adjust to it?
Fertility preservation
I feel so strongly that every woman should freeze their eggs at a young age whether they think they want kids or not because you never know what’s going to happen. It’s not an issue of whether you want kids or not. It’s an issue of having the option to have kids down the line.
I would rather say I don’t want kids but I have the option because I froze my eggs than say this cancer took away my ability to have kids. I was lucky in the sense that I had frozen my eggs a few years prior.
I did have time. They offered that if I wanted to do another round of retrievals, I could. But after having my ovary surgery, I was still really sore and tired. I knew I had this other big surgery coming up.
I was happy with the retrieval that I had. I was lucky because I know a lot of women are not even offered that because either their bodies can’t handle the hormones or they don’t have time.
Mine wasn’t an aggressive cancer so I had the luxury of taking a couple of months to really do my research and heal from my first surgery before my second one so I could have done a retrieval, but, physically, I could not put myself through something like that.


I had to make the decision of removing my uterus as a precaution or keeping it because I might want to have a kid down the line. However, after HIPEC, there is no research that says you can or cannot have a child. Yes, people have gotten pregnant after having HIPEC, but there are also people whose uterus can’t hold a baby.
Fertility-wise, am I cutting my nose to spite my face here? Am I keeping my uterus to possibly have a kid one day? I’m not even going to be able to have a kid because HIPEC is going to ruin my uterus. Then I keep my uterus and mucin can probably grow there and the cancer could come back.
Another school of thought is maybe the uterus is protecting other things in that area so if the mucin comes back, it will grow on the uterus and can be removed.
There are different schools of thought, but it all really came down to fertility for me and that’s what I told my doctors. I said, “Obviously, I know that your goal as my doctor is to keep me healthy and safe so if you have to remove it, remove it. But my hope is that we can keep it just in case I want to have a child down the line.”
Fertility is so important. You never know what can happen so preserve your eggs earlier so that you don’t have to think. I felt like I ticked something really big off my cancer list, having had done that years prior. I know it’s expensive and it’s not easy, but I think it needs to be talked about more. I think people don’t talk about it enough.



Chance of recurrence
I try to stay as up-to-date as possible with this stuff. It’s interesting because the research is changing. I was told that there is a very high chance of recurrence, but it would be within the first five years. The doctor in a recent webinar I listened to said that new research shows a much lower chance of recurrence for my specific type.
My doctor does six-month CAT scans for the first two years and then upgrades it to annual scans. But I know people in my support group who are 25 years out and still get annual scans just to be safe because it could come back.
We don’t say cancer-free or in remission. We say no evidence of disease (NED) because, right now, I have no evidence of disease, but at a cellular level, there could be some stuff down there that we don’t know about and it could come back.
We don’t have a standard timeline where if you have five years of clear scans, then you’re considered in remission because there’s just such a lack of research out there.


Knowing the possibility of recurrence
It gives me a lot of anxiety. The second I feel bloated or have a stomach ache or something, I think, Oh my goodness, it’s back. But then I bring myself back down. It’s so slow-moving. There’s no way that I’m going to wake up with a belly filled with this stuff overnight
It’ll be a slow thing, but it’s nerve-wracking. Honestly, I try and take it a day at a time. I make as many plans as I can so that I’m staying busy and getting back to things that I love, like traveling and running.
My support group actually helps a lot. We do it on Zoom. It’s all appendix cancer patients and caregivers globally. There are people from literally everywhere.
It’s a very small community because there are so few of us. But it’s helpful to talk through anxieties with them and hear other people. Sometimes you think, Am I exaggerating? Should I not be worried about this? But then you hear other people thinking about it and then you say, “Yeah, it’s not just me. This is kind of what we have to live with right now.”
Possible origin of appendix cancer
I’ve gotten a lot of different answers. This particular kind is so slow-moving that I’ve probably had this for a very long time because of the amount of mucin they found. Based on what I’ve learned, it makes it sound like it’s been there for a while.
There was a tumor in my appendix that was secreting mucin, which then created the ovarian cyst. When they did the pathology, there were traces of appendix cancer in the ovarian cyst. The cyst grew so big that it must have been there for a while. They don’t know what it’s from.
There are some new genetic tests that I keep hearing about in my support group, but I think that’s more for pathology than actually figuring out where it came from. There’s a lot of stuff going on.
For example, there’s a 9/11 thing where if you lived or worked near the World Trade Center during a certain period of time, there’s some research that says that might have affected certain types of cancers, including appendix cancer. Hopefully, we’ll have an answer one day.





Words of advice
If you feel something is off with your body, listen to it. You know your body best.
Don’t be intimidated by doctors. If you’re not getting the answers that you need, no matter how much you like that doctor, go to another doctor. Don’t worry about offending them. Some doctors have bigger egos than others. You have to take care of yourself.
Ask as many questions. Don’t feel embarrassed about asking questions and advocating for yourself. It’s so important. Many doctors who don’t know what’s going on might not know how to tell you they don’t know what’s going on. If you’re not confident with the answers you’re getting, go elsewhere.
There are limited resources and not a lot of research, especially with rare cancers. Find support groups and smaller groups that you can reach out to. There’s minimal research, but there’s some research and those organizations are extremely helpful.
I have bad days but pre-cancer, I wake up every morning and say this Jewish prayer where you say basically thank you for giving me another day. I’m here, I have another day.
I say that every day and now it just feels different. Every day, I wake up and say, “I’ve got another day. I don’t know what my purpose is, but I’m still here. The cancer didn’t get me today.”
There’s a woman in my support group who says this all the time. It didn’t get me today. It’s not going to get me tomorrow. It might get me some time. But I really just try and take it a day at a time and do things that I love doing.
I try not to take things too seriously anymore. With work, I used to get so stressed out. I don’t let that stuff bother me anymore and I feel like I’m doing really well with work right now. I’m the happiest I’ve been at work in a while and I think it’s just this new attitude.
Helping others is also something that gives me hope. I love being able to pay it forward and seeing people who have had it a lot worse than me thriving. So many people stepped up for me during this.
It is what it is. I try not to say why me or this or that. I do sometimes, but I don’t think that gets me anywhere. I try to just have a positive attitude.
When I can’t get out of a funk, I work out. I get on the Peloton and take a really hard class or go for a run to clear my mind.


Inspired by Lindsay's story?
Share your story, too!
More Rare Cancer Stories
Amanda S., High-Grade Neuroendocrine Carcinoma, Stage 4
Symptoms: Breathing problems (especially during activities like walking), persistent cough, coughing up blood, urinary tract infections, pain in belly
Treatments: Chemotherapy, surgery
...
Bella J., Malignant Paraganglioma
Symptoms: Severe vomiting, chronic cough, dizziness, swelling in the neck, low heart rate, extreme weight loss, hair loss, dental issues, vocal strain, persistent pain and exhaustion
Treatments: Surgeries, radiotherapy, physical therapy
...
Burt R., Pancreatic Neuroendocrine Tumor (PNET) & Kidney Cancer
Symptom: None; found the cancers during CAT scans for internal bleeding due to ulcers
Treatments: Chemotherapy (capecitabine + temozolomide), surgery (distal pancreatectomy, to be scheduled)
...
Jennifer P., Neuroendocrine Tumor, Stage 4, High-Grade
Symptom: Pain in upper back
Treatments: Chemotherapy, immunotherapy
...
Jonathan P., Mediastinal Paraganglioma, Stage 4
Symptoms: Shortness of breath, facial and neck swelling, vein distension, dizziness and fainting, blacking out after standing up
Treatments: Radiation (external beam radiation therapy), targeted therapy, surgery (cement injection for spinal stabilization)
...
Caroline C., Gestational Trophoblastic Neoplasia & Placental Cancer, Stage 3
Symptoms: Morning sickness & an unusually high beta hCG
Treatment: EMACO chemotherapy
...
Shannon W., Choriocarcinoma
Symptoms: Molar pregnancy, vaginal bleeding, overall feeling of unwell, cramping, weight loss, elevated HCG level, feeling bloated
Treatments: Chemotherapy, surgeries (D&C, total hysterectomy)
...






One reply on “Lindsay’s LAMN Appendix Cancer Story”
I too was diagnosed with LAMN (pT4b) and had surgery. Out came the spleen, appendix, all the girl parts. I am 72 in shape and have never been sick so this was an unexpected surprise. Recovered easily enough but cannot eat nearly as much. Will get a CT scan 6 months and blood tests. Docs say it may never come back, still very scary and I worry every day.