A Creative Life, Interrupted: Red’s Experience With Tongue Cancer After Losing 40% of Her Tongue
Working as a wig attendant and makeup artist, Red had just begun embracing her creative dreams with a close-knit theater community when her health took a dramatic turn. She was in the middle of building a life she loved when a small canker sore on her tongue refused to heal. What first seemed ordinary became the start of an experience that would lead to a tongue cancer diagnosis that changed her life, tested her instincts, and forced her to examine her sense of self.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez and Jeff Forslund
As the sore on her tongue stubbornly refused to heal, Red was initially net with medical dismissal but trusted her instincts and pressed her doctor for a referral to a specialist. That one moment of self-advocacy in that first appointment led to a specialist appointment with an ENT where she finally received a frightening diagnosis: stage 3 tongue cancer. Moreover, the news arrived in the midst of a hectic photoshoot.
Rather than yielding to fear, Red channeled her energy into connecting with friends, colleagues, and even cast members at the theater, who were more than happy to support her and lend encouragement. She also found symbolic and creative ways to cope, including naming her cancer “Carl” for privacy and maintaining humor and compassion throughout her experience.

Surgery followed; doctors removed 40 percent of Red’s tongue and performed reconstructive surgery afterwards. Recovery was demanding, involving rigorous procedures to save her speech and swallowing abilities, physical therapy, dietary changes, and pain management. Eventually, she also underwent radiation treatment. The unwavering support of her medical team, family, and fellow artists made a difference throughout her experience. Karaoke nights, theatrical send-offs, and simple acts of care became touchstones of hope and solidarity before surgery and after.
Returning to work after treatment marked a new chapter in Red’s life, highlighting the emotional and psychological adjustments required after surviving tongue cancer and similar kinds of cancer. She emphasizes the critical role of self-advocacy, resilience, and the right to appear and feel confident at every stage, whether through creativity, community, or self-care practices. Red’s tongue cancer experience reminds others that healing is a lived, ongoing process that is personally defined by each patient.
Watch Red’s video and browse the edited transcript of her interview below to learn more about how:
- Advocacy is vital: Trust yourself and push for answers if something feels wrong
- Creative outlets like makeup can empower recovery and restore confidence after major life changes
- The support of community, namely, family, friends, and colleagues, provides essential strength during tough times
- Healing is not linear; recovery from cancer includes both physical and emotional milestones
- Red’s transformation involved reclaiming her confidence, advocating for herself, and finding a new purpose
- Name: Red S.
- Age at Diagnosis:
- 35
- Diagnosis:
- Tongue Cancer (Squamous Cell Carcinoma of the Tongue)
- Staging:
- Stage 3
- Symptom:
- Persistent tongue ulcer that increased in size
- Treatments:
- Surgeries: partial glossectomy, flap surgery
- Radiation therapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Hi, I'm Red
- How cancer arrived in the middle of my dream job
- The hospital bed stretch video that connected me to my crew
- Being a young non-smoker with rare oral or tongue cancer
- The “canker sore” on my tongue that turned out to be cancer
- Getting the biopsy and the phone call that confirmed cancer
- We nicknamed my cancer “Carl”
- My 10-hour tongue cancer surgery and flap reconstruction
- Walking up from tongue surgery and already speaking
- Learning to swallow again and choosing radiation
- Daily radiation, crushing fatigue, and singing karaoke again
- Returning to the theater after tongue cancer surgery
- Learning to love my scars and advocate for my body
- What I want others to know
Hi, I’m Red
I was diagnosed with oral cancer, specifically tongue cancer, in 2025.
And I am from all over, but I currently live in Stratford, Ontario, Canada. I am a dual citizen, so I’ve lived all over the US as well as up here in Canada.
Currently, I am a wig attendant as well as a makeup artist with the Stratford Theater Festival. I actually did a career change; before that, I was working in the TV and film industry with a large multimedia company, Disney, for over ten years, working at ABC News, ESPN, Disney Channel, and Disney Junior on the corporate side of things.
I’ve always considered myself to be more of a creative individual. After going through some other hardships, I reevaluated what I wanted to do with my life and realized my passion really is makeup and storytelling, and the way that we use makeup to tell a story. It’s not just a glamorous vanity thing; it gives people so much more than that.
I do glamor makeup, theater makeup, and special effects. I create scars and burns and can recreate all of that. It’s kind of funny that after everything I went through, I now have the best reference photos I could have: my own. It has been a wild journey, and to get this diagnosis right when I finally got to a point in my career where I thought, “I’m here, I’ve made it, this is the dream, I’m living it,” and then cancer showed up, it was a lot.
How cancer arrived in the middle of my dream job
There is never a good time to get cancer. There’s never a perfect schedule where it’s right on time. No one wants that, ever.
It weirdly did the work for me, which I wasn’t expecting, because of the community I was in and the location I was in. I had family support, medical support, and I was able to see specialists very quickly because it is such a rare thing.
I was very lucky. Even by US standards, I probably still would have been waiting much longer. The support from my theater community was something I never anticipated, especially because it was my first season. I had only been working with people for a short time, but when you are doing their wigs and makeup, you work very closely. People rallied behind me, reached out, and sent me so much love and support that I still could probably cry about it.
The hospital bed stretch video that connected me to my crew
Part of our warmups with the crew was stretching our bodies. We were working on Robert Lepage’s Macbeth, set during the biker wars in Quebec, and there are literally motorcycles going around on stage and backstage. We would stretch out our hands, twist, and move as though we were revving a motorcycle to loosen our wrists.
When I was in the hospital, they told me I had to stretch in my hospital bed. I asked my dad to record me doing our “rev the motorcycle” stretch. He thought I was on medication and had no idea what I was doing. Then I got a message from my crew where every single person was doing the same warmup and saying, “Hi, Red, miss you.” It was silly but incredibly memorable and meaningful.
Being a young non-smoker with rare oral or tongue cancer
Oral cancer itself is rare. From what I read, about 1% of annual cancer diagnoses are oral-related, and that includes the whole mouth. Tongue cancer specifically is even rarer. For someone my age who is not a smoker and doesn’t fit the usual risk profile, it’s very unusual.
We don’t know why I got it. It wasn’t HPV-related, it wasn’t smoking-related, and although I have one relative who had cancer in his jaw, that is different. It remains a mystery, and part of why I want to share what’s going on is that it is occurring in younger people.
People need to get checked and tell their dentist if anything seems off. I just had a canker sore I thought wouldn’t go away.
The “canker sore” on my tongue that turned out to be cancer
At the beginning, I noticed a bump on the left side of my tongue, by my teeth, and I kept hitting it. It was really annoying, and I didn’t know why it was happening. I had just accepted the job with Stratford and was still working at Sephora. One of my managers, who was interested in that kind of thing, looked at it and said, “Yeah, that is weird. I don’t know what that is.”
The mouth heals quickly if you burn your tongue or bite it, but this bump wasn’t going away. Months into my job, I realized that now that I was more settled, I needed to do something because it was starting to hurt. I began avoiding certain foods because they hurt to eat. I went to the local hospital in Stratford and, because there was no walk-in clinic, I went to the emergency room. The doctor looked at it and said I had bitten my tongue.
I am not usually confrontational, but something in me pushed back. I told him it had been like that for months, and there was no way this was just a bite. If it were a bite, maybe there was an infection, but it was definitely something more.
He did not seem to like that I pushed back, but he referred me to an ENT specialist.
Getting the biopsy and the phone call that confirmed cancer
The ENT was fantastic. She said we should do a biopsy because something odd was happening, but she kept saying how young I was (I’m in my 30s), so it couldn’t possibly be cancer in her mind. Still, she booked the biopsy.
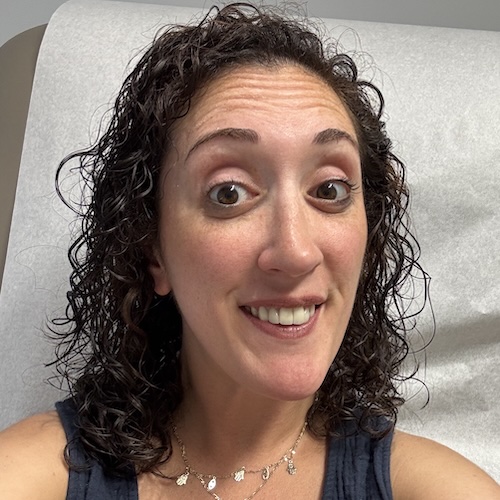
On the opening night of my musical, Dirty Rotten Scoundrels, I was in the middle of a fashion photo shoot for Pride Month. I was doing hair and makeup for friends of mine, working with photographer Neil Graham, and I knew I had a show later that night. In the middle of the shoot, my doctor called and said, “It is cancer.” I was sitting down, and it still felt like the floor gave out from under me.
Who gets told it’s cancer in the middle of a photo shoot before a show? I had to go back into the shoot knowing this, but in a way it worked out beautifully.
My friends and colleagues were there to comfort me immediately. They asked if I wanted to stop the shoot, and I said no, we needed to keep going.
The emotions that came out in that photo shoot made it really special because we created something beautiful out of something awful.
We nicknamed my cancer “Carl”
On the way back to Stratford, I stopped at a thrift store and picked up a beautiful dress I had been eyeing for the opening night party. I had thought it might be “too much,” but after that phone call, I decided if there was ever a time to be “too much,” it was that night.
I told the people who were at the shoot and my immediate team, but I did not want to throw off opening night for everyone else. They were excited and ready to perform, and cancer had already affected me; I didn’t want it to affect everyone else yet.
We started calling my cancer “Carl,” so we could talk about it in front of others without alarming them. We would say things like, “How’s Carl?” “He’s such a jerk,” or “He’s not so bad today,” as our code.
My 10-hour tongue cancer surgery and flap reconstruction
My surgery was what they call a flap surgery. They removed up to about 40% of my tongue to take out the cancerous area. They made an incision in my neck to remove lymph nodes for testing, and because I was already stage 3 squamous cell carcinoma, the staging was serious.
They also used my own body as a transplant. They took tissue from my arm, along with the veins, and used it to reconstruct my tongue and reattach it to my neck. I now have about 60% of my original tongue left, with taste buds that are slowly coming back.
I learned the hard way that my taste buds had returned when a shot that used to taste like water suddenly burned again.
The surgery feels like something out of science fiction. I had staples running up my neck, wires coming out so they could monitor the tissue, and tubes they plugged in that made ultrasound-like sounds to check blood flow. Hearing that living-tissue sound and realizing, “That’s my tongue,” was surreal.
Walking up from tongue surgery and already speaking
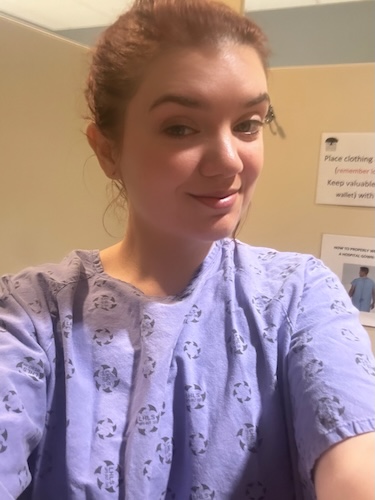
After surgery, I had my arm bandaged, staples in my neck, wires, drains, and an NG tube. The NG tube was actually the most painful part because they placed it on the side of my incision to avoid blocking my airway if the other side swelled. Every time I swallowed, it hit the incision, and the sharp pain became all I could focus on.
They told me I might need a tracheostomy and that I would not be able to speak for a while. I worked with a speech pathologist and had a communication board ready. But when I woke up from surgery, I saw my parents and said, “Mom.” Everyone was shocked that I was speaking clearly enough to be understood.
We still don’t know why that happened. I joke that my own body tried to shut me up, and even that didn’t work. I have always been a yapper, and apparently, even major tongue surgery couldn’t stop that.
Learning to swallow again and choosing radiation
The first focus after surgery was on swallowing. To get the NG tube out, I had to prove I could swallow, but swallowing with the tube in hurt so much that it became a catch-22. My team realized the tube was holding me back, cut the sutures from my nose, and pulled it out, which was not an experience I would recommend.
We started with liquids, then purees, soups, and protein shakes, and I had to relearn biting and chewing. I did tongue exercises with my speech pathologist focused on mobility and strength, and I got up to walk even though I felt like Frankenstein’s monster after a ten-hour surgery. I still do physio for my shoulder because my arm had to stay in one position for so long.
They removed 51 lymph nodes, and one tested positive for cancer. My team explained that while the amount was small, tongue cancers can move quickly. The options were to wait and risk it spreading or to do 30 sessions of radiation, Monday through Friday.
I told my doctor, “Kill it with fire,” and we moved ahead with radiation, even though they warned it would be hard and would affect my mouth and swallowing.
Daily radiation, crushing fatigue, and singing karaoke again
For radiation, I drove from Stratford to London, Ontario, Monday through Friday, a little over an hour each way, for about a 15-minute session. The treatment itself feels like getting an X-ray; the hard part is the cumulative side effects afterward. The team was wonderful about playing music for me; sometimes spa-like Zen music, sometimes upbeat, depending on my mood.
The fatigue hit like a wall. I’m someone who normally operates on very little sleep, so suddenly sleeping a full eight hours was wild. My tongue swelled, and it still does on some days. There are days, like today, that are not my best because of the swelling, but then there are days where I do big things again, like singing karaoke for the first time since surgery.
Before surgery, I hosted a big karaoke night called “Red Sing Out.” I invited people casually, thinking only my small team would show up, and we didn’t even have a real karaoke machine, just music and phones with lyrics.
Instead, stars from the shows I worked on showed up, and they could actually sing, which is so unfair at karaoke. We had a tongue-shaped cake that said “Goodbye, cancer,” and we all cut into it together. I opened the night with “I Will Survive,” and we all sang it together again to close the night.
Returning to the theater after tongue cancer surgery
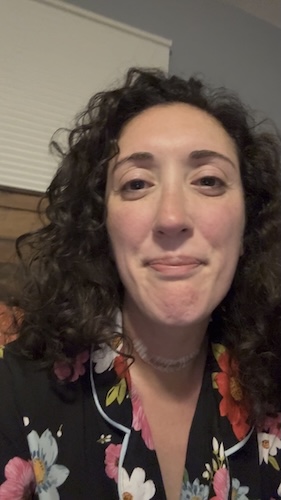
Everyone has their own timeline. If I had not come back for the rest of the season, no one would have faulted me. But I had worked so hard to get there, and the community and the work meant so much to me that coming back gave me something to strive for.
I focused on exercises, stretching, rebuilding stamina, and being physically able to do a fast-moving job with stairs, crossovers, and quick changes. The part I didn’t anticipate was the emotional impact of coming back to the same shows after being so changed. Shows like Anne of Green Gables, where a character dies in a heartbreaking scene, suddenly hit me much harder, even though I’d seen them many times.
Almost everyone at the theater was incredibly supportive. One person treated it as though I had been on vacation and made comments like, “Did you enjoy your time off?” That was frustrating, but some people simply don’t understand.
The positive support far outweighed that; performers and crew clapped for me, hugged me, and shared their own stories of surgery and illness.
Learning to love my scars and advocate for my body
Some people don’t know how to handle someone going through hardship. One colleague would stare at my scars, make faces, and say they were gross. I like my scars; they tell a story and remind me of what I have been through and how I got past it. It is all about perspective.
I have been through trauma before cancer; I am part of the MeToo movement and an assault survivor. Therapy helped me a lot, and I genuinely believe everyone, especially people dealing with cancer, can benefit from therapy. Both experiences involve relearning your body, dealing with inappropriate questions like “What did you do for this to happen?” and refusing to accept victim-blaming.
Making jokes is how I cope, but that doesn’t mean it’s right for everyone. For me, working toward coming back to the work I love, helping tell stories, and telling my own story helps me process everything.
What I want others to know
There are so many big and small moments that come from a journey like this, and there is no wrong way to handle it as long as you are not hurting yourself or others.
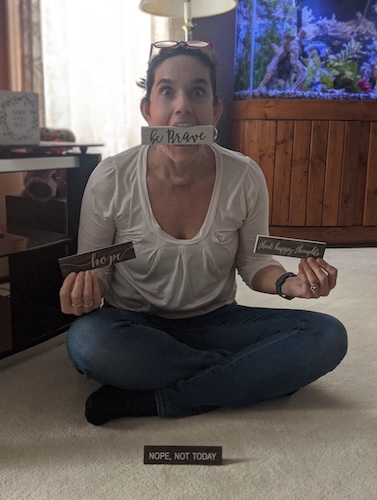
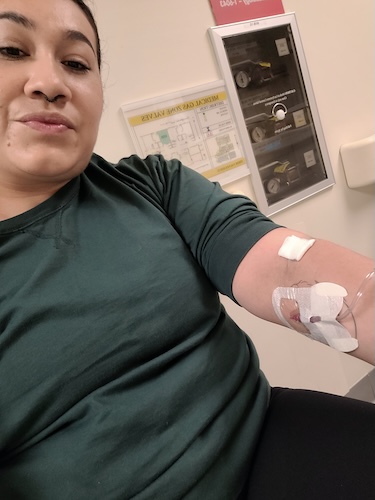
For some, putting on makeup again feels wild; for me, it was part of feeling like myself. I have a photo where my arm is wrapped, I’m wearing a turban to protect my incision and cover hair loss, and I’m in makeup. People sometimes assume hats always mean chemo, but there are many reasons people wear them.
I’m working on projects to help people get the hats they need and to get involved with organizations that help patients with makeup and skincare. Sometimes what helps you feel your strongest is as simple as a moisturizer that makes your skin less dry or a red lip that makes you feel like yourself. Other times, it’s cosplay, horror, or body gore looks that help someone reclaim their body.
As a makeup artist, I try to make beauty tools as accessible as possible. Before my surgery, I taught at a school for the blind because people often assume blind people can’t wear makeup, but they absolutely can if they want to. The same goes for any patient: whatever you need to feel better in your own skin and stronger in your journey, if there is any way I can help, I want to help.

Inspired by Red's story?
Share your story, too!
More Head and Neck Cancer Stories
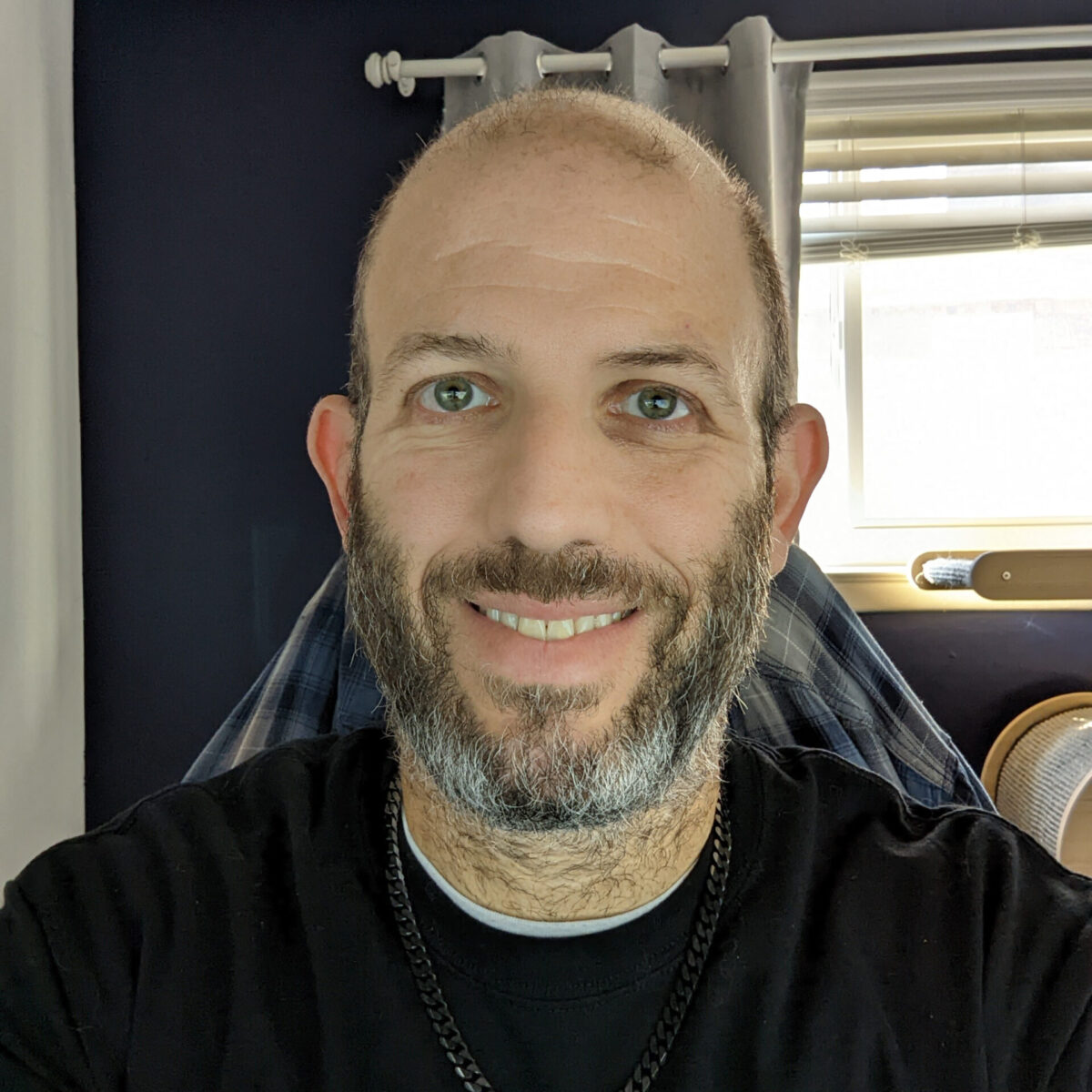
Vikki F., Head and Neck Cancer (Nasal Squamous Cell Carcinoma)
Symptoms: Nosebleeds that persisted for years, nose changed in shape, nasal pain, migraines
Treatments: Surgeries (subtotal rhinectomy, reconstruction surgery including radial forearm free flap, bone grafts, and cartilage), chemoradiation
...
Red S., Tongue Cancer (Squamous Cell Carcinoma of the Tongue), Stage 3
Symptom: Persistent tongue ulcer that increased in size
Treatments: Surgeries (partial glossectomy, flap surgery), radiation therapy
...
Alyssa N., Adenoid Cystic Carcinoma
Symptoms: Persistent jaw pain, lightning-like facial pain during the first bite of meals
Treatments: Surgery (tumor removal), radiation
...
Eva G., Oral Cancer, Stage 4
Symptoms: Sore on the tongue, which caused pain during eating and speaking; changes in the color and texture of the tissue where the sore was located
Treatments: Surgery (partial glossectomy, radical neck dissection, reconstruction), radiation
...
Teresa B., Recurrent Breast Cancer (Hormone-Positive), Oral Cancer (Lip Cancer), and Skin Cancer (Melanoma)
Symptoms: Lip cancer: chapped lips & a pimple-like growth on lip, breast cancer: enlarged left breast with lump, melanoma: none
Treatments: Surgeries (bilateral mastectomy with reconstruction, lumpectomy, craniotomy, Mohs, surgery, wide local excision), hormone therapy, radiation therapy
...