How Faith and Family Keep Jackson Going Amid Stage 4 Colon Cancer
When Jackson was diagnosed with stage 4 colon cancer with BRAF mutation at 27 years old, life flipped upside down in ways he never saw coming. A former college athlete, outdoorsman, Brazilian jiu-jitsu practitioner, and self-proclaimed extrovert, Jackson was the last person anyone expected to face a stage 4 cancer diagnosis. But looking back, the signs were there. He just didn’t realize how serious they were.
Interviewed by: Carly Knowlton
Edited by: Katrina Villareal
Jackson had been experiencing stomach issues and hemorrhoids for years, so even when he noticed thinning stool and blood, he brushed it off. That changed quickly when severe stomach pain and projectile vomiting landed him in the emergency room. Scans revealed a tumor in his colon and more than 40 tumors in his liver. Later, genetic testing confirmed that he had a rare BRAF mutation, present in only about 8% of colorectal cancer patients.

Understandably, the news hit hard. Jackson recalls the mental toll in those first few weeks, including the panic attacks, the anxiety, and the numbness. But what changed everything was a spiritual experience after reading Matthew 6:34 with his wife during a moment of deep fear and uncertainty. He describes feeling what he could only call a divine embrace, a peace that replaced panic, and a clarity that gave him purpose.
That spiritual moment became a turning point. Jackson began embracing each day without obsessing over the future. His mental health improved, his faith deepened, and his perspective on life transformed. He’s started a weekly Bible study, watched close friends get baptized, and even launched The 3929 Foundation to raise awareness, fund research, and provide financial assistance for those impacted by cancer.
While stage 4 colon cancer with BRAF mutation is a daunting diagnosis, Jackson hasn’t let it define him. He continues to work full-time, train, fish, and golf. He’s even recovered from colostomy reversal surgery and is eyeing a return to jiu-jitsu. Although he’s undergone intensive chemotherapy and faces ongoing tumors, including recent ones found on his peritoneal wall, he remains hopeful. His oncologists are amazed at his positive response to treatment, with nearly 90% of liver tumors now undetectable.
Through it all, Jackson advocates for others to listen to their bodies, get multiple medical opinions, and not hesitate to push for testing. He credits his wife, family, and faith for keeping him grounded. He’s not just surviving. He’s living fully, with a mission to educate, uplift, and inspire.
Watch Jackson’s video or read the transcript of his interview to find out more about his story:
- Why Jackson says being diagnosed with stage 4 colon cancer with BRAF mutation may have been the wake-up call he didn’t know he needed
- The emotional moment at his kitchen table that reshaped his entire outlook on life
- How his wife, family, and friends became his loudest advocates, and why that made all the difference
- The surprising reason he’s grateful to be the one facing cancer, not someone he loves
- What changed after Jackson focused on today instead of fearing tomorrow, including the Bible verse that grounded him
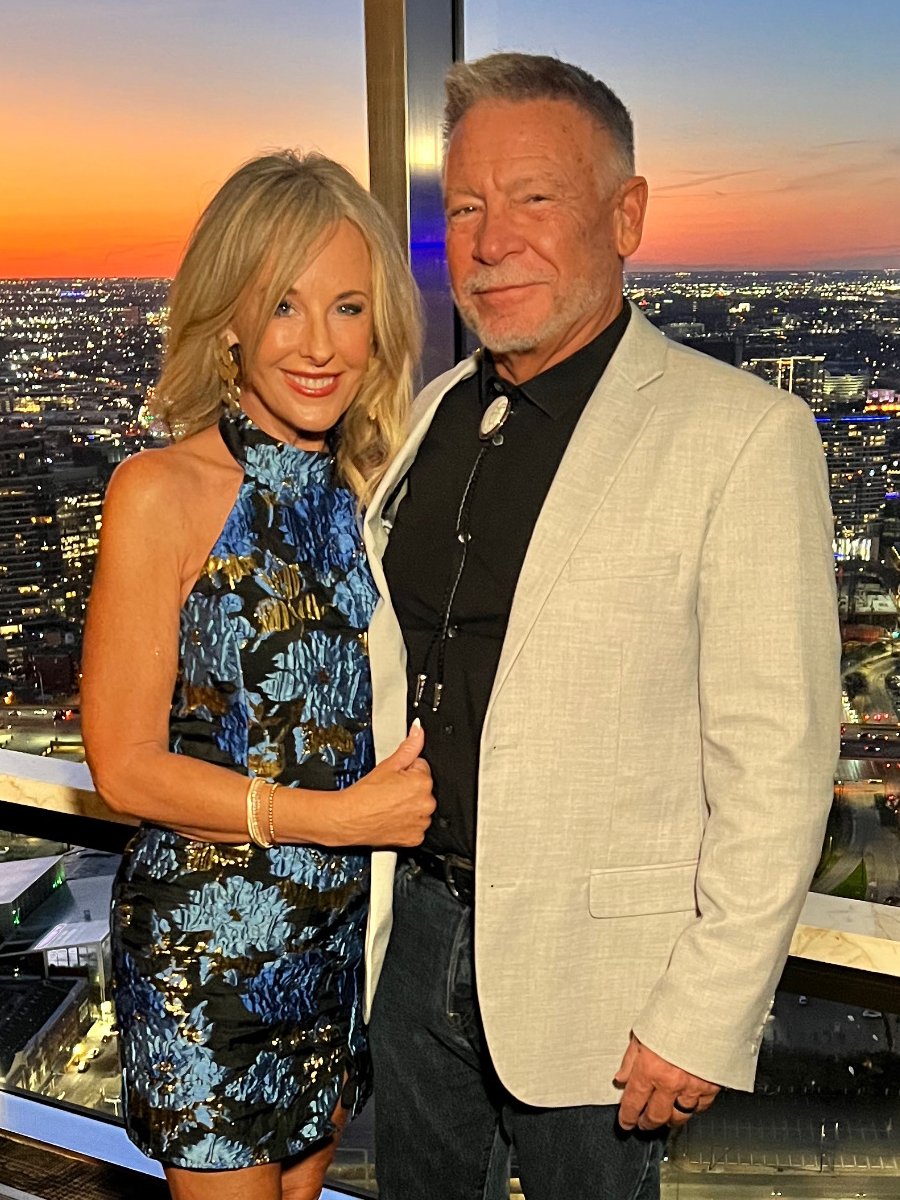
- Name: Jackson L.
- Age at Diagnosis:
- 27
- Diagnosis:
- Colon Cancer
- Staging:
- Stage 4
- Mutation:
- BRAF
- Symptoms:
- Severe stomach pain
- Fatigue
- Lack of motivation
- Anemia
- Blood in stool
- Thinning stool
- Treatments:
- Surgeries: emergency bowel obstruction surgery with temporary colostomy (to discuss the possibility of HIPEC in 2026)
- Chemotherapy
- Immunotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Hi, I’m Jackson
- When I first knew something was wrong
- I wanted a second opinion
- When I got the news “you have cancer”
- I had surgery right after I was diagnosed
- The plan moving forward
- I changed my diet
- How my diagnosis has impacted me mentally
- I had my colostomy bag removed
- The hardest part of my journey
- I grew in my faith
- How I’m supporting others with cancer
- I have a new outlook on life
- What I want others to know
Hi, I’m Jackson
I’m from Kansas City. I got diagnosed on January 11, 2025, at the age of 27.
I’m a big outdoors person, so I do a lot of hunting, fishing, and farm work at my farm. I love spending time with my wife. I’m also a purple belt and trained in Brazilian jiu-jitsu, so that’s something that I’m very passionate about as well. I love spending time with my family and our three animals.
My friends would describe me as very outgoing, talkative, and energetic. Hopefully, they’d say I’m selfless. I like to do things for other people.
When I first knew something was wrong
I ignored a lot of them as they came through. I’ve always had stomach issues for a very long time, all the way back to high school and through college. I was always told that it was acid reflux or GERD (gastroesophageal reflux disease), or that I’ve got IBS (irritable bowel syndrome) or something like that.
Over the course of 2024, I started to see my stool thinning and had blood in it, but I didn’t realize it at the time. I’ve always dealt with hemorrhoids for a long time, so I thought it was just that.
The crazy thing is that my sister is an oncology nurse, so I would talk to her about it, ask her, and send her pictures to know if that was okay. She didn’t think anything of it either because I was healthy, a college athlete, and ate right. We thought it was something with my stomach.
Then I started feeling very fatigued and lethargic throughout the year. I didn’t feel motivated to go to the gym when I used to go every single morning and train in jiu-jitsu at night. That started fading away a little bit.
I would say that would probably be the anemia, which I didn’t realize at the time. I was very pale and even when I would go to the lake every week with my parents and out in the sun, I still was not getting a tan or any color. When I had to go to the hospital, I was starting to get tired all the time and grumpy. I was starting to notice the blood in my stool and that’s when I started freaking out a little bit.
At about that time, within a week, I was in the hospital from extreme stomach pain and I was projectile vomiting. They told me I needed to get a scan and go to the ER, and that’s when they told me they saw what they thought was a tumor. I officially got diagnosed the day after that, when I got transferred to the University of Kansas Hospital.
We thought it was appendicitis or some infection. Never in a million years would I have thought it was stage 4 colon cancer. What was wild is that he walked out and said, “There’s a big tumor in your colon, and we found spots all over your liver.” When I officially got diagnosed at KU, they told me that I had stage 4 colon cancer. I had a complete bowel blockage, so I couldn’t go to the bathroom and had to get emergency surgery. They stopped counting after finding 40 tumors on my liver.
I wanted a second opinion
In March 2025, I got a second opinion at MD Anderson. I also have a rare mutation, the BRAF mutation, which is only in about 8% of colon cancer patients. I asked my oncologist and he said, “We’ll never be able to tell you how long you’ve had this or when you got it.” The interesting thing is, when I went to MD Anderson, I asked the oncologist there, and he and his team said that they would be shocked if I had it longer than a year.
They told me that in their opinion, they thought that it turned on and spread like wildfire within a year, which honestly would make sense to me because I started getting those symptoms, the fatigue and the actual blood in stool, within that year, so it would make sense to me that I’ve maybe only had it a year. But I thought that it couldn’t be out of the realm of possibility, with all the stomach issues I’ve had, that maybe I’ve had it for five to 10 years and then it slowly grew.
Education is probably one of the most important things. I feel like it’s one of my callings and the reason I’m going through this is to help bring awareness and raise awareness about the signs and symptoms of colon cancer. One of the most rewarding things that has happened is that since I got diagnosed was I probably have had over 50 people who I either know or who I have never met in my life from across the country reach out to me and told me that because of my story and everything that I’ve shared, they’ve gotten checked out and have gotten colonoscopies or gotten them scheduled or gotten tests.
There was a kid a few years younger than me who I knew from high school, and he messaged me and said, “I know you don’t know me too well. I was younger than you on the baseball team, but because of your story, I was able to get a colonoscopy set up. I’ve had stomach issues forever. Luckily, nothing came back from it.” I’ve had dozens and dozens of people tell me that and share that with me, which is literally the most important thing to me. That’s why I started this foundation, partially to help people with financial assistance who are going through cancer and everything, but the main reason is to help raise awareness and provide resources for people to get education about it because it’s not talked about enough.
Now it’s going to be the number one cause of death and cancer in people under 50 in men and women, behind breast cancer, and it’s never talked about. You see more younger people getting diagnosed with it and at a late stage, and nobody can tell us why. That’s the biggest thing for me. Part of our mission is to help get people connected with educational resources and actual care teams willing and able to help provide that.
When I got the news “you have cancer”
It still feels like it was yesterday. I was sitting in the emergency room with a screen in front of me and it was in the middle of one of the biggest snowstorms we’ve had in Kansas. My wife was at home. My parents’ house was not too far from the hospital I was at, so they drove to meet me there. When he told me, I sat there and didn’t know what to say or how to respond, to be honest. I sat with a blank stare on my face.
Then I called my wife and she started freaking out. She drove to the hospital and stayed the night before I got transferred. I felt super sick to my stomach. I didn’t know how to process it. My mom had breast cancer when I was very young. She’s 17 years clear, so she’s been doing great, but she felt just as sick, knowing that she has to watch me go through this now after she had to.
At that time, I was numb. Then, when I got the surgery and was recovering, I was trying to be optimistic and not be mad at the world. But then I started having a lot of panic attacks and anxiety attacks. Through my faith and the people I have, I’ve been able to overcome that. I’m probably too optimistic at this point, when I was told I got two years to live. A lot of people tell me they would have never guessed, with my energy levels and how I act and respond, that I was diagnosed with stage 4 colon cancer. But that’s a compliment because that’s how I want to live. I know people who are in the situation that are mad at the world and pessimistic and whatnot, and that’s not how I want to live.
My sister was working on the oncology floor of the University of Kansas Hospital. She worked there for three years. At the time, she was working at Mass General Hospital because her boyfriend and my future brother-in-law was a resident doctor at Mass General. Now they’re in New York City and both working at Mount Sinai. She’s working as a clinical research coordinator in oncology, and he’s a cardiology fellow. At the time, she was not, but a lot of her friends and connections were still there, and I’m very lucky because of that.
Her boyfriend had a friend who was working in the emergency room that day and was able to pull some strings and usher me back pretty quickly. By the time I got back, I had two doctors waiting for me, which never happens. They did some tests and were talking about doing scans. They immediately took me up to that cancer unit, and I was treated with the best care I could have ever asked for.
I’m still close with all those nurses up there. I keep in touch with them all the time. I just had my colostomy reversal surgery two weeks ago and I was getting wheeled up there to hang out with them and talk to them because I care about them deeply and they are amazing people. They are the best nurses in the world, in my opinion. They’re incredible.
I first went to urgent care and by the time I went, I was projectile vomiting and they said, “You need to go to the hospital,” so I had to drive myself while throwing up to the closest hospital and went to the emergency room. They did some blood tests and took me back for a CT scan. A couple of hours later, they told me they found what they believed were tumors but didn’t give me an official diagnosis.
I stayed overnight at that hospital. Their oncologist came down and told me that she believed that I had stage 4 colon cancer. At that point, there’s no other hospital. There’s only one option for me and that’s going to KU. They’re the best around here for that and one of the best in the country.
I had surgery right after I was diagnosed
My sister made calls and I had to discharge myself because they wouldn’t approve a transfer. My mom had to drive me over to KU and into the emergency room. I got admitted through there. That would have been on the 10th and the very next day, on the 11th, they officially diagnosed me. On Sunday, the 12th, that’s when they did surgery to remove the tumors and put in a temporary colostomy bag.
The plan moving forward
Recovery was not fun. On top of that, learning how to deal with a colostomy bag was a big challenge. Luckily, I have a brother who lives here and another brother who lives in Scottsdale, so he flew into town. My sister at Mass General, they gave her all the time off and said, “Go be with your brother,” so she flew in. She was like my second nurse. Her boyfriend was with me too. I was recovering for about a week and they said, “We typically don’t do this, but you need to start on chemotherapy as soon as possible.”
I started chemo three weeks post-op and finished my first round on my 28th birthday. I got discharged from the hospital a week after surgery. I believe a week or two after that was when I met my original oncologist. I’ve since switched to a new oncologist. I was thinking that they’ll say, “We’ve got a great chemo regimen. We’ll be able to get you past this. You’ll be good.” My oncologist looked me in the eye and told me that he doesn’t think I’ll live past two years. He straight up said, “You’d be lucky to live past two years with your mutation and how advanced your disease is.” Nope, I’m not accepting that.
I was with that oncologist for a little bit. I got a second opinion at MD Anderson. Unfortunately, they kind of told me the same thing. The only option for me was a BRAF-specific regimen and your only hope at living past three years. That hurt a little bit, as well as all the negativity around me. Everybody was telling me that I’ll be dead in two years and if I can live past that, I’ll be lucky.
But with this chemo regimen, doing a holistic approach of changing the way I eat, what I’m putting into my body, other supplements, and different types of alternative medicine, my oncologist estimated that about 90% of the disease on my liver is gone. With having more than 40 tumors originally, he’s mind-blown that I’ve had this good of a response to all the treatments and everything I’m doing so far.
Unfortunately, after the colostomy reversal, they found more tumors in my peritoneal wall. The response that I’ve been having to treatments and everything I’m doing has been very good so far. I continue to be optimistic about what I’m doing and think that eventually, I can get to no evidence of disease, against all odds that I’ve been given.
I changed my diet
When I talk to my colorectal surgeon and my new oncologist at KU, who’s incredible, I’ve asked multiple times, “Why are we getting this? Why are so many people getting colon cancer so advanced at such a young age?” He said, “We don’t know yet, but in my opinion and through a lot of research, it has to be environmentally-related to either the stuff that’s in our food supply,” like the chemicals that are getting sprayed, microplastics, all the additives and preservatives, or at least they think they could be a big factor into why so many young people are getting colon cancer, and it makes a lot of sense.
Ever since we’ve been kids, everything we’ve been eating has been pumped full of crap. They used to, at fast food restaurants, cook everything in beef tallow and now it’s all these different oils and other crap. The amount of stuff that is in our food is killing us and is being so harmful. My wife and I, as soon as I got home from the hospital, threw everything out of our pantry. We only order from Thrive Marketplace. We go to Sprouts and Whole Foods. We try to do everything organic. We started a garden at our house. Our neighbors have chickens and they give us their eggs. We try to do our best to know where our food is coming from and not get stuff that’s overly processed or has a bunch of stuff added to it. We’ve changed the way we eat for the most part. My wife falls off a little bit sometimes as she can’t help herself, but I’m very conscious now about what I put into my body.
I try to avoid a lot of gluten to reduce inflammation to fight against cancer. I take a lot of supplements, like B vitamin complex, vitamin C, vitamin E, milk thistle, turmeric, probiotics, and others. I’m trying to help my body fight this and I think a lot of it is contributing, outside of the chemotherapy and also helping me feel better from my chemo.
I urge everybody, whether you’re going through cancer or not, to change how you eat. Get all that crap out and fix it. That’s another goal of mine, too, which is to try to help people eat a lot better as well.
Getting multiple opinions is by far the best thing you can do. We’re still looking at options. We’ve got a friend who gets treated at Duke, and they do a lot of things with a HAI (hepatic artery infusion) pump for the liver. One of the best surgeons in the country is either at Mount Sinai or MSK who does HIPEC. In City of Hope and the Williams Cancer Institute in California, there are a bunch of places we look at to get opinions from because everybody has a different approach to how they do it, whether it’s traditional chemotherapy, repurposed medicine, alternative medicine, or whatever it is.
I’m open to anything to save my life and to get this out of my body. I’m not going to settle for what one person thinks. What’s great is that my new oncologist says, “I want you to get opinions from other places. If you need help getting those set up, let me know.” He’s not the type of person who says whatever he says goes. He wants me to get as many opinions as possible. If we can do it and they want to suggest something else, he says, “I’ll communicate with them and if we can do it here, I would love to. If not, get it done there.”
I’m glad I made the switch to him. He’s incredible. A lot of people don’t want to step on their doctor’s toes when in reality, it does not matter. It’s your health and your life. Do what you need to do. Do not settle for one person’s opinion. You have to see multiple people and get opinions from as many people as possible and find out different approaches as possible to see what may work and what may not. There are so many different treatment options outside of what your local or primary oncologist has or says.
My wife is the best advocate for that because sometimes I’m too scared because I don’t want to be mean or say something that I think is rude, my wife will say, “Why are you doing that? We should go look at that.” I tell her, “Thank you. I didn’t want to say it, so thank you.” She’s incredible at it. She’s not afraid to say what’s on her mind and to make sure that I’m getting the care I need.
I completed chemotherapy before my colostomy reversal. I was supposed to have another round, but one of the side effects of the regimen for my drug is a very bad skin rash on pretty much my entire body. It looks like I have painful acne, which it is. It has gotten so bad to the point where they couldn’t give me chemo because I had to see a dermatologist. Hopefully, I’ll get back on it, which will be my 16th round of chemo. For now, we keep doing it until it stops working. It depends on how long it can be effective for and then, eventually, we’ll look at other treatments. But so far, this chemo and everything I’ve been doing have been working out pretty well, so we’re not going to change course until it’s time.
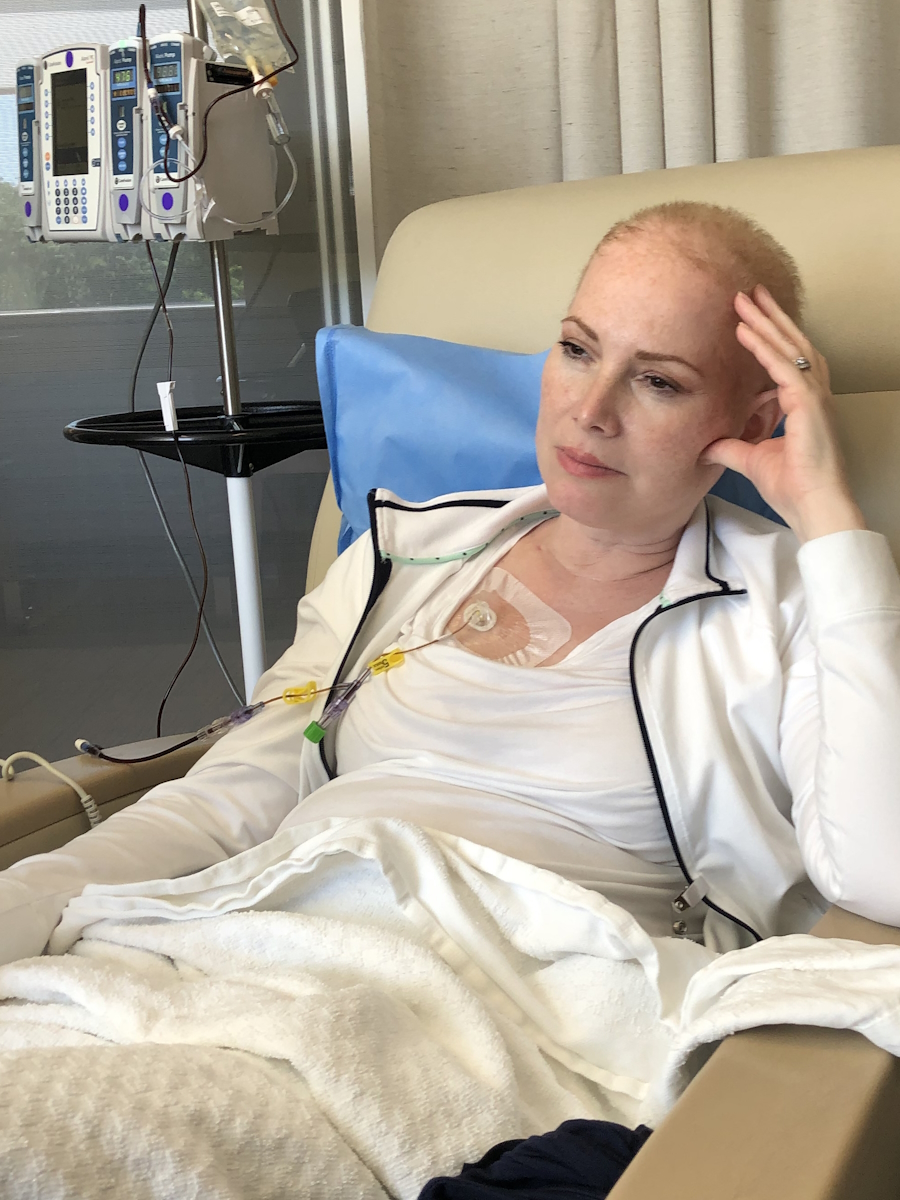
With my chemo regimen, I was on a drug, oxaliplatin, Vectibix (panitumumab), and 5-FU, and then I take oral chemotherapy, so four different chemos. I take Braftovi (encorafenib) every single day, four pills of those. I am now off of oxaliplatin because it’s so toxic and has given me almost permanent neuropathy in my hands and feet, so I had to stop that after 10 rounds because it got so bad. Now I just do oral chemo every single day. Every 14 days, I go in for my immunotherapy infusion, which I get through my port, and then I get my 5-FU pump that I’ll have for 46 hours. I’ll usually go in every other Tuesday, get chemo, and then have my pump until Thursday, and then get unhooked on Thursday.
Every day, I take four pills in the morning for my oral chemo. Every 14 days, I was getting three hours’ worth of infusions. Now it’s just one and a 46-hour pump.
I take like 25 pills a day, which is wild. It looks like I have an 80-year-old man living with me with my weekly pills on the counter.
At first, I didn’t have time to think about it because I had so much going on with recovery and trying to figure out if we could find out about this disease and how to treat it, types of treatments, where to go, what to look for, etc.
How my diagnosis has impacted me mentally
After I got diagnosed, the first month or two were very rough on me mentally. But since then, I’ve been doing well, mentally and physically.
The chemo is not as harsh on me anymore now that I don’t take oxaliplatin, which is good. I go to work in the office every single day. My company has been great about giving me time off whenever I need it, but I’ve worked full-time through everything. I’ve been blessed with the company that I work for. They give me a lot of grace and a lot of opportunity to go to my appointments and chemotherapy, and to take days off if I’m not feeling well. Most times, I’m in the chemotherapy chair working, in meetings and stuff like that. I’ve never stopped working. I’ve been working the entire time, which has helped me a lot mentally to try to stay as normal as possible.
The colostomy bag reversal has helped me a lot in terms of my quality of life moving forward, which is great. Outside of neuropathy, I work out and I’m able to still hunt and do the things that I love to do. Without the bag now, I’m optimistic that I can get back to Brazilian jiu-jitsu training, which is one of my favorite things to do in life and helps me a lot mentally. It’s a big release for me. I’ve been able to golf through all of it. It hasn’t been too much of a difficult change besides what I’m allowed to eat or not eat. I don’t drink alcohol anymore, so that’s a big change. I feel a lot better not drinking, so that’s a good change for me.
The worst is sitting at home. The last two weeks, while recovering from surgery, I would ask my wife to go drive me around the neighborhood because I needed to get out of the house. I hate sitting at home and doing nothing for all hours of the day. She, on the other hand, can do that every single day. I can’t. I have to be up and talking to people, going and doing stuff. I still have staples in me, but I’ve been going to work, seeing people, and going to meetings. I try to live as normally as I can without any change as much as possible.
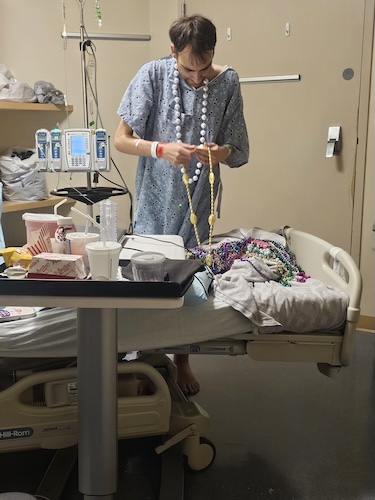
I had my colostomy bag removed
The bag reversal went well. Funny story, I was without pain meds after surgery for about 18 hours because they misplaced an epidural in me, so that wasn’t fun. But other than that, the recovery has been good so far. I’m up and moving around. I’m getting the staples out and I have a three-week follow-up, so it’s been great. I’m very blessed to be in this position to at least have this surgery.
All my cancer markers are still looking good, even with a break from chemo and having the surgery. I’m in a pretty good spot right now. I’m excited to get back on chemo and keep hacking away at the tumors. But as far as the reversal and everything, it’s gone very well so far.
They weren’t able to see the tumors and the peritoneal wall is very hard to see on scans. They could see something before, but we couldn’t tell if they were tumors or if it was scar tissue from my colostomy bag and the initial surgery. Unfortunately, when my doctor opened me up, he found four tumors right there, so he ended up taking four of them out, biopsying a couple, and then sending some off. He said those were definitely cancer. There could be more or there may not be. We don’t know how many are left in there.
The goal is to see on some PET scans coming up in September what we can try to find and the plan of attack is to continue what I’ve been doing as far as chemo and then look at HIPEC surgery potentially in 2026 to try to get all those out if we possibly can and continue to target the liver. My oncologist believed that with my scans from July that about 90% of my disease on my liver is either gone or dormant right now. My latest Signatera test came back as negative, so that’s good, meaning they’re stable and not active and spreading, so I’m very lucky for that.
The hardest part of my journey
The hardest moment was definitely the tail end of my hospital stay and then the first week at home, which is when it started hitting me that my life was changed forever. I was in a bad headspace and having very bad anxiety attacks and panic attacks. I was struggling.
I had a wild faith moment that changed everything for me following that, which is when everything changed for me and I was able to get rid of all of that anxiety, panic, and worry. Ever since then, I’ve been able to lean into that, my friendships, my family, and my wife. I was able to stay optimistic and faithful and keep moving forward and continue to focus on every single day. I used to get anxious thinking about the future. What is two months going to look like from now? What is a year from now going to look like? That gave me a lot of anxiety and worry. I now focus on every single day and not try to look too far ahead. I just enjoy what I have in front of me and not worry about what tomorrow is going to look like, so that’s helped me a lot.
I grew in my faith
I had a couple of friends who are college teammates of mine who flew into town after I got diagnosed. One of my friends and his wife brought me a new Bible and a new daily devotional, which was perfect. I have been asking and trying to get myself to hop back into my faith for a very long time. I was not happy with the person I was. It’s not like anything was super bad. I was empty and unfulfilled. I wasn’t happy with who I was and what I did. I used that as a good opportunity.
One day, I had a very bad panic attack and anxiety attack. The next morning, I sat down at the kitchen table with my wife and we opened up the devotional, and one of the verses in the devotional was Matthew 6:34. It was Jesus talking about anxiety and worry. He talked about why worry about tomorrow when tomorrow’s going to have its own troubles and today’s trouble is enough for today, so focus on today
I don’t know how to describe it other than this. In that exact moment, sitting with my wife at the table, I quite literally felt like a massive hug wrapped around me. It was crazy. I’ve never experienced anything like this in my life. The best way I can describe it is like a lake being perfectly flat and like glass. In that moment, I literally felt everything, all of the anxiety and worry, get pushed out of me. I was shaking and crying. It was the most overwhelming experience of my life.
I texted my friends. I looked at my wife Hannah and I said, “This is the craziest feeling ever.” At that moment, I have never in my life been more sure that God and Jesus are real, and that I’m going through this for a reason. The more I continued to think about it, I kept praying every single night, saying, “God, please do something in my life to bring me closer to you. Change my life and change my faith,” and then all of this happened.
I’m almost grateful that I got diagnosed with this because without this, none of this would have ever happened in my life. I feel like there are two reasons I’m going through this. One is to talk about my faith and the gospel. With that, I’ve started a weekly Bible study where I have six of my friends and two of them got baptized this year. That is the greatest thing for me. I was on a radio show talking about my diagnosis and I was able to share this story. That’s the first reason why I’m going through this is to grow in faith.
How I’m supporting others with cancer
The second thing is to be able to talk about colon cancer and raise awareness about it and legitimately try to save lives. We started The 3929 Foundation. The number 39 is for a family friend of mine, his name is Matt Fitzmorris. His dad, Al Fitzmorris, played for the Kansas City Royals and passed away from cancer in December, a few weeks before I got diagnosed. The number 29 was my number growing up throughout my entire life, so we decided to start this foundation.
We filed for our nonprofit 501(c)(3), so we’re waiting for that, but our goal for the foundation is to be able to help people and their families who are going through cancer by helping them financially. I know from experience. My chemo treatments every other week are $81,000. That’s how much it costs for my chemo every 14 days. $81,000, twice a month. Luckily, I have phenomenal insurance where it’s all after my deductible was hit in January, so it’s 100% paid for, so I’m very lucky. Otherwise, I’d probably have millions of dollars of medical debt.
We know how difficult it can be to make a payment on your mortgage or buy something for the house when you’ve got medical bills to pay, so that’s our priority. People can go to our website to apply for financial assistance. We’re also working on surprise donations to people at the KU Cancer Center, where I get treatments, to help them out.
We want to provide education and resources specifically about colon cancer to raise awareness. We formed the foundation in March and in May, we had a pickleball tournament and raised $15,000, which is super cool. We’ve got another event that’s more my style, which is trapshooting, that we’re doing on October 5th to raise money. We’re trying to do multiple events throughout the year. We’re starting to sell our merchandise on our website. We’re getting that all up and running.
I feel lucky and grateful that I’m going through this and able to help people. It’s crazy to me because I get told all the time by my friends and family, “I wish you didn’t have to go through this. I wish I were the one who got this and not you.” Absolutely not. I am grateful and lucky that I’m the one going through this because I wouldn’t be able to stand watching somebody I care about go through this. Watching somebody I cared about going through that would kill me, so I’m very glad that I’m the one who has it, because I know that I can deal with it and I’m strong enough to withstand it. I tell them, “Don’t ever say that. I’m glad I’m the one going through it and nobody else I know.”
I hope that I can help as many people as possible. I don’t know how long I will be here for. Hopefully, for a very long time. I hope that, however long I am here, I can help and impact as many people as I possibly can, so that’s what I’m here to do.
I have a new outlook on life
My perspective on everything in life has changed. It’s very wild. In a weird way, I needed this. I tell people all the time. I feel the best, but not necessarily physically. Sometimes I do, but mentally and spiritually, living with all these tumors and stage 4 cancer and all this going on, this is the best I’ve ever felt in my life. I genuinely mean that. It’s crazy for me to say that, but it’s true. I am so grateful that I’ve gotten this opportunity. Yes, it absolutely sucks. There’s a lot of stuff I can’t do anymore. Some days, chemo makes me want to feel like death might not be so bad, but I wouldn’t change anything about this.
What I want others to know
I was scared to go to the doctor, not because I was actually scared, but because I hated it. I thought it was pointless. Listen to your body. If you notice anything, pay attention to your body and to anything going on. If anything is different, go get checked out and see somebody. I would always push it off, no matter what it was, thinking that I didn’t need to go to the doctor and that it’d go away.
I often think about 2024. What if in July, when I started, I paid attention and cared about the things going on? If I noticed I was starting to feel fatigued and my stool was thinning, changing, and looking different, if I got checked out and they found something, maybe I wouldn’t have had a complete blockage. Maybe I wouldn’t have had 40 tumors on my liver. Maybe it would have been two and it would have been a lot different story. Maybe I would have been stage 2 or 3 instead of stage 4.
Listen to your body. If you feel like anything is off or wrong, don’t neglect it. Get checked because I was the exact opposite. Obviously, I regret it a little bit by not having myself checked earlier. Be aware of that. Take your body and your health seriously. Change the way you eat. Be conscious of what you’re putting into your body and how you’re treating it. Exercise as much as possible. Try to make a change in your life in a good way.

Inspired by Jackson's story?
Share your story, too!
More Metastatic Colon Cancer Stories
Raquel A., Colorectal Cancer, Stage 4
Symptoms: Frequent bowel movements, pin-thin stools, mild red blood in stool
Treatment: Chemotherapy
Steve S., Colorectal Cancer, Stage 4
Symptoms: Blood in stool, changes in bowel habits, feeling gassy and bloated
Treatments: Surgery, chemotherapy, monoclonal antibody, liver transplant
Jessica T., BRAF Mutation Colon Cancer, Stage 4
Symptoms: Severe stomach cramps, diarrhea, vomiting, anemia (discovered later)
Treatments: Surgery (hemicolectomy), chemotherapy
Jennifer T., Colon Cancer, Stage 4
Symptoms: Weight loss, coughing, vomiting, sciatica pain, fatigue
Treatments: Surgeries (colectomy, lung wedge resection on both lungs), chemotherapy, immunotherapy
Kasey S., Colon Cancer, Stage 4
Symptoms: Extreme abdominal cramping, mucus in stool, rectal bleeding, black stool, fatigue, weight fluctuations, skin issues (guttate psoriasis)
Treatments: Surgeries (colectomy & salpingectomy), chemotherapy