Hasegawa Kazuo Turned His Stage 4 Lung Cancer Diagnosis Into a Mission to Help Others
It started with a cough that just wouldn’t go away. How can you tell if the symptoms are the common cold or something worse? (like stage 4 lung cancer) This was Kazuo Hasegawa’s concern after he continued to cough for weeks. But everything changed when he started to cough up blood.
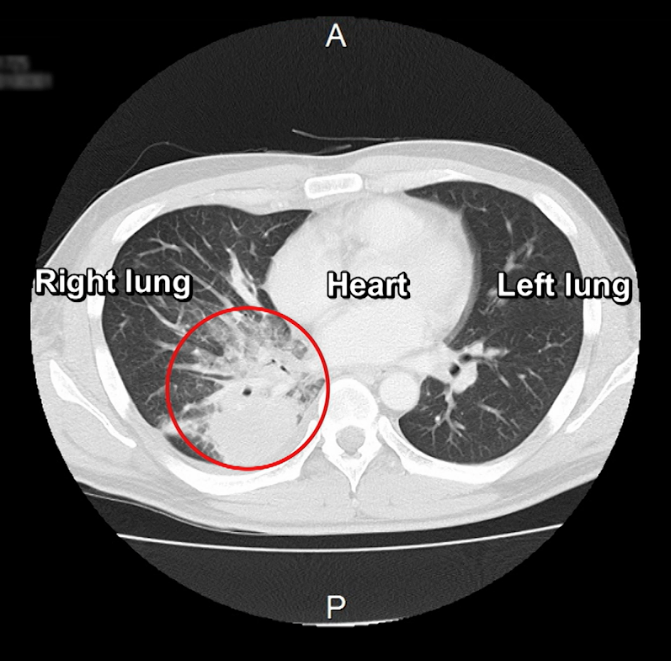
Kazuo ended up in the emergency room where doctors eventually ordered imaging. A scan revealed a shadow on his lungs. Reality became clear to him even though the doctor hesitated to say anything about cancer. The diagnosis would be stage 4 lung cancer.
Interviewed by: Stephanie Chuang
Edited by: Chris Sanchez & Jeff Forslund
Editor’s Note: This interview was conducted in Japanese. It has been translated for clarity into English.

His mind went first to his young children who were just five and seven years old at the time. He struggled to tell them exactly what he was dealing with, so he told them he was “sick.” At the same time, the father of two was also having a hard time figuring out how to navigate the healthcare system in his home country of Japan. He says many people there follow what doctors say, but he decided to advocate for himself, getting multiple “second” opinions.
Now he’s galvanized a group of thousands of other Japanese people who are dealing with cancer by creating the first patient advocacy group of its kind there called “One Step.” Dive into Kazuo’s incredible story of self-advocacy and empowerment, and how he’s trying to help strangers navigate a healthcare system to get the best outcomes for themselves and their loved ones.
Watch Hasegawa Kazuo’s video and read his story to take a deeper dive into:
- A terrible cough led to a diagnosis of advanced lung cancer
- The initial prognosis was ten months to live
- Faced with uncertainty, he became an advocate for patient access to information
- Kazuo founded One Step to support other patients
- He now lives with intention, knowing each day is irreplaceable
- Name:
- Hasegawa Kazuo
- Diagnosis:
- Lung Cancer (Pulmonary Adenocarcinoma)
- Staging:
- Stage 4
- Symptoms:
- Persistent cough that lasted two months
- Coughed up blood on one occasion
- Worsening headache
- Treatments:
- Chemotherapy
- Clinical trial

Thank you to Johnson & Johnson for supporting our patient education program. The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I’ve come to really feel the importance of time. Everyone only has one life.
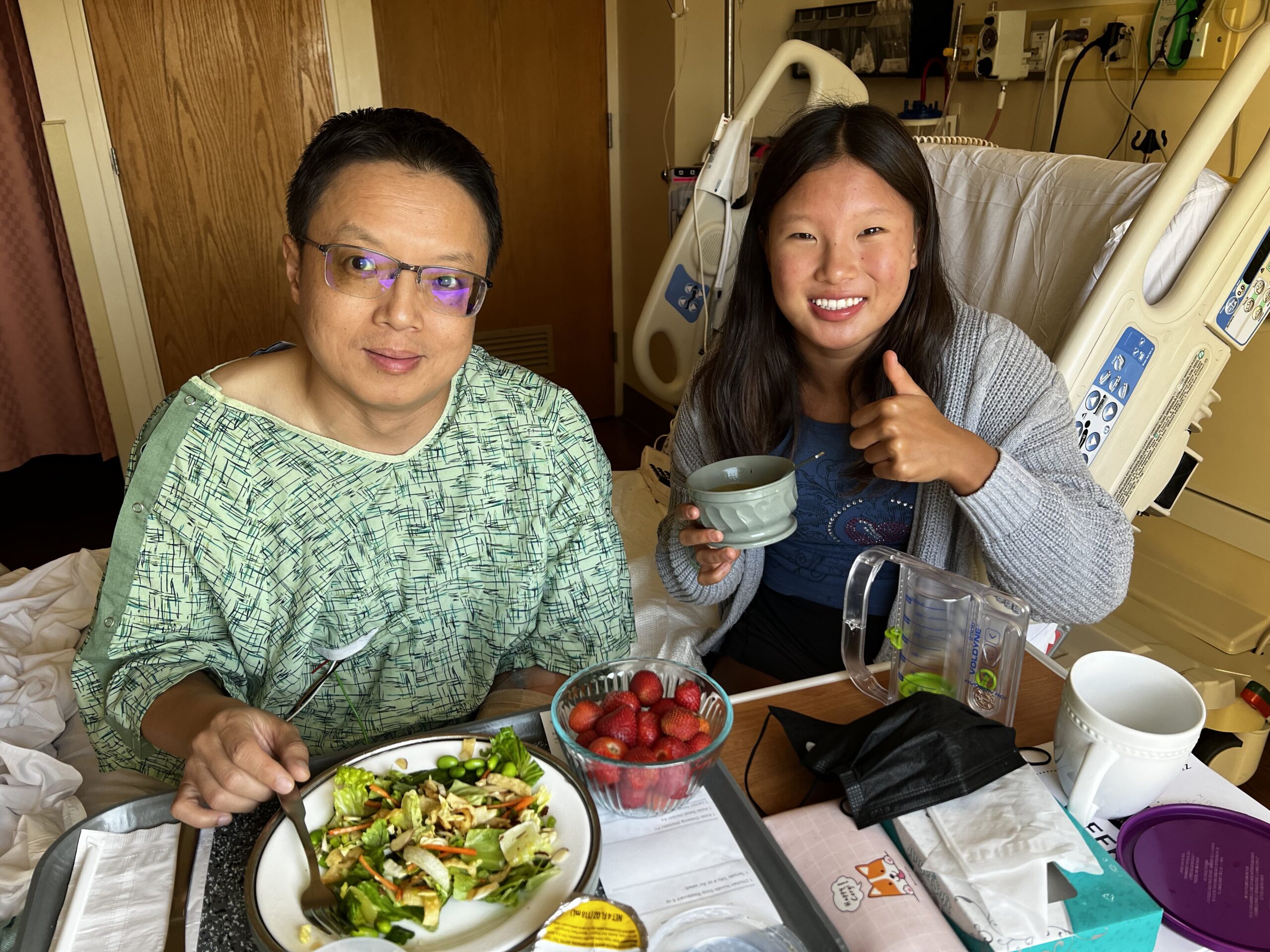
About Me
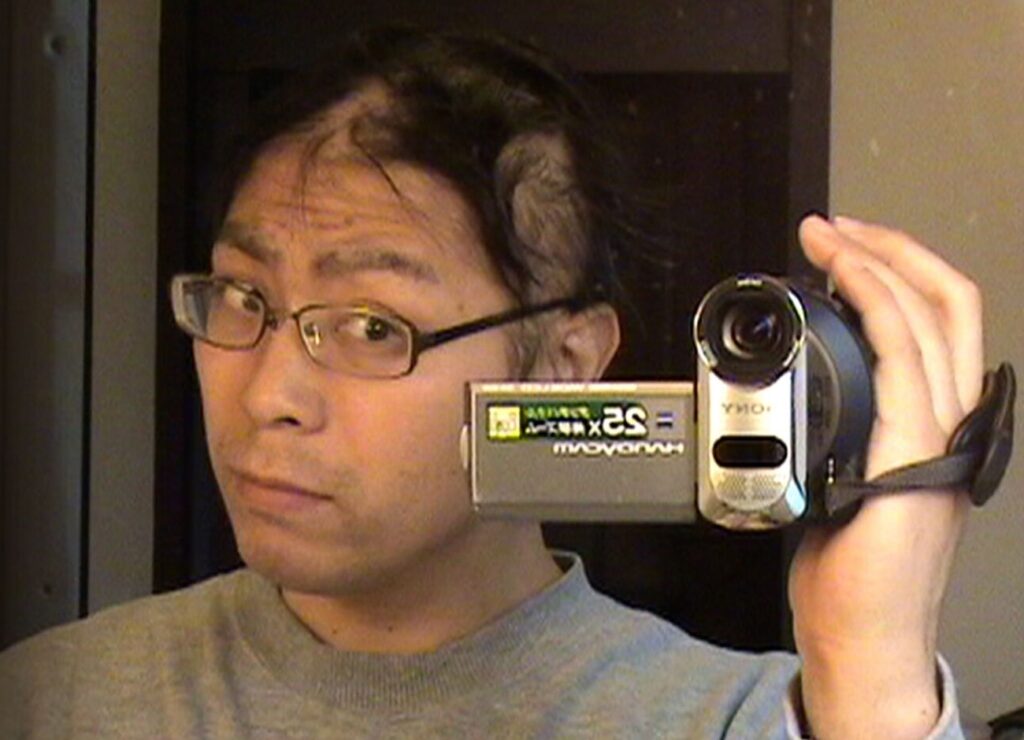
My name is Hasegawa Kazuo. I’m a father of two. I used to work as a TV director in Japan.
I was diagnosed with stage 4 lung cancer (pulmonary adenocarcinoma) in 2010. And since, I’ve come to really feel the importance of time. Everyone only has one life.


The Cough That Changed Everything
It all started back in 2010, with a terrible cough. At first, I thought it was nothing, just a cold. I ended up having that cough for two months.
One night, it got so bad that I had to be taken to the hospital. There, I coughed up blood.
I had a terrible headache when the symptoms first appeared. It just kept getting worse. I remember thinking, “Something strange is happening.”
How I Found Out I Had Stage 4 Lung Cancer
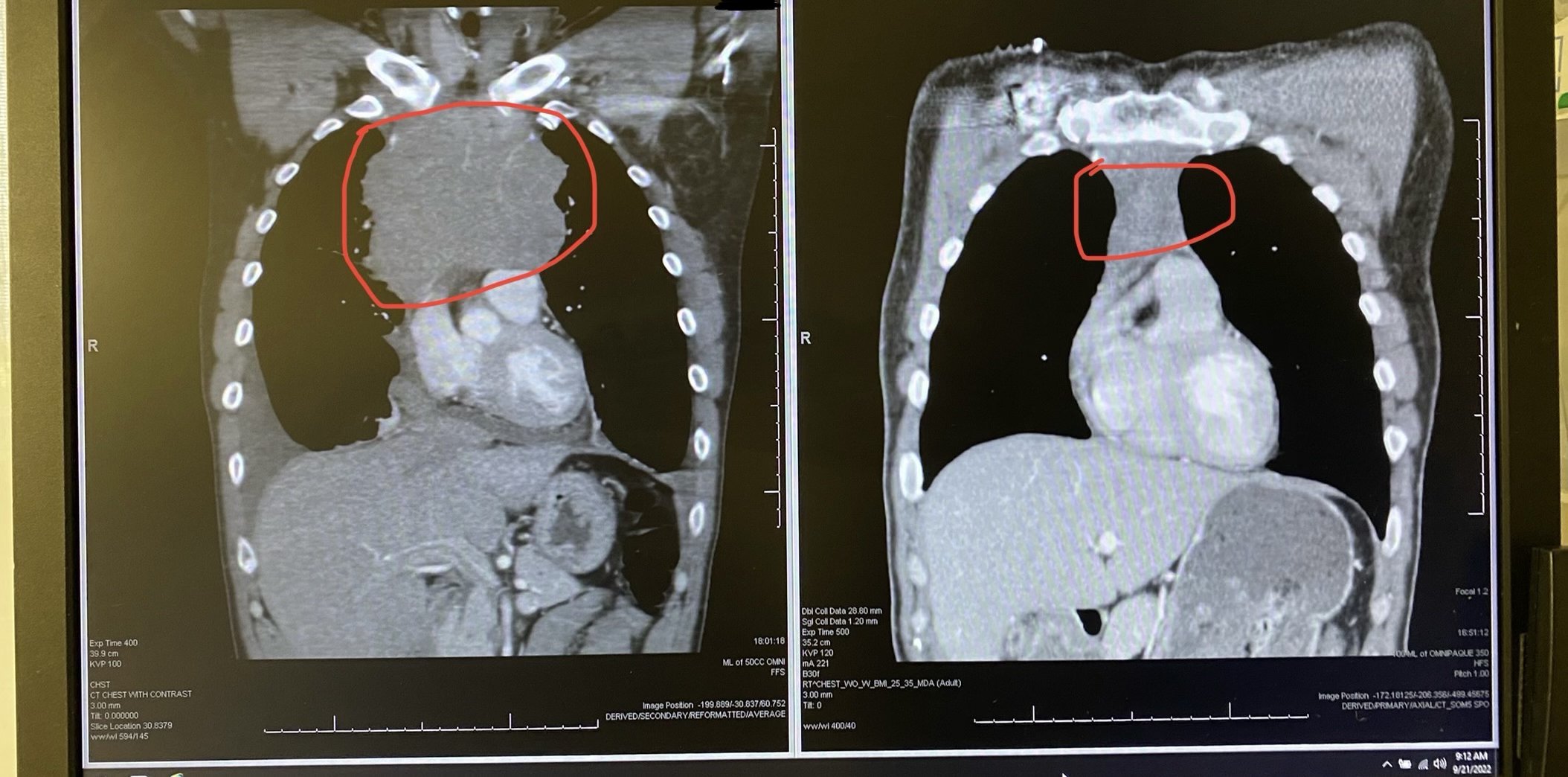
In the examination room, I had a CT scan. It found a big shadow on my lungs.
The doctor was very silent about it, however, and seemed hesitant to tell me if I had pneumonia or something like that. He looked uncomfortable, like he wasn’t sure how to tell me. I kept wondering why he wouldn’t just say what he saw. A simple explanation like, “There might be something suspicious. We should do more tests,” would have helped. But he stayed quiet, and that left me to fill in the blanks myself.
My wife was with me when I found out. Our children were seven and five years old at the time. We struggled with how to tell them. In the end, I didn’t use the word “cancer.” I just said I had a serious illness, but that I was going to try my best to get better. And they supported me, even at that young age.
But even though the word “cancer” scared me, it was better than not knowing at all.

How I Reacted to My Diagnosis
Strangely, once I finally had a name for what was happening to my body, I felt some relief. When I was in the hospital, before I knew it was cancer, I couldn’t look anything up. The fear of the unknown overwhelmed me.
But even though the word “cancer” scared me, it was better than not knowing at all. I still think those few days of not knowing were worse than the diagnosis itself.
I Got Ten Different Second Opinions
A normal hospital visit takes just five to ten minutes. I’ve been told that the median survival time is 12 months, and the doctor told me that I have about ten months left to live if I keep going at this pace.
Given that, five to ten minutes in the examination room is not enough time to think about how I will face my cancer. What would my next move be?
So I ended up getting ten different second opinions so I could see every treatment option available to me for my stage 4 lung cancer.

Your health data should be in your hands… I wanted to make informed choices about my treatment, and I couldn’t do that without understanding what was going on inside my body.

Owning My Own Data
It shocked me how little time you actually get with a doctor. Five or ten minutes is not enough to make big decisions or understand your options. If you want to talk strategy, you have to pay extra or find time outside the system.
That’s why I decided to take control of my own medical data. I started asking for my records: CT scans, PET scans, everything. I had to buy the reports. The data for one report costs about 3,000 Japanese yen. (a little more than $20 US dollars) The hospital put the files on a CD-ROM, and I kept them. I wanted to be in charge of my care. I didn’t understand why other patients just left their information with the hospital and only asked for it when they needed something.
Your health data should be in your hands. You should decide what to do with it. I wanted to make informed choices about my treatment, and I couldn’t do that without understanding what was going on inside my body.
Shared Treatment Decisions
I’ve learned that modern cancer care, especially lung cancer, isn’t just about doing what the doctor says. It’s about discussing your options together. The latest trend is for patients and doctors to consult and make decisions as a team. We have to understand what quality of life means to us. Treatment isn’t just about surviving, it’s about how we live.
Doctors should be clear and direct. They need to say, “This is what’s happening inside you. Here are your options.” Then patients can decide what matters most to them. That conversation is crucial.
I’m taking my stage 4 lung cancer experience forward by helping other patients become empowered.
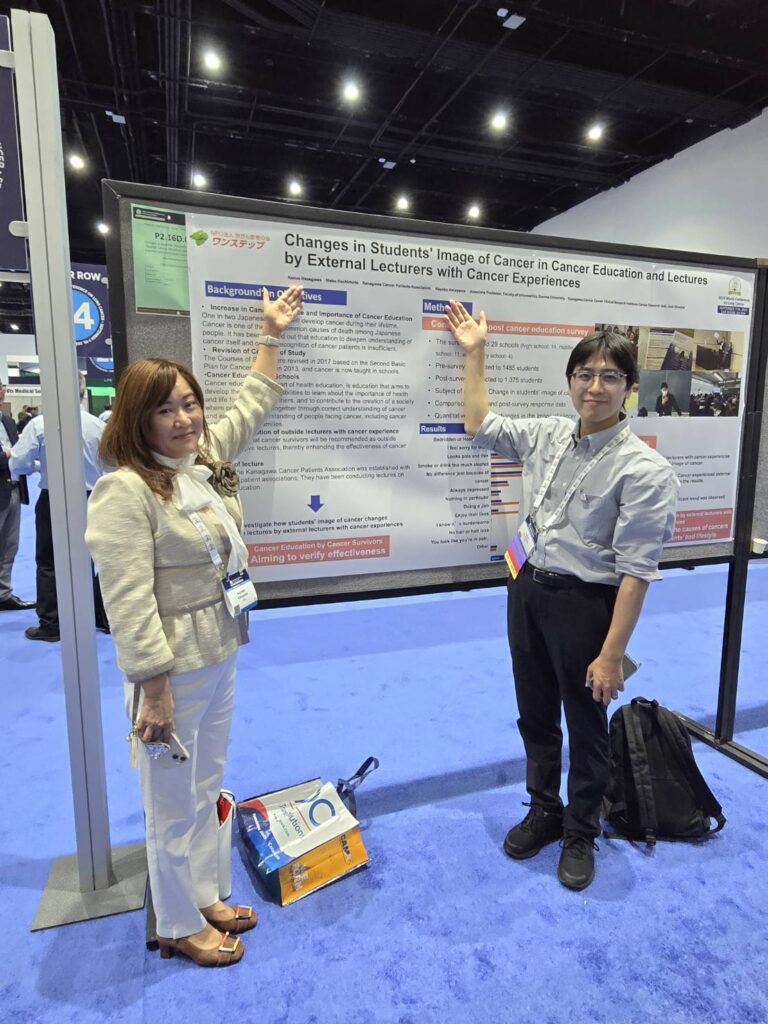
Stronger Patient Empowerment with ‘One Step’
Right now in Japan, most of the information available to patients comes from textbooks. But that’s not enough. It’s like learning boxing from a book and then being thrown into a match. You’d be terrified. You need practice first. Cancer treatment doesn’t give you that time to prepare. The match starts immediately. That’s why I want to provide better resources in that in-between space.
I’m taking my stage 4 lung cancer experience forward by helping other patients become empowered.
That’s why I helped start a patient group called One Step. The main vision of the group is to help create the courage to live. The group now reaches 12,000 people, mostly lung cancer patients and caregivers throughout Japan.
We try to provide useful information: details about treatment, financial support, and what’s happening in the world of cancer care. We also push for patient involvement in research. Instead of just leaving everything to doctors and scientists, we want patients to be part of the process.
We even helped propose a clinical trial, and it got approved. That showed me what’s possible when patients are involved from the start.
When you find yourself saying, “I’ve never faced such a dilemma before”… It helps to ask yourself: What are my values? What do I truly cherish?
There is Hope in Stage 4 Lung Cancer
When you find yourself saying, “I’ve never faced such a dilemma before,” it’s time to consult with others and make a decision. It helps to ask yourself: What are my values? What do I truly cherish? Or, if you were seeing a doctor, you’d bring in information about your physical condition or scientific evidence, and then you’d discuss it together. That’s the kind of process that’s the latest topic in lung cancer right now.
Treatment has evolved. The doctor’s decision or the patient’s decision is not the only decision, but now it’s the choice.
You are making a completely different choice based on your values. It’s very important that you look at the situation from a bird’s-eye view and let patients know that they have a choice to make right now. Of course, in some situations, you should just accept what the doctor says. If you have a major disease like cancer, you won’t know how to deal with it or treat it. You must learn about these things.
So patients are going to have an increasing amount of options for treatment, specific information that they can interpret, and choices regarding treatment and so on. And they are going to be able to think of how to make those choices for themselves. And those treatments are going to evolve more and more.

I want to live. And I believe I can. That belief drives my daily life. I keep going, one step at a time. Maybe this is the answer. Maybe it isn’t. But I’m going to try.

How I See the World Now
Motivation is a wonderful thing. I want to live my life with no regrets.
I think about that, and about my stage 4 lung cancer experience, when I wake up today, the first thing I do is to tell myself that I have only one today. I think it’s because it’s obvious to me that my life is shorter than others’ lives. So I want to do something that makes my life more satisfying.
You see scenes in dramas and on TV where people say goodbye to their families with grace, but I don’t feel that everyone gets to have that kind of ending. Some people die angry or confused, asking, “Why me?” I don’t want to live that way.
Even if my life is short, I want to be satisfied with it. I want to live. And I believe I can. That belief drives my daily life. I keep going, one step at a time. Maybe this is the answer. Maybe it isn’t. But I’m going to try.
Special thanks again to Johnson & Johnson for supporting our patient education program. The Patient Story retains full editorial control over all content.

Inspired by Hasegawa Kazuo's story?
Share your story, too!
More Metastatic Lung Cancer Stories
Lisa G., Non-Small Cell, ROS1+, Stage 4 (Metastatic)
Symptoms: Persistent cough (months), coughing up a little blood, high fever, night sweats
Treatments: Chemotherapy (4 cycles), maintenance chemo (4 cycles)
...
Tara S., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptom: Numbness in face, left arm and leg
Treatments: Targeted radiation, targeted therapy
...