Stephanie’s Stage 4 Primary Mediastinal Large B-cell Lymphoma (PMBCL) Story

After her father’s Hodgkin lymphoma diagnosis, Stephanie still never thought her persistent cough was anything more than allergies or asthma. But after her cough progressed and she couldn’t do or say anything without coughing, she finally decided to go to urgent care.
As doctors cleared fluid from her lungs, they found a mass in her chest. She was then diagnosed with stage 4 non-Hodgkin’s lymphoma only two years after her dad’s diagnosis.
She voices how she processed her diagnosis, how she advocated for her health, and how her father’s diagnosis impacted her cancer journey.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
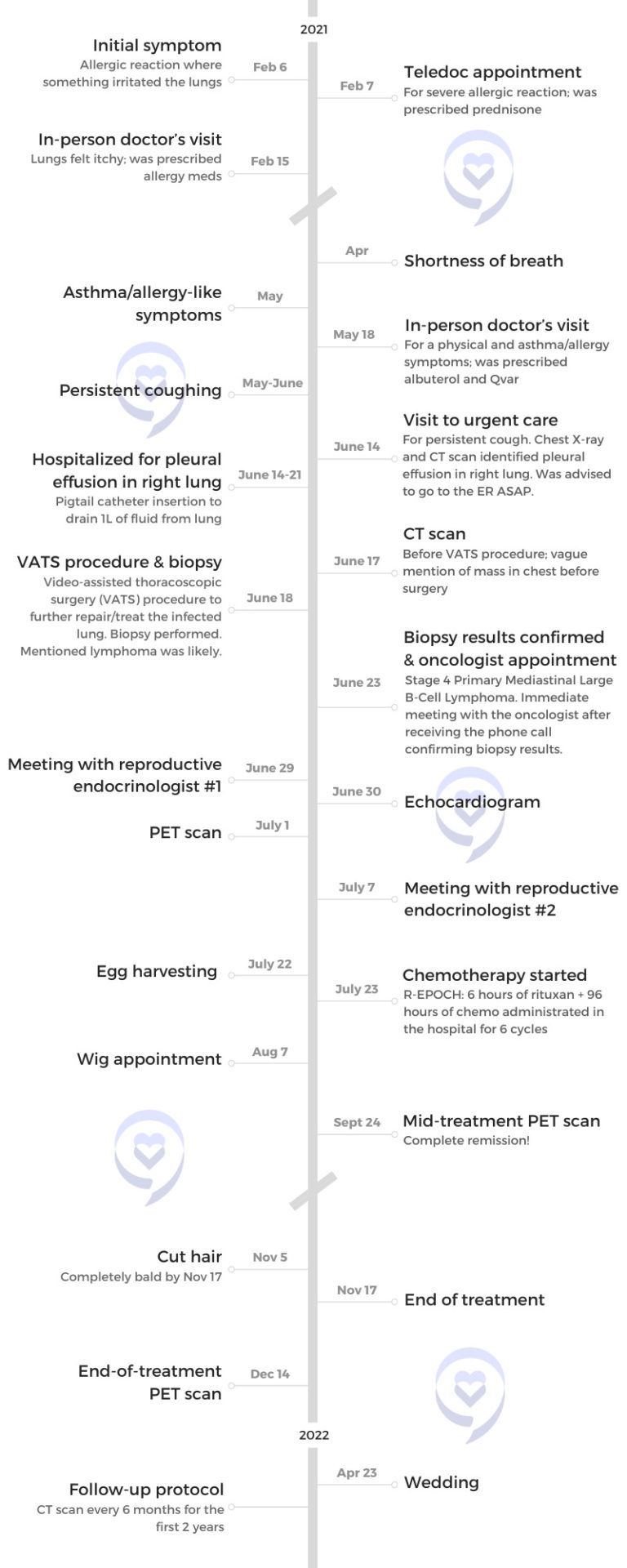
- Name: Stephanie V.
- Diagnosis:
- Primary mediastinal large B-cell lymphoma (PMBCL)
- Staging: 4
- Initial Symptoms:
- Allergic reaction
- Lungs felt itchy
- Shortness of breath
- Asthma/allergy-like symptoms
- Persistent coughing
- Treatment:
- Pigtail catheter for pleural drainage
- Video-assisted thoracoscopic surgery (VATS)
- Chemotherapy: R-EPOCH

Introduction
I work in private wealth management. I manage a team that oversees investing high net worth accounts. I enjoy developing my team members and associates that report to me; that’s always been something I’ve been interested in since I started with the company. I’ve been with them for almost eight years so it’s been quite an endeavor in that sense.
In my spare time, I like remaining active. I’ve danced since I was 2.5 years old. My passion was always ballet, but I also did tap, jazz, [and] contemporary.

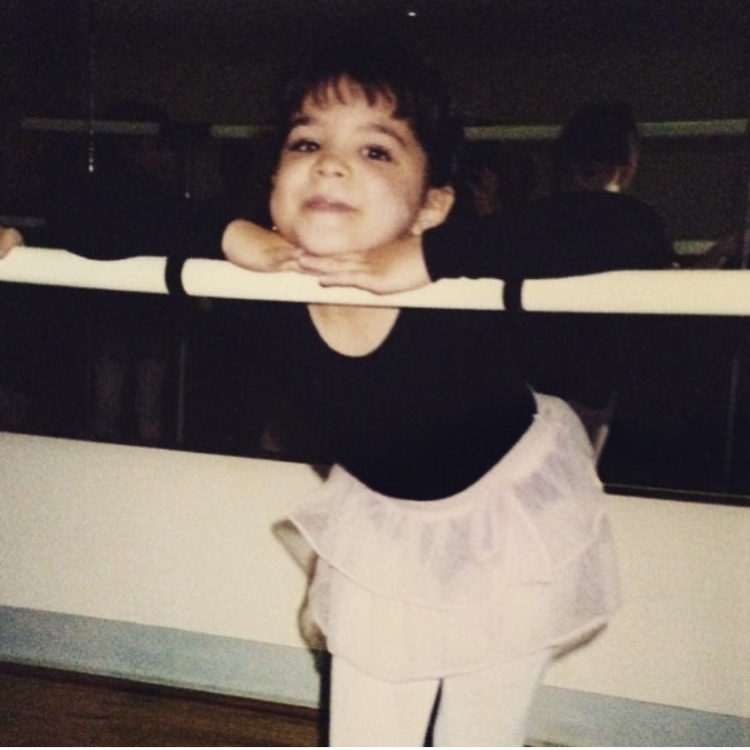
I studied dance in college with a focus on economics. I did dance on the side knowing that it wasn’t going to be my end goal or career, but something that I kept up with. Now I’ve translated that into exercising on a regular basis and trying to keep active. Remaining active has always been something important to me.
In the winter, we go skiing and spend time with family. It’s always been very important to me.
My father’s Hodgkin’s lymphoma diagnosis & journey
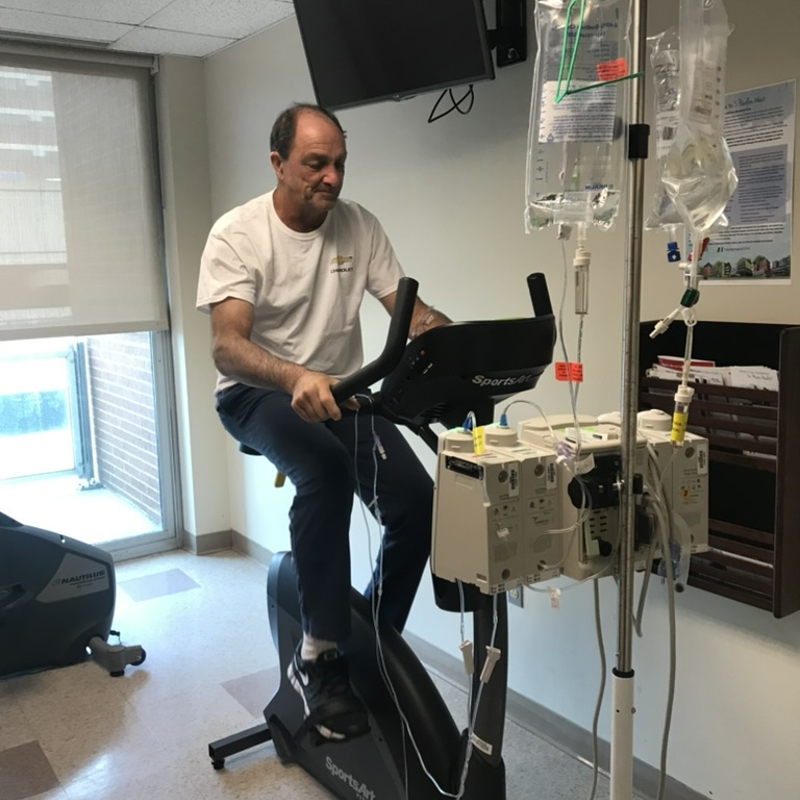
We’re very healthy individuals, my dad specifically. He works in construction so [he has] an active job. He’s very tall, very lean, [and] very healthy.
We started to notice [that] he had this cough in late 2017-early 2018. He works in dirt so we thought, Oh, he’s inhaling too much dust. He’s just coughing it out. It did become very persistent and we said, “Maybe he should go to the doctor [to] get this checked out.”
He hadn’t been to a doctor in 20 years; didn’t really need to go because he’s a healthy person.
His tumor was so dense [that it was] difficult to get a good sampling. He had many biopsies because every time, the results came back inconclusive.
The doctors knew that he pretty much had Hodgkin’s lymphoma. He had every symptom in the book: night sweats, weight loss, coughing, and itching. We knew he was sick, but we couldn’t get that confirmed diagnosis.
After about three or four months of going back and forth and finally getting that confirmed diagnosis, he was able to start treatment. I forget what treatment he did, but I consider it an old-school treatment. It wasn’t the ideal treatment that they wanted to do for him, but they did that one I think because of insurance purposes.
He went through his treatment cycles and had a clean scan, but within three or four months, he had the cough, itching, [and] night sweats again. It came back.

The next plan was to do a stem cell transplant where he was his own donor. Now, this is [the] summer of 2019. He was in full isolation. We were wearing masks and gloves to visit him. We could have visitors at that time as it was pre-pandemic. He started to do immunotherapy as [a] maintenance treatment after the stem cell transplant.
He’s been good ever since, thankfully. He has his regular checkups with our lymphoma team at the cancer center. He’s now doing one-year scans but has a checkup every six months. He was pretty much confirmed clean before the pandemic started.



Initial symptoms
I didn’t really have any symptoms other than a persistent cough. I pinpoint this back to a day in February [when] I might have had a food allergy mixed in with some dust contact shortly after. I guess my immune system might have been down and couldn’t fight whatever was coming into my body at that point.
I did a teledoc appointment that weekend. My face was very swollen and I was prescribed some prednisone. A few weeks later, I still didn’t feel very well. I still had itchy lungs.
I went to the doctor in person. They prescribed allergy medication. It was winter in New Jersey. I already have food allergies [and] eczema and so I said, “Okay, add it to the list.”
I noticed shortness of breath in April 2021. I was actually supposed to get married [that month]. My husband, then fiancé, [and I] were in Newport, Rhode Island, for our would-be wedding date and we were walking around. Our hotel was over a little bridge that had an incline.
I noticed that I was getting out of breath and we were just walking around, not even having anything to drink. It was just a nice day and I was very out of breath. I had to stay in the hotel room more than we’d liked.
May 2021 was when my symptom progressed. I started to have a cough and more asthma allergy-like symptoms where I definitely was more short of breath. I went to the doctor and they said, “It’s probably asthma. I’m going to give you two inhalers.” One was albuterol and something called Qvar, which was a little bit more intense. I said, “Okay, this was probably coming.”
Coughing progressed
By June 2021, my coughing had progressed a lot more where I really couldn’t do anything or say anything longer than a sentence without coughing nonstop. It was impacting my work.
I speak a lot. I do training for my team and I couldn’t get through a presentation or even a sentence without coughing so that was becoming a lot more noticeable. Definitely, not a time when you want to have a persistent cough. It was confirmed many times [that I] didn’t have COVID.
After not feeling well to the degree that I was that morning, I finally decided to go to urgent care. I was going to go that week, but I realized that morning I had to go. I did get sick from coughing so much. I think my body was probably doing it out of habit at some point, too, just because I couldn’t go more than two minutes without coughing.
I was convinced it was pneumonia at that point just because [of] the way I was coughing. I just couldn’t breathe.


Pre-diagnosis
Going to urgent care
First, I went to urgent care where I demanded an X-ray. They said, “You might have COVID.” I knew I didn’t. I asked for a chest X-ray.
Before I even put my clothes back on, they said, “You have something that’s called a pleural effusion or an empyema and you need to go to the emergency room right away.”
This was a different medical group than where I ended up getting all my treatments. They said, “Go to this hospital. We’ll call you in.”
I said, “If this [has] anything to do with my lungs, my dad already has a pulmonologist that’s at a different hospital network. We know people there. I’m going to this emergency room instead.”
They called the hospital that I wanted to go to. You need to advocate for where you want to go [and] what you want to do because it is all about you at that point.
Going to the emergency room
I did get to the emergency room. This is the middle of the day on a Monday [so there were] a lot of people in the emergency room, probably about 50 people waiting. I [was] waiting my turn and the second I said my name, they said, “We’ve been waiting for you.”
They pulled me into another room, threw a gown on me, [and] started to do all these tests. I’ve never been to the hospital other than when I was born. I go to the doctor [for] my yearly visits. All these tests, all these patches on me, [I was] getting a little nervous.
Then they said, “Okay, we have your blood.” At urgent care, I did not have a fever. The second I got to the emergency room, I was 101°F or 102°F. I think my body was just saying, “Okay, this is time. We’re going to show every symptom we have now.”
They put me on a gurney and rolled me into my other room. I did start to cry a little bit because I was very overwhelmed. I was with my sister and at first, [we] were very lighthearted. We make a joke out of everything so I was said, “Oh, I guess it pays off going to urgent care first before going to the ER because they can give a heads-up.”
Everyone else is either walking to an exam room or in a wheelchair, but I get a gurney and I said, “Okay, no one’s really telling me what’s going on. They’re just all acting a little fast.” That’s when I got a little bit nervous.





They told me I had about a liter of fluid in my right lung that needed to be taken out. They couldn’t do it that day, but they would be able to do it the next day. Not only was this my first trip to the hospital, [but I’m also] now automatically staying [the] night.
I was admitted on a Monday. They didn’t know it was cancer until Friday. There’s so much fluid in my lung that they first thought pneumonia or pleural effusion and they need to get that out. Once they cleared out the lung, that’s when they did the CT scan and saw the mass in my chest.
They didn’t tell me until Friday. They were just concerned about what was happening in the lung and how to treat it. I don’t know if they didn’t care to look at it. I don’t want to make it sound like the doctors were being careless, reckless, or anything like that, but I think they were just addressing that issue first.
Rolling into the OR, they said, “Oh, by the way, can you sign here? Because we’re also going to biopsy this mass in your chest.” All I remember thinking was, Interesting. My dad had a mass in his chest, but at that point, I still didn’t think it could ever be lymphoma. I said, “Oh, that’s interesting,” and the next thing I know, [I’m] getting a mask on me and going to sleep.
There’s so much fluid in my lung… Once they cleared out the lung, that’s when they did the CT scan and saw the mass in my chest.
Requesting a chest X-ray
That is a lesson learned from my dad’s experience. He is considered young by most standards so I’m considered extra young.
When he had the cough, I think he had gone to the doctor maybe two times, one for a physical because he hadn’t gone in so long.
At that point, I think anyone over 50 should be getting a chest X-ray from what I understand. But that first doctor did not do a chest X-ray so he could have seen something earlier.
When I was coughing so much, my mom said to me, “When you do go, get a chest X-ray because that’s where we’re going to start every time,” not thinking that this was going to turn into stage 4 cancer.
We said, “Okay, it’s what? $12 for a chest X-ray with insurance or something like that. It’s very harmless and we’ll just cross that out.”


Getting back from the OR
I wake up. They cleared out my lung, but there was still a lot of infection in there. While they were in there, they took [a] biopsy of the chest and the lung as well.
I get rolled into the surgical ICU for recovery. This is pandemic time so we only had two visitors at a time. A couple of minutes later, my mom, dad, and fiancé came in. I thought, “Interesting. We have three guests. How did we do this? This is very nice.” If my sister was there, that would have been the goal but, obviously, we can’t push it.
I had my important people there and I was asking my fiancé because he was sitting right next to me. I asked, “ Did they say anything? They mentioned a mass [in] my chest. Did they mention anything about it? I don’t know what that is.” He just shook his head and said,, “I don’t know about that.”
I have a popsicle in my mouth because I had a sore throat from the anesthesia. I’m licking away and I said, “Okay, well, this is it, guys. I’m going to be here for a couple of days, go home, and we’ll all laugh about this later.”
She immediately called the cancer center and said, ‘My husband’s a patient and I believe my daughter’s about to be a patient. What can I do?’
Diagnosis
Getting the official diagnosis
The doctors come in. I thought they were just going to go through the surgery and say what I have to do to fix myself. It was actually a team of surgeons. They can’t say it without having [the] biopsy results, but the doctor was very confident that I had lymphoma in my chest.
I looked at my fiancé and my parents and asked, “Are you sure you didn’t pull my dad’s files? We’re in the same hospital unit and he had [a] mass in his chest. Dad has lymphoma, not me.”
They left. My mom’s face, I knew she already knew the information. What I came to learn was the doctor called her, telling her that I was out of surgery. He said, “I was able to look at the actual mass and at the cells and I believe it’s lymphoma.”
She said, “Please do not tell my daughter until I get to the hospital with her father [and] her fiancé. She cannot hear this news alone.” That’s how they got three visitors in the hospital.
The second she got that phone call, she went into her mode. This is Friday afternoon. She immediately called the cancer center and said, “My husband’s a patient and I believe my daughter’s about to be a patient. What can I do?”

We didn’t have the biopsy results but she wanted to get our names on the board immediately.
She did say she paused because again, I’m in this transition of getting married and my spouse might be the one who wants to make some decisions, too. She had to pause and turn to my fiancé and say, “Are you okay if I start running with this?” He said, “Please. Go right ahead,” because she knew the road to take and we just had to get right in there.


Reaction to the cancer diagnosis
I still think it’s absolutely bizarre. We’ll never understand. I’m not sure when I’m going to say, “I just had stage 4 cancer and my dad had it, too, all within five years.”
I was very calm. I don’t think it actually hit me until someone mentioned family planning. That was hard to understand, especially as I’m trying to get married and I have someone who is looking to me to start a whole life together. I thought,“Well, this might get cut short.” But otherwise, I was calm.
I like to deal with things as they come. I accept it and say, “Okay, what are we going to do about this?” I do that in my work. I’m learning in my life, too. That’s not to say I don’t have anxieties or stresses about it, but I do think I remain calm under these pressures.
You never want to see that look on both my parent’s faces. You never want to be the cause of their worries. I think that that happens naturally when you become a parent, I’m sure. But to this degree, I don’t think you ever want that.
My mom’s got her way of reacting [to] things. But I know with her, I was in good hands. We knew what we were going to do. It was going to get done.
With my dad, [it] was hard to look at him, and over the course of the next couple of months, too, because he knew what I was about to go through more or less. You don’t want that for anybody.
He said, “If I could trade places with you, I would ten times over,” and you just don’t want to hear that. I don’t want him to go through it again, too.
I think it’s more stressful for me to see everyone else worry about everything… You don’t want to be the cause of people’s worries and restless nights.
We’re [a] family who jokes and tries to make light of things when we can. Looking at my fiancé at the time, I said, “You can get out now. It’s going to get ugly.” My mom said, “Yeah, James, we’re going to give you three tries and after three, you’re in. So here’s your first try. You can go.” Of course, we’re joking and, obviously, he wouldn’t leave.
You don’t sign up for those things. No one does. But we didn’t even say “I do” yet and this is the “in sickness and in health.”
I think it’s more stressful for me to see everyone else worry about everything. That was the heaviest weight to carry. Not my health or what I had to go through but seeing other people go through it. Seeing it with my dad, I knew as a loved one how that felt. You don’t want to be the cause of people’s worries and restless nights.
Having a support system when you get your cancer diagnosis
I wouldn’t have expected it any other way. There’s no scenario where they wouldn’t have been there. I think that’s the part that she gets done every time, like having those three people in the room knowing that this is life-changing news. If she could get my sister in there, too, she would. I think that’s just the way she does things.
You can’t just hear about it by yourself with a SpongeBob popsicle stick. You need those people around you. That’s when day one starts.
You’re never alone in this process. But to hear that news, you cannot be alone. For her to do that, that’s the person that she is, knowing that she’s done it before.


Treatment
Starting treatment after cancer diagnosis
It was about a month afterward. I got the confirmed diagnosis a few days after I was released from the hospital. I got [a] phone call from the surgeon.
I called my mom right away and said, “Okay, it is lymphoma.” There was a case where it could have been some lung disorder or disease that would still be treated with chemo, but it wasn’t cancer, so that was also a blessing in disguise. We said, “Well, we know lymphoma so we’ll take it.”
My mom immediately called the cancer center and said, “We officially have the diagnosis.” The surgeon was about to call the cancer center as well.
The cancer center called me back and said, “Our oncologist has an appointment open [in] 45 minutes. Can you go?” My mom’s at work, I’m at my house, and the cancer center was about 25 minutes away. I said, “I don’t know if we can get there. Let me call you back.”
I called my mom. I said, “She’s available in 45 minutes, but you’re at work, Mom.” My mom said, “No, we’re going. I’m dropping everything.” She had an amazing boss at the time who was so understanding and knew everything about my dad’s history. Anytime anything happened, she would just say, “I have to go,” and he said, “Okay.” That’s it, no questions asked.
She picked me up. We sped down to the cancer center and got our appointment with the oncologist. She’s a rock star.
These are people who’ve known my mom now for a little over two years. They know my dad. They’re the younger couple so people tend to recognize them and know them in the unit.
The look on their faces… The head oncologist and her team of nurse practitioners had this look. My doctor said, “I’m so sorry.” She genuinely was upset that we were in there.
She went through the whole thing and that’s when they said the staging. My dad never got a staging. They just treated him. My parents had asked a couple of times, but they never really clarified. We think maybe 2 or 3 and I could totally be wrong about that.
But for me, right away, it was, “Okay, well, you’re stage 4.” I said, “What?” I didn’t have any symptoms other than this cough, but my lung was completely infected and that was all the cause for it.
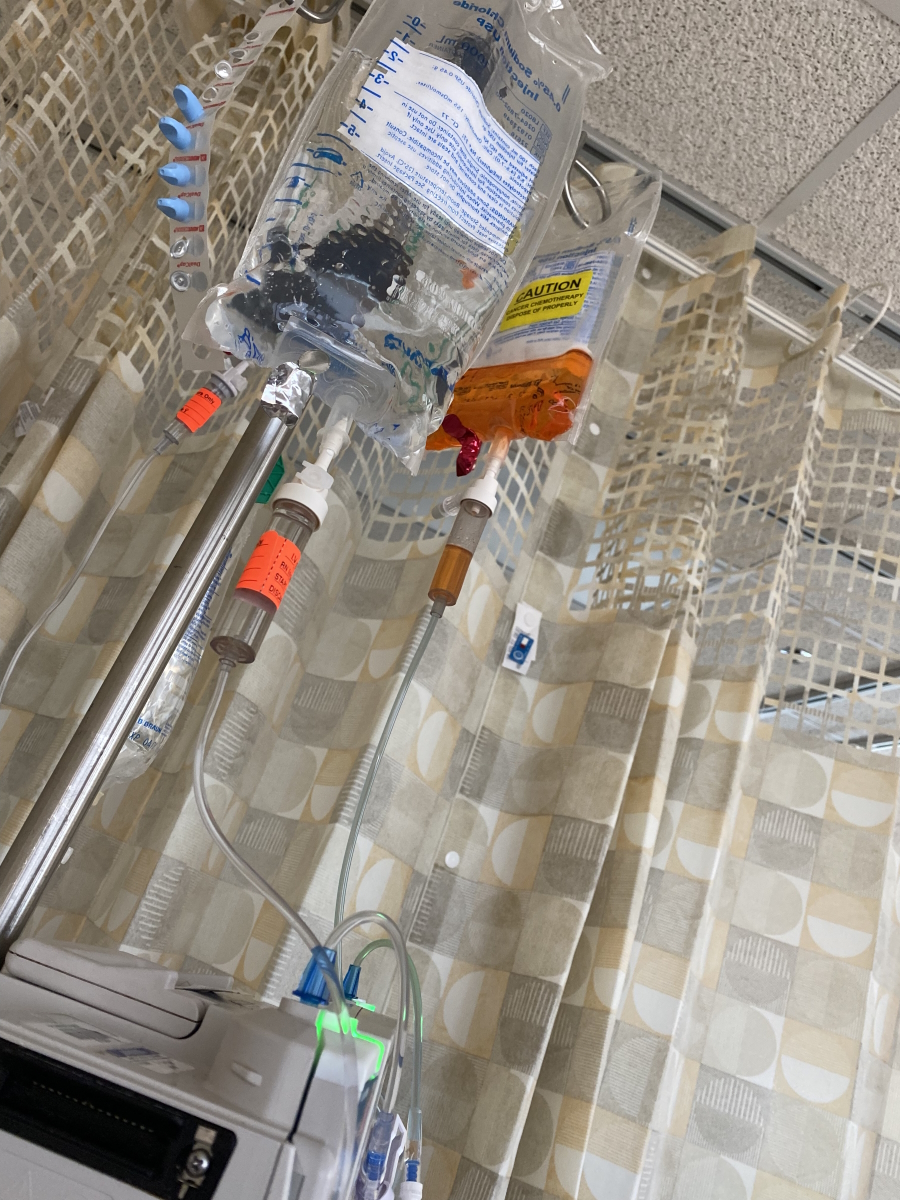


Immunotherapy & chemotherapy treatment
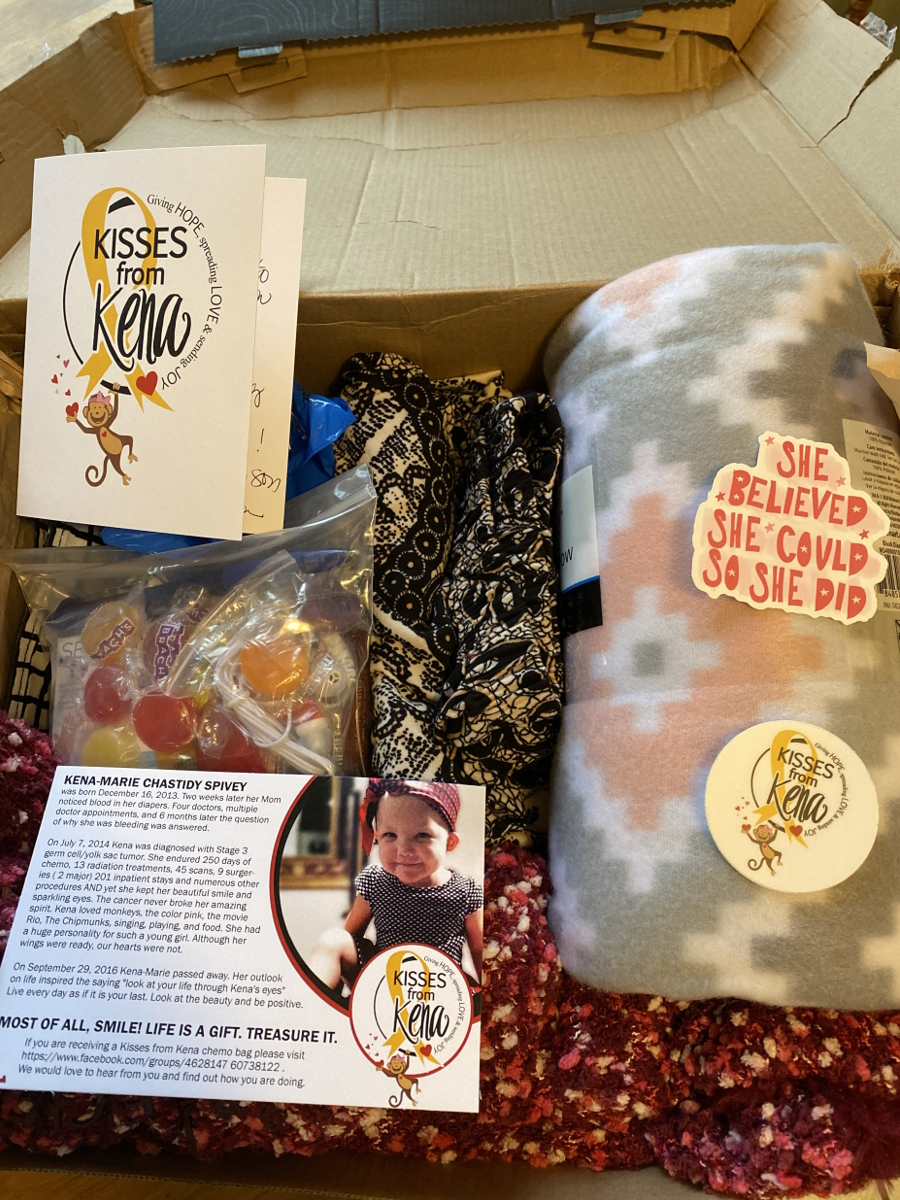
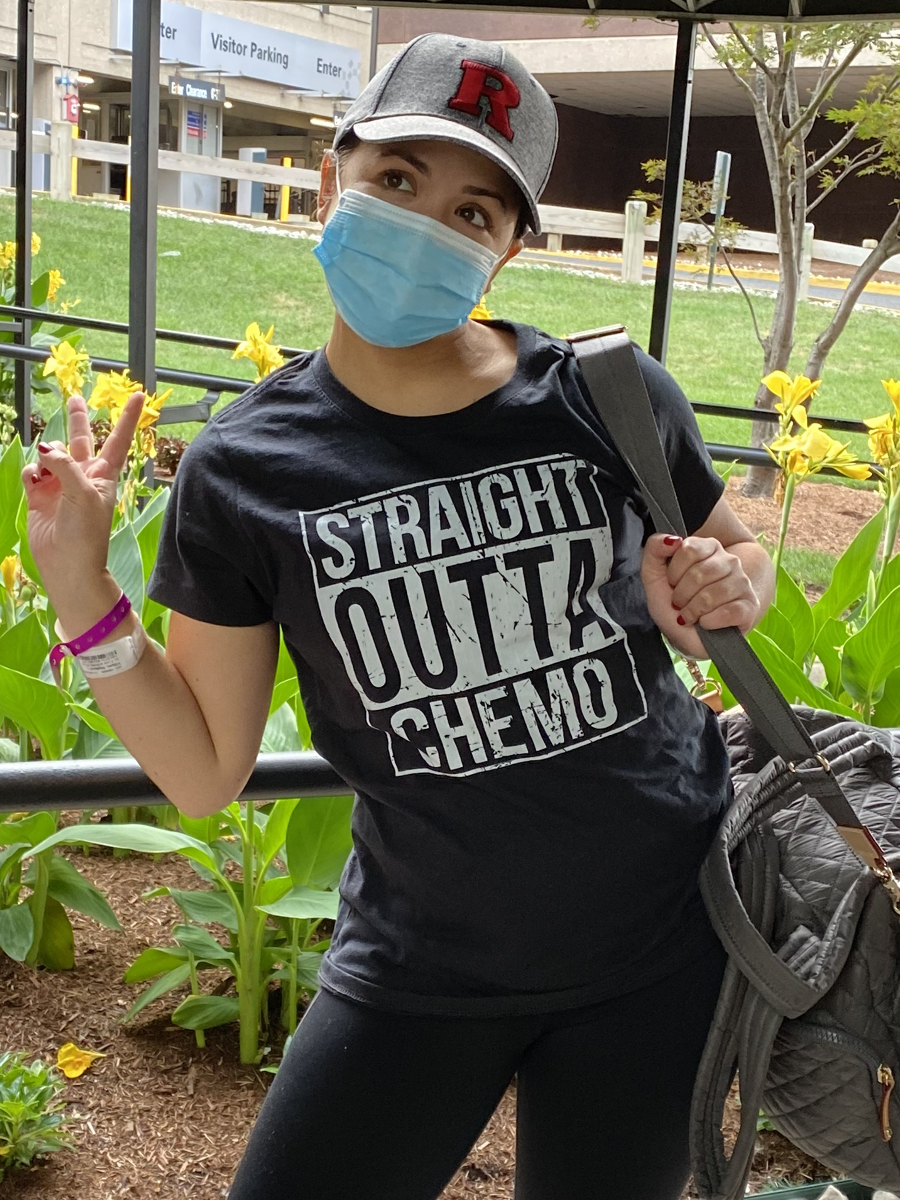
I did the egg retrieval on a Thursday. That Friday, I did my first round of immunotherapy and rolled right into chemo.
I first started the chemo treatments end of July. I did R-EPOCH.
Side effects of chemotherapy & what helped alleviate them
I, fortunately, did not have many side effects. I was nervous because when I learned what R-EPOCH entailed, which was 96 hours in the hospital every round, that was not what I was expecting. I was expecting a couple [of] hours once a week outpatient, just like my dad had all these months or years.
Digestive issues, yes, but I always have digestive issues anyway. I did have shots that I had to take at night after each treatment cycle for about five or seven days to boost my white blood cell count. Those give you achy bones literally. That’s pain that you don’t know exists until it actually happens.
I would remind myself that the pain I’m feeling is my body producing white blood cells so I would just try to imagine that and cope with it. I would find going for walks helpful because when you do sit for too long, that’s when the aching really did come.
When I was in the hospital, I would walk because I can. Most people in the oncology unit cannot walk so I said, “You got to get up because no one else can and you have absolutely no excuse.”
I think I would do like three miles a day around the unit. I would walk anywhere that had space and anywhere that I could. That was basically the most helpful thing to do because otherwise, you’re just sitting in a hospital bed. Sometimes you have a roommate and you’re hearing their pain so walking was what I had to do.

I was exercising here and there. Still tried to do Pilates [and] yoga when I could. If I don’t work out X amount of times a week, that’s mentally not good for me.
I also did it because of the weight fluctuations that you experience with treatment. That was hard especially that first round because I was coming off IVF drugs and I got bigger because they pump so fluids in you to protect you from all the drugs that you’re getting.
At the time, going through the whole process of freezing my eggs was a huge inconvenience to me because I just wanted to get better… I had a bigger fish to fry in a way.

Fertility preservation prior to cancer treatment
We wanted to do family planning. She knew I was getting married and she made it seem more important to me than I think I really realized. She explained that the drugs we’d probably go with could impact my fertility, but it’s not guaranteed. She felt that it would be important for me to take the time and do that.
Sometimes patients don’t have that time. She did say, “You do have time. I will give you time to do it. We think it’s probably best to do so.”
At the time, going through the whole process of freezing my eggs was a huge inconvenience to me because I just wanted to get better and then have a wedding. I knew every day counted because my hair, whatever it was going to be, needed to grow. I said, “The faster I’m done, the faster it will grow.”
I went to the first doctor that she recommended. They do egg retrieval in the office and although it is local anesthesia, they weren’t comfortable with where my mass was with being able to breathe properly. They didn’t think they had the proper facility to do that procedure for me.
She confirmed that I should go to a doctor at Cornell in Manhattan because they do the procedure in a hospital. I went to that appointment [and] then found out that their labs were closed for a full week so I had to delay the process. But once we started with the shots and everything, it was a quick 10 days.



Family planning decisions with your fiancé
That part of the journey is a bit of a blur. We knew about lymphoma. We knew how to do cancer. We didn’t know about this.
This was something that we did together because my mom’s said, “Oh, I’ll handle the cancer part. This is your family.”
We knew we were going to do it, especially after the strong recommendation from my oncologist. One thing we did discuss was eggs versus embryos. That will be one of the first questions that you’re probably asked.
Freezing your own eggs is the first step of IVF if I am explaining it correctly, where you’re producing as many eggs as possible to retrieve all in one.
With the embryos, that’s when you mix in the sperm that you could freeze as well. I believe there are some benefits to freezing embryos. I think there’s a higher success rate.
We discussed it and decided that just freezing the eggs was what we wanted to do at the time. There was some extra time needed in order to do embryo freezing. But just in case anything were to also go wrong in our relationship or anything like that, these are my eggs.
Because we weren’t married yet, even though we were about to be, these are mine. He said, “Absolutely. This is the decision that we want to go with.”

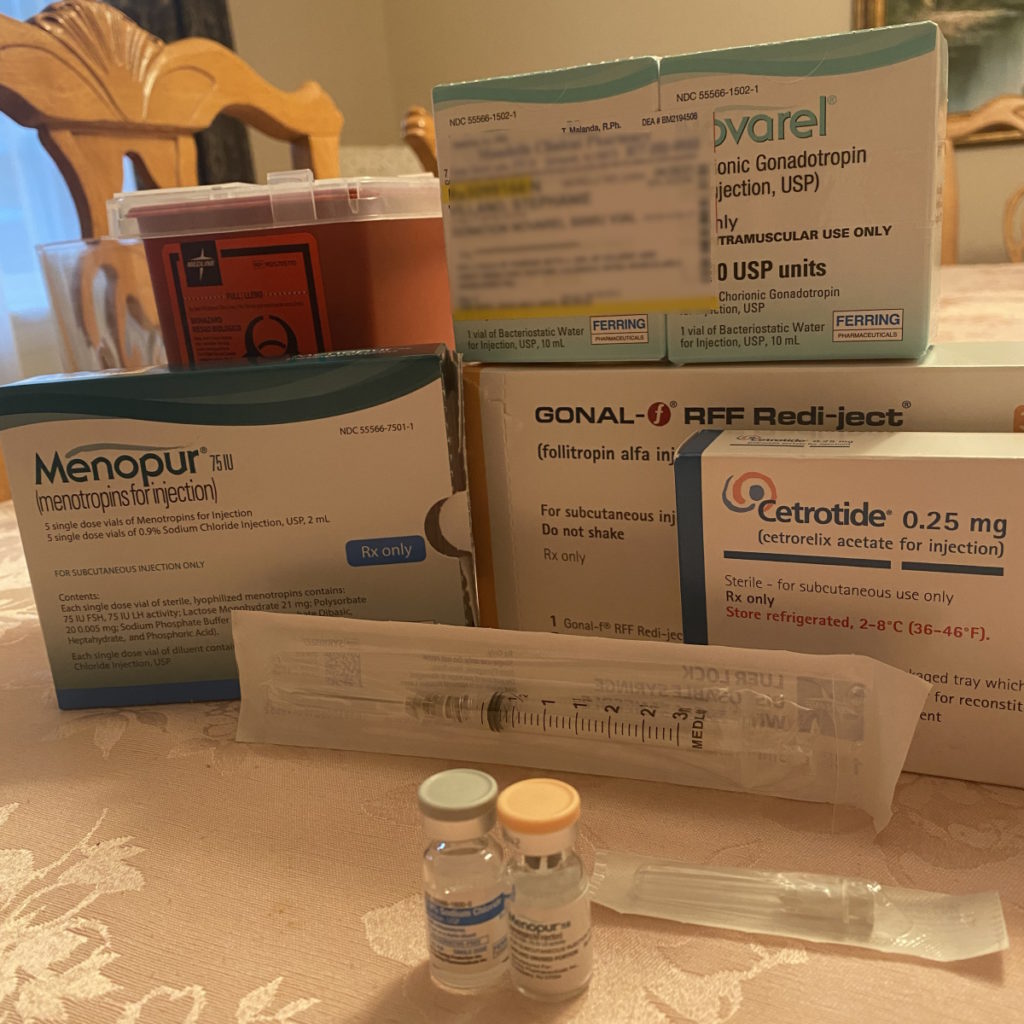
Process of freezing eggs
The hardest part for me was the last couple of years. I know that I was in a very different circumstance than most people and I fully recognize that, too. I saw this as somewhat of an inconvenience because I had a bigger fish to fry in a way.
But looking back, it’s completely different because you don’t know what’s going on in that next stage. Because I have to go to two doctors and [the] time that it took to get through all those appointments, that was more of the inconvenience for me.
The whole process is very, very difficult. You become a nurse for yourself immediately.
I’m very fortunate [that] I was a beneficiary of programs that help with paying for those medications. But if you’re doing that because you want to start a family and you’re not a cancer patient, I cannot imagine how people pay for multiple cycles.
The stress of keeping your needles clean and becoming a nurse overnight is absolutely insane. Learning the exact dosages and getting everything in order is crazy. Then administering the shots.
I’m someone who doesn’t mind needles, but I couldn’t give myself the shot. I was living at my parents’ house at the time. We bought a house in the same town so my fiancé was living in the house and he would come over every night for dinner.
After dinner, [he] and my mom would rock-paper-scissors for who’s going to give me my shots. I would mix them.
My mom was used to giving needles because she had given my dad white blood cell count boosters a few years ago. But that was in his arms; we were doing it in my belly.
James — and he would say this, too — was a little bit more, I don’t know, reckless. I would always bleed after he would give me the shots. One shot, Menopur I think, burns so badly.
Getting stuck every single day and then drawing blood in the morning, I was getting tired and I would cry. I would try to hide my crying, lying down on the couch. That Menopur shot would just send you over.
They knew they had to stick me two more times that night; that’s what was hard. You don’t want to do that to somebody. I was crying because I [didn’t] want them to feel bad, but they [did] because they’re inflicting pain on me.
In hindsight, probably the best thing that we could have done to ensure, hopefully, a family going forward whether we have to use them or not. It’s good to know that we had them.


Taking care of your mental health
I’m in the suburbs of New Jersey. I have to go to my morning monitoring in Manhattan at 6 o’clock in the morning. A lot of mental work there.
I just had the mentality, “This is what you have to do. While it’s not the cure for what you’re actually sick with, you have to do it because this is your future.”
At that time, I had gone back to work basically after I was admitted and had my initial diagnosis. I was off a week or two to start the whole cancer process, but then I did go back to work for a few weeks before I officially started treatment.
I was just in a mode at that point: morning monitoring, back to my house, work, dinner, shots. I kept that routine pretty consistent and just added doctor’s appointments. That helped me keep focus and remain distracted from these bigger things that [were] happening. That’s just how my brain is wired.
I did work through all of my treatments. When I wasn’t in the hospital, I came home for a couple of days and took some rest but then I did work when I could work. That’s a testament to the company and the team that I work on. They were very understanding.
They allowed me to have that mental space, too. I don’t think I took on anything brand new during that time, but they allowed me to keep the things that were important to me, which was very helpful.



Planning a wedding & getting married
I should have gotten married originally [in] April 2021. We moved it because of the pandemic. Then when I was diagnosed, obviously to me, that was the last thing I needed. I said, “We will see what happens.”
My oncologist said my treatment plan was six cycles. She said after three, she would expect remission. Up until that halfway point, I didn’t think about the wedding very much, other than my hair. I was said, “We’re not talking about it.”
At this point, it’s not really happening, but we haven’t canceled anything. We did tell our vendors, “We’re dealing with this. We’re not talking about anything else,” and they were all very understanding. I don’t think they looked for payment. Good people out there.
After the midway point, I had my PET scan and the oncologist told me that I was in complete remission. I still had three cycles left. That’s when the wedding planning came.
Ironically, after that scan, I started to get more [anxious] because we’ve been in this bubble the last few months of, “We don’t have to worry about anything other than me literally surviving.”
I had that routine: wake up, work, maybe have a doctor’s appointment, have dinner, [and] go to sleep. That was the routine. I go to the hospital [if I] have treatment. That was it.


My doctor said, “You can start to plan. I’m comfortable with you moving forward with your wedding.” I said, “It’s in April.” She said, “Yes, that’s fine. You should be good.” I said, “We’re inviting more than 200 people.” She says, “That should be fine.” She gave us the okay. That’s when it all started to sink in.
One night, I just could not sleep. I was naive for a while with the hair because I had a few nurses tell me they had seen some patients not lose all of it so I hadn’t shaved my head or even cut it at that point. I just basically looked like Gollum from Lord of the Rings. It was bad. I should have cut it a lot earlier.
But that was an area where they knew I could joke about my hair, but no one else could. I know my mom and sister were definitely texting each other, being like, “She still hasn’t cut it.” That’s fine. Talk about it between them.
I thought, “I don’t think I’m really going to have a lot of hair,” because I was imagining maybe a Charlize Theron little bob-pixie thing going on.
I was constantly Googling “stages of hair growth after chemo.” I wanted a month-by-month playbook of it. Not many pictures out there to give you what you could look like. Obviously, everyone’s hair is different. Constant Googling of “how fast you can grow your hair safely.”
One night, I could not go to sleep. I tried some of the anti-anxiety medications that they sent me home with and that didn’t help. I think it made me worse.



I just remember texting my fiancé, saying, “Today is not a good day.” It was probably the only bad day I really had. He works in finance as well; very market-sensitive job. He asked, “Do you want me to just come over and sit with you?” I said, “No, no, there’s nothing to do.”
I thought,“Okay, life is going to start again and it’s going to be fast because I’m going to be done in November, God-willing, and if all looks good, I’m going to get married in April.” It was like the freight train was just pushing past anything that was blockading it and we were full steam ahead.
I think April was the true finish line in that sense. Technically, May, when I sat down on the beach in Turks and Caicos for my honeymoon. The wedding was the end in sight.
Follow-up protocol after cancer treatment
[I got] my results right before Christmas. I had so [much] vacation time left over for the year that I basically took off most of December, which I never do.
My fiancé and I got massages that day. We had brunch then he came with me and we thought, “It’s either going to be a good Christmas or a bad Christmas,” but it was a good one.


We were used to every three months checkups for my dad, but she said, “I don’t want to see you until June and you’re going to be married.”
I wasn’t sure if she did that because three months would be around March if I were to do that and maybe she didn’t want to ruin anything.
Now, my checkups are every six months. I don’t even do PET scans anymore. I just do CT scans. So to me, she’s not as worried about anything because you don’t have to do the more detailed scans.
Everything so far [is at] complete remission. That’s where I think I have scanxiety and mostly because of what we’re finding more now afterward.



Getting diagnosed with Chiari malformation
I was getting migraines and they definitely were more pronounced after chemo. I thought that was because [I was] coming off a lot of bad, bad drugs. I noticed they were tension headaches. There were certain situations where I would get them.
My sister did remind me that I did get these headaches and tension headaches before I was sick, too. The night I got engaged, I had a terrible migraine. My head was throbbing.
I was sensitive to light as well. If it’s a beautiful, sunny day and I’m outside, throw in a high noon hard seltzer or something like that [and] I’ll get a migraine. I can only have maybe a couple of sips and I’ll get a massive migraine.
I did mention that to my oncologist. In that June scan, I was clear of cancer, good on that front, but she did mention that I had something called Chiari malformation, which is something that could cause the headaches that I was getting.


She recommended [for] me to go to a neurologist, which has been something that I’ve been on a new journey with learning a new topic and health area itself.
Many people can have it. You might not have any symptoms, but I’m pretty asymptomatic, given how severe it has become where it’s caused some issues. It’s caused the syrinx in my spinal cord.
Something that you look back and say, “Yes, I had cancer, but if I didn’t have cancer, I would have never probably mentioned my migraines or tension headaches or I thought they were really normal.”
People tell you, “You’re a woman between the ages of 25 and 50,” which is a very broad age range by the way, “so it’s pretty common for you to have migraines.” You just named half the population so we’re all supposed to have migraines? If I had stuck with that, I’d probably have not gotten the surgery because I’d say, “Oh, I’m just a woman who gets migraines.”


Words of advice
Be very detailed with what you’re experiencing. I went to the doctor for my yearly checkups until I was 28 years old. Now, I try not to overdiagnose myself, but I’m realizing I think I’m onto something when I have some of these issues.
Keep a notebook of every appointment [and] everything you discuss. I learned that from my mom. She has my dad’s whole medical life written in a notebook. We started my own notebook when we got into this whole mess.
Know your baselines. I learned that my temperature is in the high 97°F so if I get to 99°F, that’s off. I’ve also known my resting heartbeat. When it’s low, it might be because I’m on steroids and that’s what makes it super low. Then when I come off those and when I come out of surgeries, I run really high but I’m getting enough oxygen.
No matter how specific it might sound, start to log certain things you’re experiencing, like hand tingling. That’s definitely something that comes up with a lot of these drugs, neuropathy.
That’s something that I knew from my dad. He sort of has permanent neuropathy [whereas] mine was expected to be temporary, which it was. With my Chiari, the hand tingling is also a symptom so I don’t know where it came from, really.


That notebook is, for lack of a better term, your Bible. That’s your journal and that’s where you also can hold your medical team accountable.
In my IVF journey, someone dropped a term. They said, “Oh, by the way, did you know this?” I said, “No, I didn’t,” so I wrote it down.
The doctor said, “Not something you need to address today, but maybe something that you might want to address in the future or know about.” I wrote it down and that’s something that I need to go back and address as well.
Write down terms that you know and terms that you don’t know then research them. There is harm [with] over-researching, of course, as we all know. You go down the rabbit hole.
I read my scans and reports afterward. I’m lucky enough [that] I have a radiologist in the family. I could text her at any point and say, “What is this? What is that?”
Utilize the resources that you have or the people around you because, unfortunately, everybody has an experience with cancer. I’m not the first and I’m, unfortunately, not going to be the last. Everybody has an experience or a trick or something to do. I knew walking was my thing for treatments and staying whole [at] that point.



Family conversations about cancer
[In] my first round of chemo, I was in the same hospital room that he was in and I walked the same hallways. I actually have a picture of him walking with my mom and I was walking behind him. Then, two years later, I’m walking those same hallways. I had some of the same nurses as he did.
When he first got sick, I listened to Bob Marley’s Three Little Birds. “Don’t worry about a thing. Everything’s going to be all right.” My mom is from Jamaica so it’s special to us.
I would listen to that song every single morning when he first got sick and I never told anybody. He would also listen to that song when he was in the hospital for his stem cell transplant. [For] three weeks, he would listen to that song every day as well.
That was our father-daughter dance. It all says it in the song. “Everything’s going to be all right,” whatever it is. We both know that.


There’s probably a lot we could say to each other, but I don’t think we need to because we both just know. It’s not a great world to be around, but I think there’s a lot of beauty that comes out of it with the people that you meet [and] other experiences that you see.
We know that we are healthy. The other people that we see in that unit are sick people. We are very fortunate. I don’t think that goes unnoticed either where we were able to control what we could, whereas we know there [are] a lot of situations out there where you can’t. I think that goes unsaid as well, but we both know it.
For anybody who’s going through anything, whether it’s cancer or seeing an individual go through it, there are definitely dark times but after every storm, the sun does come out and shine. Trying to keep your head up in those times is helpful, no matter how hard it is.



Inspired by Stephanie's story?
Share your story, too!
PMBCL Patient Stories
Lauren D., Primary Mediastinal (PMBCL)
Symptoms: Dry cough, extreme fatigue, trouble breathing, swollen and discolored left arm, lump under the arm
Treatment: Chemotherapy
Daniella S., Primary Mediastinal B-Cell Lymphoma (PMBCL), Stage 2
Symptoms: Prolonged cough; low-grade fever; night sweats
Treatments: Chemotherapy (R-EPOCH), radiation, CAR T-cell therapy
Stephanie V., Primary Mediastinal (PMBCL), Stage 4
Symptoms: Asthma/allergy-like symptoms, lungs felt itchy, shortness of breath, persistent coughing
Treatments: Pigtail catheter for pleural drainage, video-assisted thoracoscopic surgery (VATS), R-EPOCH chemotherapy (6 cycles)
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.


