Family, Loss, and a Second Chance: Valerie’s Metastatic Thyroid Cancer Story
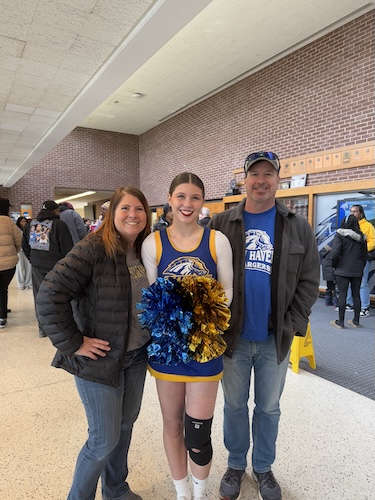
Valerie was diagnosed with metastatic thyroid cancer (papillary thyroid carcinoma) in January 2025 after a series of concerning changes in her body, including unexplained bruising, persistent weight loss, and extreme cold intolerance. Her first concern, had her previously-fought leukemia come back? And while these aren’t typical symptoms of thyroid cancer, looking back, they were early signs that something in her thyroid system wasn’t functioning normally. As a registered nurse and devoted family advocate, she drew strength from her loved ones while navigating one of the most challenging periods of her life.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez & Jeff Forslund
Valerie was concerned her symptoms could be attributed to her history of having had leukemia. But new tests came back negative. After an unrelated car accident and neck pain that was getting worse days after the accident, radiology colleagues recommended scans that revealed suspicious thyroid findings. The diagnosis of thyroid cancer, which was confirmed through a needle biopsy, brought news of a malignant form with a gene mutation associated with rapid progression and lymph node spread. Valerie’s support system mobilized: her husband returned home from a work trip, and her family rallied around her.

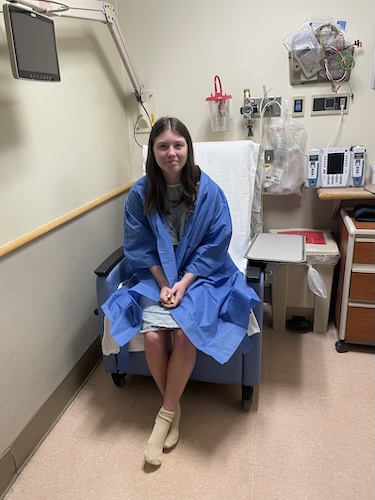
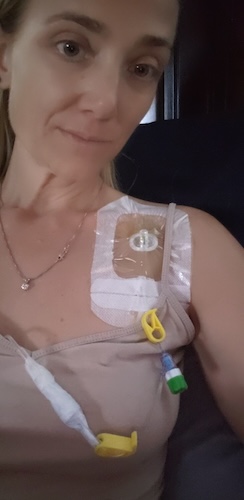
Valerie’s treatment was supposed to begin with a thyroid lobectomy, but it escalated to a total thyroidectomy when scans showed that the cancer had spread to her entire thyroid gland. While surgery margins were clear, subsequent bloodwork and imaging soon revealed that it had also spread to various lymph nodes, making further biopsies necessary and ultimately requiring lymphadenectomy and neck dissection surgery. Valerie encountered the possibility of voice loss and the need for radioactive iodine therapy. Side effects were difficult, including loss of taste and fatigue.
Throughout her experience, Valerie has remained proactive and reflective. She adjusted to the need for lifelong medication, adopted daily routines to ensure consistency, and processed layers of grief from infertility and family loss. She met each setback with gratitude and by focusing on small wins, thanks to her community and the comfort of advocacy. She now manages regular monitoring and medication while emphasizing emotional resilience, acceptance, and the power of patient support. Valerie’s experience offers a powerful lesson: with self-advocacy, support, and inner strength, patients can find meaning and healing even in the face of formidable illness.
Valerie’s video and the edited transcript of her interview provide key insights and lessons from her experience:
- Early, persistent symptoms such as bruising and cold intolerance should always prompt a thorough investigation for thyroid cancer and similar conditions
- Advocacy within healthcare, whether through using medical connections or self-advocacy, can accelerate diagnosis and timely treatment
- Emotional and family support underpin resilience through the challenges of advanced cancer treatment
- Lifelong management (such as thyroid hormone suppression therapy) is common after total thyroidectomy and can be a major adjustment
- Healing is not linear, but finding moments of gratitude and hope is always possible, regardless of circumstance
- Name: Valerie V.
- Age at Diagnosis:
- 29
- Diagnosis:
- Thyroid Cancer (Papillary Thyroid Carcinoma)
- Staging:
- Stage 4
- Warning Signs & Symptoms:
- Bruising
- Extreme fatigue
- Cold intolerance
- Weight loss
- Treatments:
- Surgeries: total thyroidectomy, neck dissection, lymphadenectomy
- Radiation therapy: radioactive iodine therapy
- Hormone therapy: thyroid hormone suppression therapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Valerie
- Family, nursing, and what matters most to me
- My early warning signs
- Losing my son, and the car accident that changed everything
- The scan revealed something suspicious about my thyroid
- Hearing “You have thyroid cancer” at work
- Telling my husband: “There’s no good kind of cancer.”
- My surgery plan changed overnight from a half- to a total thyroidectomy
- “You’re cancer‑free” — and then a shocking recurrence
- “I don’t think anyone will touch you”: I had risky lymph node surgery
- My high-risk neck dissection surgery and radioactive iodine
- My PET scan results: “As of now, you’re cancer-free.”
- My daily life after treatment: scars, pills, and small routines
- The emotional toll on my parents and the burden of being a survivor
- Grieving our son, infertility, and being forced to wait
- What survivorship means to me now
- My message to others living with cancer
My name is Valerie
I was diagnosed with metastatic papillary carcinoma [thyroid cancer] in January 2025. I’m from Houston, Texas.
Family, nursing, and what matters most to me
I am a big family person. I adore and I’m obsessed with my little family. But also my siblings and my parents and my in-laws, and the siblings I’ve gained from them. I love doing anything and everything with family. That’s probably what occupies my time most. If I’m not with my family, I’m at work. I am a registered nurse, and I just try to balance that whole nurse life and family life because they are very important to me.
I am probably most passionate about being present for my family and my patients. I love my role as a radiology nurse in interventional radiology and how it lets me support people at really vulnerable moments, but nothing compares to being with my husband and our dogs.
One of my favorite photos is probably a picture with my dogs, or of my dogs, or of my husband and my two dogs. Like I said, I’m obsessed with the little family that we’ve created. I am that person who is like, “These are my four children, these are my two daughters.” People think I’m crazy, or people love it. I don’t care.
My early warning signs
The only symptoms I had that made me suspicious that something was going on in my body started before the official diagnosis. I have had leukemia in the past, and I remember that I was bruising so much. It was so random. I would wake up with so many bruises. I went back into that mindset of, “Oh my gosh, is this leukemia?” It could have been a million things, but leukemia was at the top of my mind.
I went to my doctor because I had been experiencing weight loss. I had lost these 10 pounds that I could not, for the life of me, gain back. When you lose weight, it’s not like every time you’re begging to gain it back, but those 10 pounds were so tricky because I am pretty active. I also had extreme cold intolerance. I would be wearing four layers, with a heating machine at work. I could not control my body temperature.
When I went to the doctor, I initially said, “I think I have leukemia.” We did a leukemia workup, but did not check my thyroid. She came back and said, “No, you’re good.” I thought, okay, maybe this is just weird stuff, and I just have to live with it.
Losing my son, and the car accident that changed everything
Then I got pregnant with my son. He was stillborn. I gave birth to him at the end of December. Two weeks after that, as I was leaving my doctor’s appointment for my clearance postpartum appointment, I got into a car accident.
I work in radiology as a radiology nurse in interventional radiology. A couple of days after the accident, I went to work and told my team, “You guys, my neck is killing me. Something’s going on with my neck. I feel like there’s a lot of pressure.” They said, “Get yourself on the CT. Let’s scan you and do it all. Let’s get the X‑rays and the CT.”
I know I am so fortunate and blessed to be in that position. I know it’s not like that for every patient. Typically, with thyroid cancer, you are advocating to the ends of the earth just for someone to scan you or take you seriously. After I did that CT scan, I went to the radiologist and asked if he had time to look at it really quickly, to see if I had any fractures or whiplash.
The scan revealed something suspicious about my thyroid
He immediately pulled up my scan and said that my thyroid did not look good. I asked, “Can you elaborate on that? What do you mean?” He said, “I think we need to do a biopsy.” I explained that I have a history of Hashimoto’s and that thyroids can look lumpy when you have Hashimoto’s. I asked why he wanted to do a biopsy and what he was seeing.
I will never forget his face. He turned back and said, “I’m not going to alarm you, but I just want to get a biopsy done.” I said, “Okay, great. Let’s do it.” They were so quick. That same day or the next day, I was in the ultrasound room getting the biopsy. It’s never fun to have a needle in your neck around all those important structures.
It took about five days to a week to come back. Those five to seven days, you’re trying to be calm, but you are thinking of everything it could be.
Hearing “You have thyroid cancer” at work
I was at work the day the results came back. The same radiologist who had looked at my scan initially and did the biopsy found me in the middle of the hallway and said, “Hey, when you have a moment, I need you to come into my office.” I think I knew then and there that it wasn’t good news. If it had been good, he probably would have just high‑fived me and handed me my report.
My husband was out of town for work. I went into the radiologist’s office. He had my scans up and the pathologist on the phone. He said, “Val, I think you should call your husband.” I said, “No, just tell me. I don’t like what’s happening. Just tell me what’s going on.”
The radiologist told me it came back positive: I had cancer. He explained that there is almost a scoring level for how malignant or dangerous it can be, and mine was the most malignant possibility. With papillary carcinoma, it’s pretty common to have a gene mutation that makes it spread faster or have the potential to spread faster. He held my hand and stayed with me. I am so grateful for the medical team that has been with me on this journey.
The pathologist explained that people can live with papillary carcinoma for years before it becomes a problem, but with the mutation I have, it has the potential to spread and metastasize to my lymph nodes. I asked if I needed to get it removed, and he said he would not wait any longer than a month to remove it. I said, “Okay, great. Let me call my husband.”
My adrenaline was rushing. I was focused on action: getting on the schedule with the surgeon, getting recommendations, and doing any scans I needed. It wasn’t until later, after talking to the doctors, that it truly hit.
Telling my husband: “There’s no good kind of cancer.”
I called my husband and said, “Babe, I have thyroid cancer.” At the time, life felt really heavy. We had just lost our son. My husband was working out of state. And then you hear the C‑word. No matter what kind of cancer, even thyroid cancer, which is considered a “good kind” of cancer, there is no good kind of cancer.
Making that call to my husband, telling him, “Honey, I have cancer, thyroid cancer, and they said I shouldn’t wait longer than a month to get it out,” was heartbreaking. He flew home immediately and was on a red‑eye about three and a half hours later just to be with me. My family also supported us, and I am very thankful for that.
From there, I got more scans to check for lymph node involvement. I had another CT scan with contrast to better visualize my thyroid. I met with a general ENT surgeon in the area who was very reassuring.
My surgery plan changed overnight from a half- to a total thyroidectomy
At first, scans showed cancer only on the left side of my thyroid. The surgeon said we would just remove one side, so I wouldn’t have to go on levothyroxine every day. That sounded amazing. I know how much the thyroid does for every aspect of your body, so I wanted to preserve whatever we could.
About two to two and a half weeks passed after the diagnosis, meeting with the surgeon, and getting scheduled. The night before surgery, my surgeon called and said he needed me to get one more scan. I told him I had already had two scans in the last two and a half weeks. He insisted.
The stat scan that night showed the cancer had actually spread completely onto the right side of my thyroid and was covering my thyroid. I remember thinking, “That’s so crazy.” The plan changed from a half-thyroidectomy to a full, total thyroidectomy.
He reassured me they would get it out, but I would have to be on medication for the rest of my life. No one wants to be on medication forever, and I wasn’t looking forward to it, but surgery went great.
My margins looked good. It was a very successful surgery, and I healed well.
“You’re cancer‑free” — and then a shocking recurrence
After surgery, I was referred to my first endocrinologist. I followed up three weeks after my total thyroidectomy and did blood work. She told me my cancer marker, thyroglobulin, was undetectable. She wanted to keep me in suppression. She said I would be considered in remission for thyroid cancer after three years, though my most recent endocrinologist later told me five years.
I asked, “If it’s undetectable, are you saying the cancer is gone?” She said, “Yeah, Val, you’re cancer‑free.” I was ecstatic. I thought, “This is the end of it.” Even though it was annoying to deal with, it felt like a short cancer journey that I could handle. We celebrated with my family.
Then that endocrinologist moved out of state, and I had to find another one. I hadn’t even met the new endocrinologist yet. He was brand new to the area and had just opened his practice. Around that time, I started feeling like something was pushing against my throat. I couldn’t swallow well. My thyroid pill is so tiny, but I was starting to choke on food and on thicker liquids like smoothies. I told myself it would go away.
At my first appointment with the new endocrinologist, I don’t think he even asked my name. He said, “Sit on the table. We’re going to do another ultrasound.” We laugh about it now because I told him later, “Did you realize you didn’t even ask my name?” He said he had business to take care of and needed to check things.
He pressed so hard with the ultrasound probe and then said, “This is not good.” I responded, “What do you mean? Hi, my name is Val. Can you tell me your name before you tell me this is not good?” He looked at his medical assistant and asked for a fine needle aspiration kit. He said we needed to do a biopsy.
I felt whiplash. I had already celebrated and accepted being cancer‑free. I asked him to explain what was going on. He finally told me I had suspicious lymph nodes and needed to check if the cancer had spread. I said, “No, I don’t have cancer. I was told I don’t have it anymore.”
He said it was up to me if I wanted to do the biopsy, but I had a really big lymph node right up against my vocal nerve. He said, “If anything, let me biopsy that one. That’s probably why you feel such pressure there.” I agreed.
I called my husband, and he didn’t believe me at first. He thought I was joking because my bloodwork had come back negative, and we were told I was in the clear. The biopsy was expedited and came back in about three days.
I was getting false negatives from my thyroglobulin, and it happened twice. He ended up doing about three biopsies. They all came back positive for papillary carcinoma. I asked what I needed to do, and he said I needed those lymph nodes removed with a neck dissection.
“I don’t think anyone will touch you”: I had risky lymph node surgery
I did another CT scan to see how many lymph nodes were involved. I called my original surgeon after he read the CT. He told me, “Val, I can’t even touch you.” I had lymph nodes in my chest, some on my vocal nerve, on my carotid artery, and on my aortic arch. He said the surgery was so risky he didn’t think anyone would touch me.
I remember feeling intense anger. I am not usually an angry person, but I felt like, “You told me my margins were good. You told me there were no lymph nodes. How did we miss this?” The lymph nodes were large, and my endocrinologist said, “You’ve had this the whole time.”
After I calmed down, I reminded myself that I work with some of the greatest radiologists. It may have been at such a cellular level that it didn’t appear earlier, and because of my mutation, it grew very fast. The confusing part was the false-negative thyroglobulin results.
I asked my original surgeon who I should go to. He recommended a second surgeon, Dr. Jason Diaz, an oncologic ENT who studied at Huntsman Cancer Institute. This is his specialty — anything around the neck; it’s his bread and butter.
When I called his office, they said his next available appointment was in six months. I thought, “Great, I’ll just let it fester in my body.” I didn’t trust anyone else. My husband told me I couldn’t wait six months. We called back and asked for a cancellation list. Forty‑eight hours later, they called and said he had an opening on Monday. I said yes immediately.
I went with all my paperwork, scans, and reports. He was so detail‑oriented. Surgeons aren’t always the warmest personalities, but I appreciated his honesty. He said, “Listen, I’m going to take such good care of you, but this is what’s going to happen.”
He told me the chances of my ever talking again were probably slim to none if he had to remove the lymph nodes around my vocal nerves because it would damage the nerve. He also said he was debating whether to touch the lymph nodes near my carotid and aortic arch. They were millimeters away. He said the risk of my not making it out of surgery was too high to remove those. I respected that honesty. I told him to tell me what I needed to do, and I would do it.
He showed me an implant he might place to help my vocal cord so I could talk somewhat, but I would never sound the same or be able to sing. Going into surgery, I knew I might still have cancerous lymph nodes left that could continue to spread. He explained the chances of metastasis to my lungs or bones would be higher.
In my mind, I kept hearing people say thyroid cancer is an “easy cancer,” yet I was sitting in a room being told I might lose my voice or not make it out of surgery. Everyone says it’s an easy cancer, yet I’m sitting in this room, potentially losing my voice and potentially not even making it out.
My high-risk neck dissection surgery and radioactive iodine
When I had the surgery, it went better than expected. He was very successful in getting all of the lymph nodes, even the ones in my chest. Later, he told me I had basically been positioned upside down, with my head tilted back 180 degrees, which helped lift those lymph nodes so he could reach them. He came out of surgery so happy and said, “I did it. I got all of them.”
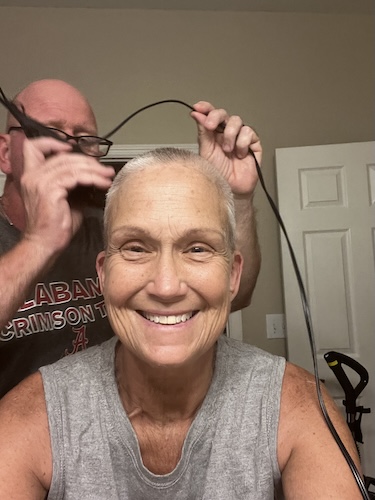
Because it had already spread to my lymph nodes, I needed radioactive iodine. From my second surgery, which I am incredibly grateful also went well, to radioactive iodine, it has been a lot. My mom always joked because even when I had leukemia as a kid, every time they listed the “less than 1%” side effects, I would get them.
For radioactive iodine, I had to do Thyrogen injections. I got blurred vision and called my endocrinologist, saying, “I think I’m going blind.” My peripheral vision was completely blurred. He said it happens to less than 2% of people. My mom was right again. I had extreme nausea, bone‑deep fatigue from going from high suppression to being stimulated, and a sore throat and fever the first time. The second injection went a bit better because I was prepared with my Zofran ready to go.
Then I went in for the radioactive iodine and was put in isolation for a week. I had neck swelling, jaw pain where I thought my teeth would fall out, runny eyes, and a choking sensation from inflammation. I couldn’t taste good food, so I joked that I was on the salad and kale diet until my taste came back.
My PET scan results: “As of now, you’re cancer-free.”
I did a full‑body PET scan. The big concern was that the cancer might spread to my lungs or bones. I opened the results on my phone after a workout class, sweaty and not feeling my best. It said there was no indication that the cancer had moved and no indication of active cancer in the lymph nodes.
I read it to my husband, and he asked, “Does that mean it worked? Does that mean your cancer is gone?” I still didn’t quite trust it yet. A few days later, I met with my endocrinologist. She said that, as of now, I am cancer‑free, but we would continue checking every three months because recurrence with thyroid cancer is fairly common. You can never remove every single piece of thyroid tissue from the body.
My TSH or thyroid-stimulating hormone had stopped responding to the previous dose, so she increased my levothyroxine to keep me in a suppressed, hyperthyroid state as long as I can tolerate it. The side effects of being hyperthyroid are real, but if it means avoiding another surgery or radiation, I would choose the side effects most days.
My daily life after treatment: scars, pills, and small routines
The plan now is to keep me in suppression and monitor me closely every three months. In the meantime, I am rocking my scar and dealing with everything that comes with remembering to take a pill every day before eating. That is honestly one of the worst parts.
I am not a 5:00 a.m. person, but I try to get into routines. I joke that there is one reason I’m grateful I don’t have to take birth control, because remembering a pill at the same time every day is hard. But with thyroid cancer, you’re told, “You’re going to have to take a pill for the rest of your life anyway.”
My thyroid regulates so many vitamin levels that I now have a full regimen. I have a little pill container I refill every Sunday night, like I’m 80 years old. There’s nothing wrong with 80‑year‑olds and pill containers, but it’s not what I pictured as a 30‑year‑old. It’s been a wild ride.
The emotional toll on my parents and the burden of being a survivor
Navigating this again with my family has been complicated. With my first surgery, the total thyroidectomy, I barely shared anything with my parents. The way I felt scared, I knew my mom would feel it times a thousand. She’s just a mom. The doctors were so confident that I downplayed it.
When the cancer came back and I was told I needed another surgery in very risky locations, I broke down like a kid again and just wanted my mom. I called her at midnight, 1:00 a.m. her time in Houston. The phone barely rang before she answered.
We were FaceTiming, and I said, “Promise not to freak out.” She said, “I’m already freaking out, so go ahead and tell me.” I told her, “Mom, it came back, and the risks are a lot higher.” I was so beaten down and exhausted after everything this year that I reverted to being her little girl who needed her mom.
My parents flew out the following week, arriving the day before my surgery. I had tried to keep it from her, but eventually I said, “Listen, I’m having surgery again on this day,” and she said, “Okay, we’ll show up on Sunday.”
When I saw her at the airport, she broke down and cried, and we cried together. I kept saying, “I’m sorry.” There is a guilt you feel as a cancer survivor: the burden you put on your family.
My mom reminded me to stop apologizing. She was grateful I let her in. She said her reaction is her own and that I should know she loves me, is worried for me, and believes I’ll get through this. Seeing her and remembering how terrifying it was when I had leukemia as a child brought all those emotions back.
Grieving our son, infertility, and being forced to wait
On top of cancer, my husband and I have been dealing with infertility, partly from my history with leukemia, and then losing our son. Earlier this year, there were times when I physically could not get out of bed. We hadn’t fully processed his loss because two weeks after his stillbirth, I was thrown into this cancer fight.
We recently talked about how we have to wait a full year before trying to get pregnant again. He said, “Let’s use this year to honor him and think about how beautiful life really is. Let’s find different ways to honor him.”
Strangely, we are grateful for having to wait a year. We want to fill it with ways to honor our son, to find joy even when it hurts. We also have another chance to try to be healthy, and we have each other. I’m very aware that not everyone has a supportive spouse, so I don’t take that for granted.
We hope to use this next year to learn how to breathe again and find our new normal; still getting scans and bloodwork every three months, hoping we don’t need more surgery… but truly trying to heal.
What survivorship means to me now
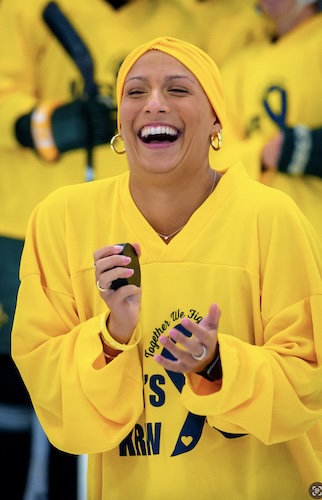
Survivorship, to me, is choosing every day to see life as a gift, even when it doesn’t feel like one. After hitting five‑year remission from childhood leukemia, I used to tell myself that everything is a gift — trials, heartache, and joy. You have to continuously choose to see the lighter days and take every emotion as it is. Where there is a lot of heartache, there is also a lot of joy and love.
Somewhere in my 20s, I think I lost some of that perspective. I got more inward, more focused on my own world, letting weeks go by without talking to family or friends. After dealing with infertility, losing our son, and then a second round of cancer, that earlier sense that “everything is a gift” has been reignited.
Now survivorship looks like using my time intentionally: showing gratitude, loving the people in my circle, and serving where I can. It means accepting that there will be scans every three months, side effects from being in a hyperthyroid state, and days when the emotions are heavy and I can’t pull myself out of a sad moment. But it also means celebrating tiny wins.
My message to others living with cancer
If someone came to the end of my story and I had one piece of advice or one message to leave with people, it would be this: find the happiness and gratitude in the small things.
Life can be full of a lot of unfairness, but there is good out there. Keep going, even when it’s hard.

Inspired by Valerie's story?
Share your story, too!
More Thyroid Cancer Stories
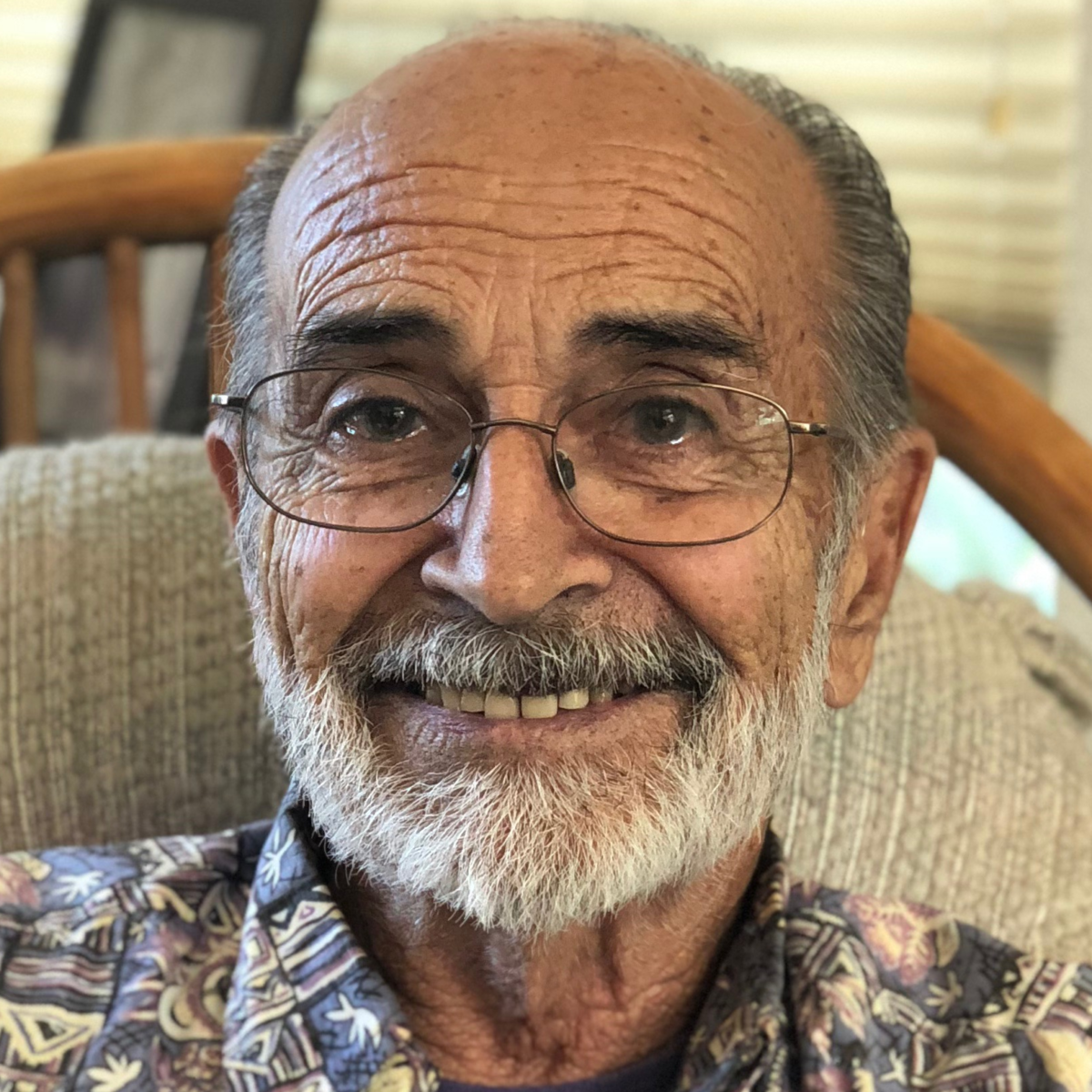
Greg S., Metastatic Papillary Thyroid Cancer, Stage 2
Symptoms: Fatigue, lump in neck near Adam’s apple
Treatments: Surgery (thyroidectomy), radioactive iodine therapy
...
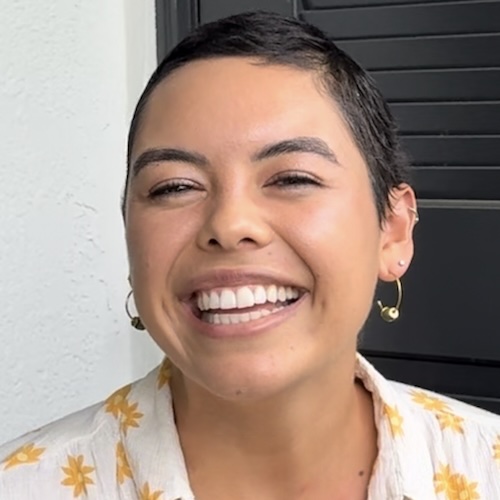
Nancy, Metastatic Papillary Thyroid Cancer, Stage 2
Symptom: Lump in neck
Treatments: Surgery (thyroidectomy), radioactive iodine therapy
...
Sarah J., Papillary Thyroid Cancer, Stage 1
Symptom: Enlarged thyroid
Treatments: Surgeries (thyroidectomy, partial neck dissection), radioactive iodine therapy
...
Jamie K., Papillary Thyroid Cancer, Stage 1
Symptoms: Difficulty swallowing, lump on neck
Treatments: Surgery (thyroidectomy), radioactive iodine therapy
...