Cindy’s WM Non-Hodgkin’s Lymphoma Story
Cindy was diagnosed with Waldenstrom Macroglobulinemia, a subtype of non-Hodgkin’s lymphoma, right before her 50th birthday. She shares her full story below, including undergoing 6 rounds of chemo, cancer’s impact on relationships, and managing anxiety throughout the experience.

- Name: Cindy S.
- Diagnosis (DX):
- Waldenstrom Macroglobulinemia
- Subtype of non-Hodgkin lymphoma
- Staging: N/A
- Age at DX: 49 years old
- 1st Symptoms:
- Hyperproteinemia (high blood protein)
- Treatment:
- Chemotherapy
- Bendeka and Rituxan
- Infusions for 2 days every 4 weeks
- Total of 6 rounds (6 months)
- Chemotherapy
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

I’ve just had to tell myself that the remnants of chemo can linger. My body has had to adjust.
I have to give myself grace when I’m feeling tired or weak.
If I take it one step at a time and slowly get back to my workouts and eating habits, that’s fine.
Cindy S.
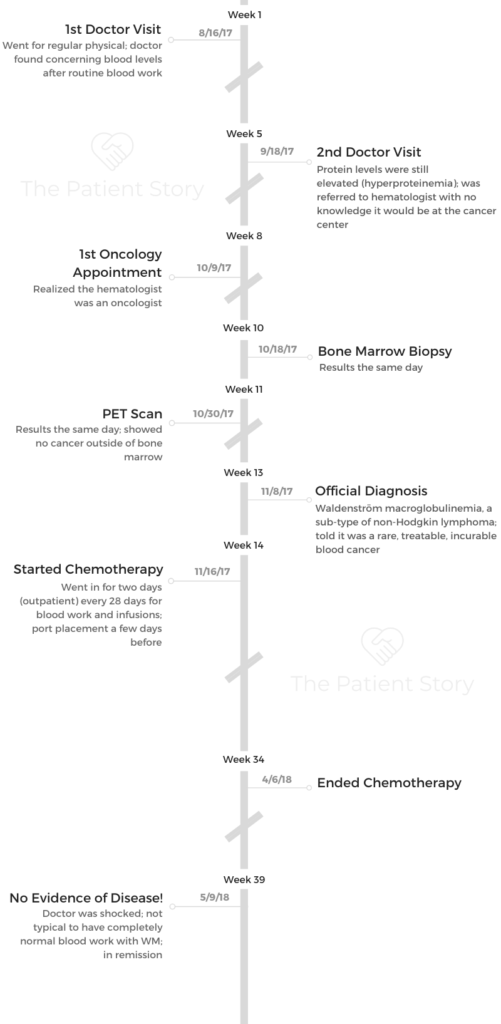
Diagnosis
What happened when you went to the doctor the first time?
I went in for a normal physical. I try to go yearly. They did routine blood work, and my total blood protein count was high.
I went back 5 weeks later, and it was still high, so they sent me to a hematologist. I looked up the hematologist and found out he was an oncologist.
They did more in-depth blood tests. They took 8 vials of blood. He told me they were looking at multiple myeloma because of the blood results. They wanted to do a bone marrow biopsy because of that.
Describe the bone marrow biopsy
It was interesting. It hurts. They did it in the office. I didn’t have to go to the hospital or anything. They numb the area near your tailbone in your spine.
I had to lay really still because they didn’t want to tap into the wrong thing. They do numb the area, but it is painful. They have to go into the bone, so it’s similar to a drill.
They break into your skin, and the tool they use goes down into your bone, so you can feel the pressure as they go deep into your bone to get the marrow.
They had to do mine 3 times. He couldn’t get deep enough in to pull out a good sample, but on the third time, it finally was enough to run tests on it. They still sent the sample off, but they ran a preliminary test right there in the office. It was positive for whatever they were testing for.
The big takeaway from the bone marrow biopsy is that it’s definitely painful, but it’s manageable. You can feel them pressing into your bone, but it’s mostly just pressure in the tailbone area. Yes, it’s numbed, but the pressure was pretty intense.
PET scan
I did a PET scan after the biopsy, and it came back completely clear. They sent everything off for the bone marrow.
The PET scan was looking for other cancerous cells in my lymph nodes, and there was nothing.
From what I understand of Waldenstrom, it can turn into tumors later, but it’s really more of a blood cancer. My body was just producing way too many white blood cells.
Later on, if it keeps recurring, they’ll probably do more PET scans, but they didn’t see any need to continue those.
The PET scan being clear was great news, but at the same time, the biopsy results came back from the bone marrow, and that’s when they said it was Waldenstrom macroglobulinemia.
It was great that I didn’t have any tumors or anything, but whatever level they tested was supposed to be under 300 or so, and mine were 4,000 or so.
They were very concerned about how high my numbers were. I didn’t have any symptoms, but they were still concerned. My oncologist wanted to immediately start treatments because if we didn’t, I was going to continue making too many abnormal white blood cells and overcrowd all the good cells. In order to get my blood corrected, it was going to take chemotherapy.

Processing the cancer diagnosis
It was surreal. I didn’t feel like it was happening to me. I got hit with it out of the blue.
I had been tired a lot and experiencing a lot of fatigue, but that was it. I didn’t feel sick, so it was shocking.
I was upset. I will say, I have a really strong faith in God, so I knew to stop looking stuff up on the internet and just trust. I knew I was going to read stuff that was way worse than reality anyway.
I knew I could start to fret and think about the negative. I could start worrying and wondering about what I did to cause it. I had a choice. I could do that, or I could stay positive.
I’m an optimistic person, anyway. I knew if I started dwelling on the negative, that was going to make it worse.
I believe a lot of it is mindset. If you think on the negative, the more you’ll get, and the same for positivity. Even though I was taken aback, I tried to stay positive and speak that positive out there.
I drew on my faith. I prayed about it. I had people around me stand in agreement with me that I was going to be okay.
How did you break the news to loved ones?
My husband was going through all the testing and stuff with me. We had looked things up online. I had looked into Waldenstrom and multiple myeloma. We were worried.
We weren’t married yet. We were just dating. Here we were in this new, wonderful relationship, and in walks cancer. He was there the day I got diagnosed. The doctor broke it to him, I guess.
I had to tell my mom. That was hard. It’s hard to look at your mother and say you have cancer.
I wasn’t about to call her on the phone and tell her. I went to her house. She knew something was wrong because of that. Not that I don’t go see her, but it was an out-of-the-blue visit, and she knew I had been going to the doctor.
She took it pretty well, all things considered. She took my positivity about it and ran with it. I just told her the game plan and said, “We’re just gonna go after it and see what happens.” She asked all kinds of questions, of course, but took it well.
After I told my mom, I told other family and friends. My mom told some people for me. Everybody had known I was going in to the doctor, so everyone wanted to know the results.

Chemotherapy
What was the port placement like?
It was outpatient. The whole day took about 8 hours. I’m not sure how long the procedure was, but probably about an hour. I was under when they put it in. The only thing is you end up having a big circle under your skin.
It didn’t hurt. I didn’t really know it was there except for being able to see it. It wasn’t sore after surgery.
I didn’t notice any feeling of it being there until the next day. It never really hurt, but I knew it was there.
At first, I couldn’t get the bandages wet. They put a plastic protective cover over it. I’m assuming they do that with everyone unless you’re allergic to the material or something.
Every time they would access it, they would put a new cover over it when they were done. I didn’t really have to do anything special to take care of it.

What was your chemo regimen?
I was on Bendeka and Rituxan. I would go every 28 days for 2 days at a time, and I did that for 6 months.
It was all outpatient in the cancer center. The first day, they did Bendeka and Rituxan. I also had Benadryl, Tylenol, Ativan, steroids and anti-nausea medicine.
The first day took 6-8 hours. The second day I just got Bendeka.
I had an allergic reaction to the Rituxan about 30 minutes into the first infusion.
She told me if I started getting itchy, thirsty or found it hard to breathe, I needed to say something. Well, I started to get super thirsty.
They did some sort of check, and she saw that I was having a reaction. It can swell your throat, so if you don’t tell them, it can close your airway.
That’s why I got the Benadryl the first day. They stopped the Rituxan for a little bit. Then I got Benadryl, and they started the Rituxan back again even more slowly.
What side effects did you experience?
I asked about hair loss, but I didn’t lose my hair. That was nice. I didn’t mean to be vain. I just wanted to know because I wanted to be prepared for it. My doctor said that my particular cocktail wouldn’t cause hair loss.
I never got sick to where I puked or anything like that, but I slept a lot. The steroid made me really hungry. Had they not given me the steroid, I probably wouldn’t have eaten anything because I was a little queasy and really tired all the time.
I was weak. At times, I would get lightheaded. If I would try to do too much, I’d have to go lie down. I was fatigued before chemo because of the cancer, but at the time of infusions and a few days after, I was especially exhausted.
I would always get infusions on Thursdays and Fridays, so I would take the weekend to recuperate, and I’d be back at work on Monday morning. I wasn’t always super productive on Mondays, but I was at work.
I’m used to doing an exercise routine. I was fit and healthy, or I thought I was. I’m used to being able to get out, work out, do yard work, and all that stopped.
As time went on, it didn’t hit me as hard. I think that’s because the chemo was working and fighting the cancer. I never felt 100%. I was still tired all the time.
During the last 2 months, I started feeling more like myself. It took me a while to get back to really feeling like myself, though.
»MORE: Cancer patients share their treatment side effects
What got you through chemo?
I just kept going. I just kept doing. Part of that is just who I am. That helped me. God gave me enough distractions like staying positive, going to work, planning a wedding, and the holidays that I was able to just put one foot in front of the other.
I didn’t ignore it if I felt like I needed to lie down for a while, but for the majority of it, I just kind of kept taking care of business.
What advice do you have for someone who is about to go through chemo?
Stay positive. Seriously. That is much easier said than done. People are going to be like, “Really? Stay positive?”
It’s hard, I know. They’re giving you all these drugs and your body is changing, but just take care of yourself the best that you can.
If your body says rest, you just rest. You’re not going to be able to do all the things. Have the right mindset through that even though things are changing.
Your mind wants to say, “Great, now you can’t do anything like you used to anymore.” You can’t, but you can. You just have to find the balance.
Hopefully, you’re surrounded by people who are going to support you and pick up the slack. If you’re like me and don’t like to delegate, do it anyway.
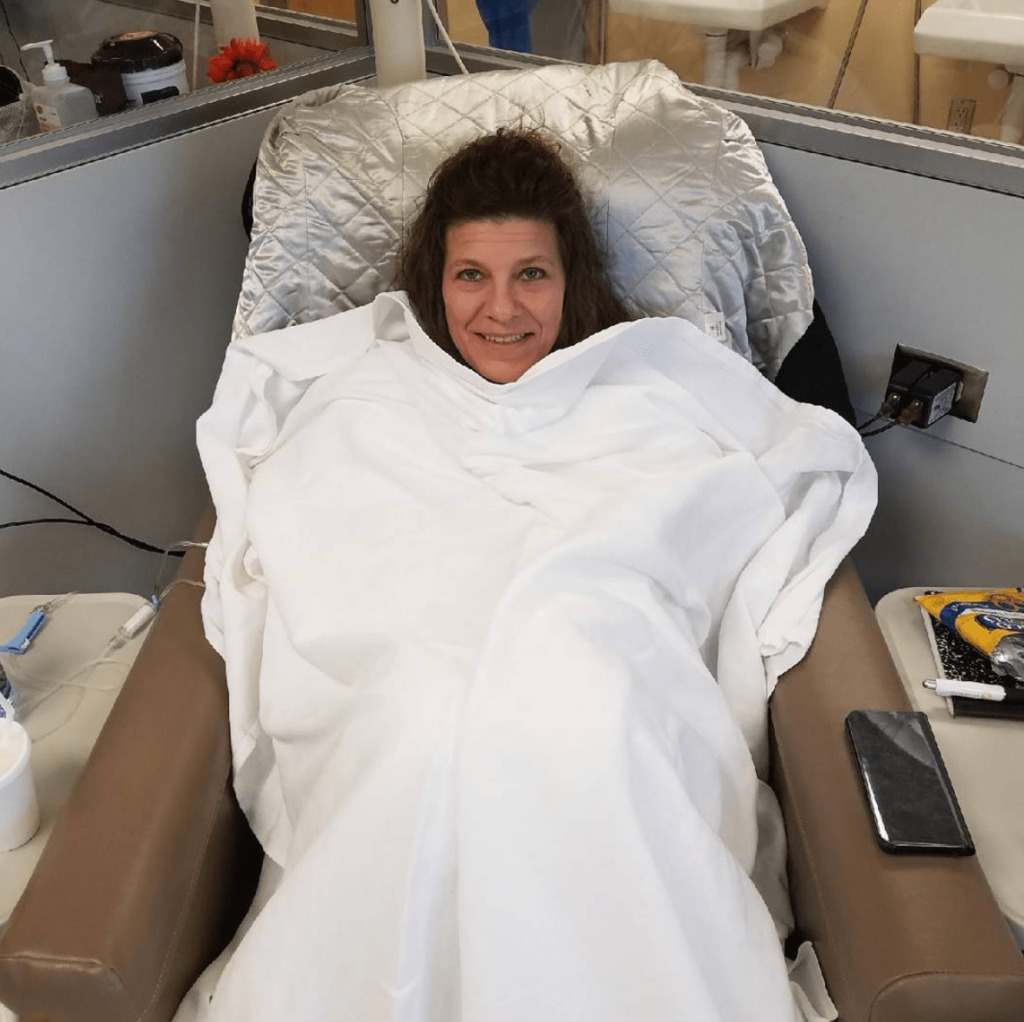
You went into remission
I felt great. We watched all my blood work and my levels the whole 6 months. Every time I went in for chemo, my levels were dropping. We checked them every time I went in.
When I went in for my April appointment, my IgM levels had dropped from 4,600 or so to about 400, which was fantastic. Most all of my blood work looked good.
I felt good. I wasn’t 100%, but I felt better than I had. When we did blood work again in May, my IgM levels were completely normal. All of my blood work was normal.
I went from the initial diagnosis, through chemo, to no signs of cancer at all. It was gone. My oncologist didn’t know what to say. He said I was in remission. That’s all he could say. He was surprised.
Everything has stayed fine since. I’m going back every 3 months, and every time, it’s great news. It’s fantastic. It’s kind of mind blowing. We’re switching to every 6 months now.
With Waldenstrom, you can go into remission for years. It’s a slow-growing cancer. Usually, though, there’s something residual, but I don’t have that.

Support & Emotions
What can loved ones do to show their support?
Don’t go overboard or be overbearing, but figure out what you can do. Whether that’s cleaning their house, cooking dinner or something like that, figure it out and do it.
People in our church did a food train for us. That was nice. A couple of times a week, they’d bring food. You’re worrying about everything else, so not having to worry about cooking or going out is helpful.
When people ask you what you need, that’s so much better than just saying, ‘Oh no, I’m so sorry.’ That’s sweet. I know they’re sorry, though. I’m sorry, too. It’s more helpful to say, ‘What do you need?’
It’s hard for me and people like me to say, “Yeah, you know what, I need a meal brought over,” but when someone’s offering their support, it’s nice.
You can offer to go to appointments if their primary caregiver can’t make it to one. Let them know that you’re there to help with the little things, even if that’s just coming to sit with them, pray with them, clean or anything like that.
How important is it to have a support system?
If I had to pick one thing that helped me stay positive throughout the whole thing, it would be having my church family stand with me.
They spoke life, and they prayed. Any time we went to church or someone from our church family came to visit, it was always positive.
They never questioned what might happen. They would hug me and tell me that they believed I was going to be healed. I knew I was.
My pastor’s wife was especially amazing. When I wanted to quit or when I was feeling down, she would say, “No matter what, speak life anyway.” With faith, you’re going to have to believe in what you can’t see.
My treatments all went well, and I firmly believe that faith did that for me. I understand that some people don’t believe that way.
I’m not here to change how somebody believes, but even for those people, it still comes down to your mindset.
»MORE: What kind of support cancer patients say helped the most

Anxiety about recurrence
I’ll admit I do have my fears. I don’t think about it until it starts getting closer to my appointments. When I start getting closer to those anniversaries of when everything started, it starts to get to me a little.
There’s a little anxiety there when I go in for blood work. There’s always the possibility that it won’t be normal when you go in to get it checked.
I really have to stop myself when I start thinking those ways. I’ll worry myself if I don’t keep it in check. I can’t say it’s not there, but I remain positive.
How did cancer affect your relationship?
It brought us closer. There were times it was really hard, but it brought us closer. He was fantastic. He supported me, he loved me, and he helped keep me up when I started to feel down. He would reassure me that I was going to live and not die.
He is a recovery advocate. He helps people in their recovery process. He’s a coach by trade, so he was very motivating and upbeat. He was so great.
We had to rely on God and rely on each other. We had to keep each other positive. There were times I would catch him reading something or upset by something, and I would support him, too.
It went both ways, and that brought us together. He was always at my appointments. He was there every step of the way. The whole thing solidified our relationship.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer

Did you get involved in a cancer community?
Not as deeply as I wanted to. I did join a Waldenstrom group on Facebook. I would read some of it, but I tried to stay away from reading about it.
I didn’t put myself in a bubble, but I did block myself from reading a lot about it because I believed God was taking care of it, and I didn’t really need to obsess about it.
I did like to get in that group every now and then, though. If people had questions I could answer, I would. If it got negative, I would try to speak positivity to them.

There isn’t really anything for me locally because it’s a more rare type of cancer. That’s why I’d like to start something.
I don’t know how that would look necessarily, but I’d like to help other people who were in my position.
Cancer’s “new normal”
I’ve just had to tell myself that the remnants of chemo can linger. My body has had to adjust. I have to give myself grace when I’m feeling tired or weak.
If I take it one step at a time and slowly get back to my workouts and eating habits, that’s fine.
I just listen to my body and do what I can each day. I’m trying to get back on my clean eating. I do more of a morning routine than I used to.
I’m not a morning person. I try to get up and read. I take time for me before I have to rush off to work.
I look at life differently. I always had a positive outlook on life anyways, but life is more about what’s important to me and the things that matter.
You don’t ever know what’s going to happen, so we ought to live our lives doing the things we want to do and the things that bring us peace.
Instead of working toward retirement, I’m working on ways to do some of those things people usually save for retirement now, because I don’t know what later looks like for me.
Obviously, I have to put food on the table and work, but I’m shifting my focus to things that will make me happy, things that will help others, and things like that.
Paying for cancer treatments
I’ve struggled a bit financially. I was lucky to have insurance, but even still, that doesn’t cover everything. You still have to pay for regular life, and cancer adds on top of all that.
It’s a lot. I worked out a payment arrangement with the hospital. Most hospitals do payment plans.
I told them, “I can pay this much, and that’s what I’m doing.” There are programs and organizations you can use, but I didn’t reach out to any of them.
Advice for someone who has just been diagnosed
You’re going to grow through this. The idea is to grow in a positive way so that you can impact other people somehow. If you can focus on that positive, you can use this to help someone else.


Inspired by Cindy's story?
Share your story, too!
Waldenstrom Macroglobulinemia Stories
...
Pete D., Waldenstrom Macroglobulinemia
Symptom: Irregular blood test results during a regular workup for Crohn’s
Treatments: Chemotherapy, surgery, radiation, monthly IVIG
...
Sheree N., Waldenstrom Macroglobulinemia
Symptom: Feeling anemic
Treatment: Chemotherapy (bendamustine & rituximab)
...




2 replies on “Cindy’s WM Non-Hodgkin’s Lymphoma Story”
Hi, Cindy,
I am really inspired by your story and your positivity. My sister-in-law was just diagnosed with WM and will be going to Reno, NV for 3 weeks of treatment after already having 3 blood transfusions. They have 4 kids under the age of 10. I plan to help with caretaking for the children. But I am also wondering what you recommend in terms of positive reading materials you found to be helpful or raw/organic/vegan food items you enjoyed. I want to be as helpful as possible and like you said ask, “What can I do?” rather than say, “I’m sorry.” Better yet, I don’t even want to have to ask. I just want to know what is the most helpful thing for individuals going through this. Thank you so much for telling your story and being a resource. Congratulations on your remission and wishing you all the very best each and every day as you live each day fully and deeply.
Hi, Cindy,
I am really inspired by your story and your positivity. My sister-in-law was just diagnosed with WM and will be going to Reno, NV for 3 weeks of treatment after already having 3 blood transfusions. They have 4 kids under the age of 10. I plan to help with caretaking for the children. But I am also wondering what you recommend in terms of positive reading materials you found to be helpful or raw/organic/vegan food items you enjoyed. I want to be as helpful as possible and like you said ask, “What can I do?” rather than say, “I’m sorry.” Better yet, I don’t even want to have to ask. I just want to know what is the most helpful thing for individuals going through this. Thank you so much for telling your story and being a resource. Congratulations on your remission and wishing you all the very best each and every day as you live each day fully and deeply.