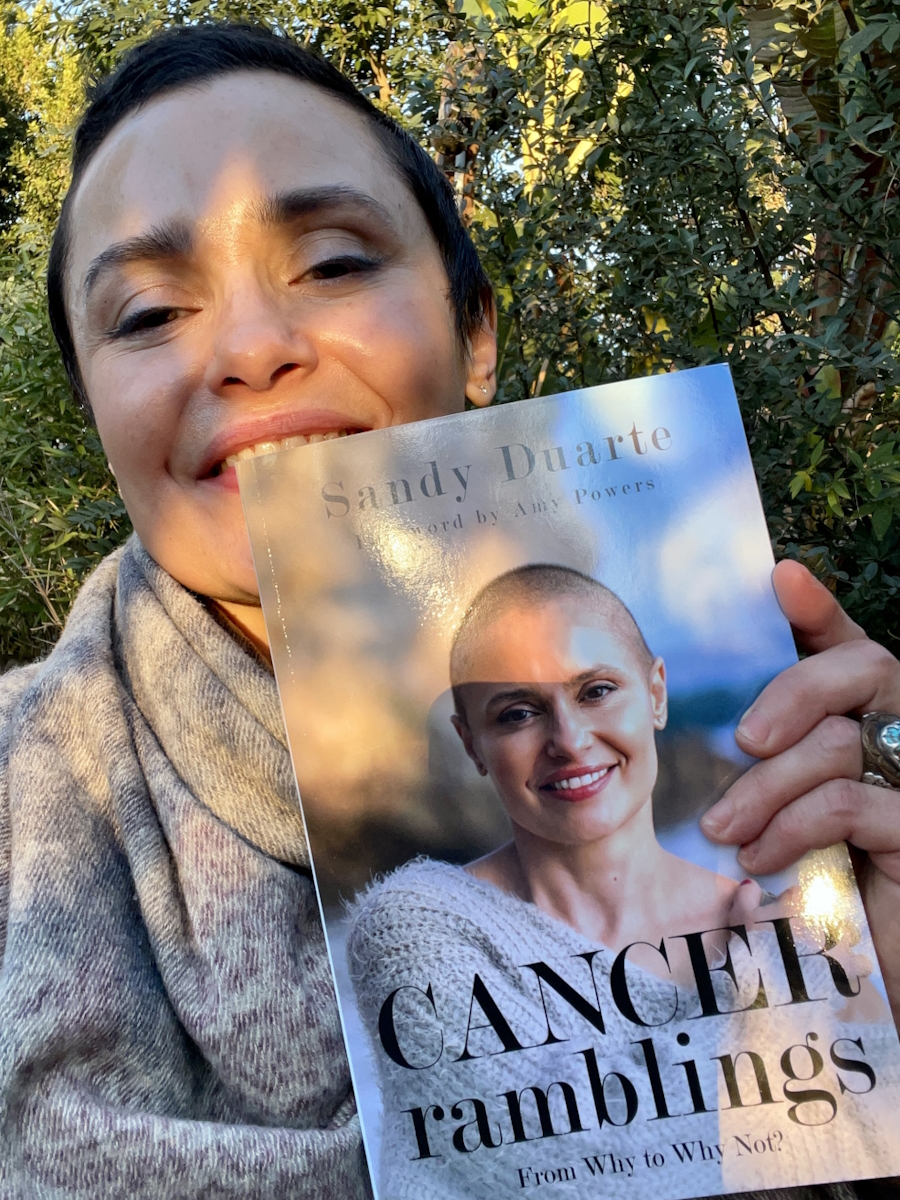
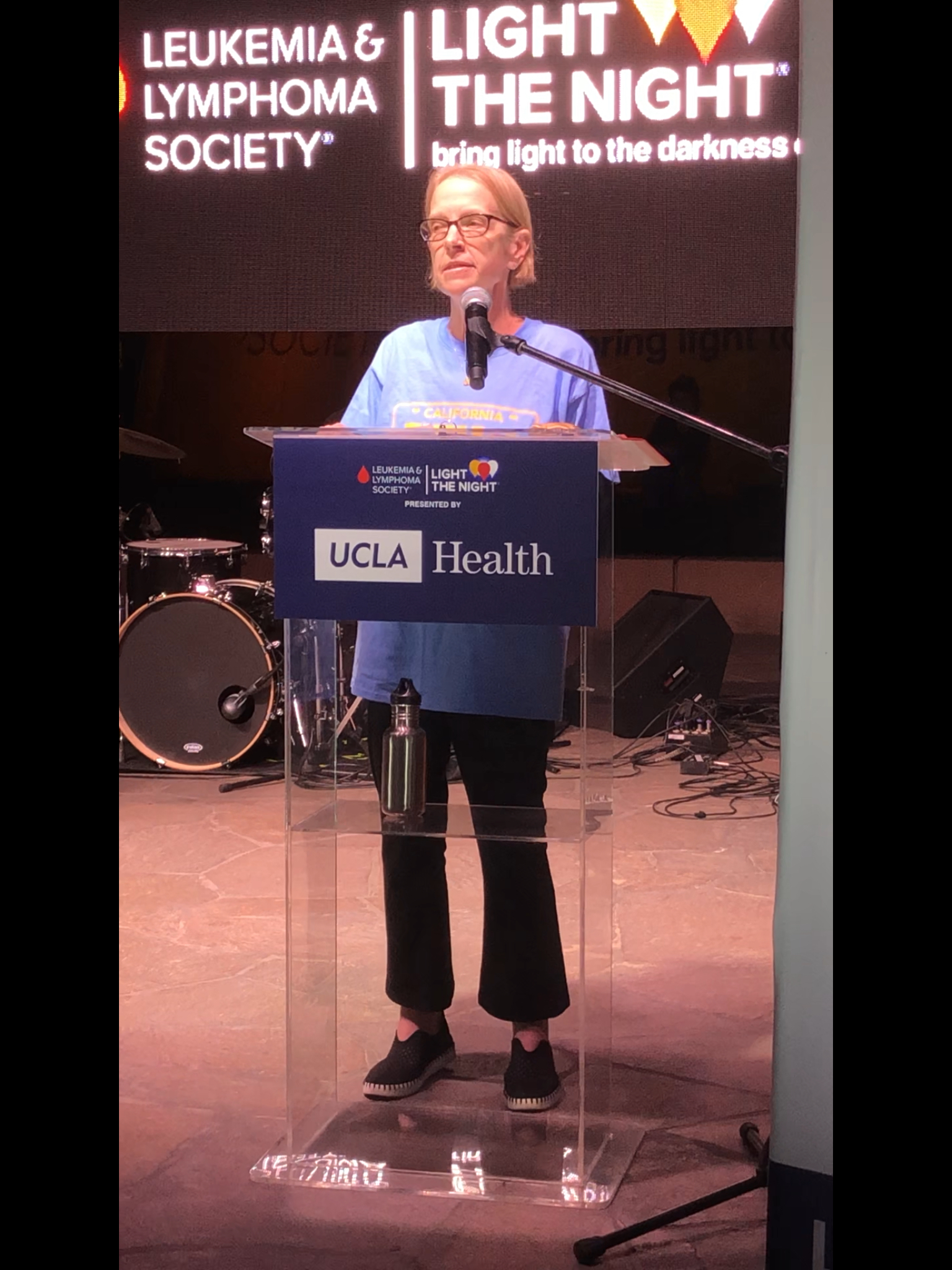
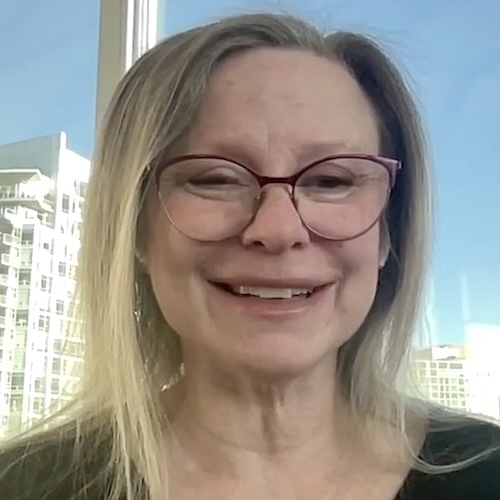
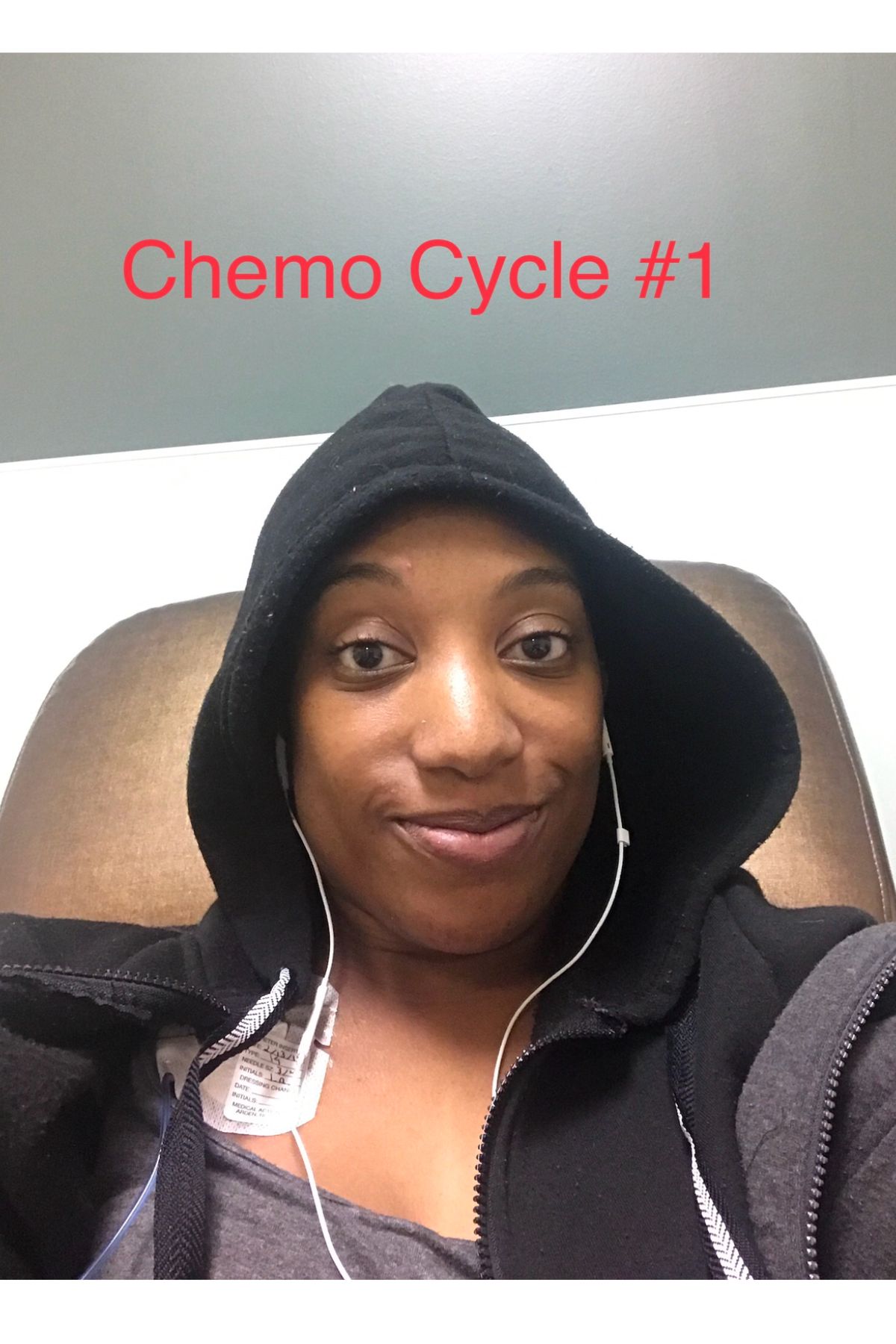
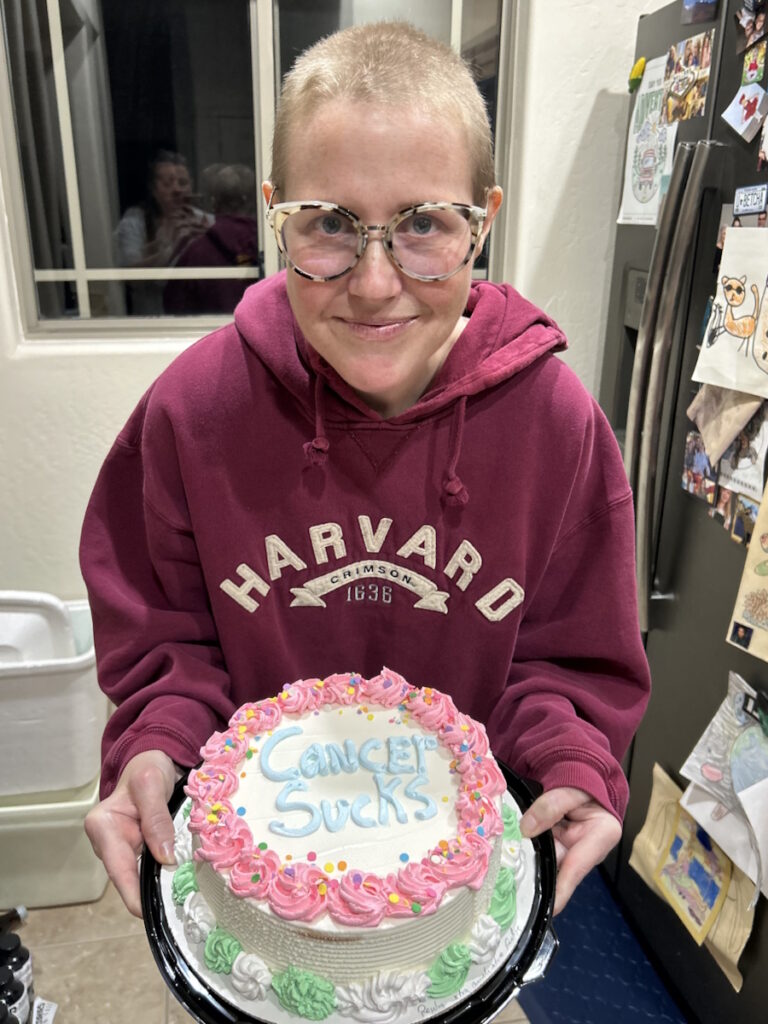
Sandy’s Stage 4 Non-Hodgkin Lymphoma Story
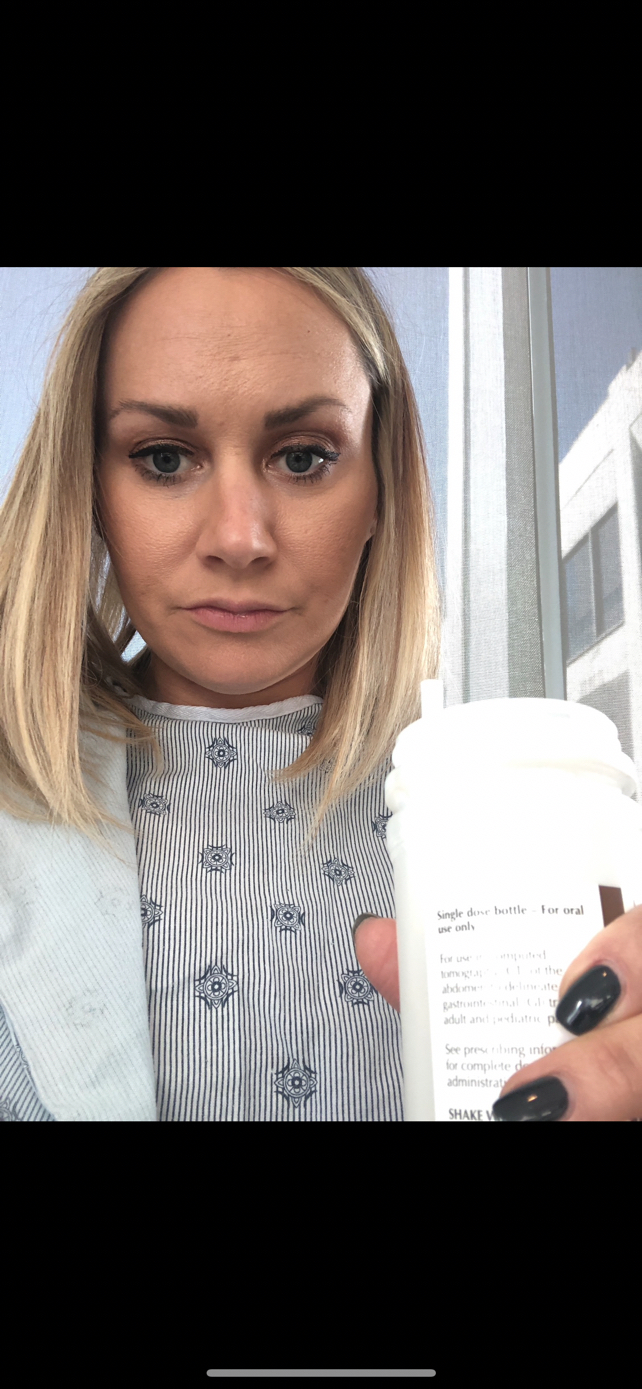
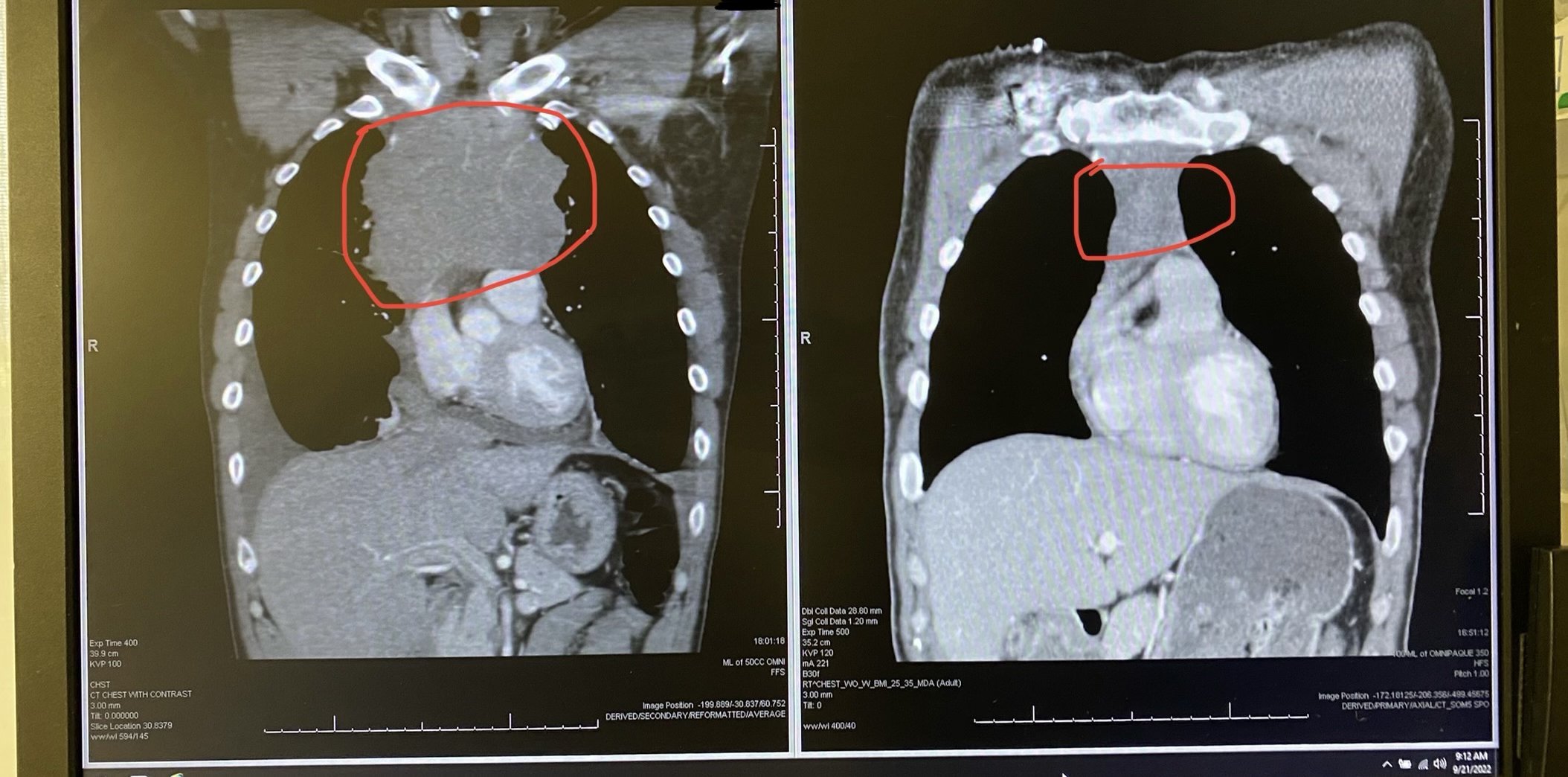
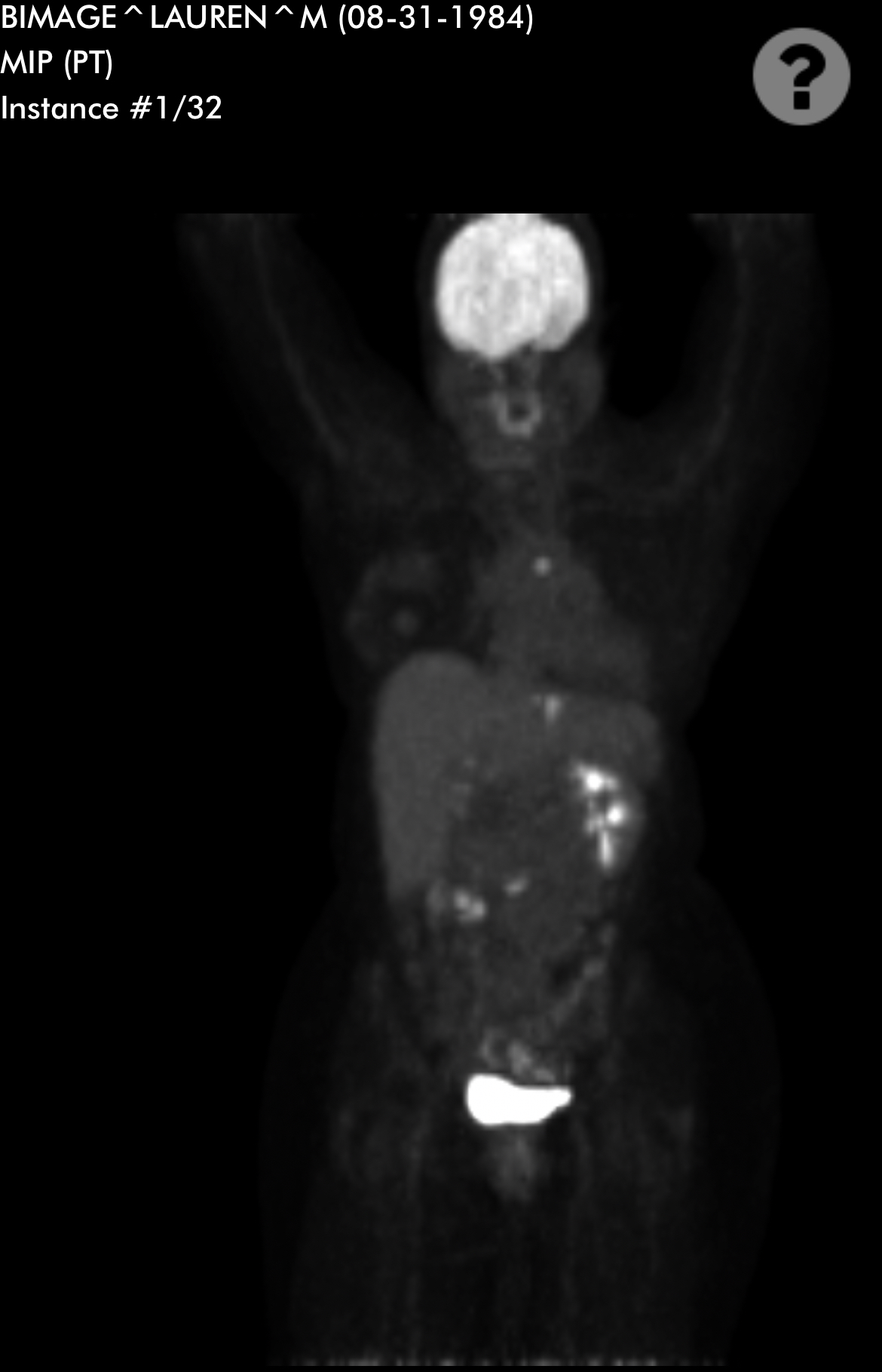
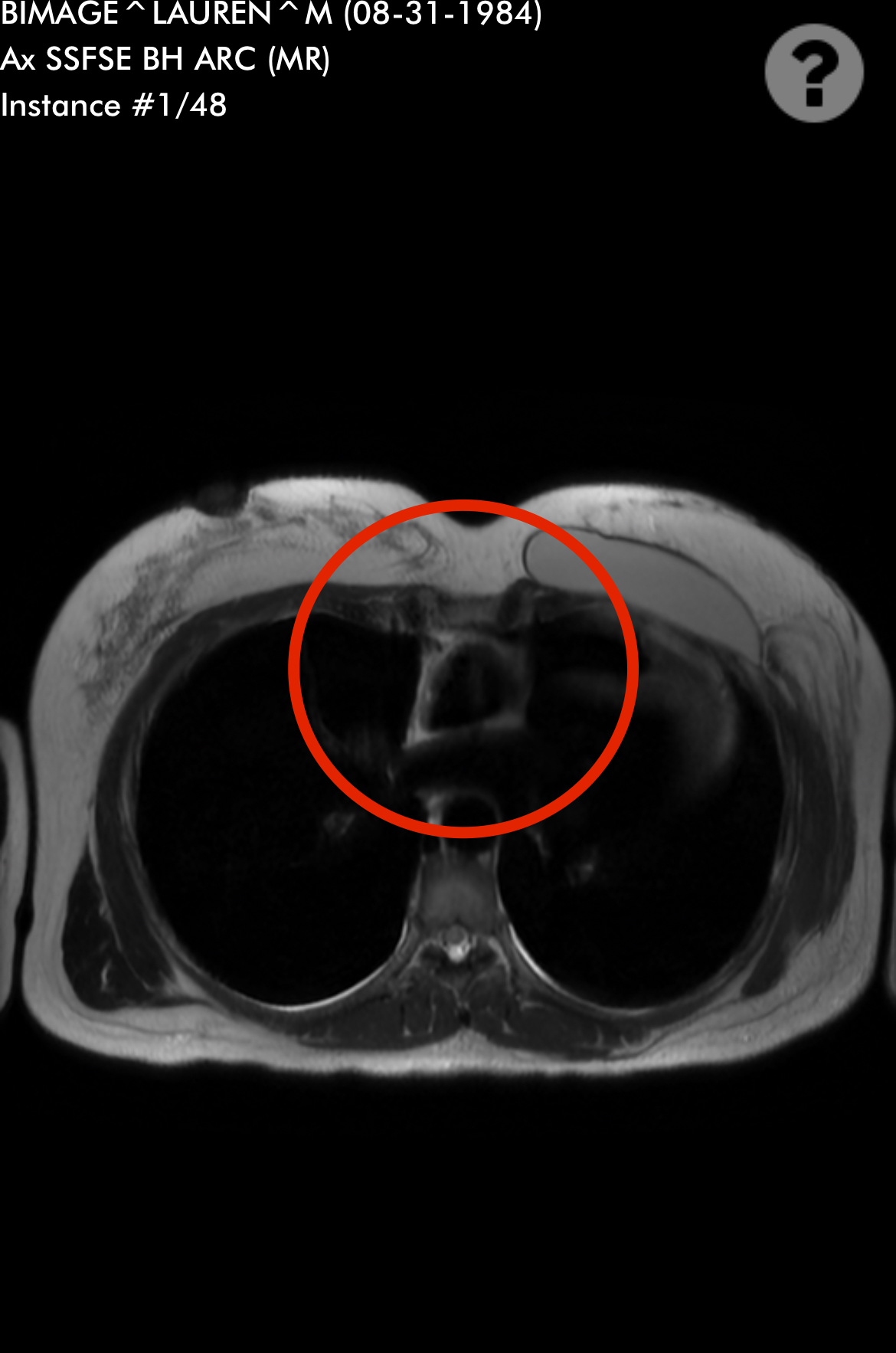
Sandy was diagnosed with stage 4 non-Hodgkin lymphoma in 2024. Her initial symptoms included persistent coughing, weakness, and shortness of breath. After weeks of worsening symptoms and ineffective treatments, an MRI revealed a large mass in her chest, which eventually led to the collapse of her left lung due to a massive tumor. A biopsy confirmed the diagnosis of lymphoma, a cancer that Sandy later described as a blessing in disguise due to its responsiveness to chemotherapy.
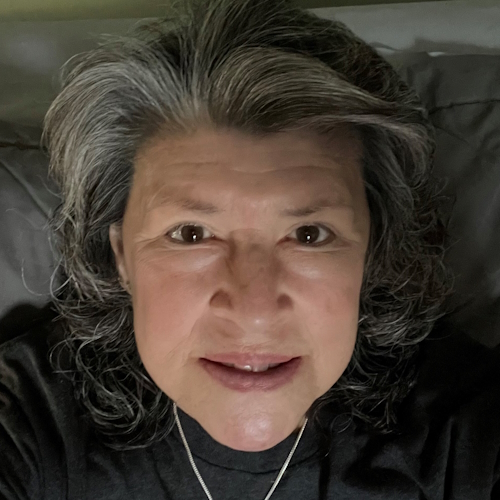
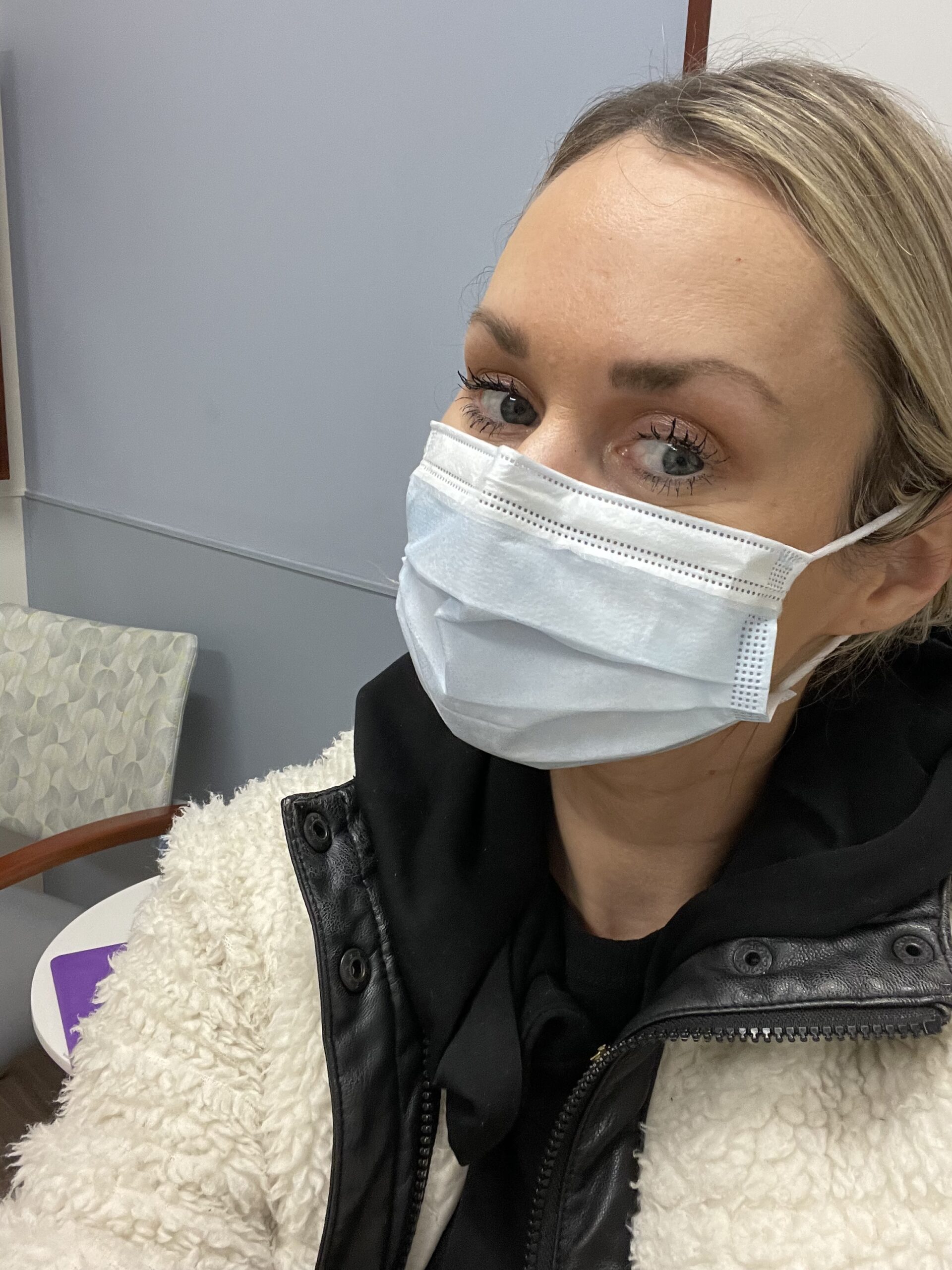
Interviewed by: Nikki Murphy
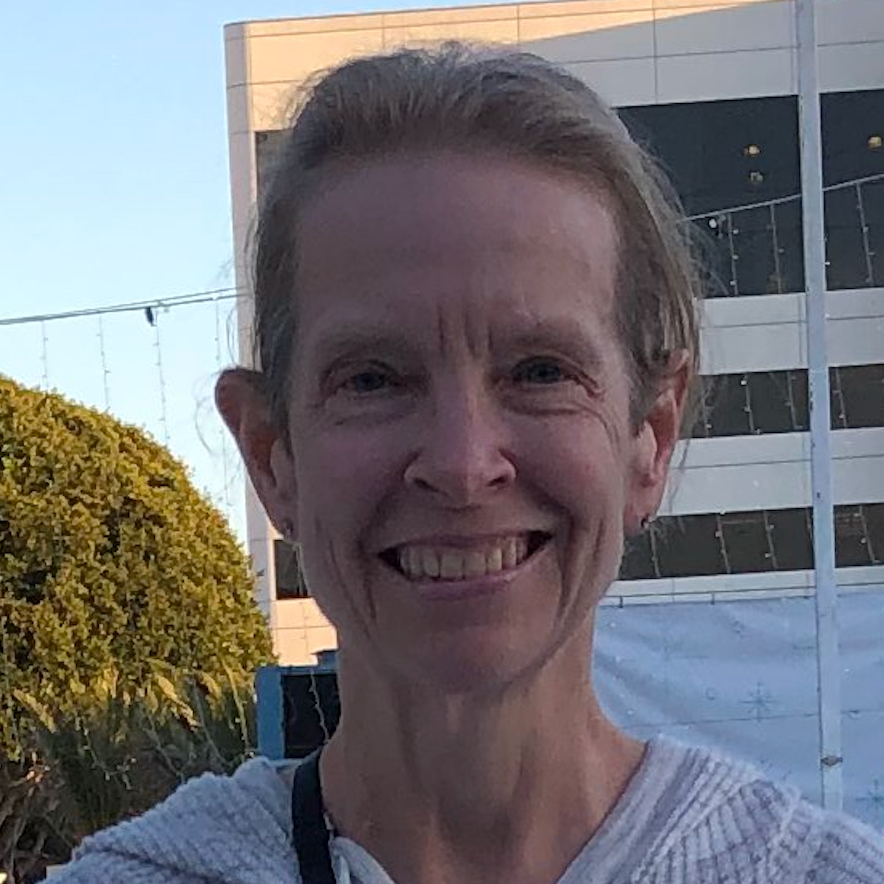
Edited by: Katrina Villareal
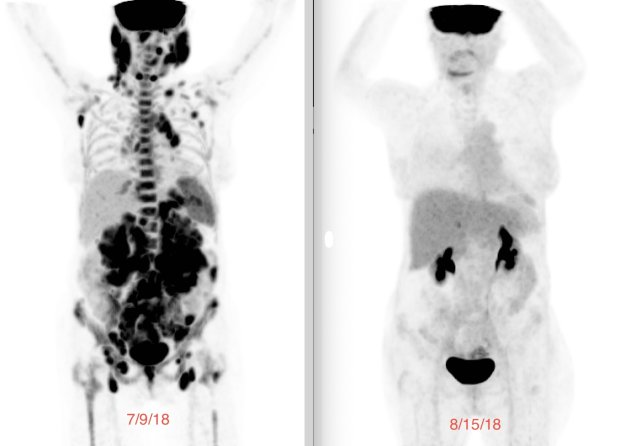
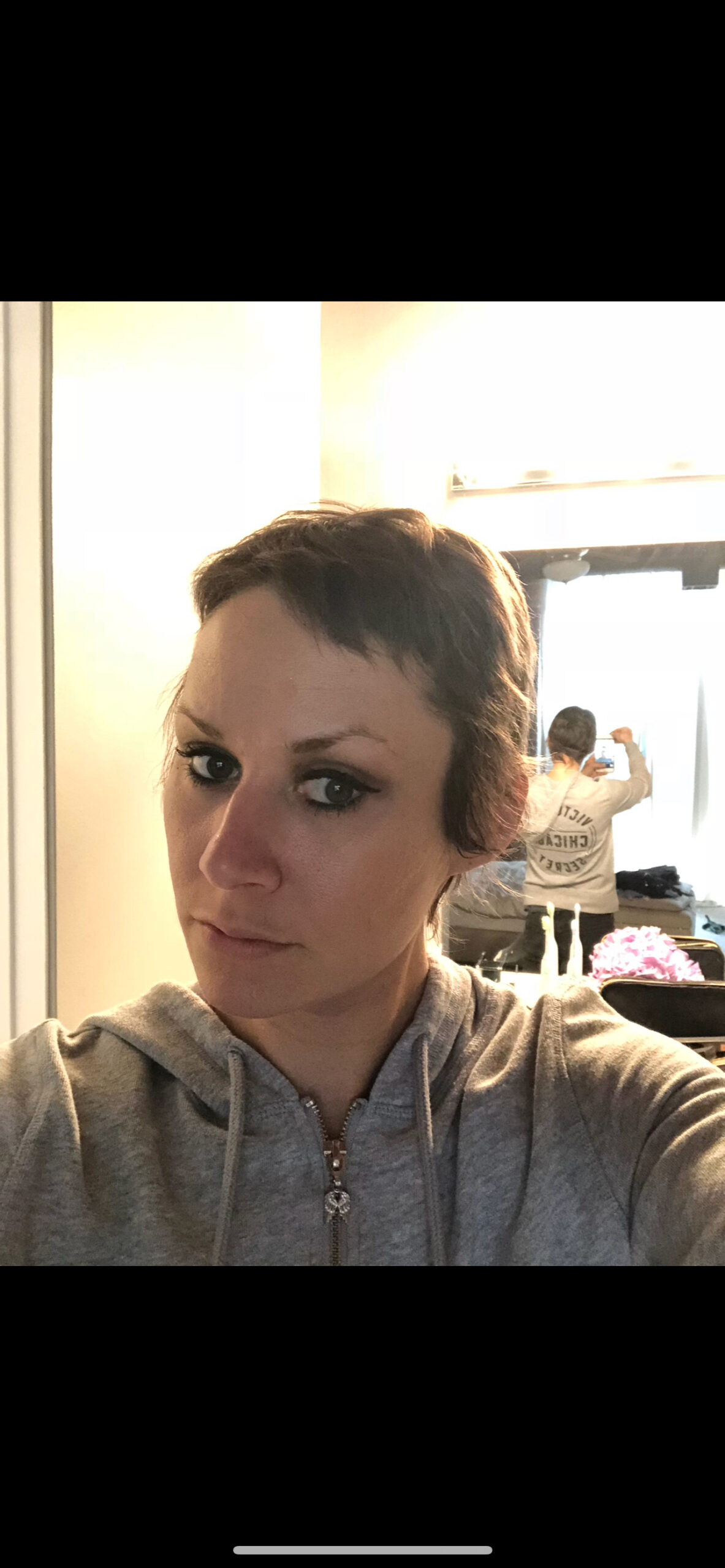
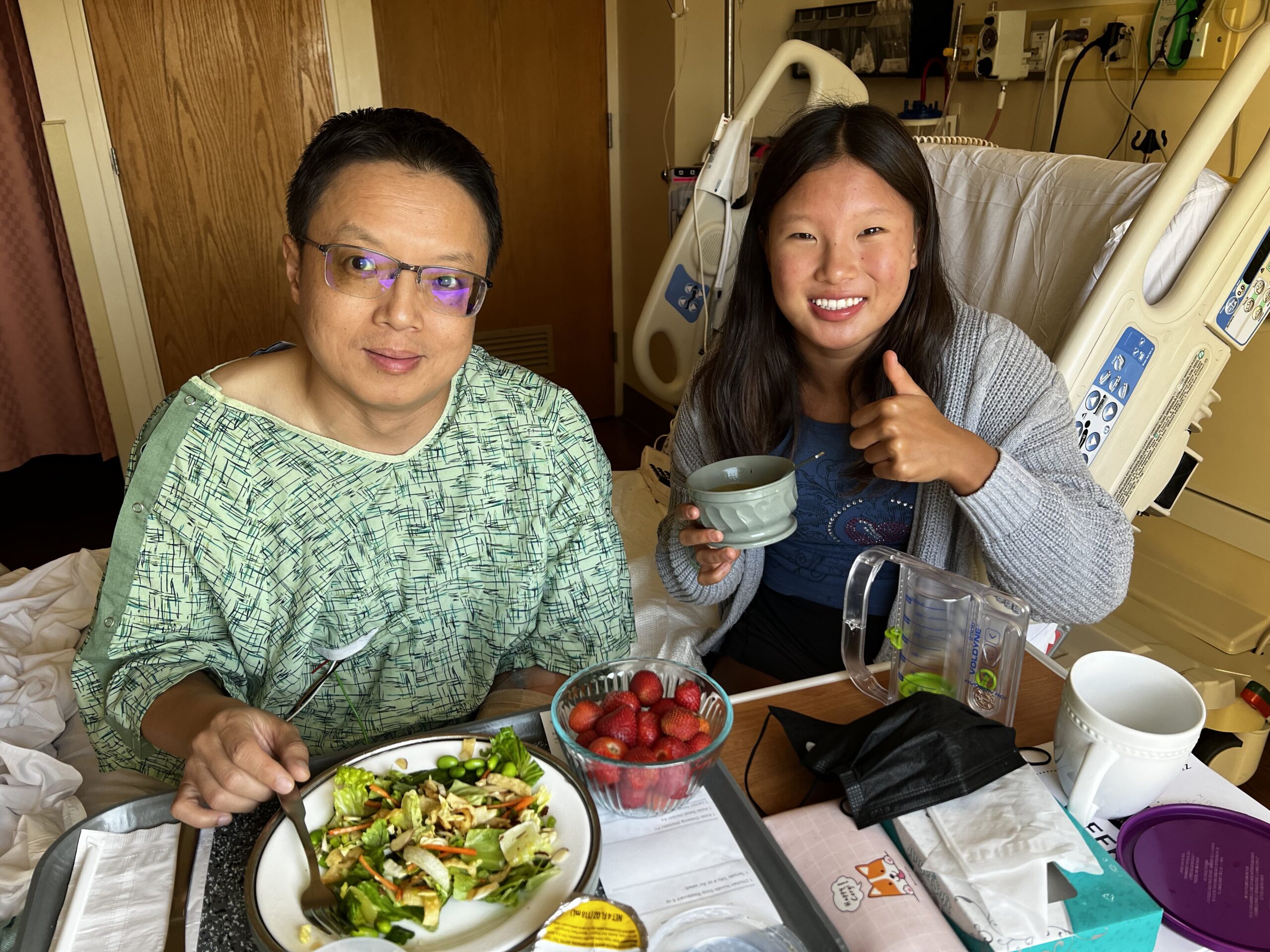
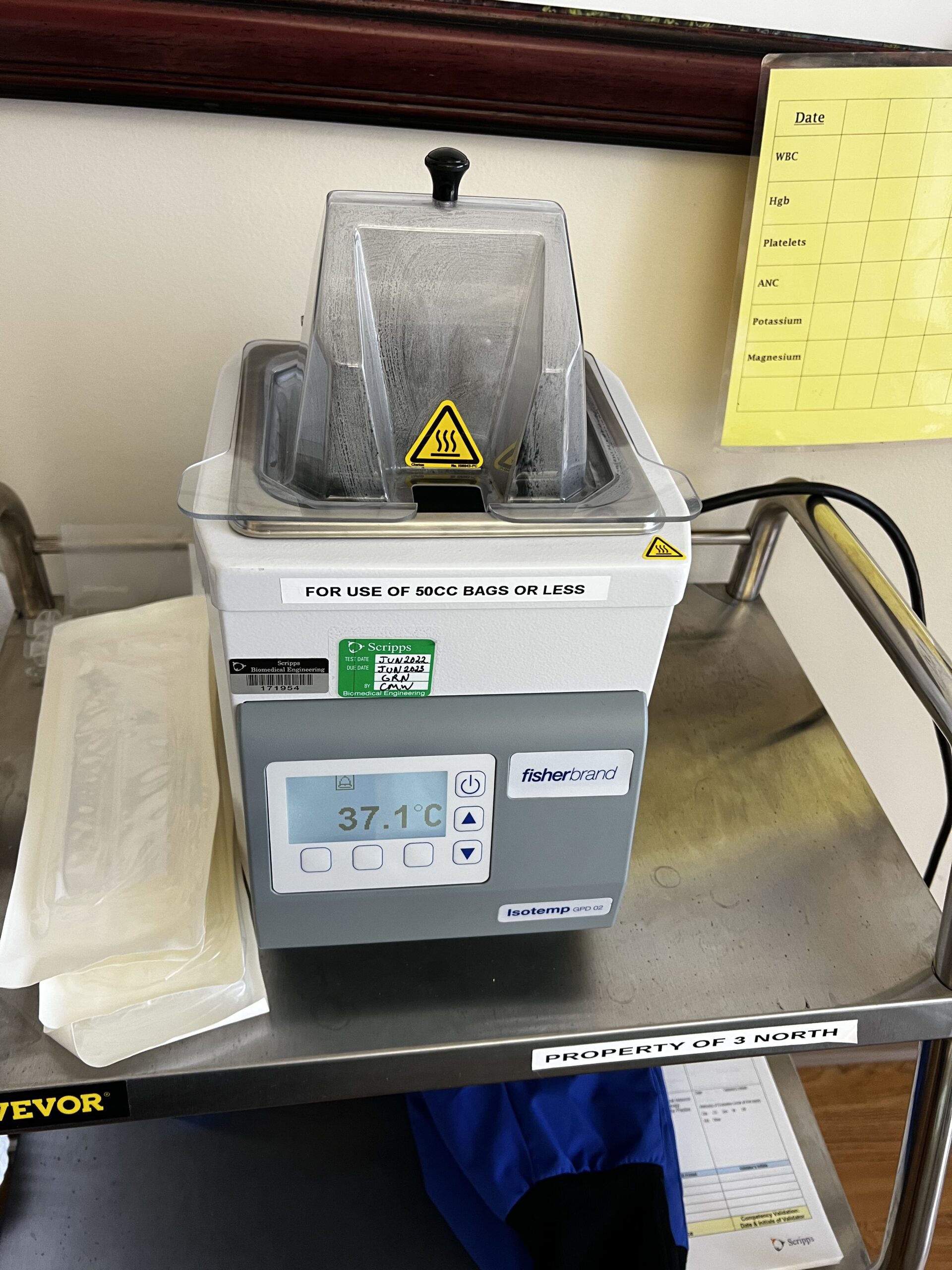
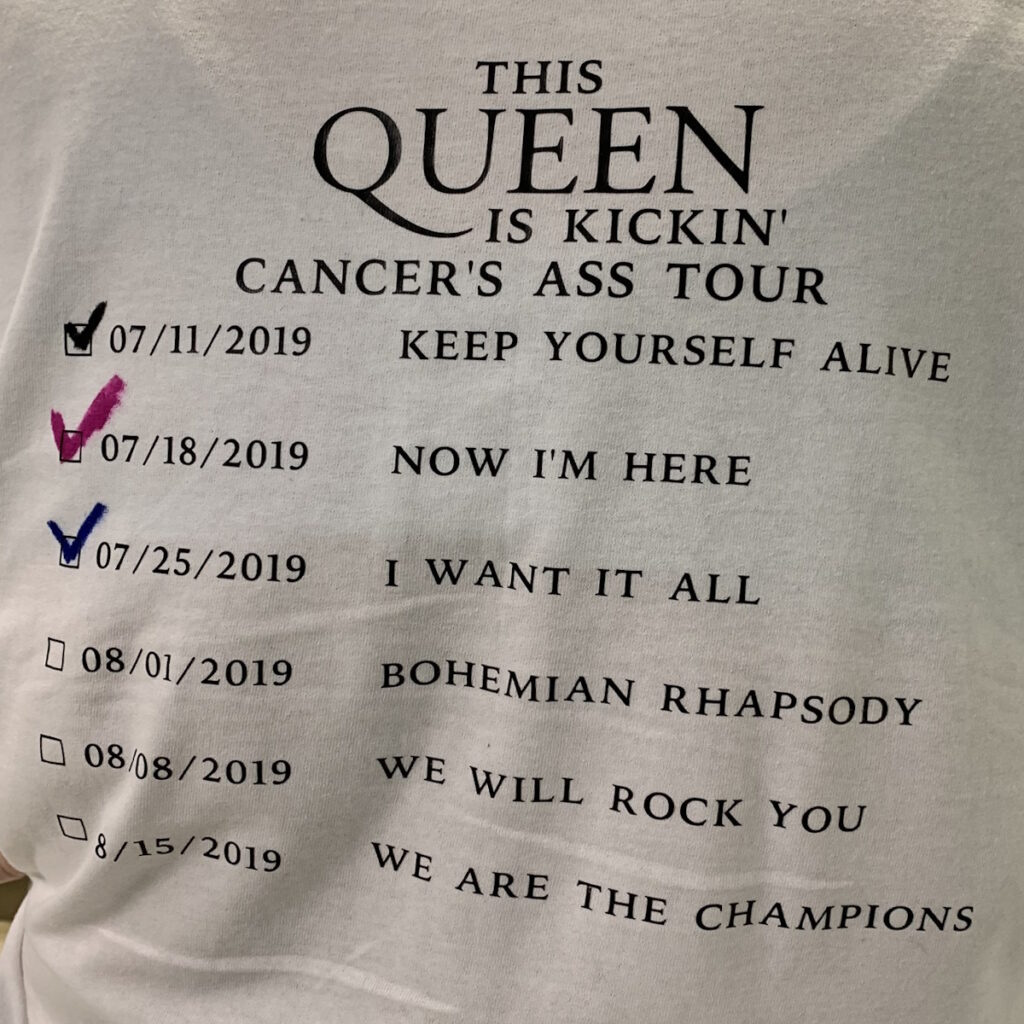
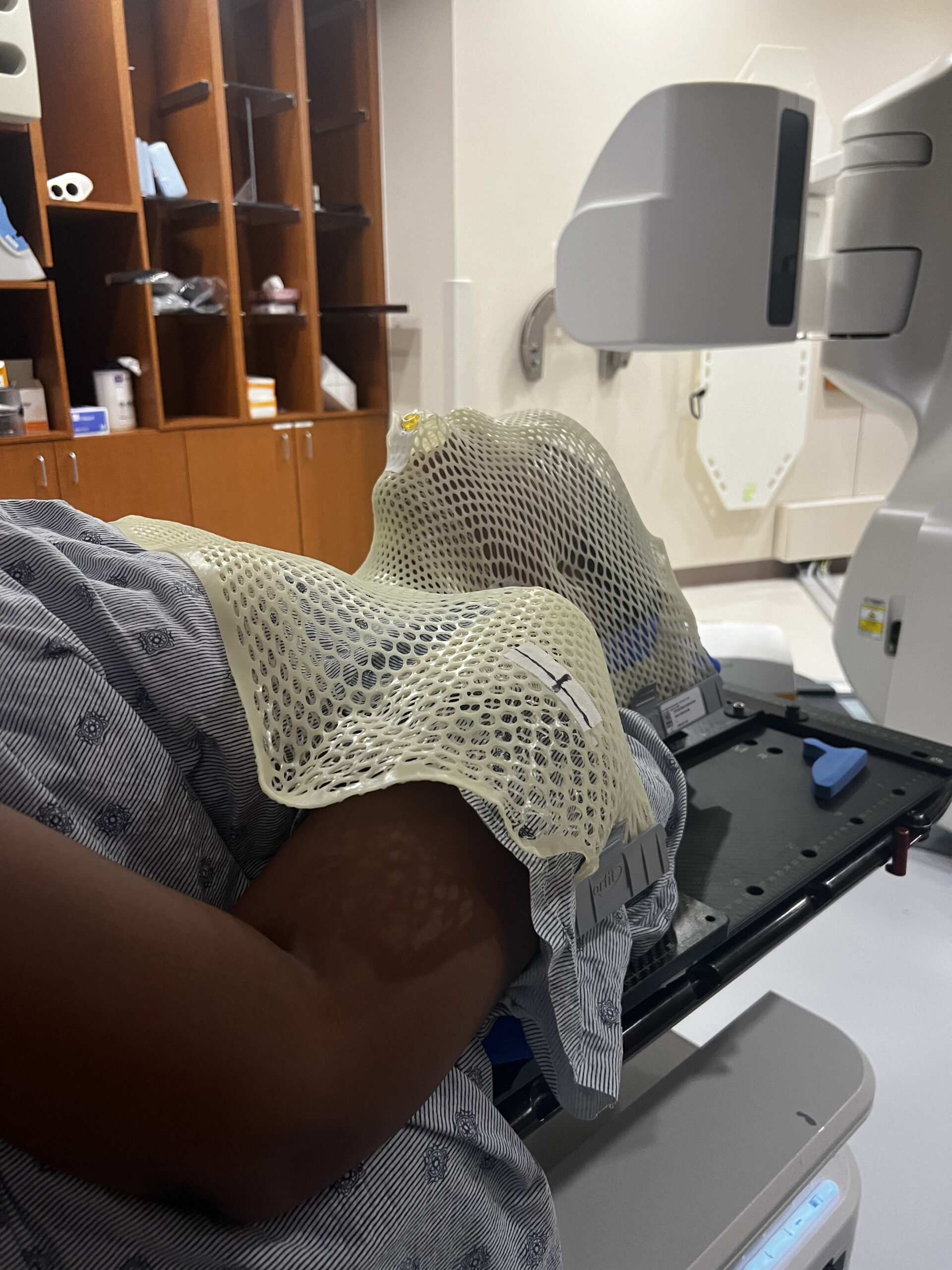
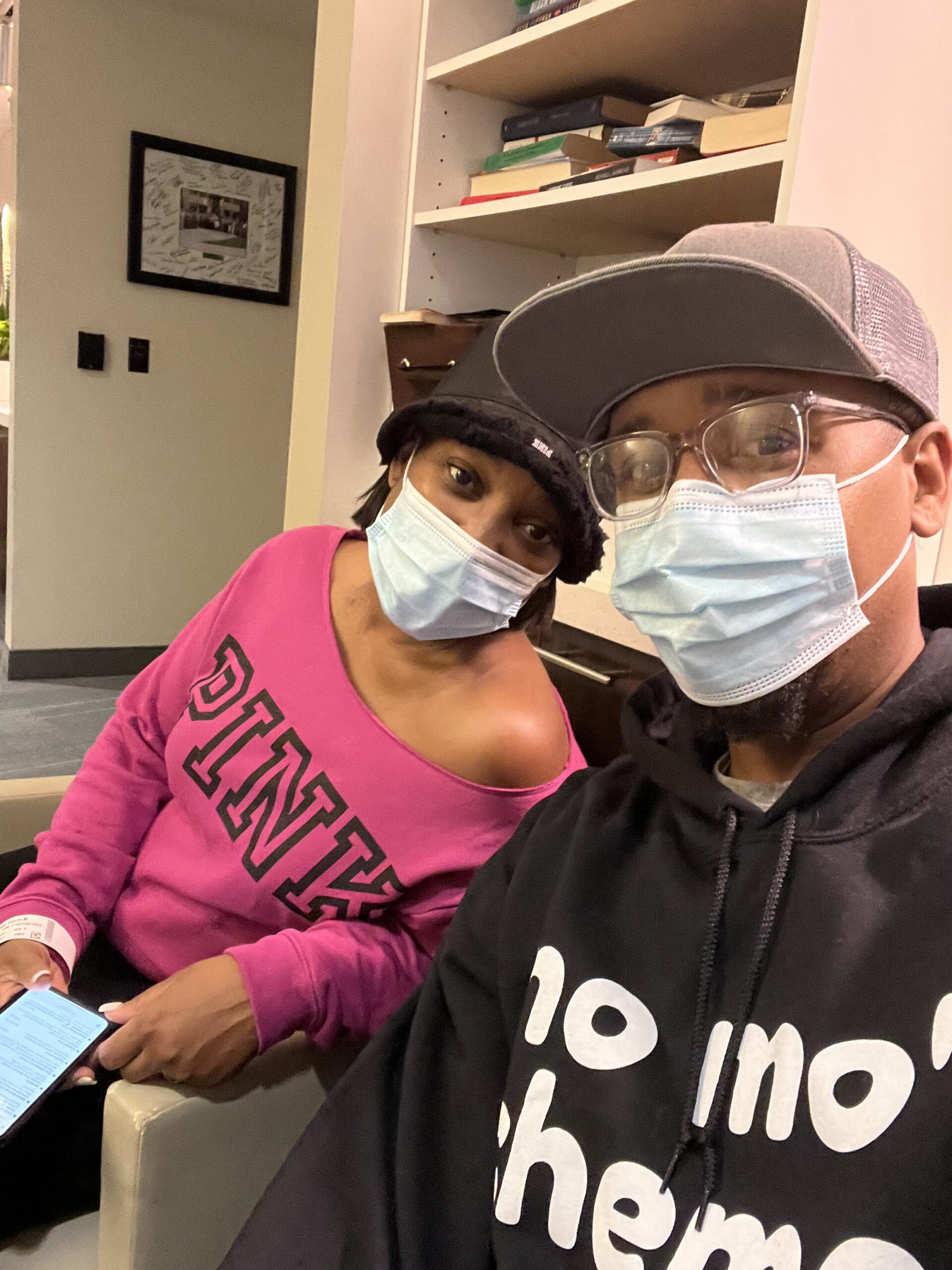
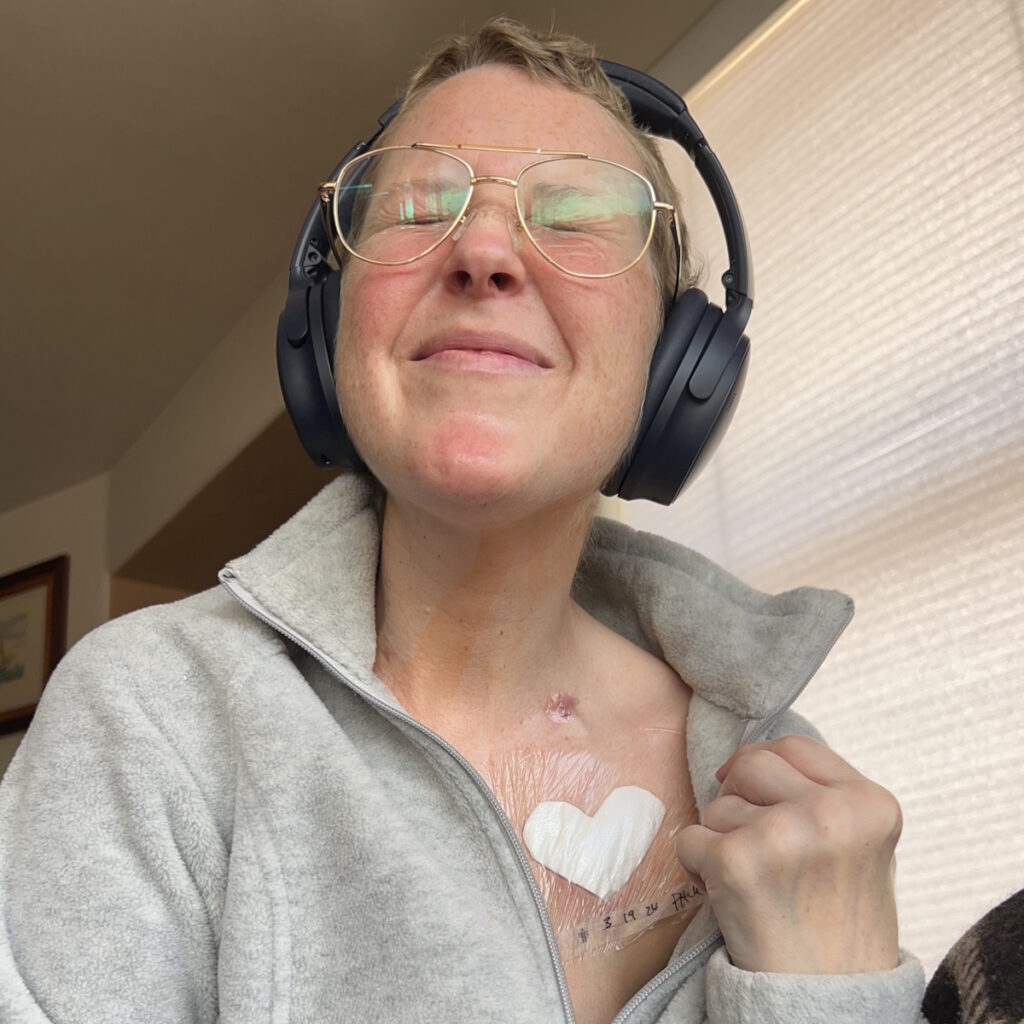
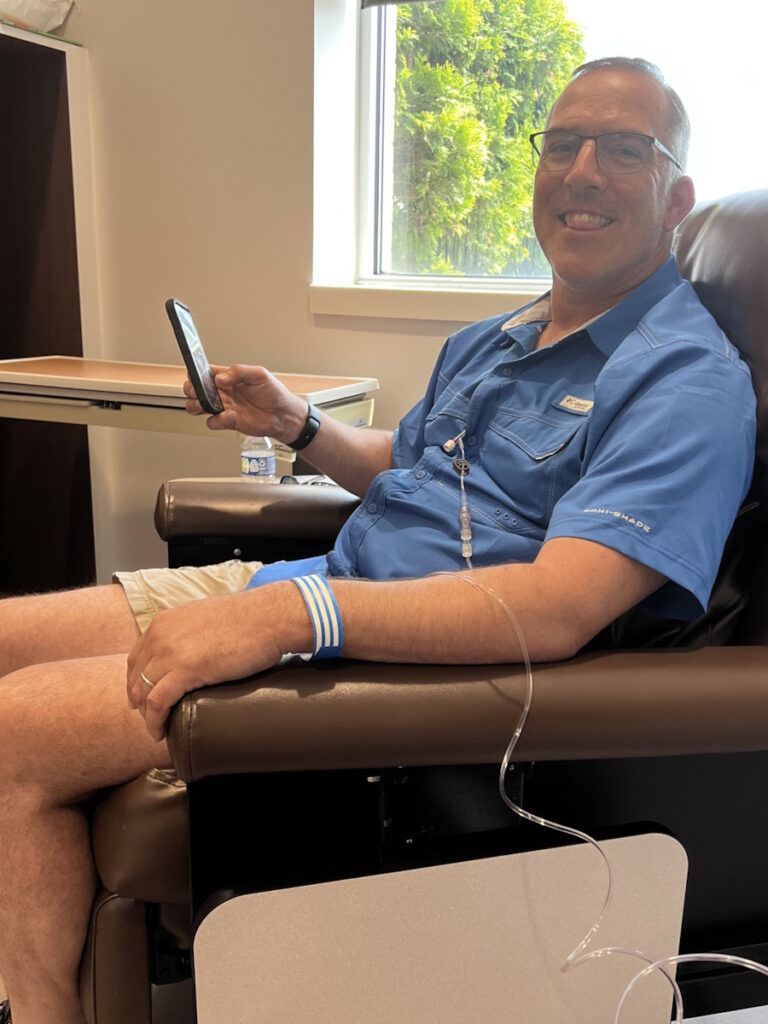
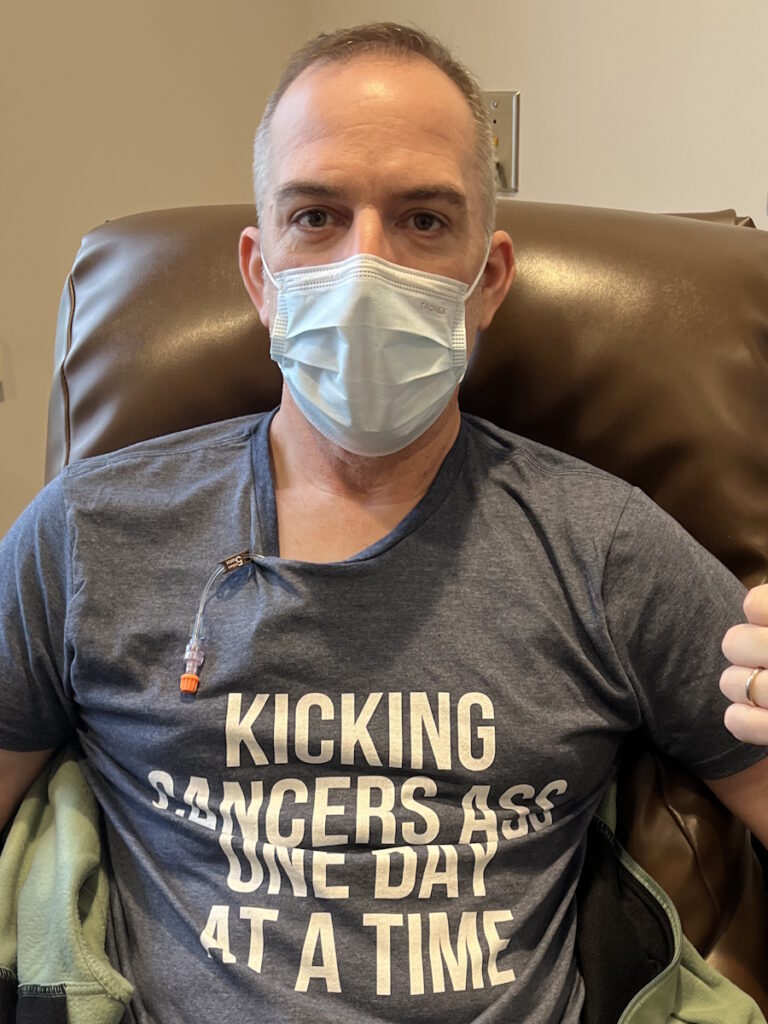
Treatment began immediately, consisting of six intense rounds of chemotherapy, each lasting five days in the hospital followed by two weeks of recovery at home. The process was physically and emotionally grueling, marked by extreme fatigue, weight loss, and hair loss. Despite these challenges, Sandy focused on mental resilience, which she believes was critical to her survival. She emphasized the importance of maintaining movement, even during the most debilitating moments.

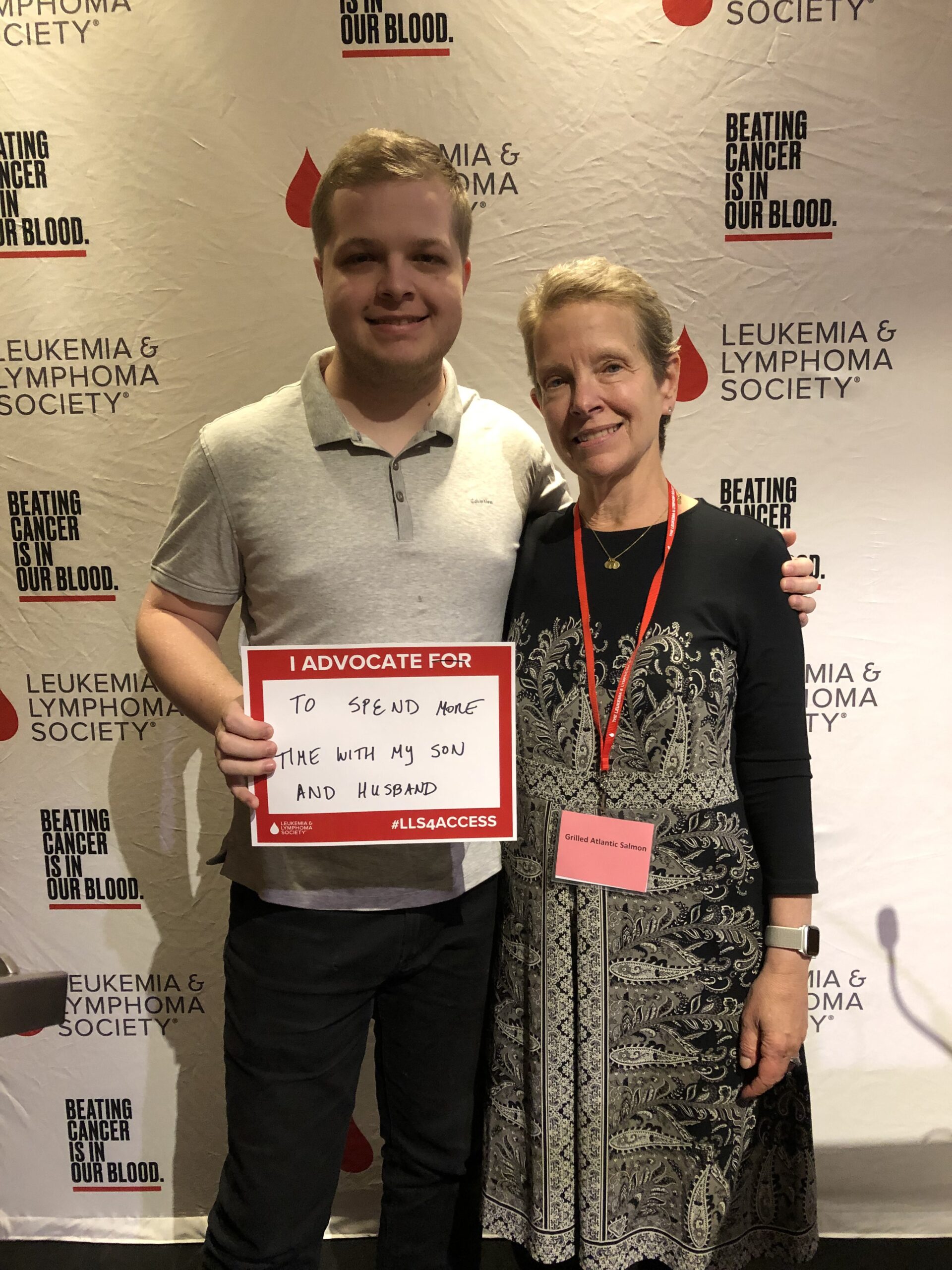
To cope mentally with stage 4 non-Hodgkin lymphoma, Sandy turned to spirituality, meditation, and writing. She frequented a meditation garden where she found solace. Writing became a therapeutic outlet, leading to the creation of her book, Cancer Ramblings. Writing helped her process her experience and turn her pain into purpose.
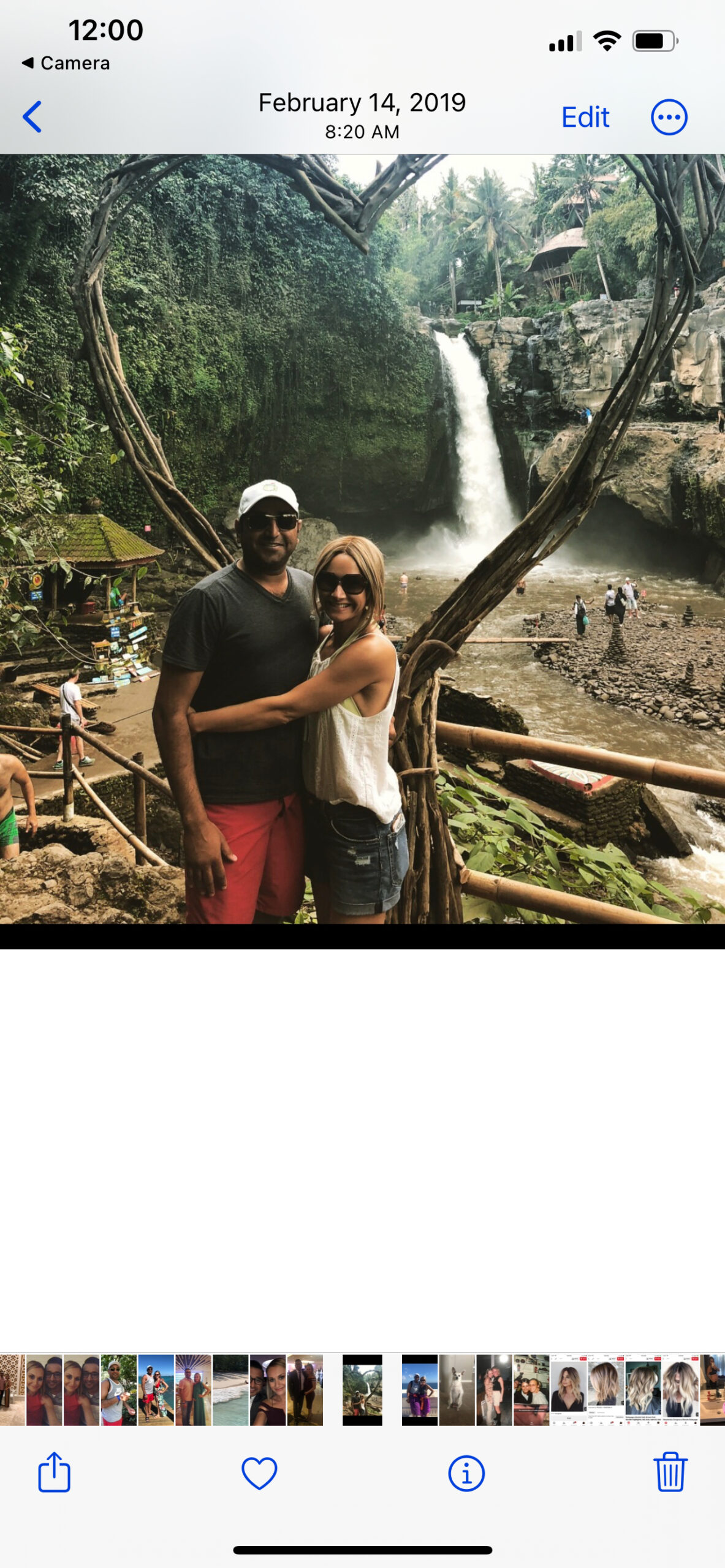
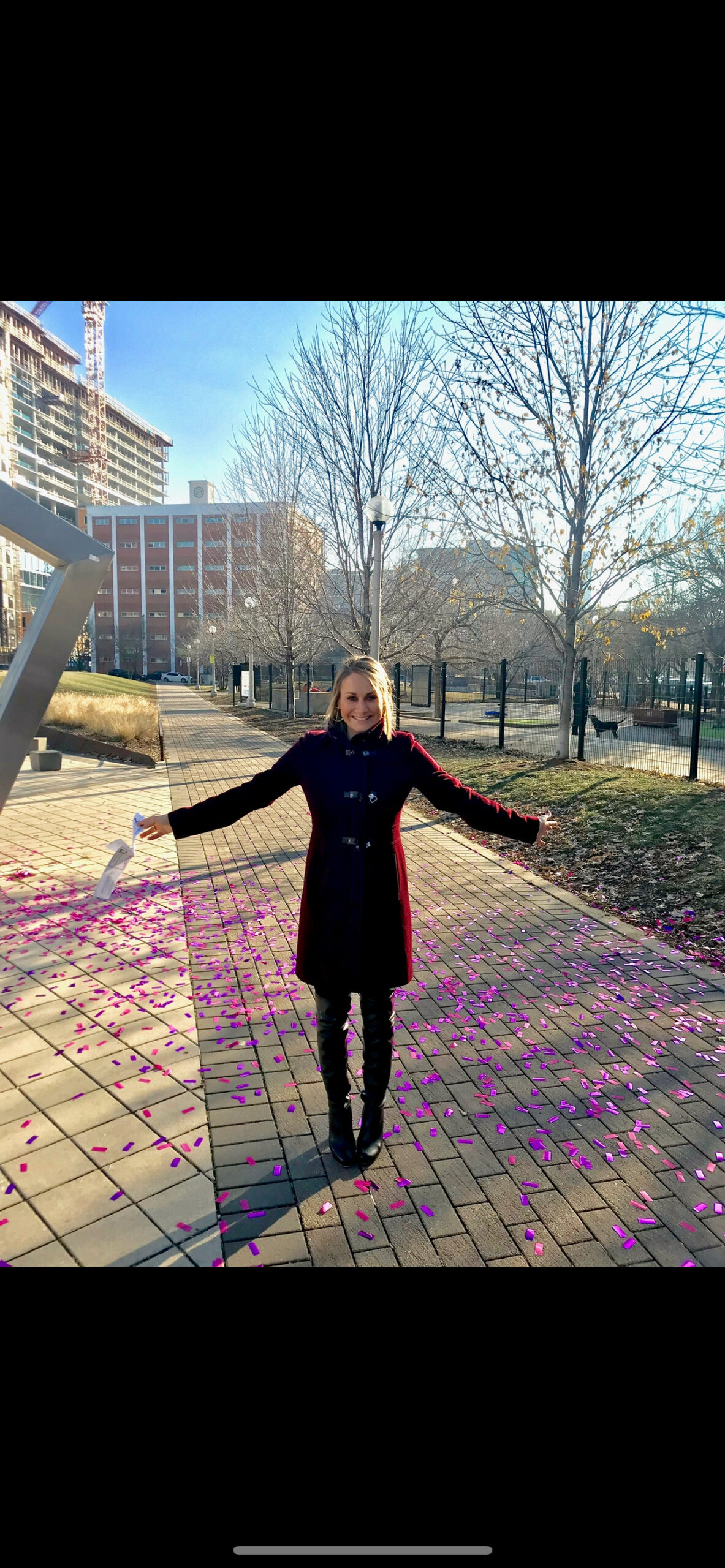
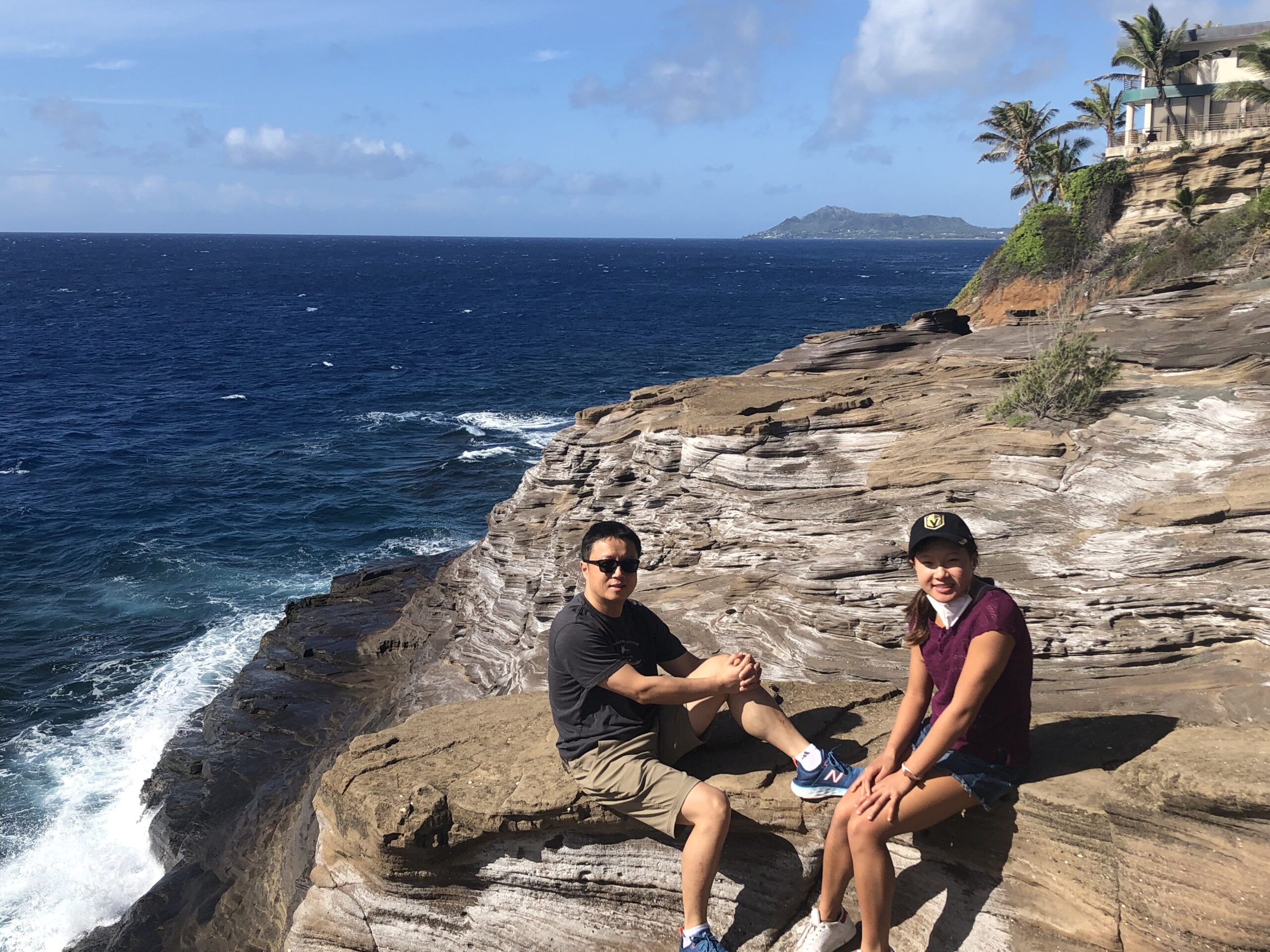
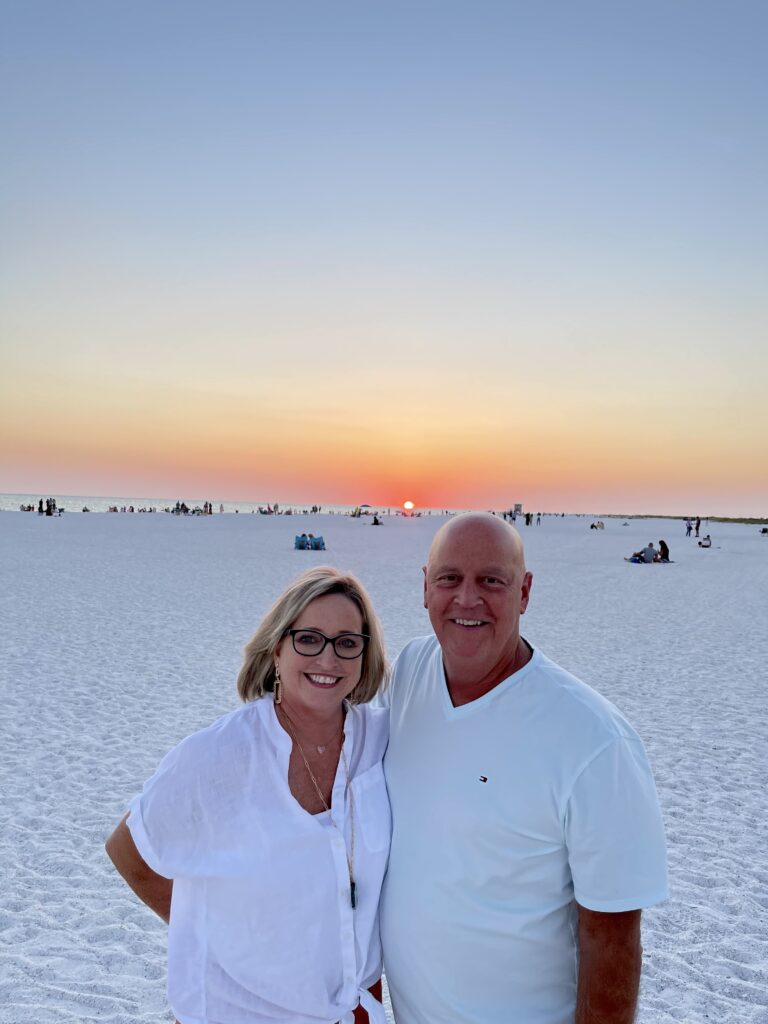
Sandy celebrated her remission as a profound moment of liberation and gratitude, describing it as a second chance at life. She plans to monitor her health closely while maintaining a conscious lifestyle. She views sharing her story as a way to inspire others, providing hope and comfort to those facing similar challenges. Her key advice is to visualize a positive outcome and hold onto it as a guiding light through the darkest moments. Sandy’s enduring image was of herself running on the beach—a vision she ultimately realized.
- Name: Sandy D.
- Age at Diagnosis:
- 45
- Diagnosis:
- Non-Hodgkin lymphoma
- Staging:
- Stage 4
- Symptoms:
- Persistent coughing
- Weakness
- Shortness of breath
- Treatment:
- Chemotherapy (six rounds)
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.

Inspired by Sandy's story?
Share your story, too!
More Metastatic Non-Hodgkin Lymphoma Stories
Aleeshia T., Burkitt Lymphoma, Stage 4B
Symptoms: Severe fatigue, deep shoulder pain, ear pain with inflammation, abdominal and pelvic pain, bloating, early fullness, nausea, difficulty eating, inability to urinate despite feeling an urgent need, internal bleeding, delayed period/bleeding, intense whole‑body pain leading to collapse
Treatments: Surgeries (emergency laparoscopic surgery with left ovary removal), chemotherapy (R‑CODOX‑M/IVAC), immunotherapy, hormonal therapy (to protect the remaining ovary)
...
Stephanie V., Primary Mediastinal (PMBCL), Stage 4
Symptoms: Asthma/allergy-like symptoms, lungs felt itchy, shortness of breath, persistent coughing
Treatments: Pigtail catheter for pleural drainage, video-assisted thoracoscopic surgery (VATS), R-EPOCH chemotherapy (6 cycles)
...
Stephanie R., Mantle Cell Lymphoma (MCL), Stage 4
Symptom: Elevated white blood cell count
Treatments: 6 months of rituximab + ibrutinib, 4 cycles of hyper-CVAD chemotherapy
...
Sheryl B., Mantle Cell Lymphoma (MCL), Stage 4
Symptoms: (Over 15 years) Skin irritation from temperature changes, rising WBC levels, unexplained fatigue, retinal hemorrhage, hardened abdomen (from enlarged spleen)
Treatment: 6 cycles Hyper-CVAD chemotherapy
...
Shari B., Mantle Cell Lymphoma (MCL), Stage 4
Symptom: None; lymphoma discovered at unrelated doctor appointment
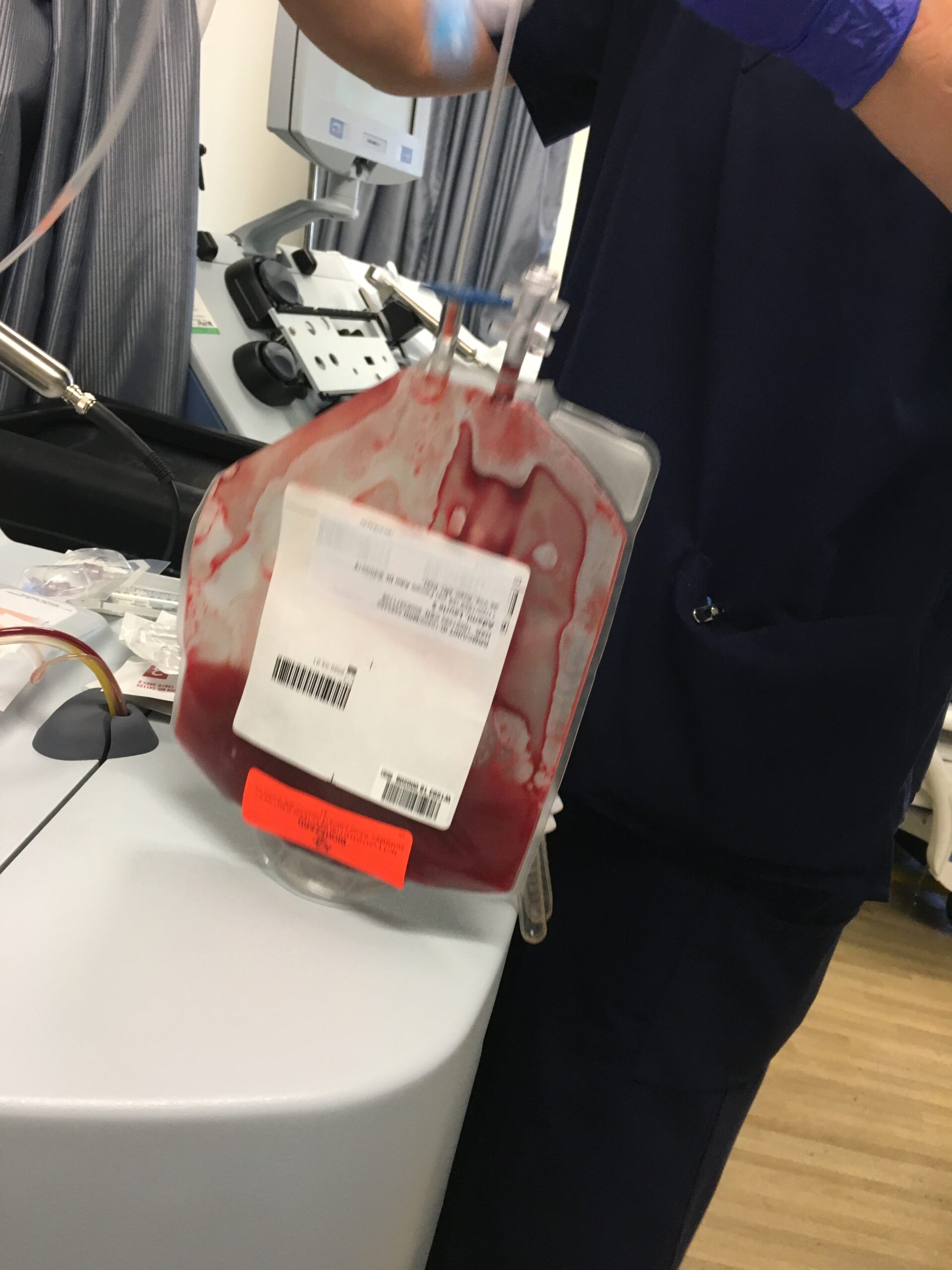
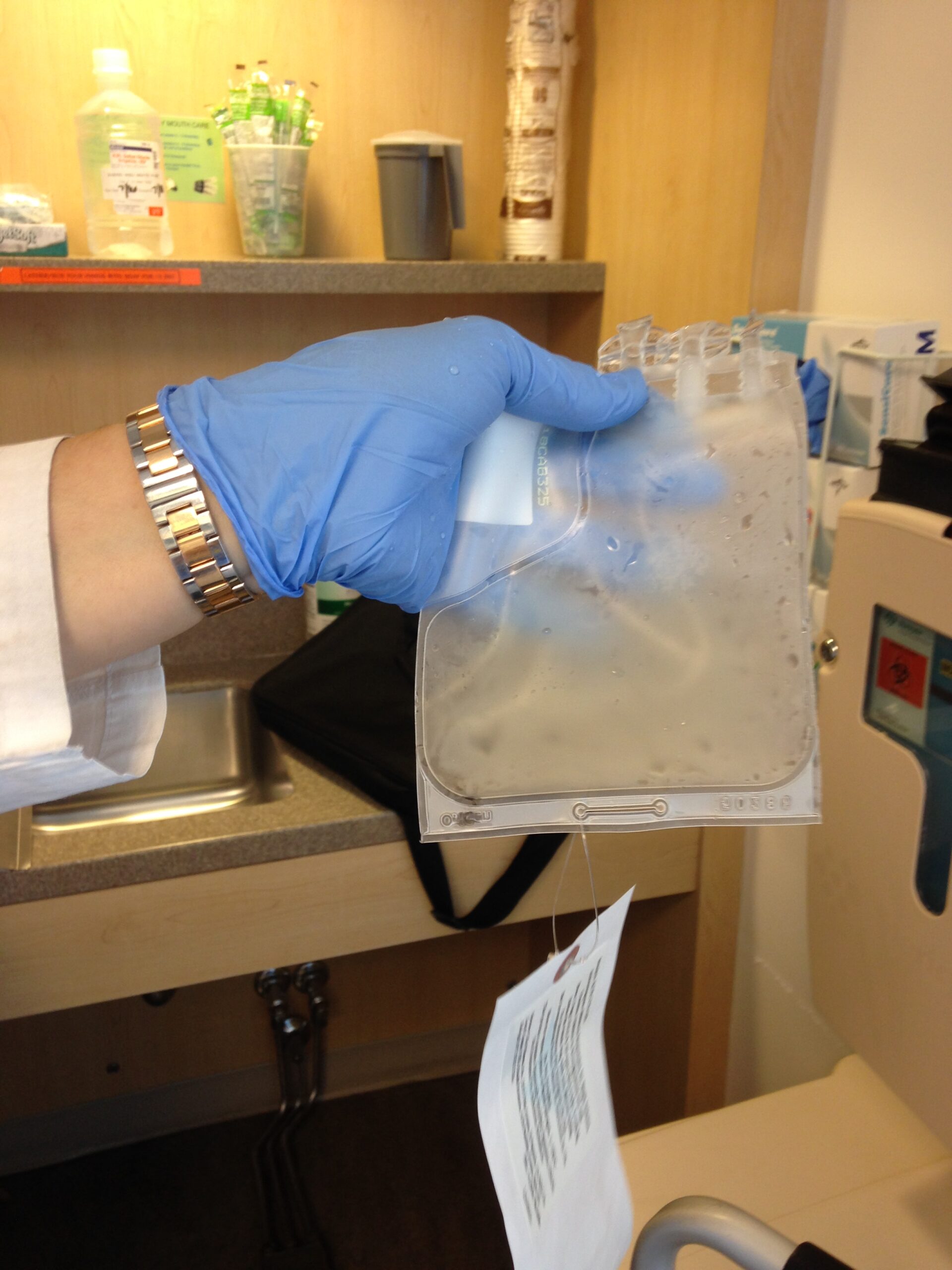
Treatments: 6 cycles R-CHOP, 5 cycles phase 3 trial of Velcade + Rituxan (normally for multiple myeloma), allogeneic bone marrow transplant (BMT)
...
Shahzad B., Refractory Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Extreme fatigue
Treatments: R&B, R-ICE, R-EPOCH, CAR T-cell therapy (cell-based gene therapy)
...
Sandy D., Non-Hodgkin’s Lymphoma, Stage 4
Symptoms: Persistent coughing, weakness, shortness of breath
Treatment: Chemotherapy
...
Symptoms: Chest pain, back pain, bump on neck, night sweats Treatments: Chemotherapy, CAR T-cell therapy...
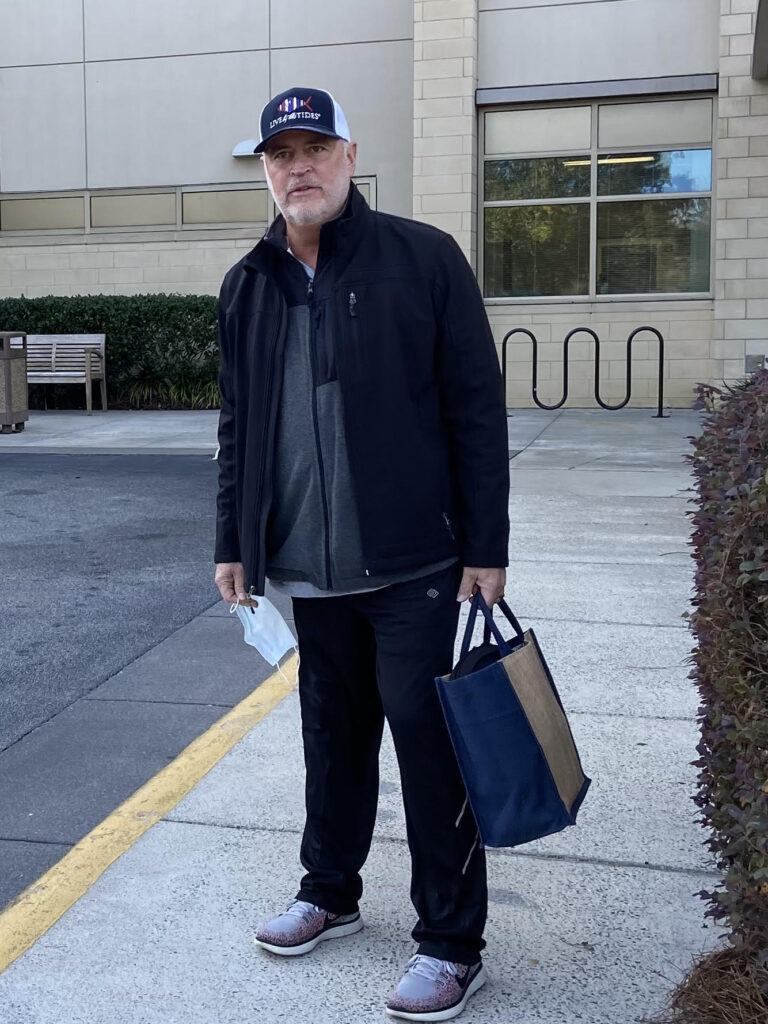
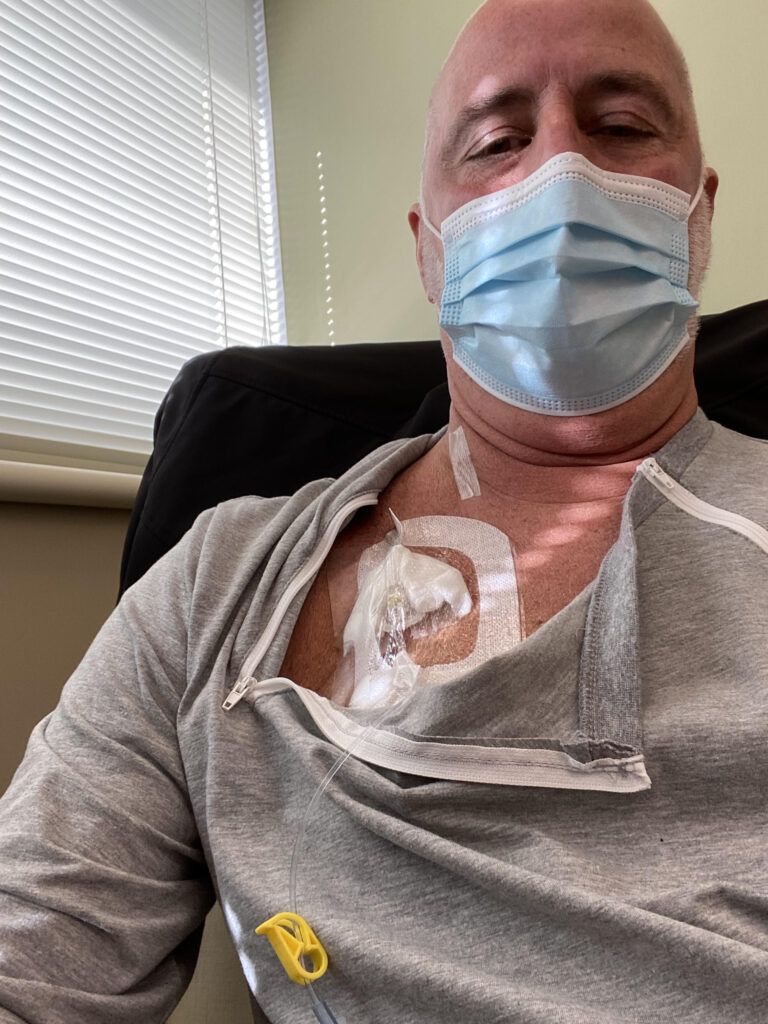
Richard P., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Relapse Symptoms: Swelling in leg, leg edema Treatments: R-CHOP chemotherapy, clinical trial (venetoclax-selinexor)
...
Paige C., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Weight loss, extreme fatigue, swollen lymph nodes in the neck
Treatment: R-EPOCH chemotherapy
...
Ashley P., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Feeling like holding breath when bending down or picking up objects from the floor, waking abruptly at night feeling “off,” one episode of fainting (syncope), presence of a large mass in the breast
Treatments: Chemotherapy, bridge therapy of chemotherapy and radiation, CAR T-cell therapy
...
Nolan W., T-Cell/Histiocyte-Rich Large B-Cell Lymphoma (T/HRBCL), Stage 4
Symptoms: Debilitating fatigue, flu-like symptoms without a fever, swollen lymph node under the left arm
Treatments: Chemotherapy (R-EPOCH & RICE), bone marrow transplant
...
Nina L., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Hip and lower extremities pain, night sweats
Treatment: Chemotherapy (R-CHOP)
...
Symptoms: Fatigue, weight loss, lumps in the neck and groin
Treatments: Chemotherapy, radiation, platelet transfusion...
Mike E., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Persistent, significant back pain
Treatments: Surgery, chemotherapy
...
Mags B., Primary Mediastinal (PMBCL), Stage 4
Symptoms: Exhaustion, migraines, persistent coughs, swelling and discoloration in left arm
Treatment: Chemotherapy (R-CHOP, 6 cycles)
...
Luis V., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Persistent cough, fatigue, unexplained weight loss
Treatment: Chemotherapy (R-CHOP and methotrexate)
...
Laurie A., Follicular Lymphoma, Stage 4 (Metastatic)
Symptoms: Frequent sinus infections, dry right eye, fatigue, lump in abdomen
Treatments: Chemotherapy, targeted therapy, radioimmunotherapy
...
Kris W., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Pain in the side of the abdomen
Treatment: R-CHOP chemotherapy
...
Kim S., Follicular Lymphoma, Stage 4 (Metastatic)
Symptom: Stomach pain
Treatments: Chemotherapy (rituximab & bendamustine), immunotherapy (rituximab for 2 additional years)
...
Jonathan S., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Severe shoulder pain
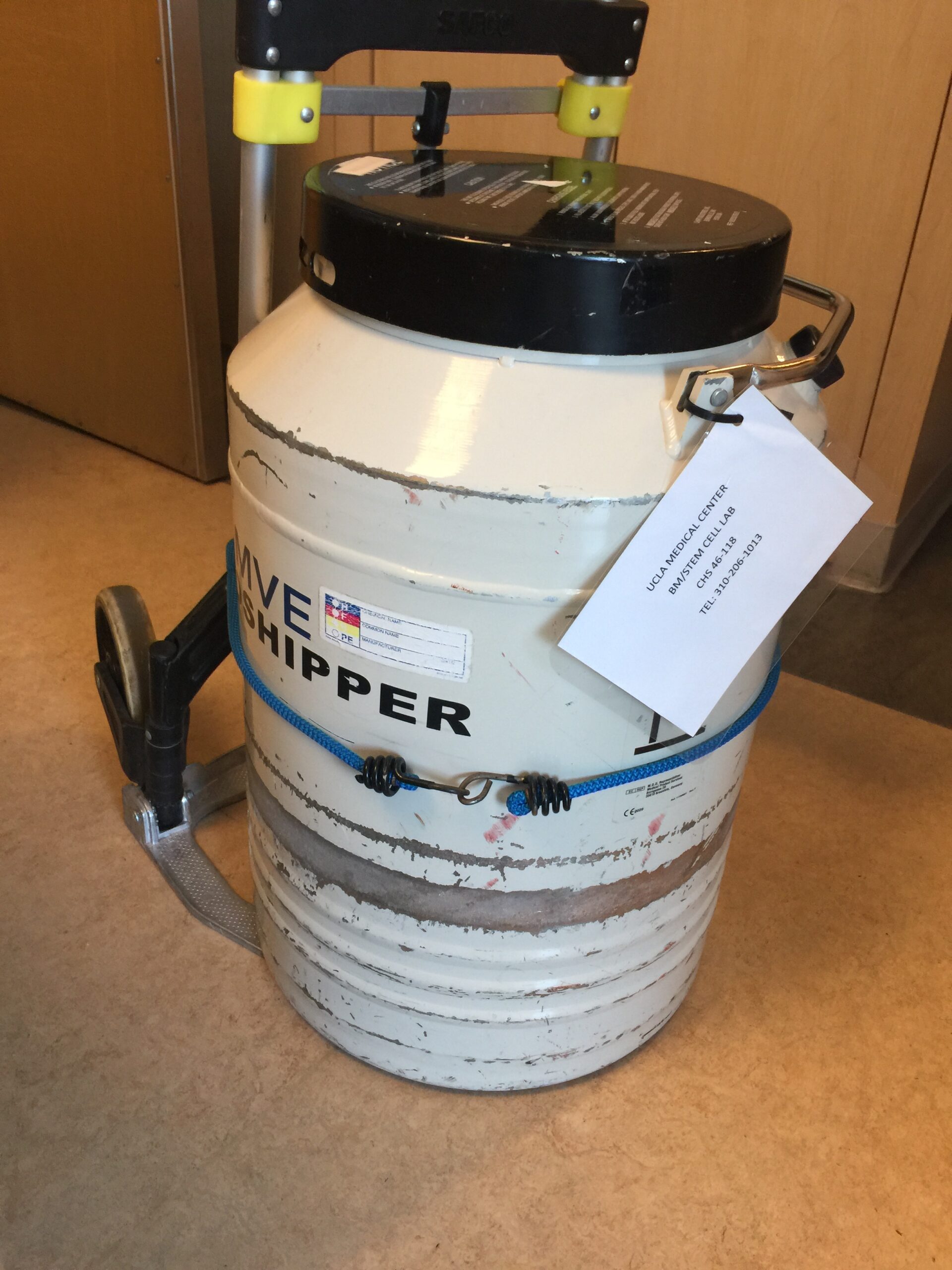
Treatments: R-CHOP chemotherapy, methotrexate, focal radiation, autologous stem cell transplant
...
John S., Follicular Lymphoma, Stage 4 (Metastatic)
Symptom: Swollen lymph nodes
Treatments: Clinical trial, chemotherapy
...
Jason W., Mantle Cell Lymphoma (MCL), Stage 4
Symptoms: Hives, inflamed arms
Treatments: Calabrutinib, Lenalidomide, Rituxan
...
Harjeet K., Subcutaneous Panniculitis-like T-Cell-Lymphoma (SPTCL), Stage 4
Symptoms: Persistent, high fevers; red, tender rashes on legs
Treatments: High-dose chemotherapy, allogeneic stem cell transplant
...
Anna M., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: a rRapidly growing, painless lump on the breast
Treatment: Chemotherapy
...
Erin R., Diffuse Large B-Cell Lymphoma (DLBCL) & Burkitt Lymphoma, Stage 4
Symptoms: Lower abdominal pain, blood in stool, loss of appetite
Treatments: Chemotherapy (Part A: R-CHOP, HCVAD, Part B: Methotrexate, Rituxan, Cytarabine)
...
Emily G., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Pain in left knee
Treatments: Chemotherapy (R-CHOP and high-dose methotrexate)
...
Emily S., Burkitt Lymphoma, Stage 4
Symptoms: Constant fatigue, tongue deviated to the left, abscess in right breast, petechiae on legs, night sweats, nausea and vomiting, persistent cough
Treatments: Chemotherapy, stem cell transplant, immunotherapy
...
Cindy M., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Itchy skin on the palms and soles of feet; yellow skin and eyes
Treatment: Chemotherapy (R-CHOP)
...
Cherylinn N., Mantle Cell Lymphoma (MCL), Stage 4
Symptom: None
Treatments: R-CHOP chemotherapy, rituximab
...
Bobby J., Mantle Cell Lymphoma (MCL), Stage 4
Symptoms: Fatigue, enlarged lymph nodes
Treatments: Clinical trial of ibrutinib + rituximab, consolidated chemo of 4 cycles of Hyper-CVAD
...
Barbara R., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Abdominal and gastric pain
Treatments: Chemotherapy R-CHOP, CAR T-cell therapy, study drug CYT-0851
...
Ashlee K., Burkitt Lymphoma, Stage 4
Symptoms: Abdominal pain, night sweats, visible mass in the abdomen
Treatments: Surgery (partial colectomy to remove 14 inches of intestine), chemotherapy
...