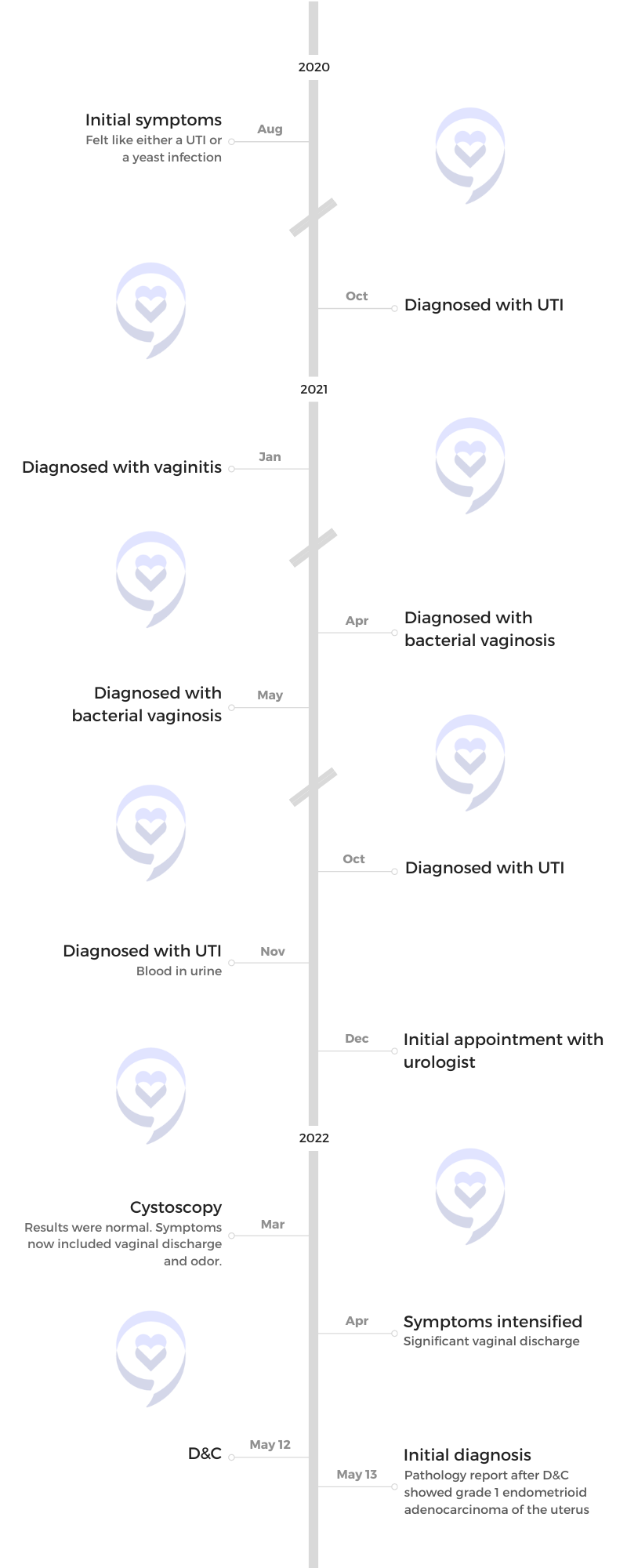
Ellen’s Stage 3C, Grade 3 Endometrial Cancer Story

Ellen was diagnosed with stage 3C grade 3 endometrial cancer.
She started noticing symptoms similar to a urinary tract infection or a yeast infection. After being diagnosed and treated for recurrent UTIs, her symptoms got worse.
A transvaginal ultrasound revealed that her uterine lining was thick, so her gynecologist recommended doing a D&C. After the procedure, they found out she had endometrial cancer.
She shares how she experienced medical gaslighting, going back and forth with different doctors before getting to the root of her symptoms, and the importance of listening to your body and advocating for yourself.
In addition to Ellen’s narrative, The Patient Story offers a diverse collection of patient stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Name: Ellen P.
- Diagnosis:
- Endometrial Cancer
- Staging:
- Stage 3C, Grade 3
- Initial Symptoms:
- Felt like either a UTI or yeast infection
- Treatment:
- Chemotherapy: Carboplatin and Taxol (paclitaxel)
- Surgery: Hysterectomy
- Radiation
Introduction
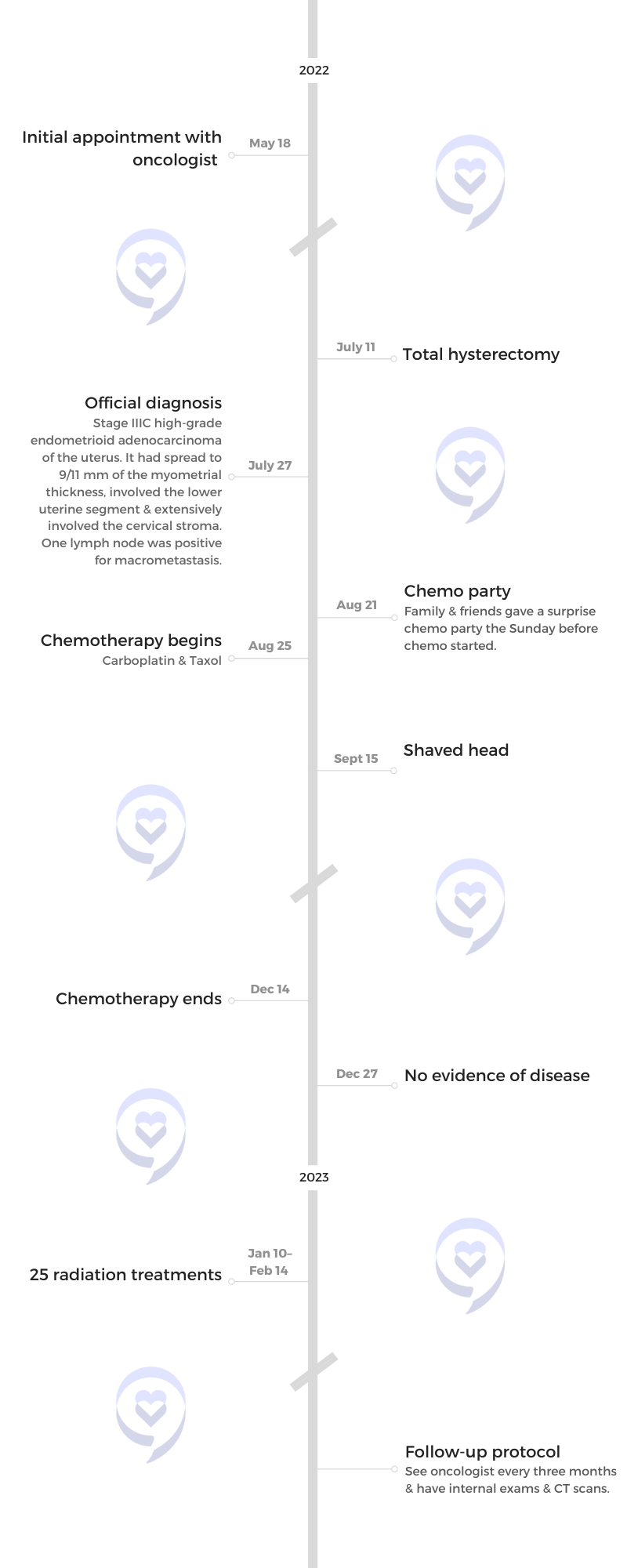
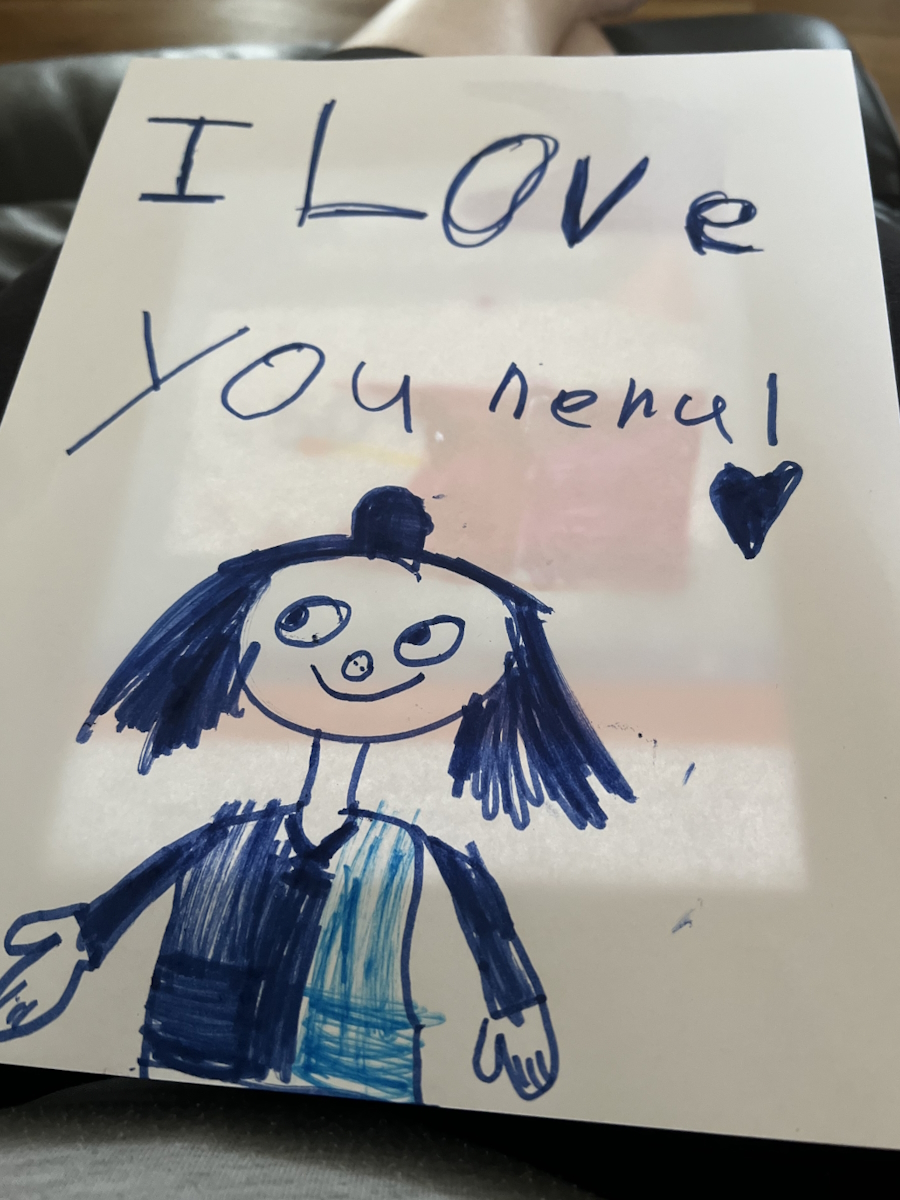
I’m first and foremost a Christian. I’m a wife, a mom, and a Nana. Being a Nana is my favorite. I have five grandchildren.
I love to read. I love to do things with my family. We all live really close together so it seems like my grandchildren are always at my house.
Pre-diagnosis
Initial symptoms
In late July 2020, I started feeling like I had a UTI or a yeast infection. I called the doctor and said, “I’ve got something going on.” They tested me for both and said, “No, you don’t have it. You’re good.” That was August.
Then [on] September 1st, I had my yearly physical. When my blood work came back a couple of weeks later, they called and said, “You’ve got a UTI. We’re going to start you on some antibiotics,” but I [didn’t have] any major symptoms then.
Through the end of 2020, I had a couple of UTIs so I decided to make an appointment [with] my gynecologist instead of my family practitioner.


Seeing a gynecologist
They said I had an infection and gave me some medicine. Then they said I had a yeast infection and gave me medicine for that.
I saw him a few times and I said, “That’s not helping me get any better so obviously that’s not it.” I started feeling maybe it was urine and not vaginal discharge. I thought, That’s probably what it is. I’m having all these UTIs.
Through 2021, UTIs and discharge got worse. Through all of this, I never saw blood. It was a clear discharge so it didn’t connect with me that it might be vaginal. I was post-menopausal for 13 years already. I thought all of that was behind me. I didn’t even think about that.
At that time, my mother was sick and she moved in with me. She was in her late 80s. She was incontinent. I thought, This is what’s happening to me. What I thought was UTI didn’t turn out to be. It turned out to be the cancer getting worse.
My family practitioner said, “It’s time we go to a urologist.”


Seeing a urologist
I went to see the urologist and he said, “This really worries me. Let’s schedule a cystoscope.” It ended up getting put off until March because my mother passed away.
He did it, came back in, and said, “You don’t have anything wrong with your bladder. If you would just lose weight, you wouldn’t have to worry about incontinence.”
I said, “I’ve been overweight all of my adult life and this has never happened to me before. But I can assure you I’m not going back here.”
Follow-up appointment with the gynecologist
I went straight to the car, called the gynecologist, and said, “I need another appointment. This is vaginal. We got to do something.” I saw him within two weeks.
He scheduled a transvaginal ultrasound and said, “Your lining is really thick. Let’s put you on some progesterone.” I said, “No, I’m not taking progesterone. I told you many years ago I was not taking that anymore.” He said, “Let’s do a D&C then put in a Mirena IUD,” which we had done in 2008 and had worked great.
We did that the [following] week. When the D&C was over, he came out and told my husband and then told me later, “We’ll talk when the pathology report comes back. I don’t like the looks of it.”
Diagnosis
Getting the official diagnosis
He called me and said, “I’m sorry to have to tell you this, but you have endometrial cancer. Don’t worry. We probably got it early. It’s not a big thing when you catch it early.”
He said slow-growing. I asked, “How slow is slow? Because I know that I’ve been having symptoms that I can feel for almost two years.”
That was Friday afternoon. Charlotte has Levine Cancer Institute and I got in to see the head of the department on Wednesday and scheduled a hysterectomy. My sister was with me.
I had a big tumor and she used her fist as [the] way she describes it. I told my gynecologist, “That tumor is on my left side, isn’t it?” He said, “Oh, no, it’s not a tumor that you can see.” The lymph node that the cancer had spread to was on the left side and it was where it hurt. It had spread to my cervix and to that one lymph node.
When the pathology report came back, it was grade 3. I’m stage 3C and it’s grade 3, which is a more aggressive cancer.
We were coming home from the meeting after the pathology report came in. My daughter-in-law said, “If you hadn’t been proactive, if you hadn’t pushed, they would have let you die.”


Reaction to the diagnosis
[When] my gynecologist said we’re going to do a D&C, it was a frozen-in-time moment. I said, “Thank you because I’m telling you something is very wrong with me.”
I don’t need negativity in my life. I tried to let that go because I can’t fight the fight being bitter or upset about the past.
I know that doctors are in a big hurry and they have a whole lot to deal with. I wish all medical people would not look at someone’s size and assume that if they lose weight, their problems would go away and not assume that you don’t know what’s going on in your body.
I knew something was wrong. I don’t know how to make people listen to your concerns. Even if you go through a whole bunch of tests and it comes back that it’s nothing, then great.
Had somebody listened to me a little bit earlier, we could have gotten this cancer while I was still in stage 1. Now, I’m in stage 3. Maybe I haven’t processed it yet.
Treatment
Discussing the treatment plan with the medical team
I had carboplatin and Taxol (paclitaxel). I had six cycles every three weeks.
Then I had 25 radiation treatments.
I have a wonderful gynecologist-oncologist. She came in and said, “Ellen, you are going to lose your hair, but we’ve got medicine for everything else. We will work through it and we will treat your symptoms.”
Preparing for treatment
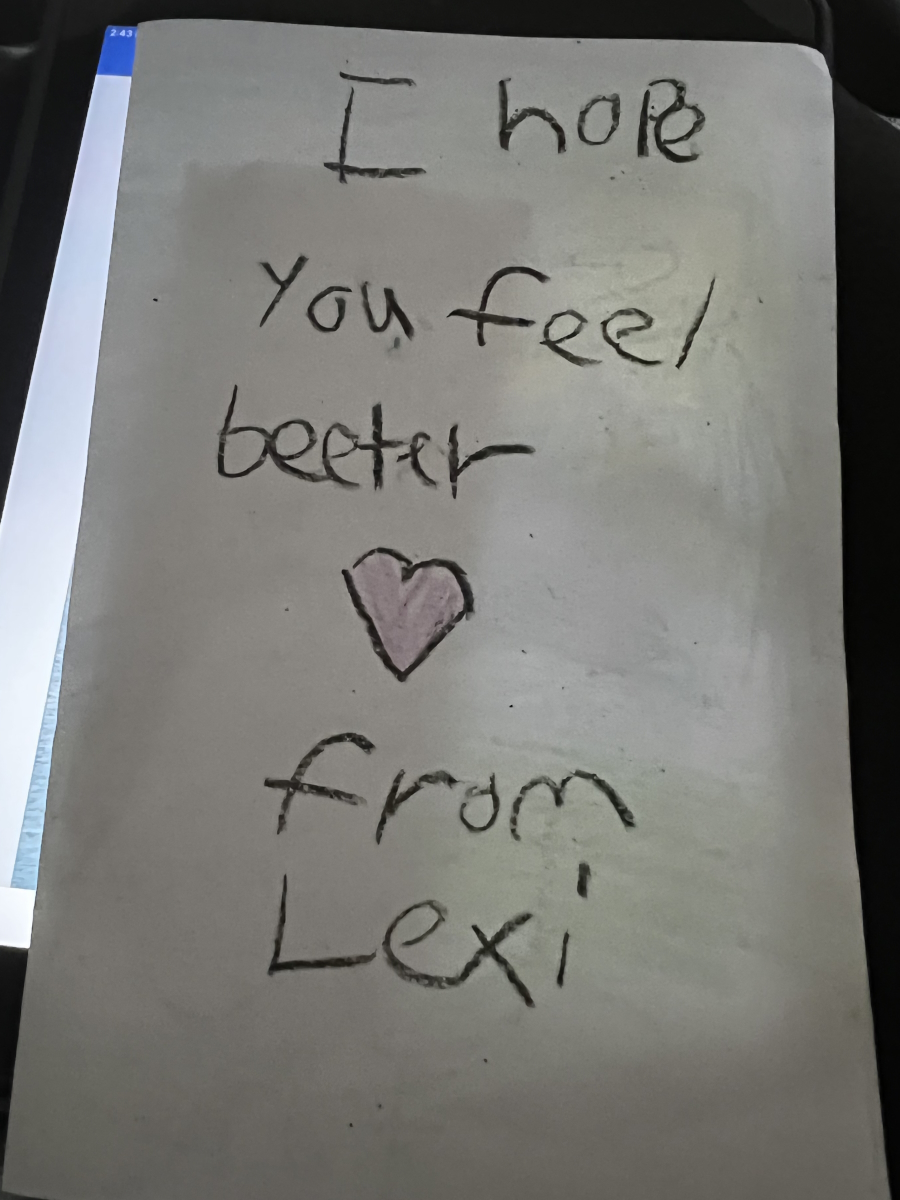
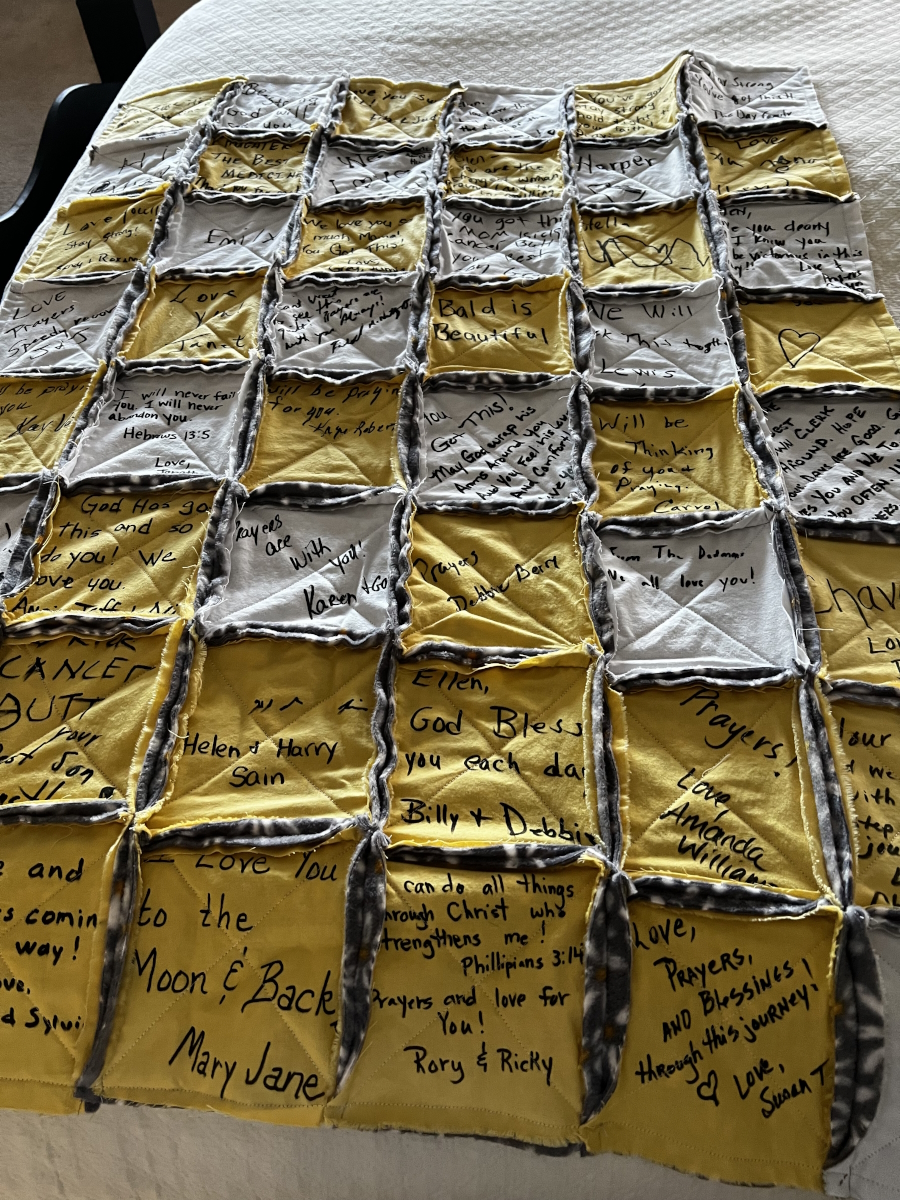
My family and friends gave me a surprise chemo party on [the] Sunday before my chemo started. Everybody who is somebody to me was there. It was a big, wonderful party. One of the things they had as decoration was a bald Barbie and all of my granddaughters loved it.
When we were talking to the pharmacist and nurse navigators, getting ready for the chemo, they gave me enough bald Barbies for all of my granddaughters to have their own bald Barbie. They all really loved them and played with them. That helped prepare them for the fact that Nana was going to look different for a while so that was a really good thing.
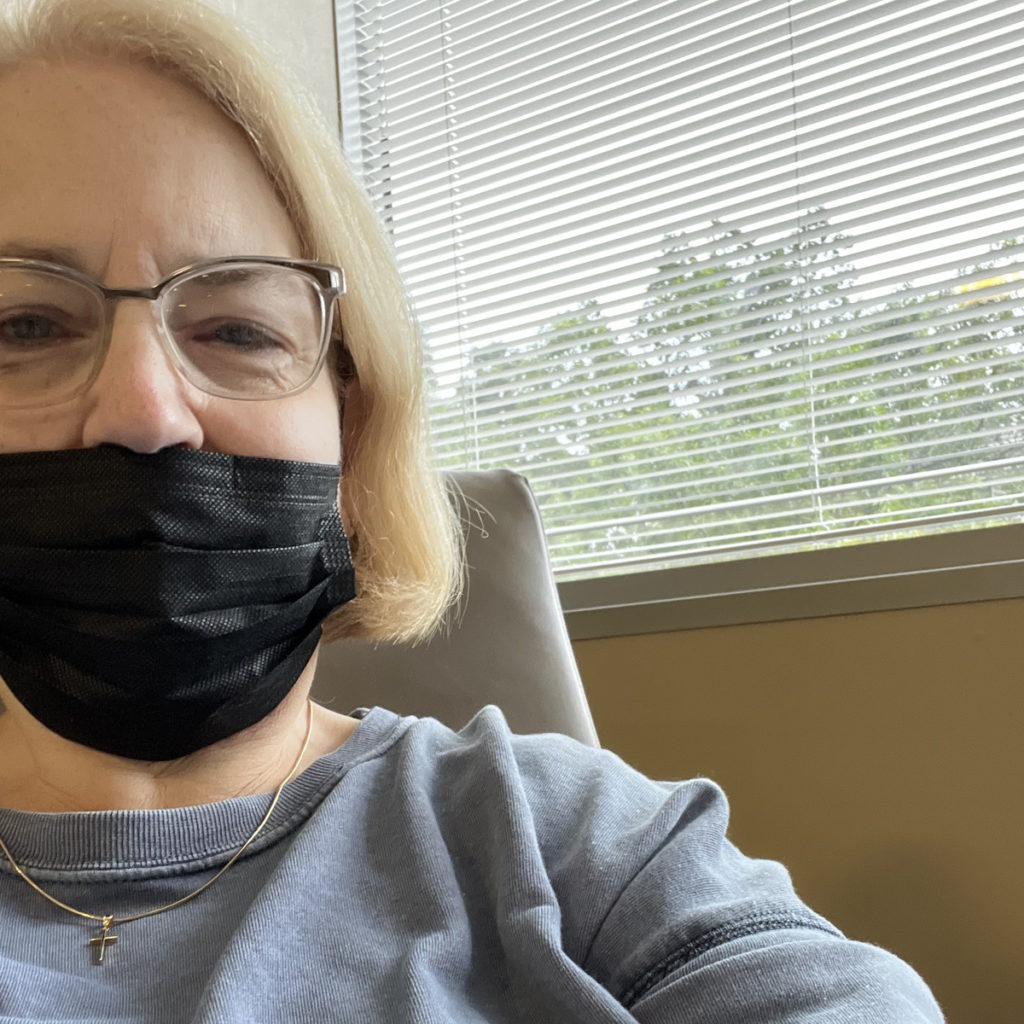
I know that’s been this way for every cancer patient since COVID, but it was really sad to have to go in there by yourself. Treatment lasted for six hours. It was so hard.


Side effects from chemotherapy
I didn’t even know chemo dread was a thing. You have such a bad feeling the day of chemo or when you even would think about a chemo treatment coming up.
I got really nauseous, but there is good nausea medicine.
My hair fell out. I got proactive about that a little bit. I started cutting it shorter and then as it started coming out, I shaved it off because I could not stand my hair being on everything.
The first one made me really sick. The steroid made me feel bad. But for the last five cycles, the steroid kept me feeling good for the three days that I took the steroid. The fourth and fifth days were really bad. Then I started feeling a little bit better.
Before the third or fourth cycle, I told the nurse navigator, “I’m so tired.” She said, “Usually the people who stay as close to their regular schedule do the best.” I said, “I stay ‘til I work all day, get home, and get supper. I’m worn out.”
I missed a few work days every cycle. As the cycles progressed, the harder it was to work. I would be so tired.
I’d be asleep early and sleep for a long time. I remember telling my doctor, “Sometimes I go to bed at 6 o’clock at night and I sleep ‘til 6 o’clock in the morning.” She said, “You’re tired. That’s not strange. It’s not abnormal to need that much sleep.”
Managing the side effects of chemotherapy
I took Claritin every day and that really helped with the bone pain. As the treatments progressed, my nausea lessened.
The hardest thing was the fatigue. It was bone-deep weariness. Getting up and getting to my chair was an effort. Going to the bathroom and back to the chair was an effort. Being able to get in the shower was a no-go for a couple of days. I don’t even have a word to describe how that felt.
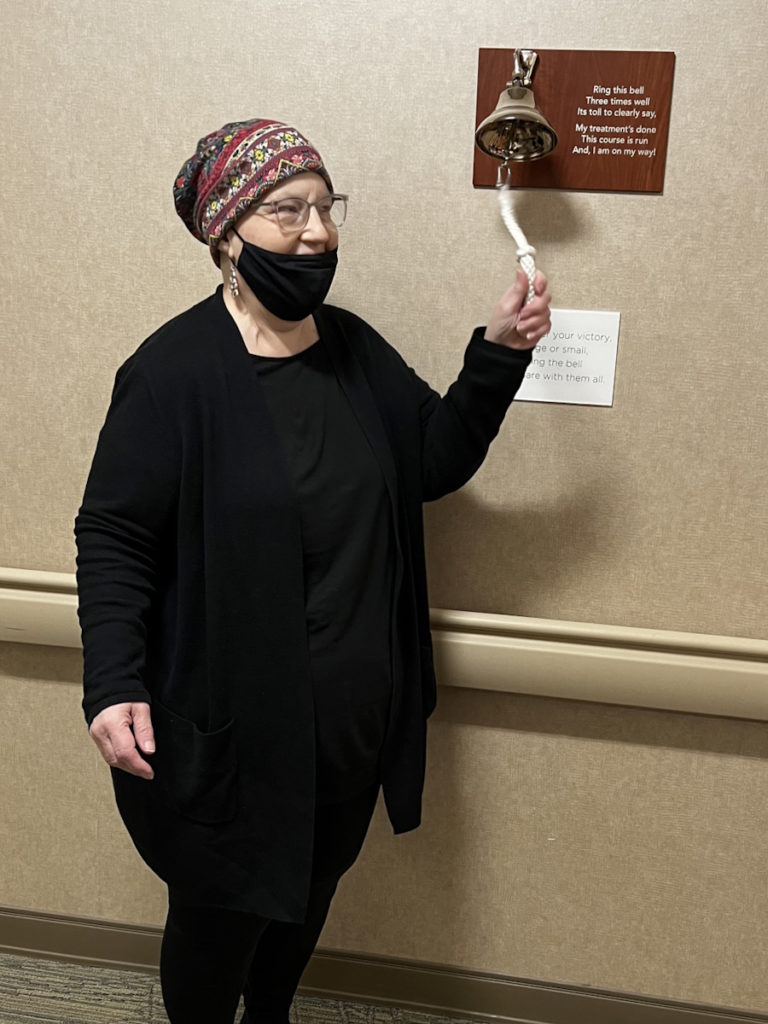
No evidence of disease
I had a scan at the end of the six cycles and I have had no evidence of disease. I still have no evidence of disease so that is really great.
Honestly, I was so sick and felt so bad that all of the people in my life were much more excited about it than me. I felt so bad that it was hard to be totally excited. That still seems a little unreal to me.
I had that at the end of December then I started my 25 radiation treatments in January. The first week, I was so tired. I could not function. I thought, There’s no way I’ll be able to do 25 of these treatments. After those first couple of days, I had bad diarrhea, but the diarrhea [was] not much after the chemo tiredness.

Words of advice
See a gynecologist
If you’re a woman, you need a gynecologist. Ten years post-menopause, I thought, I don’t need a gynecologist anymore. I’m not having a period. I have had zero issues. I can just let my family doctor do that. I made that decision and that was a bad, bad decision. I will have to [deal with] the repercussions of it for the rest of my life because I let it go.
You can’t rewrite history. It may not have made any difference because they may have just let that go. Women should not ignore their feminine health, whether that’s a mammogram or a pap smear. If something’s just not right, we need to have a doctor who we’re seeing regularly, who knows us.
Listen to your body
I never really thought it wasn’t a UTI until the urologist said, “You have not been having any UTIs. Your bladder does not show that.”
Every time, the culture grew something different. I think a gynecologist would have put all of the pieces together.
They removed my cervix. I still need a gynecologist because things can happen in your vagina. You can have cancer there. You still need somebody checking all these places. Everybody does.
Have faith
It’s very important to have faith when you’re facing such a big diagnosis. I’m not really sure how people face it without faith.
Panic was such a major thing for me. I would feel it rising inside of me. If I let that take over, there is still so much to be panicked about.
More women die of endometrial cancer now than ovarian cancer. Endometrial cancer does not have the same press as breast cancer or ovarian cancer, but it is something that we need to put as much emphasis [on] as the other three. It is still very scary.
I know everybody handles it differently, but my faith gave me that peace. The Bible says it’s a peace that surpasses all understanding. I can’t explain it, but that did give me peace in the middle of this journey.


Advocate for yourself
The main thing is to be an advocate for yourself. Doctors have a lot of patients. You have to be able to say, “No, wait a minute. This is wrong. Something is not right here. You’ve got to look at me.”
One time long ago, I had an allergic reaction to medicine. I made an appointment because I was itching and they messed up my appointment time. I lost it in the doctor’s office. I said, “No, I can’t stand this itching one more day. You’ve got to do something.” They got me straight into the doctor.
If you push enough, you’re going to get in and get somebody to listen to you. You just have to keep pushing. Stand up for yourself.

Inspired by Ellen's story?
Share your story, too!
3 replies on “Ellen’s Stage 3C, Grade 3 Endometrial Cancer Story”
A good friend was just diagnosed with Stage 3C endometrial cancer. She went through many doctors to determine this diagnosis. She is a young 63 yr. old. She says she is going to refuse radiation and chemotherapy. This sickens me, because I feel this will reduce your chance of survival. I understand she doesn’t want to put herself through those treatments. What should I do?
Thank you Ellen, I was diagnosed September 2024,October 2024 had. Total Robotic Hysterectomy,Im Stage 2 , Ive currently has completed 3 cycles and cycles 4&5 will be Feb 7 and 28th.
I can so relate to your story as I am a survivor of Endometrial Adenocarcinoma Stage 3 C with metastasis to the peri-aortic lymph node. It is so important women learn about the wide range of symptoms associated with uterine cancers, which makes everyone’s story so important. It is regrettable you battled this during the main throes of Covid, but I know you still met some wonderful people along the way. I myself experienced a great deal of gaslighting concerning my symptoms, yet even with my gynecologists. I did not have chemotherapy but radiation.You so wisely stated– you must be your own advocate! God has His hand over you, and He will lead you through this and out from it! One month from today, I will reflect on my 19 years as Endometrial uterine cancer survivor–Stage 3 C as yourself! So I know you will be a survivor too! I look forward to meeting you one day, with Christ by our side!