Michelle’s Relapsed Stage 4 Colorectal Cancer Story

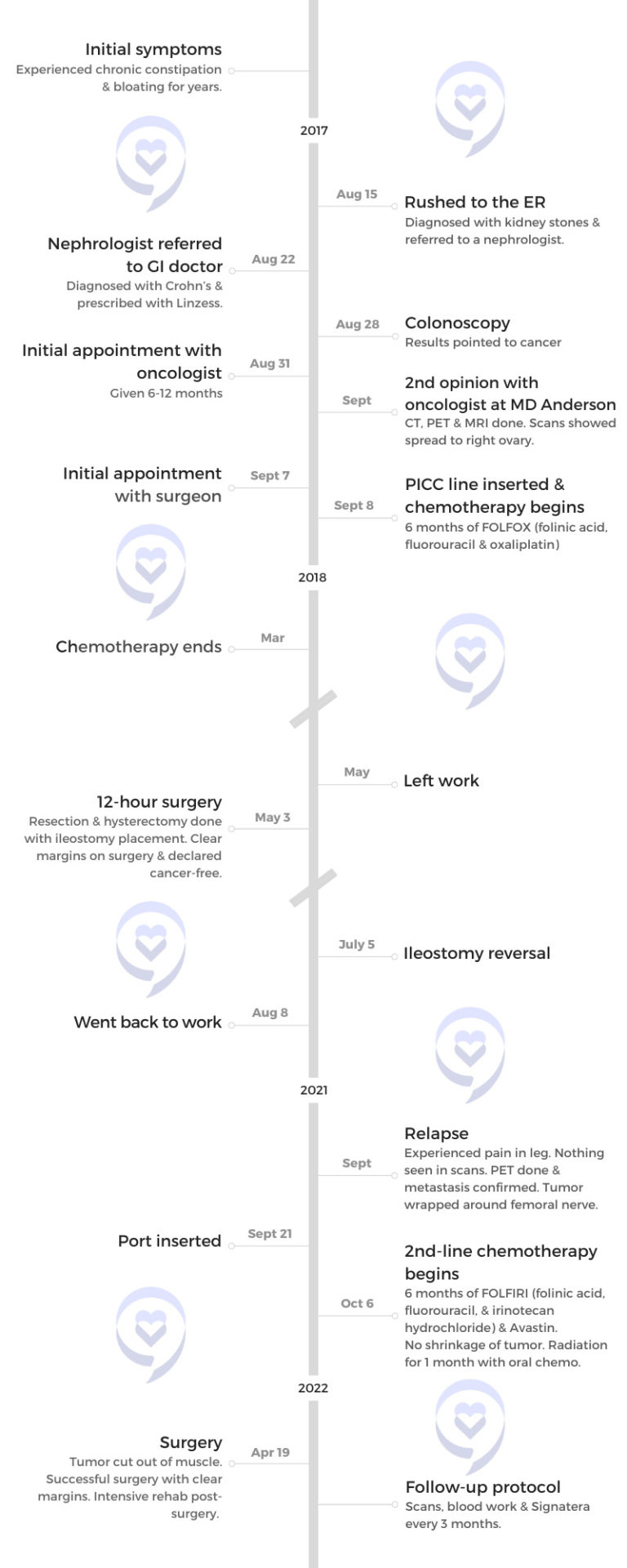
Michelle was first diagnosed with stage 4 colorectal cancer in 2017.
For years, she had been experiencing chronic constipation and bloating, not knowing that these were already symptoms of cancer. An episode of severe pain took her to the emergency room and eventually to a gastrointestinal doctor.
Though her symptoms were similar to Crohn’s disease, her colonoscopy proved otherwise and revealed that she had cancer.
After her initial appointment with an oncologist, she was told that she would have a permanent ostomy and was given 6 to 12 months to live. This prompted her to seek a second opinion.
After chemotherapy and a 12-hour surgery, she was in remission. She had no evidence of disease for two and a half years until she started feeling pain in her leg. A PET scan showed the tumor wrapped around her femoral nerve.
She shares her journey through treatment and recovery, how she was able to work through cancer treatment, the importance of knowing about your disease and advocating for yourself, and how she copes with survivor’s guilt and thoughts of death.
In addition to Michelle’s narrative, The Patient Story offers a diverse collection of colorectal cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Name: Michelle C.
- Diagnosis:
- Colorectal Cancer
- Staging:
- Stage 4
- Initial Symptoms:
- Chronic constipation
- Bloating
- Treatment:
- Chemotherapy: FOLFOX (folinic acid, fluorouracil, and oxaliplatin)
- Surgery
- Relapse Symptom:
- Pain in the leg
- Treatment:
- Chemotherapy: FOLFIRI (folinic acid, fluorouracil, and irinotecan hydrochloride) & Avastin
- Radiation
- Surgery
Introduction
Love big, live big, and do whatever you can in this space to help make other patients’ journeys just a little bit easier.
MIchelle C.
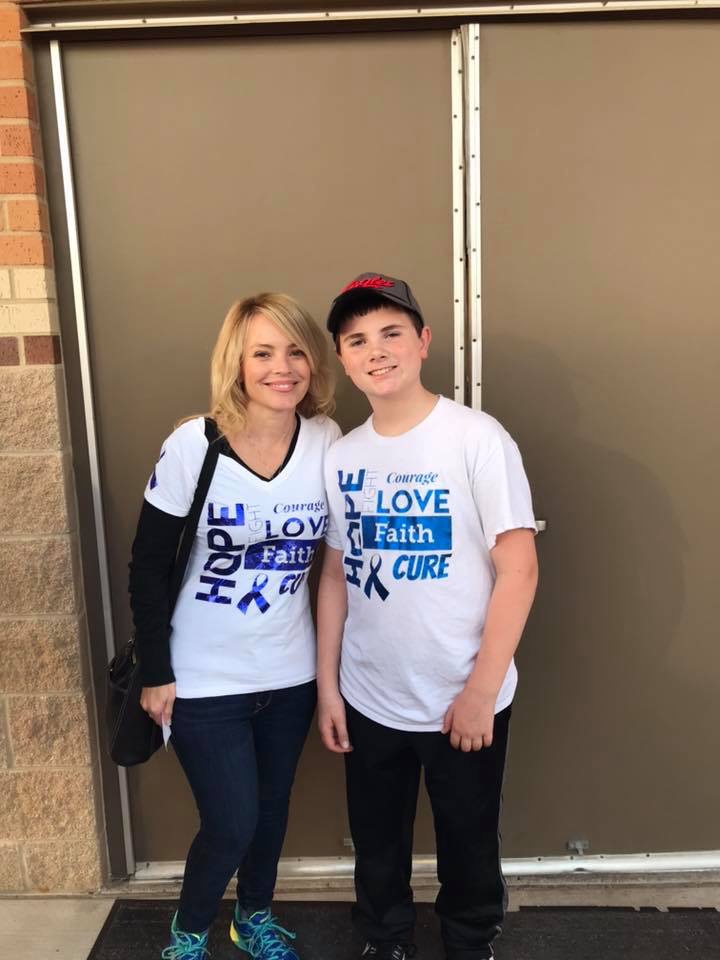
My name is Michelle Capell. I’m a stage 4 colorectal cancer patient and survivor.
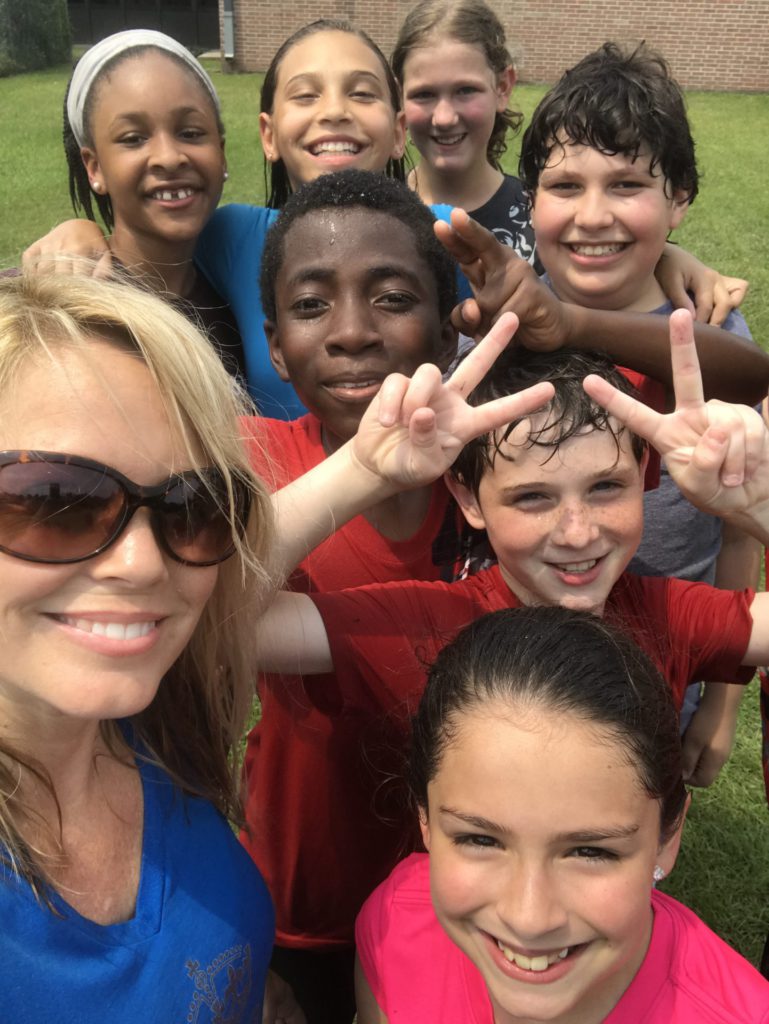
I’m a teacher. I teach fifth grade and have taught fifth grade for 17 years so that is one of my passions. I take my job very, very seriously and really love what I do.
I like to work out a lot and spend time with my little doggy. I have a dog who is part toy poodle and part bichon. She has her own little personality. She’s a little bit aggressive, but she’s special.
I do not have my own family. My students are an extension of my family. They know that I love them. They know that they’re my family. I tell them that. Their families [have] become my family. I’m very close with all of my student’s families. Even though it’s summer, I spend time talking to them [and] meeting up with some of the families.


Pre-diagnosis
Initial symptoms
If anyone really listened to me years ago, maybe this would have been caught a lot sooner.
Michelle C. >>> Read More about Medical Gaslighting
For years, I had tons of symptoms but I didn’t know what to attribute them to. I always had chronic constipation. I was on antidepressants and was told that the antidepressants cause constipation.
The doctors give you a pill to make your stool softer and come out. If someone would have taken the time to figure out exactly why that was so bad for me, maybe it would have been caught sooner.
Looking back, you see all these little things that added up. At a conference once, I raised my hand when a doctor was speaking, and asked, “I dealt with this for years and years and years. Could this cause colorectal cancer?” He said, “We don’t know 100%, but absolutely. With that stool sitting in your colon, that’s bacteria that can form polyps, which can potentially cause cancer to form.”
If anyone really listened to me years ago, maybe this would have been caught a lot sooner. I went through that for years. I had hemorrhoids here and there and still, doctors said, “Oh, well, that’s normal, too. People get that because of constipation.” It’s a golf ball-sized hemorrhoid. It’s very staggering to me.
I was in the bathroom at my parents’ house and I said, “Mom, something’s wrong with me.” She said, “Oh, that’s hemorrhoid.” I said, “It’s the size of a golf ball though.” It’s not what you think a hemorrhoid is like. It was huge. Again, I was pushed off and they said this is another side effect [of] antidepressants.
This still is not sitting right with me, but I listened to what [the] doctors say. They’re the experts. They know what they’re talking about so I listened to it all. I took it all in. Increase your fiber, increase your water, watch my diet, all of those good things, but it never seemed to really get any better.
I was always very bloated as well and I worked out a lot. I went to doctors for that and they told me I was gluten sensitive, which runs in my family. They said, “You’re borderline celiac so that’s why you’re so bloated all the time.” I cut gluten out and still didn’t get any better.
I’m trying to do all these things, but something’s still not adding up. Then finally, it became [to] point [where] I could no longer work out. I had excruciating pain in my stomach. I was doing a lot of spinning classes. In the spinning classes, you bend forward a little bit so pressure was put onto that area. It hurts. I would get off the bike. I would walk around until it felt a little bit better then I would go back to class and finish. I really didn’t know what it was.
I had a friend in class who was a nurse and she also had Crohn’s disease. She said, “It really sounds like Crohn’s. Here’s the name of my doctor. He’s great.” I was going to make an appointment with him and then the pain got so bad, I could barely walk.


Abdominal pain intensified
I lived in Houston by myself. I don’t have family here so I drove myself to the medical center. I walked around the streets of Houston literally bent over, trying to decide what E.R. I was supposed to take myself to.
I ended up in the E.R. They did a scan and told me I had multiple kidney stones in both kidneys, which was also something that I chronically dealt with my whole life. I said, “No, I’ve had kidney stones. I’ve had surgery for kidney stones. I’ve had lithotripsies done. This isn’t the same pain.” They brushed me off, too.
But in going there, I got another doctor. He was a referral. I only saw him for five minutes, but he said, “I want you to make an appointment. I’ll see you this week.”
He saw me and I brought all of my history. He said, “To be quite honest, I don’t know what’s wrong with you.” He was very matter-of-fact. He spoke to me like he was speaking to a friend. He was very nice. I got so blessed to get this amazing doctor.
I was in tears. I said, “I don’t have weeks to see a specialist because I’m in pain right now.” He handed me his phone and said, “Please put your name and number in my phone. I am going to contact my friends and tell them to get you in immediately. You’re not going to have to wait weeks.”
Initial appointment with a gastrointestinal doctor
I had all these doctors set up, but the first one I was a GI doctor because we thought that’s the direction we were headed first. He, too, said, “This really does sound like Crohn’s,” so he put me on Linzess to make me go to the bathroom and flush my system out. But he said, “I still have to schedule a colonoscopy just to confirm.” I was 40 at that time so I still wasn’t old enough to need a colonoscopy.
Getting a colonoscopy
I went for a colonoscopy. My friend who took me was my 34-year-old friend who already had lost both parents to cancer. It was unfortunate that it was her that took me.
I came out and they come and talk to you a little bit. He basically said, “What I saw in you, I wasn’t expecting to see. And when I see it that bad, it’s not just in your colon.” I was still digesting everything and still weaning off of the medication.
When we got to the car, my friend said, “Do you understand what he said to you?” I said, “Yeah, I think so. It’s that I have cancer and it’s bad.” She said, “Yeah, that’s what it sounds like.”

Diagnosis
Reaction to the cancer diagnosis
“She was giving me anywhere from 6 to 12 months at that point.”
Michelle C.
At that point, I was very hopeful and assumed that because I was healthy, worked out, and was young, this was going to be a small cancer that we were going to just cut out. I was going to move on, make sure I ate better, and do all the things I thought I should do. That’s not how it went at all.
They sent me to Texas Oncology and they did some scans themselves. I met with the oncologist there. She was recommending chemo first then surgery and I would have a permanent ostomy. She was giving me anywhere from 6 to 12 months at that point. I said, “No, I’m going to get a second opinion.”
When I looked at her business card, she had ten different cancers under her name and I said, “I don’t mean any disrespect, but you’re not a specialist and I’m going to see a specialist. I obviously need someone who deals [with] just colorectal cancer and someone who sees the toughest cases every day. I don’t want to go to the doctor that sees one tough case once a year. I want to go to someone who sees the toughest cases every single day.”
I was very freaked out. This was all going on right at the beginning of my school year. I was not there [during] the very first week of school. My principal was not happy. She thought I just needed a routine exam. I said, “Something tells me this isn’t routine. I have to go. I have to figure this out.” She felt guilty when she found out. She said, “Oh my gosh. I really tried to stop you from going and you really needed to go.”
Getting a second opinion
I went to MD Anderson. They do all of their own scans. They will not take any tests from any other hospital. They did the CT scan, PET scan, MRI, echocardiogram. and I had a biopsy scheduled as well. At that point, we weren’t sure exactly what stage. We didn’t know if there was lymph node involvement. We didn’t know if it had metastasized.
I was in an O.R. getting prepped for a biopsy of my kidney. While I was on the table, they called and said, “Nope, stop now. We can already tell radiologists read the report. It has metastasized to her ovary. She’s stage 4. It’s not going to matter. We need her out. We need her to start treatments immediately.”


Treatment
The surgeon that I saw was amazing. He pulled down a chart of the anatomy of the body. I was double-sided. I had a tumor on my right side and on my left side so technically, I was colorectal. I was colon and I was rectal.
They do tumor boards where they discuss the case. They wanted to know which one was the primary tumor. Was it colon cancer? Was it rectal cancer? The tumor board was split down the middle. They couldn’t make a decision and I said, “I don’t really care. Just get it out of me. It doesn’t matter to me.”
They were trying to figure out: with the metastasis, where did it come from? Did it come from the colon or did it come from the rectal? Where was my spreading going to be? Because it was just not the typical metastasis for a CRC (colorectal cancer) patient. It’s just not what you normally see.
I did the genetic testing and it’s not in my family. I don’t have FAP (familial adenomatous polyposis), I don’t have Lynch, I have none of those. The fellow who did all the tests said, “I don’t know what to tell you other than you have really bad luck. We can’t find any reason.”
The surgeon said, “I’m going to cut here, I’m going to cut here, we’re going to resect it. You’re going to have a bag, but don’t worry about it. I’m going to be able to reverse it. We’re going to do chemo. We’re going to shrink it. We’re going to do this, we’re going to do that.”
This is the guy I want. I want this guy because at least he’s giving me some hope. He’s not giving me a timeline of X amount of years to live. I felt so much better with my team there.
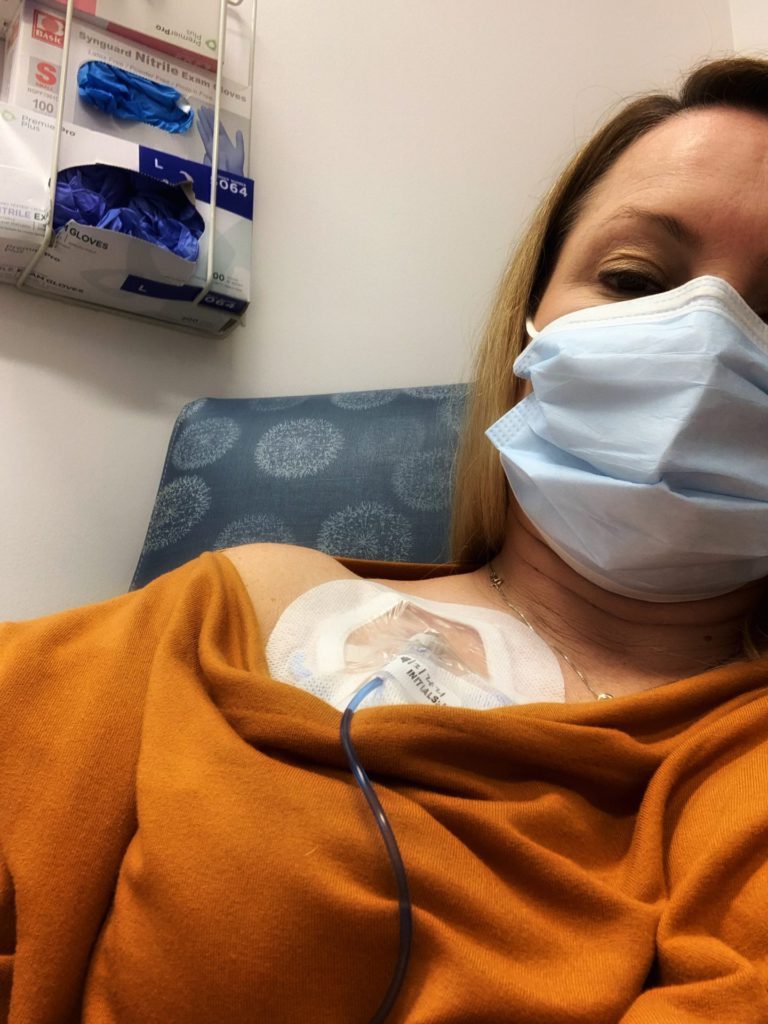
I met with my oncologist after that and my oncologist said, “You need to be in the chemo chair this week. We don’t have time for a port.”
I was still trying to process it all. It was so much to take in. I said, “I don’t even know what that means. What do you mean I don’t have time for a port?” A port is another surgery and it usually takes a week or two. He said, “You don’t have a week or two. We have to start immediately.”
Chemotherapy
Within two days, they put a PICC line in my arm and I was in the chemo chair that night. I would get chemo Friday nights then I would infuse Saturday and Sunday.
My chemo regimen was Friday, Saturday, [and] Sunday so that I could continue working. I would leave work a little bit early on Friday and get home at 11:00 and then I would have treatment Saturday, Sunday, and then drop the pump back off Sunday night.
I had six months of FOLFOX (folinic acid, fluorouracil, and oxaliplatin) at that time. I worked through all of that and I took every precaution I could.

Working during cancer treatment
My principal [and] the counselor talked to my students before I came back. They asked my permission. They told them, “She might lose all her hair. She’s going to be tired. She’s going to be this, she’s going to be that, but just watch for these things in class.”
They wrote a letter to the parents explaining what was going on with me. To be quite honest, I was blown away. I assumed the worst. I thought, I’m going to have all these parents that want to pull their kids out of my classroom because [they] don’t want [their] kid to have the teacher with stage 4 cancer all year. Who knows what’s going to happen? None of the parents did that. They were all completely supportive. The kids were wonderful.
I told my doctors, “You’ve got to get me through [the] testing season. After state testing season is done, I can do whatever needs to be done.”
They didn’t do radiation the first time because I was very responsive to FOLFOX. My CEA went down drastically so my body really responded really well. FOLFOX is very tough. It’s not an easy chemo, but it did its job for me.
Side effects of FOLFOX
Being a school teacher, I had 28 kids that depended on me all day long.
Michelle C.
Cold sensitivity is a huge thing. I wore gloves all the time because I would forget. You grab something from the fridge and if I forget, I would drop something and break it because it feels like shards of glass. It’s a horrible feeling.
I had a lot of nausea with FOLFOX. I lost a lot of weight. I got down to about 84 lbs so I looked sick for sure. They put me on prescription-strength weight gainer shakes at one point
I didn’t lose all of my hair. I have a ton of hair. I lost half of it so I had normal hair for once. I assumed I was going to lose it all. It started falling out.
People looked at me, and said, “You don’t really look sick.” When you say that to cancer patients, it’s really rough. I know people are trying to be nice when they say that, but it’s almost like a slap in the face. I would love to tell you I’m not sick, but I’m super sick, I might not even make it. I’m that sick. It’s frustrating.
I would get super tired. Being a school teacher, I had 28 kids that depended on me all day long. If I sit down and they see me about to literally close my eyes, they knew to go and get another teacher to come into the classroom.
The chemo has an accumulation effect. In the beginning, it doesn’t seem so bad. A little bit is left in your body so it keeps building on itself. By the end, it’s a lot. I could barely stay awake.


The other thing that my principal allowed me to do was when my kids went to PE or Music or wherever they went, teachers were told not to disturb me, not to go in my classroom. I turned the lights off. I had a pillow and a blanket, laid down in the back of the room, and I would pass out.
I would literally pass out for 45 minutes and I would have to set an alarm on my phone to go get my students or someone else would go pick them up for me. But that 45 minutes helped get me through the day. Had I not had that, I don’t know that I would have made it through work because you get that tired.
FOLFOX is rough and not everybody can make it through all of the oxaliplatin. That’s the one with the cold sensitivity. It causes neuropathy.
I had neuropathy in my hands and feet. The first time it happened, I was laying on an air mattress and I went to get up and completely fell. I couldn’t even use my feet. I wiped out completely. I wasn’t prepared for that at all.
One of the places [where] I first felt chemo enter my body was in my female parts. Everything felt like it was on fire. Either my mom or my best friend usually went to infusions with me. We joked about it and I didn’t think twice about mentioning it to my doctor or my PA.
It closes all of your parts down there. It just kind of shuts them all and I didn’t really know that. How would you know that? It got warm and hot.
When I finally mentioned it to my PA, she said, “Oh my gosh, why didn’t you tell me this? There were things that we should have done for you that we didn’t because we didn’t know this.”
Tell your doctor everything you’re feeling, every little side effect you’re experiencing. Speak up, even though it might seem little or insignificant to you.
I ended up having to go through pelvic floor therapy to help put those pieces back together the way they should be working and to make sure they were functioning.
A lot of people don’t know about pelvic floor therapy. It’s wonderful for colorectal cancer patients. They’re able to do wonders. I was able to do that for probably about eight months.
I was getting good results. They said, “Your CEA level is lowering. We know the tumor is shrinking. Your CT looks great.” I’m getting good news so I’m not thinking of these little things being of any significance. The more you know, the more you’ll speak up.
Now I tell people, “If you’re female and you experience this, tell your doctor. There are things that they can do to prevent something from happening.”


Getting a nerve block
All that stuff gets painful, too. Cancer is very painful. At one point, they put me in a wheelchair because I had a tumor that was pressing on a nerve in my spine. That was rough. Nothing they gave me touched the pain at all so they wanted to do a nerve block.
I went in twice for the nerve block and backed out twice because I could hear people screaming. I said, “No, this isn’t for me. I don’t know what’s going on here, but people are screaming and this doesn’t sound good.” Finally, the third time, I said, “Okay, in order for me to keep working, I have to do this.”
When they do a nerve block on you, you’re in what looks like a CT scan, but it’s a small circle. They do that so that they can see where they’re putting the needle in your spine and it guides them. What I didn’t know at the time was that they were letting a fellow do it.
You’re awake through the whole process. I can hear my doctor giving directions to someone. I can hear her telling him, “Pull up, pull up, pull up,” then all of a sudden, the entire right side of my body started convulsing. I was shaking on the table.
Now I know why people scream because they’ve hit a nerve. They got the wrong spot. Obviously, it must be something that happens because I heard other people yell and so it must happen.
I’m sure it’s somewhere in the fine print that you sign saying this is a teaching hospital. I told the doctor, “Don’t ever do that, letting a fellow do a procedure. You knew how worried I was about having this done. You knew it took me three times to even come in. You shouldn’t have done that to me. Please don’t do that again. That was horrible.”
But that in itself saved me. I got out of the wheelchair. I was able to walk [and] that got me all the way through to surgery. Chemo was shrinking everything, too, so I don’t know if it was just the nerve block or the chemo that was shrinking everything.
Those are some of the bad side effects of FOLFOX. I still have neuropathy. It’s a severe cold sensitivity.
I’ve had instances on airplanes where I’ve had what appears like a seizure and I end up kicking and hitting everything. I can’t control it because I get too cold. I had several blankets. I pack a bunch of blankets in my carry-on so I can put the blankets on top of me.
Getting information from support groups
I was active in different Facebook groups so I knew what other people experienced. Everybody experiences neuropathy a little bit differently. Some people get tingling in their hands and their feet. I had it a couple times in my feet, but mine is more of a full body thing.
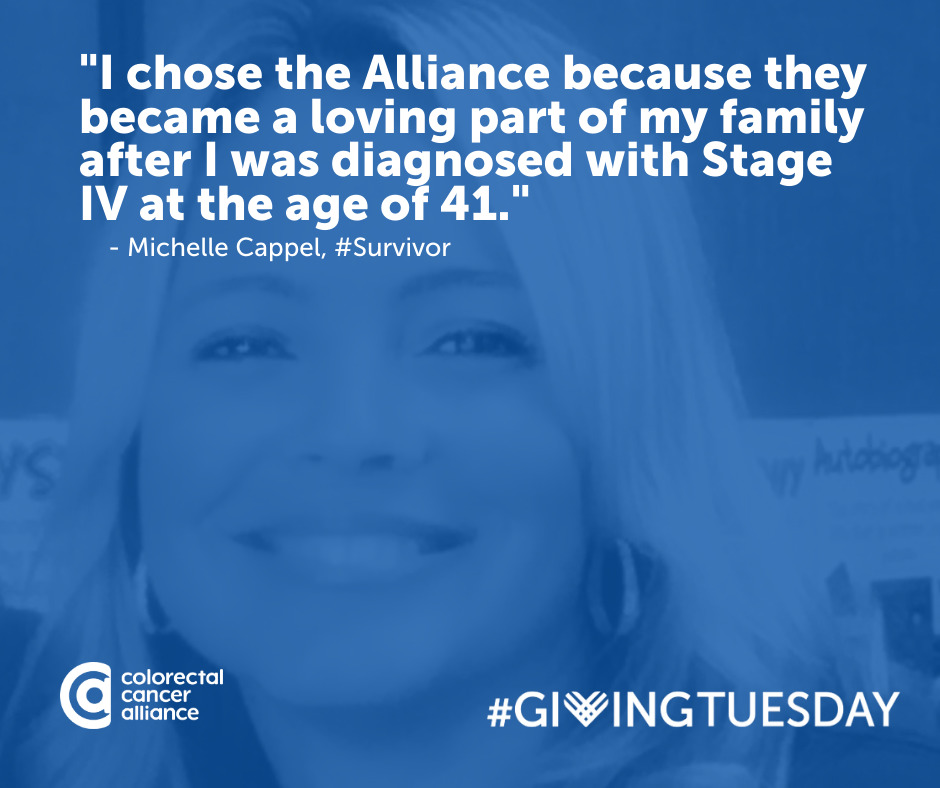
The patient advocacy groups are what helped me navigate through treatment. If it weren’t for them, I don’t know how I would have gotten through that. The doctors don’t tell you everything you need to know nor do they probably understand and know them for themselves. They don’t understand.

Surgery
I went in for a 12-hour surgery. When the doctors came out to talk to my family and friends that were waiting, they did admit that they really thought they were going to open me up and not be able to help me.
They anticipated finding so much cancer inside of me that I was going to be an open-and-close case. They said it was nothing short of a miracle that they were able to perform the surgery and get clear margins.
MD Anderson doesn’t do maintenance chemo. They don’t believe in it unless you have residual cancer after surgery.
Preparing for surgery
After surgery, I had an ileostomy.
I put complete faith in my doctors. I really didn’t ask a ton of questions because I loved my team. I have a very strong faith as well. Between my faith and my team, it was out of my hands. Whatever was going to happen was going to happen.
I remember being in pre-op with my parents and I don’t remember crying or anything. They were, of course, but I was very at peace with what was happening. My surgeon and one other surgeon, another fantastic doctor at MD Anderson, had spoken to me at length about my surgery.
I wanted to do HIPEC (hyperthermic intraperitoneal chemotherapy) surgery. He was the guru at MD Anderson for HIPEC and he said, “You’re not a candidate.” He came in on his day off, in his golf attire, and talked with me for about an hour about why I wasn’t a candidate.
He said, “Listen, I’m talking to you like you’re my sister. If you were my sister, I would not be telling you to have HIPEC. It’s intense. You won’t be going back to work. Forget about work for at least a year. This is not something we take lightly. We don’t just pour hot chemo in someone if they don’t need it. You don’t need it.”
After talking with him, I said, “You’re still in on my surgery.” He said, “I am? Why? That’s not my thing.” I said, “I requested you and my surgeon is good with that.”
He ended up actually doing the hysterectomy part of my surgery, even though it’s not what he does. He was in there with the team as well. The number of people that were in there was incredible. It was a 12-hour surgery. I had no idea it was going to be 12 hours nor did they because they thought I was going to be open and close.
They were able to get everything. I had 14 positive lymph nodes as well as metastasis to the ovary. They could have just taken the one ovary, but we discussed it and said, “Since this seems to be like your progression and yours is going downward for whatever reason, we’re just going to take it all out.”
I was 40 years old. I said, “Okay, take it all out. I don’t care. Get rid of it. Get it all out of me. I don’t want to deal with this.” I was very, very lucky that they were my doctors for sure.


Reaction to the results of the surgery
The first people to get the news were family and friends. My mom is a stay-at-home mom. She didn’t go to college, but she probably should have been in the medical field because she wanted them to draw her pictures. They literally pulled out napkins and started drawing pictures for her of exactly what they did, where they cut the tumor out of, and they went through all of it with her, which she just loved.
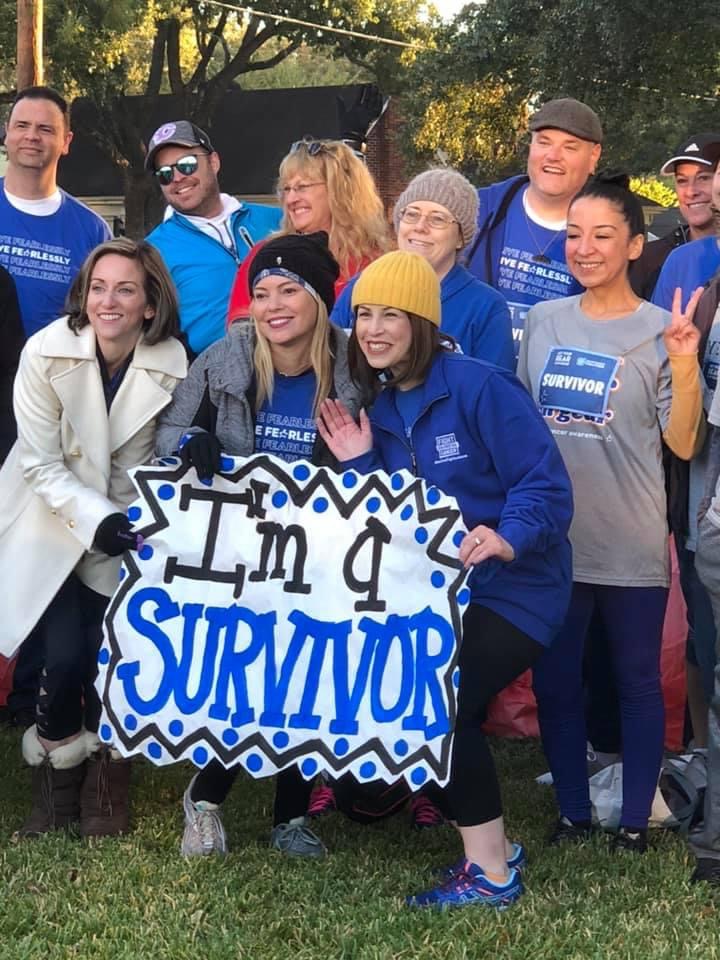
When I was told that it was completely gone, that’s a relief. I made it through the six months of chemo and now this. Thank God I’m still here because my first opinion told me I wasn’t going to make it this far.
Recovering from surgery
There was no room for me on the colorectal floor. Their floor was completely full. That’s how much colon cancer is on the rise in younger adults. I ended up on a cardiac floor.
When I was in the hospital, I had my cordless flat iron with me. Every morning, I would iron my hair, put a sparkly headband on, put some makeup on, and I would go for walks. They would all laugh at me. I said, “I need this because I need to feel like me and this gives me a little bit of sense of getting back to who I am and it’s giving me strength to get up out of bed and walk.”
I would walk and walk and walk. The nurses thought it was hilarious that I took all this time to get ready and nobody’s there but me. I’m there walking and doing everything I can to get out of there because, at that point, I didn’t want to be in there.
No evidence of disease
No maintenance chemo
When they told me no maintenance chemo, that was a tough pill to swallow. You feel like chemo is your safety net. I felt like something was being pulled away from me. I knew that a lot of stage 4 patients get put on maintenance chemo. I said, “What do you mean I’m not getting put on something to prevent it from coming back? How am I supposed to prevent it from coming back if you’re taking this away?”
I pushed and I went to the head of colorectal oncology. I spoke with her and she said, “We just don’t do it. If it’s clear margins, that’s a successful surgery. We do not believe in giving patients poison in their bodies if they don’t need it.
“To be honest, you’re stage 4. You’re going to need chemo again at some point in your life, more than likely. We don’t want you to build up a tolerance to it and have it not be effective the next time you need it. It’s not something that we just take lightly. We don’t just give it to people like that.
“Now, had you had a surgery where they came out and said, ‘There’s still some residual cancer left,’ or it’s in your bloodstream or something, then you get put on maintenance chemo. For you, you had a curative surgery so we do not recommend that at all.”
It’s rough. When you know you’re stage 4, it’s different. We don’t have good stats as far as recurrences. I felt like I needed something to help protect me.


I researched every kind of holistic treatment there was. Anything I could do, I did. Any foods I could eat, any supplements I could take, I did it all because I felt like I’ve got to do something.
I’m getting the cooking for cancer book. I’m taking supplements. I’m working out. I’m making sure I’m doing all the things that are keeping me alive and healthy.
Keeping active was really important. I worked out all through treatment. I put my chemo pump in a backpack and go to the gym. I took a dance class so I would put the backpack on. A couple of the girls in the class were nurses. They said, “I can’t believe you’re doing this. You shouldn’t be doing this,” but they would make sure that they’re around me in case something happened.
Staying strong and staying active probably helped, too. Even though I got really, really thin, keeping up with trying to stay physically fit does help in recovery.
Reaction to being cancer-free
I moved to Houston to be closer to some friends who ended up moving away. I was really contemplating moving back to Chicago. It was a really hard time in my life because I didn’t understand. I said, “Okay, God, you brought me here and now I don’t know why I’m here because I don’t have these kids to love on in my life anymore so why am I here?”
Then when I got cancer, I said, “I’m at the best place possible. People travel from all over the world to come to this hospital and I have this opportunity to be blessed with these doctors that are miraculous.”
The doctors telling me and giving me these reports, “You’re still clean. You’re still no evidence of disease.” I can breathe easy for the next three months. I can live my life. I don’t have to think about it 24/7, even though it never leaves my mind. It just doesn’t. Stage 4 doesn’t. It’s just there.
Any little feeling, you think it was cancer. Even though it’s great, you’re NED, it’s still not easy. It’s wonderful, but it’s still not easy in any shape or manner at all.
It was great until it wasn’t.

Relapse
Symptoms manifest in the leg
It was about two and a half years, almost that three-year mark. At three years, you go from getting three-month scans to six-month scans. I was really looking forward to that. If I could make it to six months, that’s another win I’m going to take.
COVID hit so I wasn’t going to the gym. I started running more. I went from running all the time to, all of a sudden, barely walking a full lap. I was limping a little bit and had pain in my leg.
I went skiing that year and I couldn’t turn. The first day, I was okay. But the second day, I couldn’t turn my skis. I could only go in one direction. I kept going to the mountain and I can’t go back the other way. We got ski patrol to get me down the mountain because I couldn’t. We thought I was really tired. We weren’t thinking [of] cancer because it was my leg.
They didn’t see anything in my scans. I said, “There’s something there. I am telling you it’s there. You’re telling me you’re not seeing it in the CTs. I’m telling you it’s there. I don’t care what the CTs say.”
It depends on the radiologist who reads them. It depends on the person who does your scan and how they move you and how they position you. They’re looking everywhere, but they’re not really zeroing in on my leg.
I said, “No. Something else has to be done.” I think they just wanted to quiet me down. They said, “Okay, we’ll order a PET scan.” It lit up like a Christmas tree.
PET scan results
I got the report from my oncologist. Oncology and surgery are very different in how they talk to you.
Your oncologist is with you from the time you’re diagnosed all the way through, especially stage 4. They are going to be with you through your whole life. Your surgeon is only going to see you if and when you are surgical. If you are not surgical, you’re not getting into a surgeon’s office because they’re not going to waste their time.
My oncologist told me, “It’s in your femoral nerve. It was relatively small.” Again, I’m going down the road of, This isn’t that bad. We’re going to get it. We’re going to cut it out.

Stage 4 Colorectal Cancer Treatment
I didn’t want to be cut fully open again. I messaged my surgeon and said, “Can we go about this laparoscopically this time or robotic? Can we do something different besides cutting me all the way open?” I got a message back immediately and he said, “You need to come in tomorrow. We need to talk.” I thought, Oh, crap, that’s not good. That’s not good at all.
When I went in to see him, he said, “I know it’s small. I get it. I get where your head is. It is small, but it’s probably in one of the worst places it could be. It’s wrapped around your femoral nerve.
“If we have to do something to this nerve, you might possibly never walk again, need a walker, need a cane — we don’t know. But we have to be prepared for all of these things. This is bad. This is not good at all.”
I left there thinking, Oh, geez. Okay. At the time, I lived [in] a third-floor apartment. I quickly had to pivot and find a house that was handicap accessible because I wasn’t sure what was going to happen.
When I met with my oncologist, they put me on second-line treatment FOLFIRI (folinic acid, fluorouracil, and irinotecan hydrochloride) and Avastin for six months. That was a little bit easier to tolerate.
Side effects of FOLFIRI
My oncologist and I joked around about that one as well Irinotecan is part of that one and colorectal patients call that “I ran to the can” because it causes severe diarrhea.
I said, “Oh, so you’re putting me on I ran to the can?” He said, “No, no, no, it’s really not that bad.” I said, “Oh, have you had it? Because maybe if you’ve had it, then I would believe that from you. But the patients that I talk to are stuck in the bathroom for a really long time so I don’t know.”
There was some of that. It definitely wasn’t as bad though as what I thought it was going to be. Now, that’s not true for everybody though. Everybody responds differently.
I wasn’t as tired. I did gain a ton of weight. I gained about 40-some lbs, which was the complete opposite [of] the last time. This is crushing me, too, because now, I feel horrible about myself and what I look like and I feel disgusting.
That was a tougher pill to swallow because I’d always been so healthy. I’d always been so tiny and I’m very short. Extra weight is just hard.
I would say that chemo regimen wasn’t very effective. It didn’t shrink anything. The doctors told me that doesn’t mean that it wasn’t successful. They said it is successful because nothing grew. I get that. However, would I have been the same just jumping into surgery or jumping right into radiation without doing the six months?
To me, it would have been the same thing. Obviously, you don’t know until you go through it so there was no way for them to know. But after the first couple of scans, things weren’t changing drastically. They said, “Okay, this time, you’re going to have to have radiation.”
Radiation
I had radiation every day for a little bit over a month. They give you oral chemotherapy and they give you radiation.
I did not have targeted radiation. Even though it was on [the] lower part of my body, it still goes [to] other places because it spreads. Once it gets in there, it spreads. Radiation isn’t always good. You don’t really want radiation if you don’t have to have it.
It seemed that radiation was doing its job. Radiation was shrinking things. Even though I didn’t want to do it, it’s what worked for me at that time.
After, they give you about a month break to rebuild yourself, make sure you’ve got energy, you’re ready to fight again.
Surgery
We had all kinds of people in that surgery. There was a team [of] about six people ready to resect the nerve. My radiation oncologist had a team in there because she wanted to do internal radiation. We didn’t even discuss this. Then my normal surgical team again.
When they and opened up, they were surprised once again. Radiation moved it off of my femoral nerve. It was inside my muscle and my inner thigh. They ended up having to cut into the muscle to get it out.
I was very blessed because the head of ortho was two surgical rooms over. They called him in quickly and said, “Can you consult on this patient and tell us just how much we can cut out of the muscle in her leg [and] she’s still going to have function? Can we get all the cancer and still give her mobility?” They didn’t want to cut too much but they also didn’t want to not cut enough and not get all the cancer either.
He came in and said, “Cut here. You’ll get it all and she will have mobility back,” and that’s what happened. They were able to tell my family once again that I had a very good surgery, clear margins.
They didn’t need to resect the nerve like they originally thought. They didn’t have to do internal radiation, which they planned on doing. All of that was taken off the table. All they had to do was cut it out of the muscle in my leg.


Recovering from surgery
They put me on the rehab floor, which was the best because I had occupational therapy and physical therapy. I had physical therapy twice a day and occupational therapy once a day.
They get you up and moving. It’s not just walking. You walk on the balance beam. You take some stairs. You’re walking these stairs as slowly as you have to do it.
I was probably in there for almost two weeks and I didn’t want to leave. At that point, I had gotten so close to that team. They were just so wonderful that I said, “I don’t want to leave. You’re helping build up my strength. I’ve bonded with all [of] you people. I look forward to seeing you every day.” They laughed and said, “That happens a lot. People don’t want to leave, but we do need the bed so you are on your way to being healthy.”
They graduated me and put me into their rehab facility. I went through another six months of physical therapy. They weren’t sure if I was going to get feeling back on the inside of my leg; that never happened.
We tried several different things. My OT had me try different things — rubbing a brush on the inside of the leg, taking a massager and massaging that area, and trying to stimulate it anyway I can.
We did that for a while and it was not going to come back. I don’t have feeling on the inside of my leg. In the grand scheme of things, that’s okay. I can walk. I can still work out.
I’m working with a trainer to build up the muscle in my leg. At first, I could barely drive because my right leg couldn’t push on the pedal. Even though I can walk, we didn’t think about building up the calf and shin muscle to push the pedal down. I couldn’t drive at first.
Even though I went back to work, I had someone driving me because I could get in an accident. My foot could easily slip off the pedal and I’m going to hurt somebody else in the process because I think I’m strong enough and I’m not. I’m still building up that area. It’s a process. It takes time.
Follow-up protocol
Every three months, I get my CT scans, blood work, and I do Signatera. Signatera detects cancer in your blood. The hope is that they can detect cancer in your bloodstream before a tumor forms. That is relatively new. I think it’s a great tool to have, one more tool to add to my bag.
At first, my doctors weren’t on board with it and now they are. It’s taken them some time and some of their own research to validate this test.
They said you only need one. I said, “That’s not true. I talked to the company that makes the test. They told me your very first one is your baseline. You still have to do it every three months. It’s not a one-and-done.” I used to have to ask them to put it in my chart. Now I don’t even have to tell them.
People didn’t know what it was. The doctors weren’t pushing it and people didn’t know to ask for it. Now people are finally on board with this. People know what it is or the doctors are finally prescribing this for their patients along with their blood work.
My last scan, I thought something was wrong. I didn’t feel so well. I was getting sick a lot and [had] a lot of digestive issues. I told my doctor, “Something’s wrong. I feel like I have food poisoning. It’s not a blockage because it’s coming from both ends. Something’s not right at all.”
When everything came back clean, he said, “I know exactly what this is. You’re getting sick from your students,” which I never did before. “What’s happening is after COVID, people get sick and they can’t kick it as easily as they once did because our immune systems are not what they once were.
“We were masked. We were isolated from all germs for so long. Now that all of this is reintroduced to our bodies, our bodies can’t fight these off anymore the way that they used to.”
It went away, but it scared me for a couple of weeks. What happened with COVID, it makes sense.
Managing scanxiety
Scans aren’t fun. Leading up to them, that week going in, you don’t get a lot of sleep. It’s always in the back of your head. Even if you feel like things are okay, you just never know, especially being in the space that I’m in.
Thoughts of death
Dying from this disease is a very painful death. Death doesn’t scare me; it’s the pain that scares me.
Michelle C.
The more you do advocacy work, the more people you meet. The more patients you learn to love on, the more patients you lose.
I’m always upset when I lose someone I know. It freaks me out a little bit, too. I think, They were stage 4, too, and they were doing so well for so long. Look what happened to them.
I shouldn’t feel like that because, to me, that’s being selfish. I’m turning what happened to them onto me. But I can’t help myself. I lose someone and I mourn and grieve for that person, but then at the same time, I think about my own morbidity.
It’s still a very real thing for me. I’ve done very, very well. How long am I going to be able to defy the odds? Right now, I am one of the miracle stories of my doctor. But for how long, I don’t know. I would love to say forever, but at some point, I feel like I’ll die from this disease.
Dying from this disease is a very painful death. Death doesn’t scare me; it’s the pain that scares me. I’m okay leaving this life. I’m not okay leaving in severe pain.
I want to be able to say goodbye to loved ones. I want to be able to spend time. Often, people are so drugged up because they’re in such excruciating pain that it’s hard for them to even get the opportunity to do that with their loved ones and their family.
You never know when that’s going to happen so you have to live your life in a different way. Make every moment count. Love everybody in your life. Love big, live big, and do whatever you can in this space to help make other patients’ journeys just a little bit easier.

Coping with survivor’s guilt
You just want to make sense of how other people not making it.
Michelle C.
I had a big discussion with some people about survivor skills. Those of us that survive that watch other people.
I, specifically, deal with it because I’m single. I don’t have a husband. I don’t have kids. I watch other people pass away that leave their husband and that leave their kids. I question that. It would be so much easier for me to be checked out versus you being checked out and you leaving your little child with no mom or no dad.
Somebody said, “The word guilt has a negative connotation and what you’re describing is not negative. It’s coming from a place of empathy. It’s coming from a place of compassion and caring. It’s not coming from a bad place.”
One of my friends said, “I’ve got it. It’s survivor’s compassion. It’s not survivor’s guilt. Let’s take that guilt word away, take that negativity away, and put a different word in there that makes it sound like you’re more caring.”
It’s still hard, but that was a very needed conversation. A lot of people feel guilty and go through all those stages and it’s hard. It’s very negative in thinking and you’re not being negative. You just want to make sense of how other people not making it.
Words of advice
Be your own best advocate. Speak up for yourself. If you can, get actively involved. Get to know your disease and educate yourself. Bring reason as to why it is you have this disease.
Michelle C.
I got involved in a lot of groups pretty early on. Even while I was still in treatment, I had people reaching out to me, “Hey, do you want to help out?” I said, “I’m still in treatment.” They said, “Yeah, but you’re so positive, you always know how to respond, and you ask very thought-provoking questions.”
I started helping out right away. I jumped in the water. Anything that I can do, especially with the younger population. We know what the research says. For whatever reason, it’s on the rise in the younger population. It’s on the decline in the older population because they’re getting screened more.
The younger patients are all told, “You’re too young.” You have to push your doctors.
I wish I would have known at a younger age to push more on some of those early symptoms. I can’t go back. I don’t know what would have happened. But they told me for it to be advanced as it was, I had to have had it for 10 years.
I eat well, go to the gym every day, didn’t eat a lot of red meat, and didn’t eat a lot of processed foods. All these things that people tell you cause cancer, I didn’t do those.
You have to know what you’re going through. Know the disease. Educate yourself. Yes, doctors are wonderful, but you are one patient out of many, many patients. They are there for you, to support you, but they’re there to support and guide all of their patients. They cannot look up every little thing that’s wrong with you because they don’t have the time.


Unfortunately, it’s growing. You think of colorectal cancer and you think the waiting room is going to be full of older men and it’s not anymore. It’s different races, it’s men, it’s women, it’s young, it’s old, it’s kids. It’s everyone now.
>>> More: Why is Colorectal Cancer Increasing in Young Adults?
They’re doing all the research they can, but nobody can pinpoint and say, “Don’t do this with your kids. Stay away from this.” I wish there was something that we had out there to tell people for the younger population out there.
For my younger friends, I tell them to ask their PCPs to screen them. I said, “Even if it’s a Cologuard test, it still will give you peace of mind.” Teachers at my school even said to me, “You’re one of the healthiest people we know. If you can get cancer, oh my gosh.” A bunch of them picked up cancer insurance because of my story.
Know what you’re talking about. Research and ask questions. When something’s not right, speak up. I didn’t speak up about some things; later down the road, I had some issues with them.
Be your own best advocate. Speak up for yourself. If you can, get actively involved. Get to know your disease and educate yourself. Bring reason as to why it is you have this disease.
I feel like I had to come up with a reason. My reason was to share my story and to help others. In helping others, that helps me give me a sense of peace as to why this has happened in my life. If I can help anybody in their journey, no matter what part of their journey it is, even if it’s just them getting a colonoscopy because of my story.
People don’t like to talk about colorectal cancer. It’s taboo. But no, we need to talk about poop. We need to talk about the symptoms.
Don’t be afraid to share your story. Don’t be afraid to tell people. Encourage people to get screened, especially if they have any symptoms or it’s in their family. Get screened.

Inspired by Michelle's story?
Share your story, too!
More Colorectal Cancer Patient Stories
Monica D., Colorectal Cancer, Stage 1
Symptoms: None; caught at a routine colonoscopy
Treatment: Surgery (low anterior resection with temporary diverting ileostomy)
Edie H., Colorectal Cancer, Stage 3B
Symptom: Chronic constipation
Treatments: Chemotherapy, radiation, surgeries (lower anterior resection & temporary ileostomy)
Shayla L., Colorectal Cancer, Stage 4
Symptoms: Stomach sensitivity, food intolerances, exhaustion, blood in stool
Treatments: Chemotherapy, surgery (hepatectomy)
Tracy R., Colorectal Cancer, Stage 2B
Symptoms: Bloating and inflammation, heaviness in the rectum, intermittent rectal bleeding, fatigue
Treatments: Chemotherapy, radiation, surgery
Paula C., Colorectal Cancer, Stage 3
Symptoms: Painful gas, irregular bowel movements, blood in stool, anemia, severe pain, weight loss, fainting spells
Treatment: Surgery (tumor resection)
Nick S., Colorectal Cancer, Stage 4A
Symptoms: Change in bowel habits, size & consistency, blood in stool, abdominal pain, fatigue
Treatments: Surgery (sigmoid colectomy), chemotherapy (capecitabine, oxaliplatin), immunotherapy (bevacizumab, pembrolizumab)





One reply on “Michelle’s Relapsed Stage 4 Colorectal Cancer Story”
I was diagnosed 14 months ago-Stage 4 rectal cancer. Your story was just what I needed to read today. Thank you for sharing!