Life Changed Overnight: Rylie’s Experience with Stage 4 Colorectal Cancer
Rylie is someone whose life has always revolved around her family, home projects, and being outdoors. She enjoys gardening with her mom, cycling with her fiancé, and caring for her chickens and dogs. In April 2025, the joys of that routine were interrupted when persistent abdominal pain and bloating kept sending her back to the ER, where she was told it was constipation. Trusting her intuition and refusing to ignore what her body was telling her, she pushed for answers. That persistence led to the discovery of a mass and a diagnosis of stage 4 colorectal cancer.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez & Jeff Forslund
Rylie had to have emergency surgery. Her surgical treatment was extensive, involving the removal of a tumor in her colon, a liver mass, and parts of her small intestine. She also received an ostomy, which she had reversed.

Her cancer treatment involved chemotherapy, immunotherapy, and targeted therapy, but not before Rylie underwent fertility preservation, a major decision made quickly after surgery. Her care team involved multiple institutions, and she and her family sought out the best specialists for her treatment.
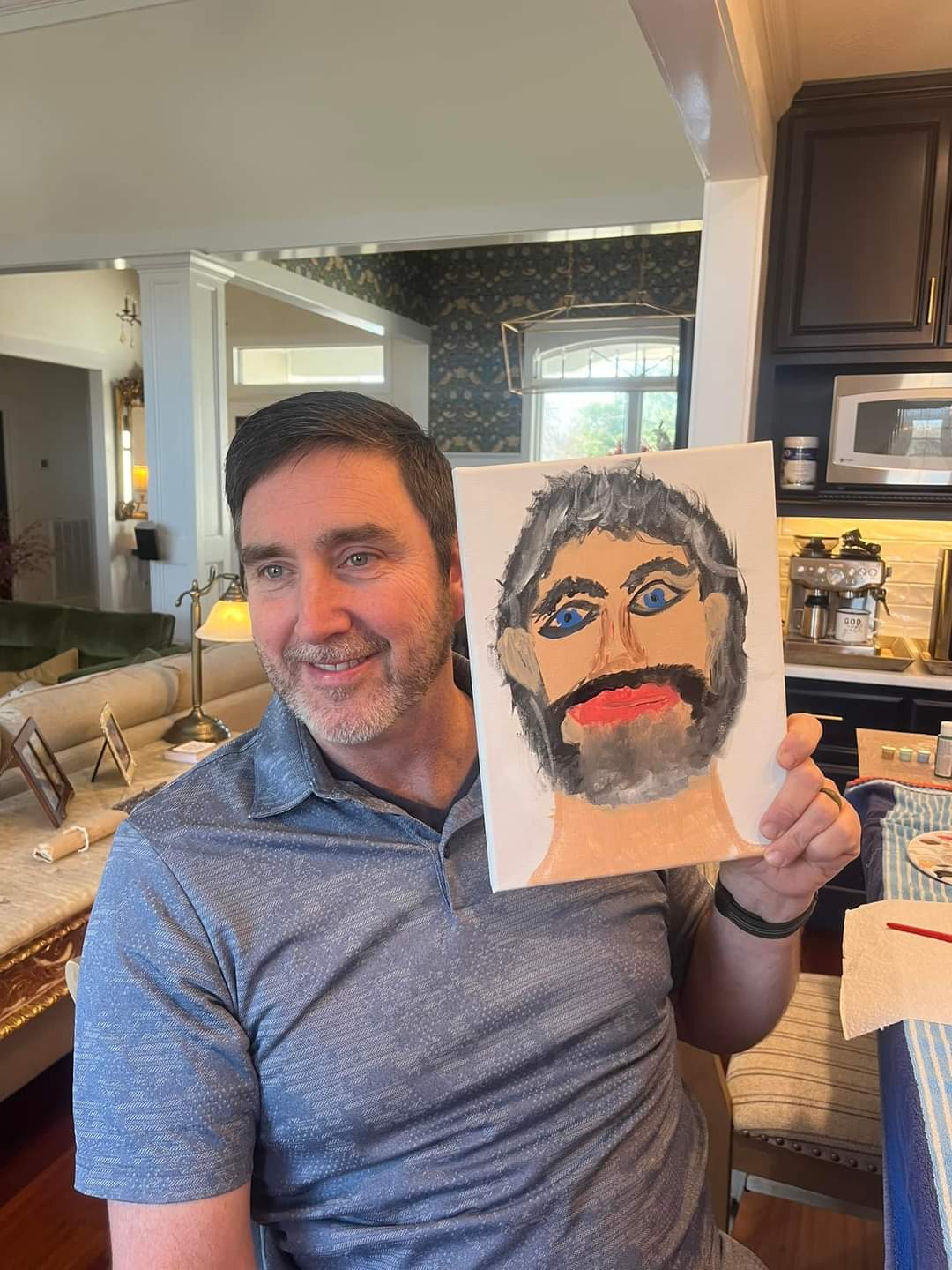
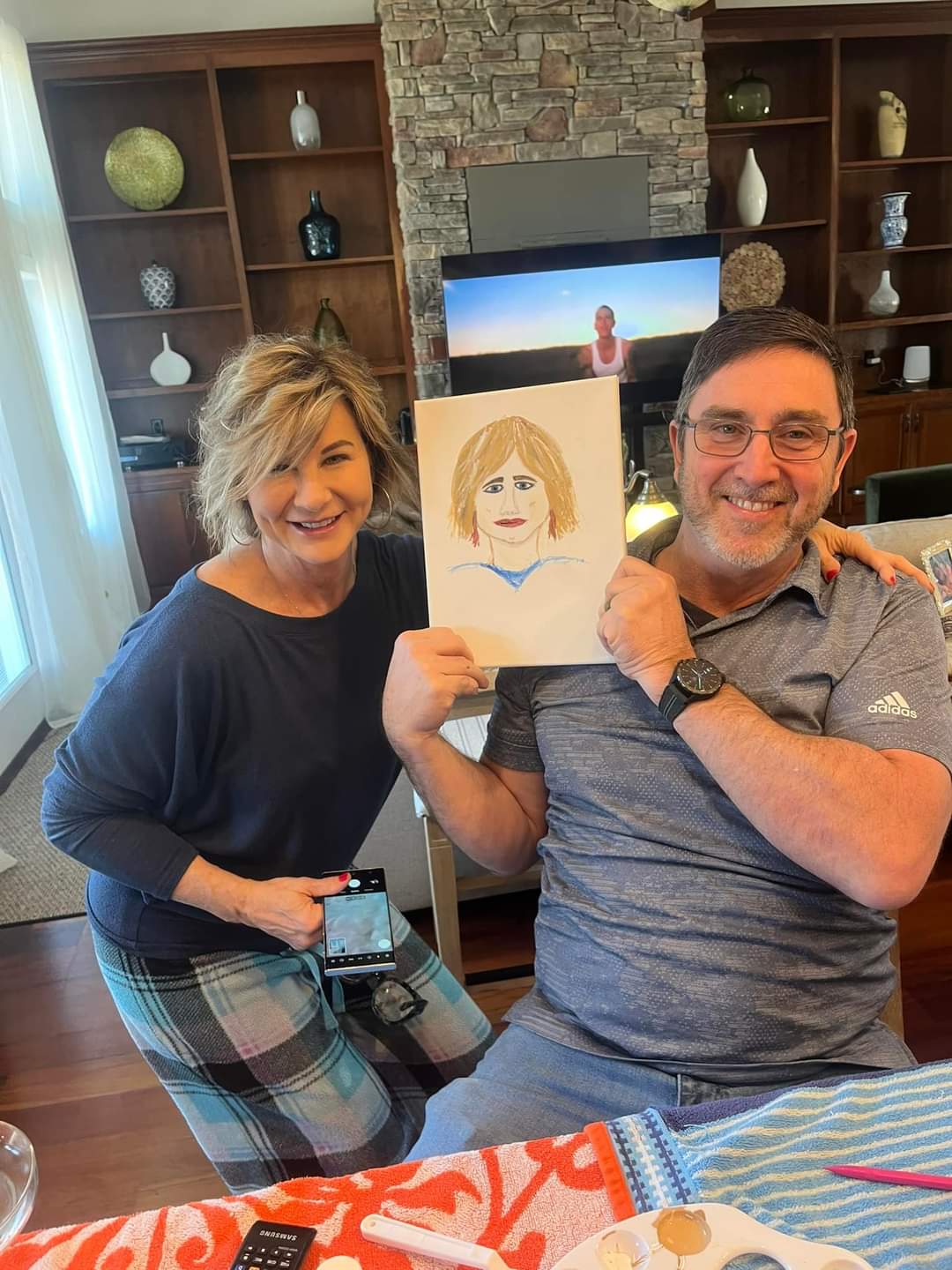
Throughout her experience, Rylie relied deeply on her faith and the support of her family, especially her mother, who she describes as her role model. She openly shares the emotional challenges of postponing her wedding plans and adjusting to physical changes, but remains grateful for the unwavering support of her fiancé and family.
Rylie encourages patients to advocate for themselves and stresses how important it is to connect with others facing similar diagnoses. Her experience exemplifies the importance of self-advocacy and persistence when navigating symptoms that don’t fit typical expectations.
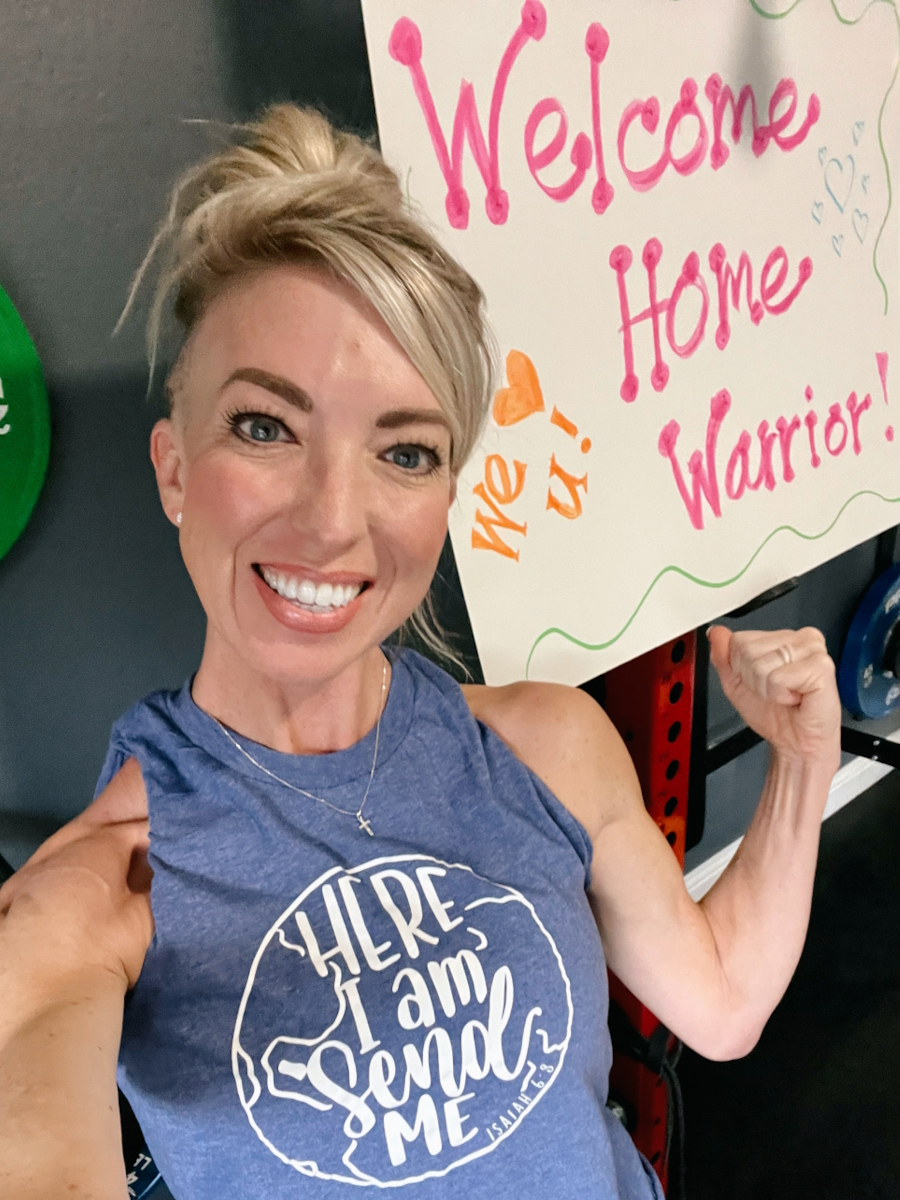
Rylie’s story is a testament to transformation, from shock and fear after diagnosis to hope and empowerment with treatment and community support. Her experience offers vital lessons for young adults and others about listening to their bodies, seeking quality care, and approaching cancer treatment with resilience and faith.
Watch Rylie’s video above and read through her edited transcript below to learn more about how:
- Early symptoms may be misunderstood or misdiagnosed; trusting your own body and seeking persistent evaluation is crucial
- Cancer treatment affects every part of life, including the physical, emotional, and relational parts, and requires strong support systems
- Fertility preservation is an important consideration, even amid urgent cancer treatment
- Seeking second opinions and specialized care can significantly improve treatment experience and outcomes
- You know your body best. Advocate for yourself, no matter what
- Name: Rylie T.
- Diagnosis:
- Colorectal Cancer
- Staging:
- Stage 4
- Age at Diagnosis:
- 27
- Symptoms:
- Sharp lower abdominal pain
- Severe bloating
- Fecal impaction
- Treatments:
- Surgeries: colon, liver, and small intestine tumor resection; ostomy surgery; ostomy reversal surgery
- Chemotherapy
- Immunotherapy
- Targeted therapy: monoclonal antibody
- Fertility conservation treatments
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Rylie
- How we navigate cancer as young adults and a couple
- My first symptoms: when things felt off
- Advocating for myself and the challenge of getting diagnosed
- My reaction to my stage 4 colon cancer diagnosis
- I had emergency surgery
- Living with an ostomy
- Finding the right care team
- What my treatment has looked like
- My treatments, including fertility treatment, and their side effects
- Scans, communication, and no evidence of disease
- Hope and faith through cancer
- Support from the colorectal cancer community
- What I want others to know
My name is Rylie
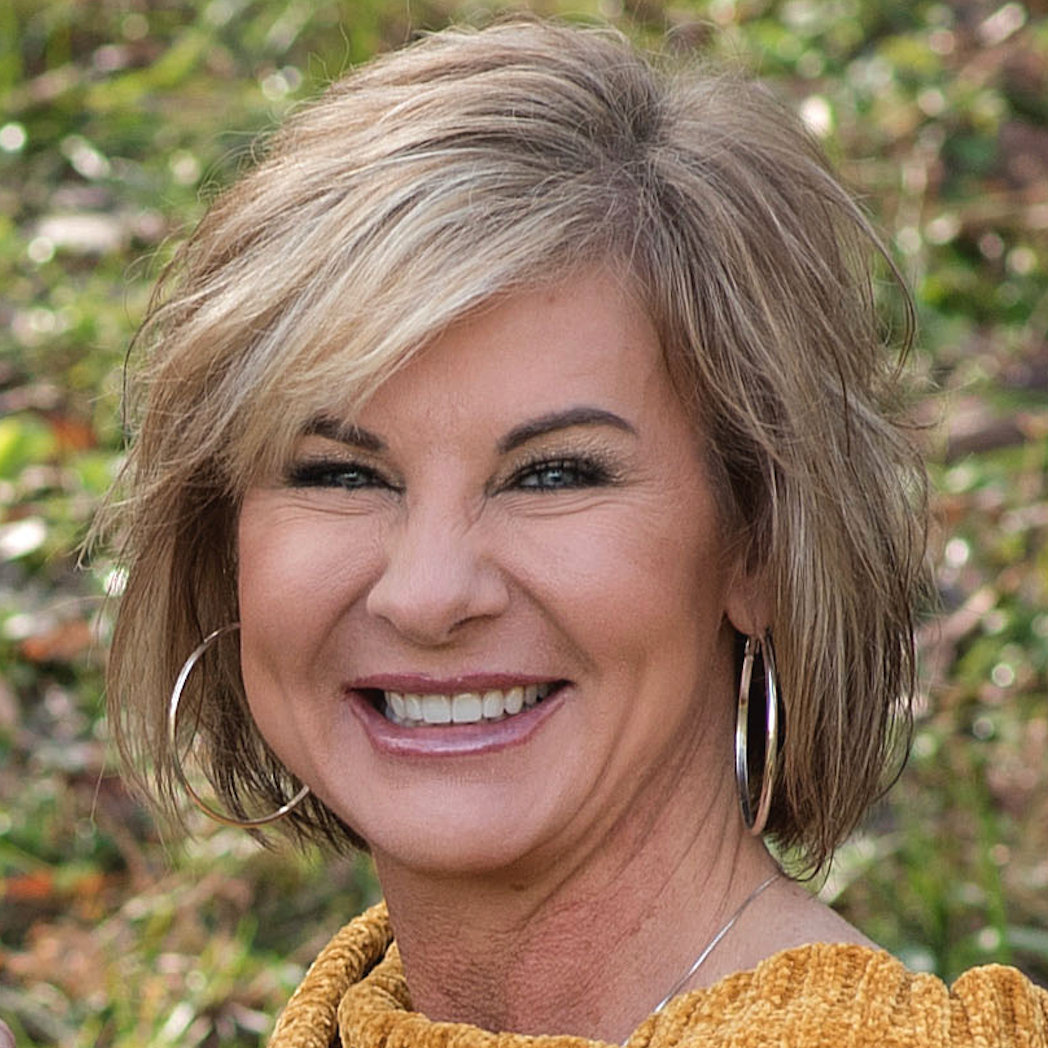
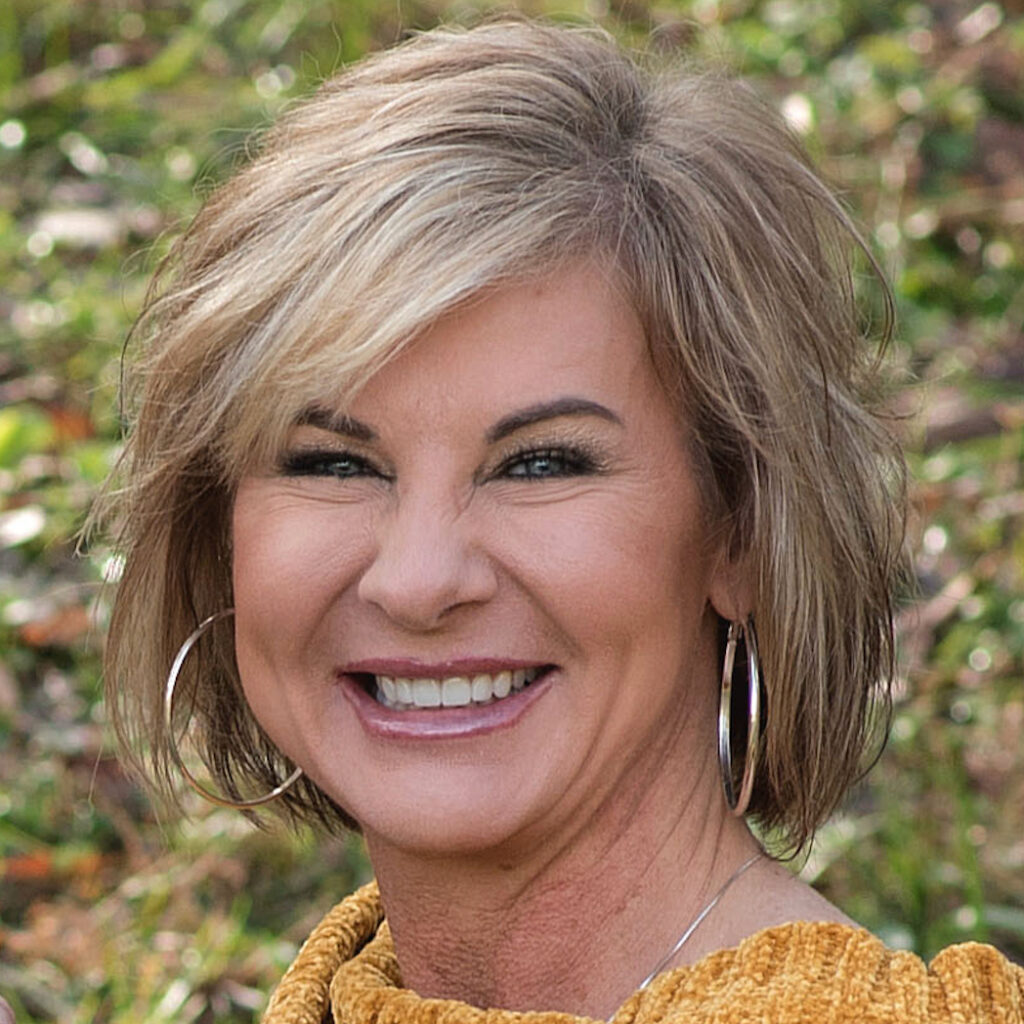
My name is Rylie. I was diagnosed with stage 4 colon cancer in April 2025.
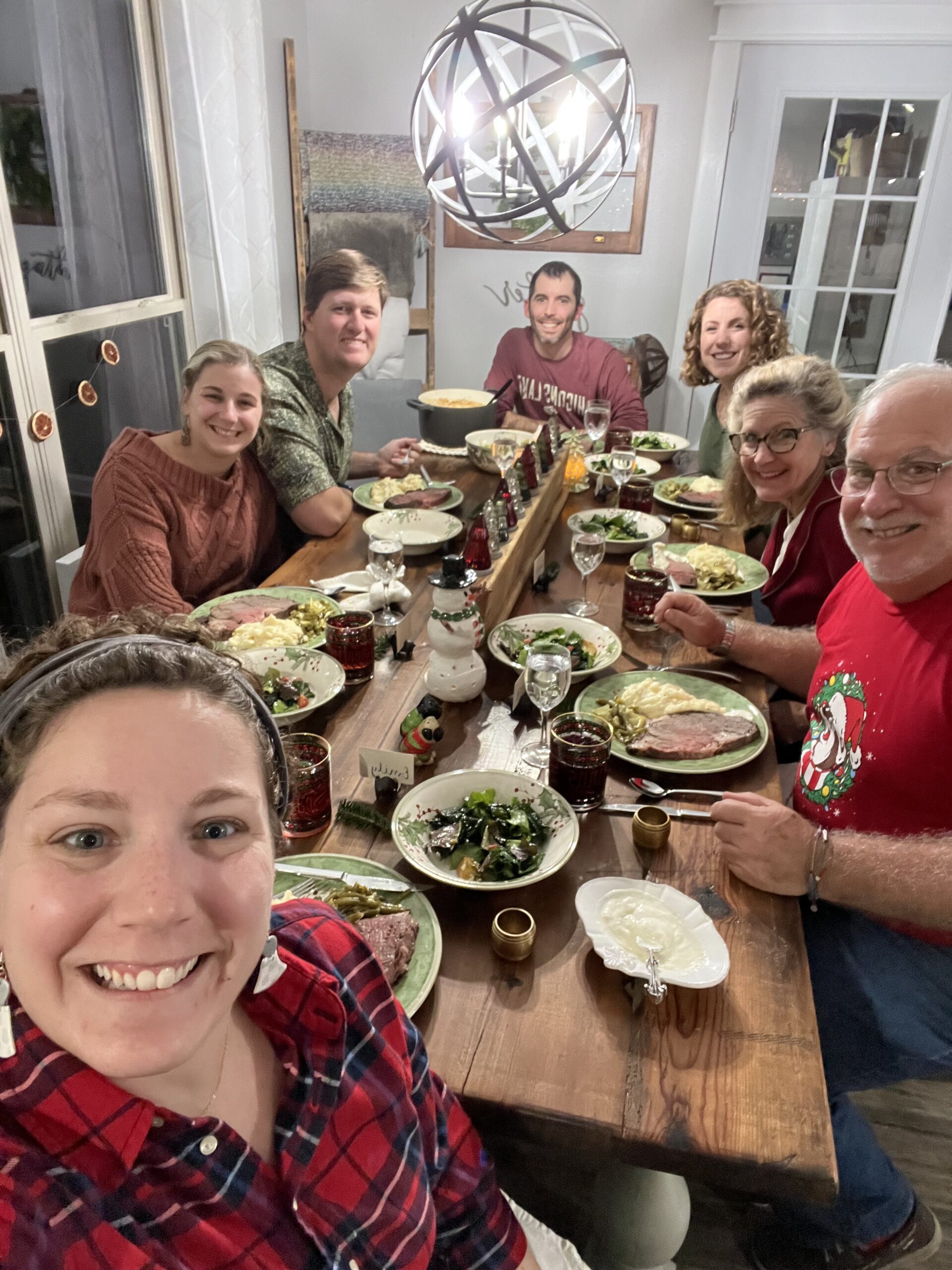
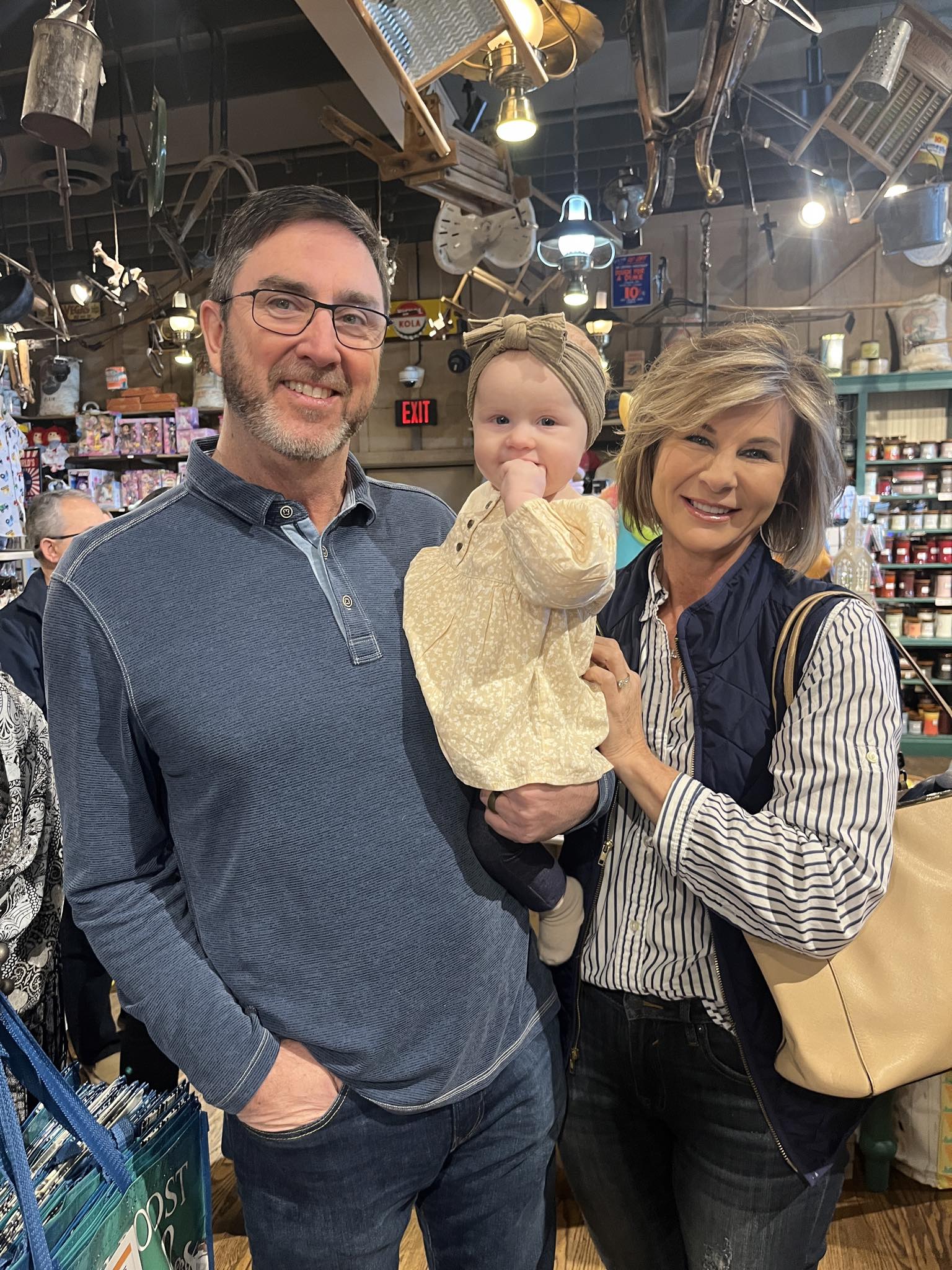
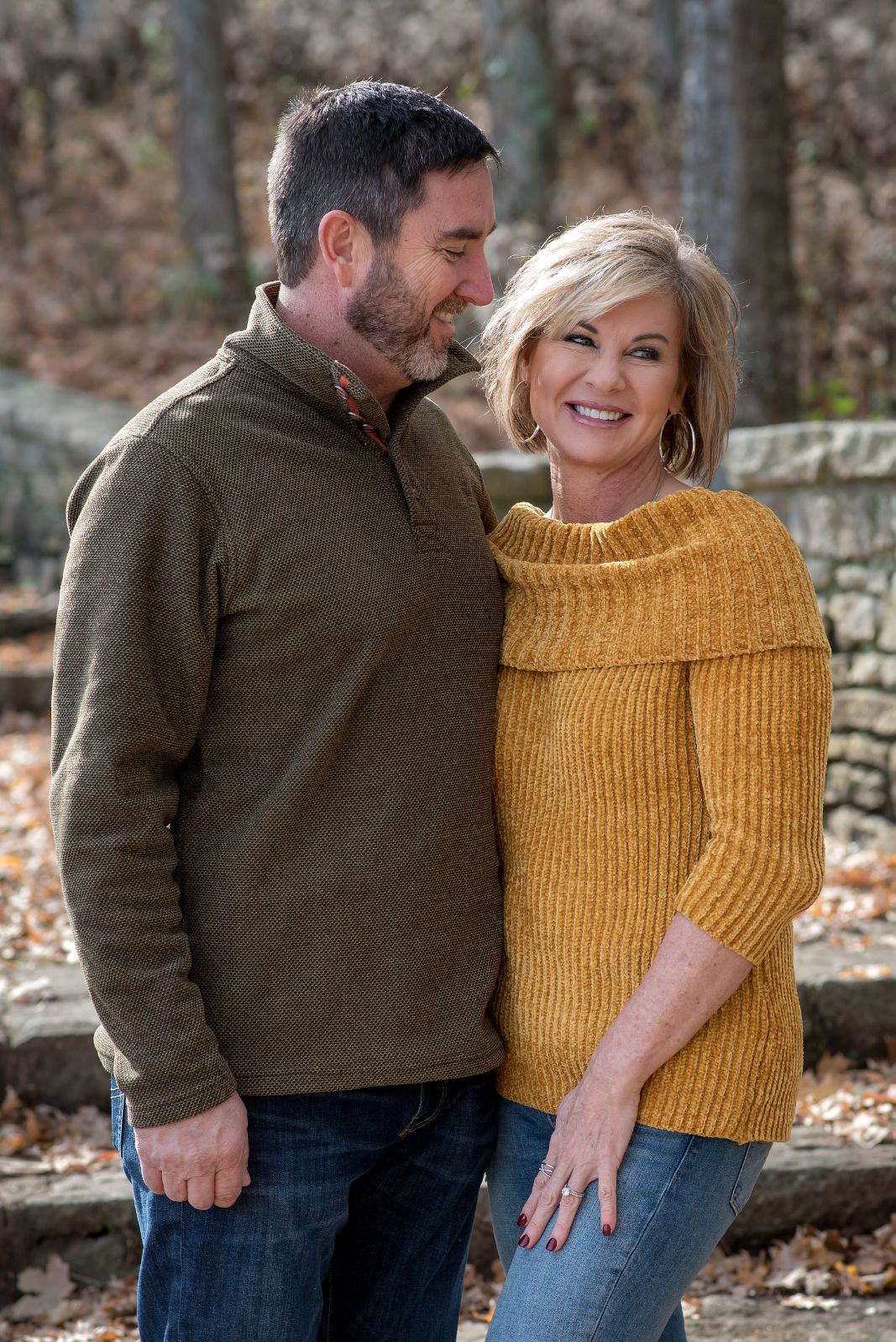
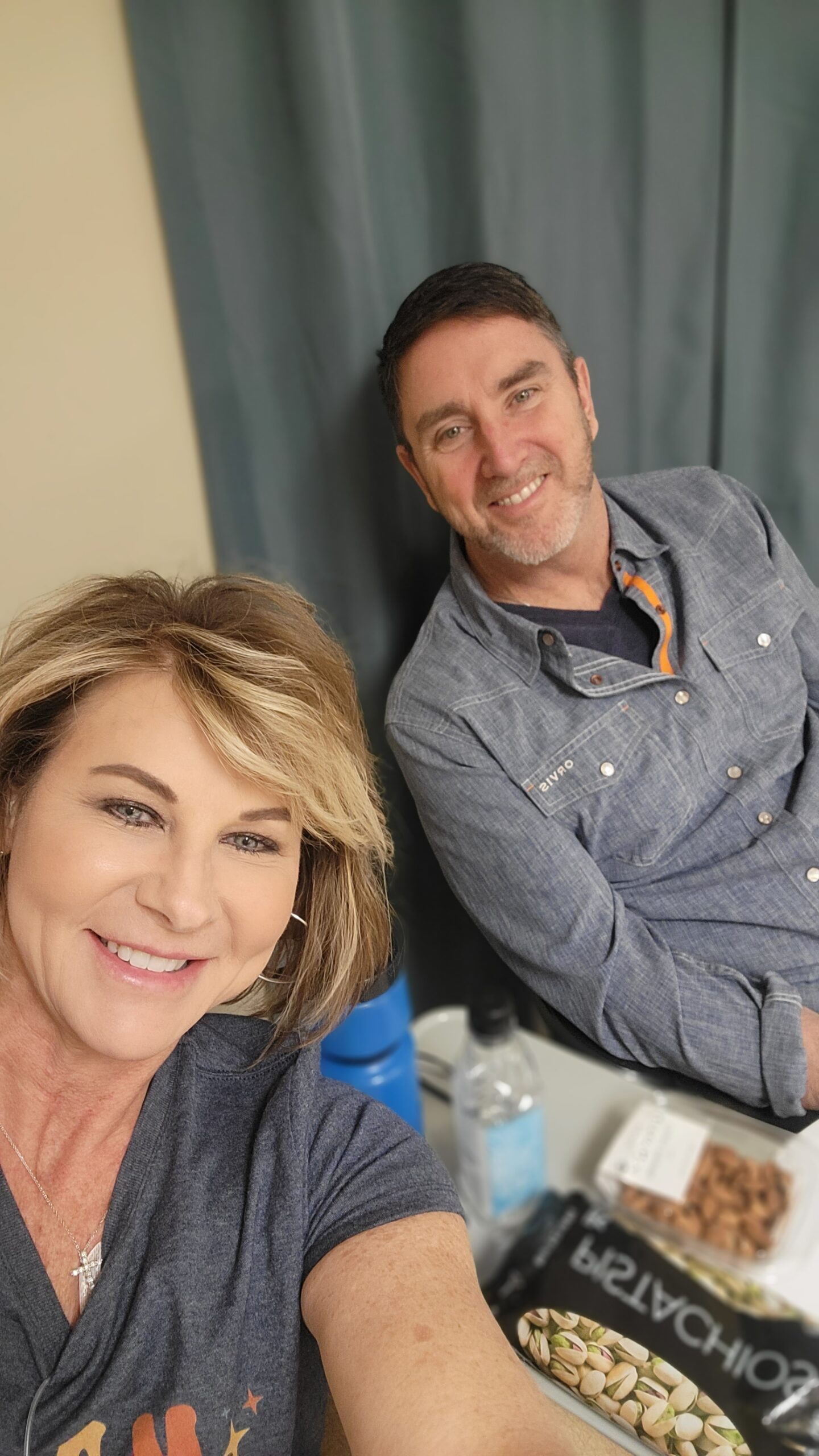
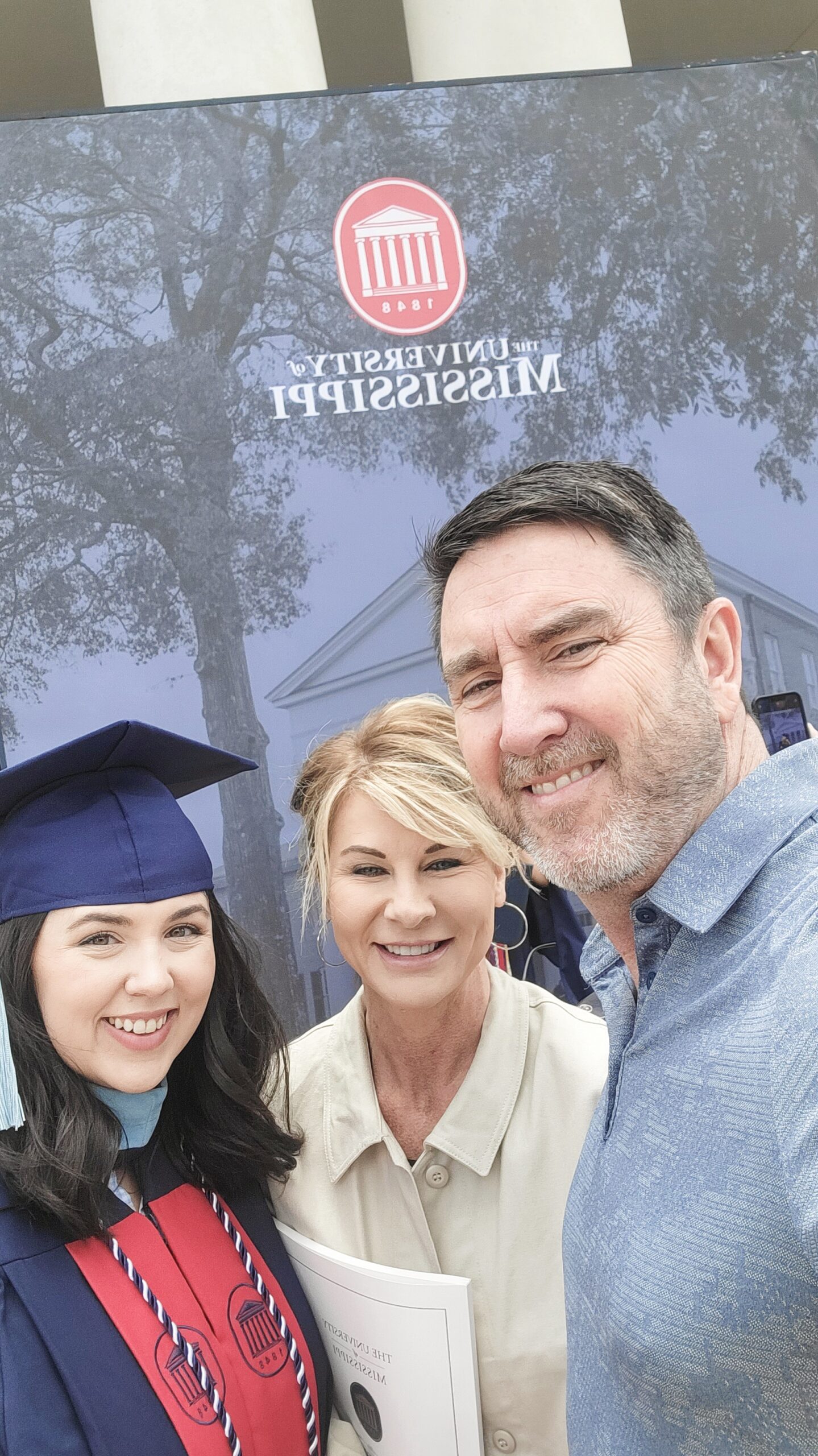
Family is my main priority. I love being with my family and spending time with them.
I got engaged two years ago. We were supposed to have our wedding in June, but that was derailed. We’re now planning for this next June.
My fiancé is my best friend. We love doing house projects together. We have chickens and two dogs. I enjoy working in the garden. I also like road cycling and am just an outdoorsy person, so I love being outside.
I wouldn’t have been able to get through this without my mom or my dad. They’re my number one supporters and have been with me every step of the way. My mom is my role model. She loves the outdoors and flowers. I try to mimic what she does, but I’m the little version of her.
How we navigate cancer as young adults and a couple
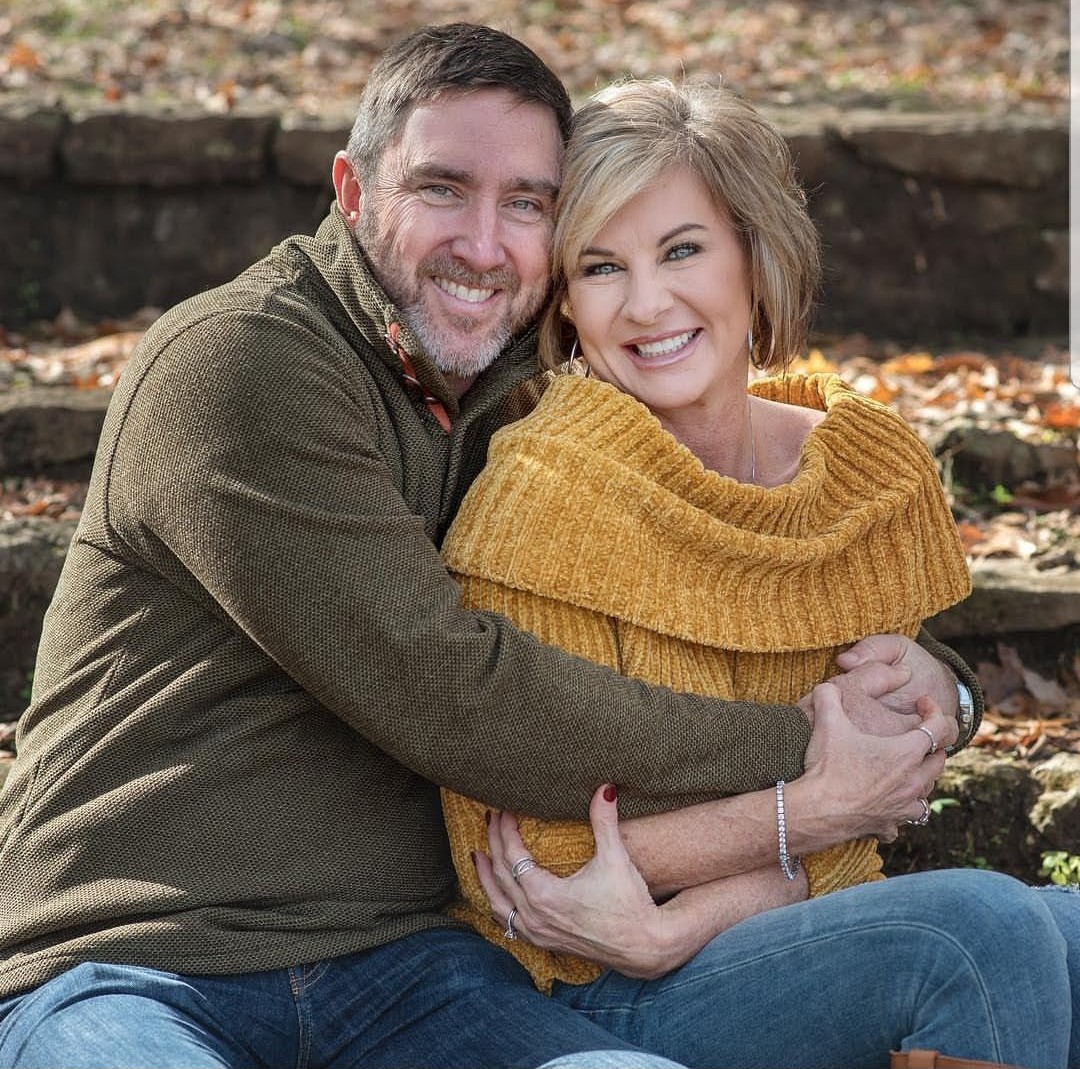
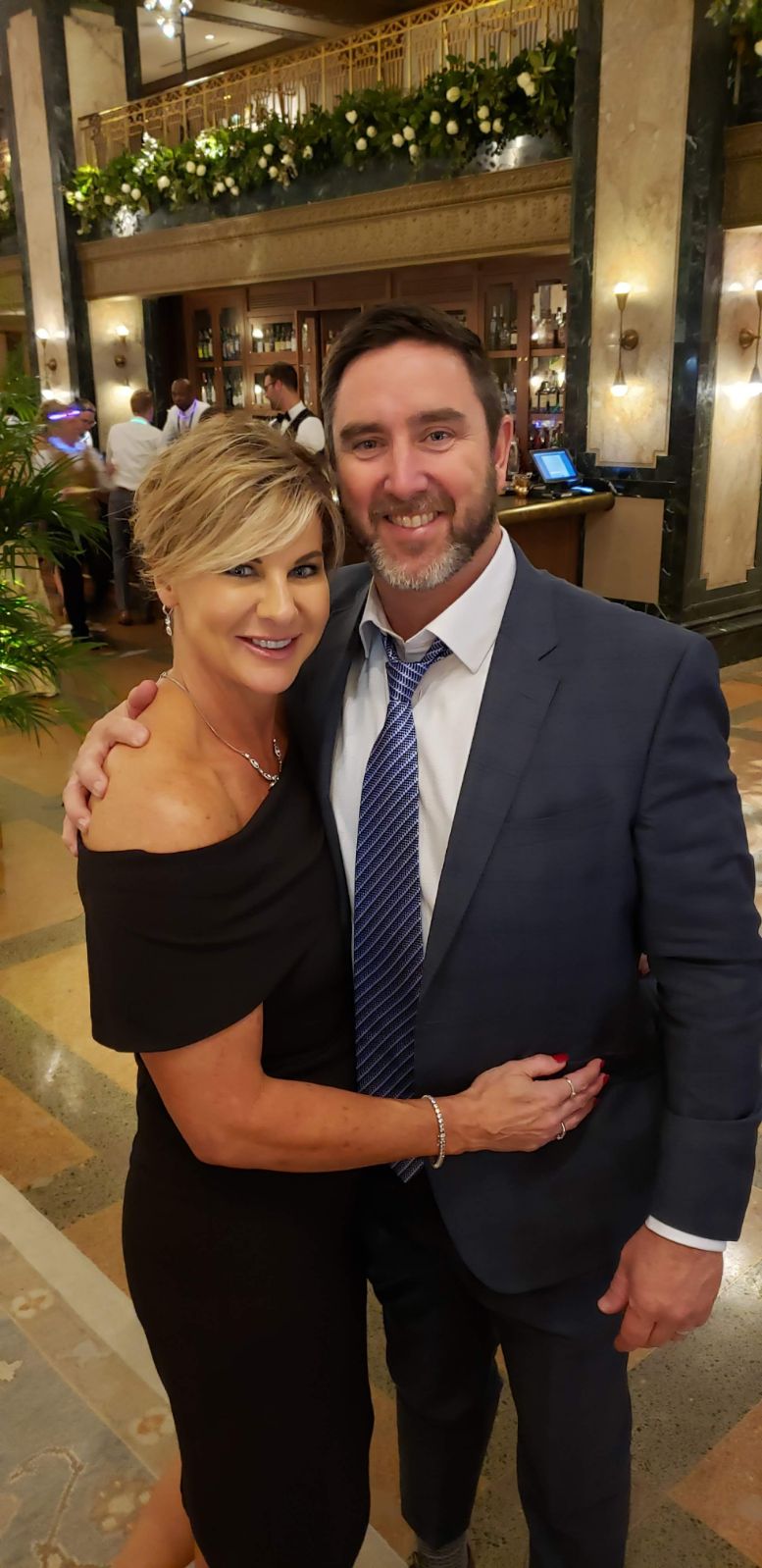
It’s been tough. It was a life-changing experience for both of us.
We used to be active every single day, but with me in the hospital for ten days at a time, my fiancé has had to support me and put house projects on hold. Pushing the wedding back was sad because we put so much work into planning, and we thought 2025 would be the happiest year of our lives, but it ended up being the worst.
Still, it’s awesome that he stuck by my side through it all. Our lives have completely changed, but we are committed to each other, and that will never change. My body completely changed, and he still loves me for who I am, and I’m so grateful for that.
After our wedding, I thought we’d have a child right away. Being a mom is all I want in life. We’ll eventually get there. Luckily, I had fertility treatments and got my eggs frozen.
My first symptoms: when things felt off
It all started in October 2024. I went to the emergency room with severe lower left abdominal pain and bloating; something just didn’t feel right. The ER staff said I was backed up and sent me home. I accepted that explanation for a while. Six months later, the pain got worse. Over three to four ER visits, I was eventually admitted.
Before the final ER visit, I saw my family doctor because I had a fever for a week and felt unwell at work. She did a check-up, but said I was just backed up. That weekend, I went to the ER three times. Two of those times, I was sent home with pills, but the third time, they kept me, saying I might have a small perforation in my bowel. I stayed for seven days and couldn’t eat or drink. When my belly went down a little, they hoped the perforation would heal on its own and sent me home.
That Sunday night, I told my fiancé something was very wrong, and he rushed me to the ER. That CT scan was totally different and showed a mass in my bowel and a mass on my liver. They rushed me into emergency surgery that night. Everything happened so fast; I had zero time to process anything.
The main symptoms were sharp pain in my lower left abdomen, severe bloating, and being backed up. I struggled to go to the bathroom, and even when I could, it wasn’t much. Those symptoms just continued to worsen.
Advocating for myself and the challenge of getting diagnosed
It was crazy… You know your body best. Doctors can run scans and tell you things, but only you know how you’re actually feeling.
I knew something was wrong. Being sent home with a diagnosis of constipation was embarrassing. I was raised with two brothers; I was built to be tough. Still, it was demoralizing.
I had several CT scans. The doctor said that it’s actually easier to read CT scans for a heavier person because their intestines are more spread out, but I have a smaller frame, so everything is squished together. All the scans showed I was backed up, but they couldn’t see underneath the congestion.
My reaction to my stage 4 colon cancer diagnosis
Originally, when they performed a biopsy on my liver after seeing a mass, it came back as scar tissue. One doctor said, “If there’s a mass on the liver, it’s stage 4 colon cancer.” He called it from the start.
The biopsy showed scar tissue, which was strange. They suspect it was a false negative, or it may have been a different mass. Other than that, no one mentioned “cancer” until a few days later, after more tests.
I was in complete shock. I asked doctors not to share results until my parents were with me. When he said stage 4 colon cancer, the first thing I thought was, “I’m going to die.” Everyone was in shock.
I had emergency surgery
For the emergency surgery, they sliced me from my sternum down to my pelvic area. They took out the tumor on my colon and removed a mass from my liver and parts of my small intestine. They also gave me an ostomy, which was a huge life change. It’s something I’ll never fully get used to.
I still have my ostomy, but am having it reversed on November 18th. I cannot wait to have my body back.
Living with an ostomy
It’s wild to see something on my stomach and learn that it’s my bowel. I’m grateful because it saved my life, but I don’t like it and hate it.
I feel bad saying that because it did save my life. I had a great nurse who taught me how to take care of it. I couldn’t wear the same clothes; I had to wear baggier clothes to hide it. I’m very self-conscious, so it was hard not being proud of it, but I got semi-used to it and am happy I’ll get a reversal soon.
A doctor was honest with me and said some people never get used to an ostomy. For some, it’s okay, but it’s not my lifestyle. I’m thankful for honesty.
Finding the right care team
My surgeon was amazing, and the nurses at UPMC West Shore were great. We met an oncologist there, but we wanted the best care possible, regardless of cost. We contacted several cancer centers, and Memorial Sloan-Kettering resonated most; they’re in the top two in the nation.
Their team was easy to reach and supportive, unlike the original oncologist team, which lacked good bedside manner. Bedside manner is critical, as I want to feel cared for.
Don’t be afraid to reach out to multiple cancer centers and get a second opinion. Memorial Sloan-Kettering was our first choice because of its track record. Doing this research is a lot of work, and my family was an incredible support team. I couldn’t have done it without them.
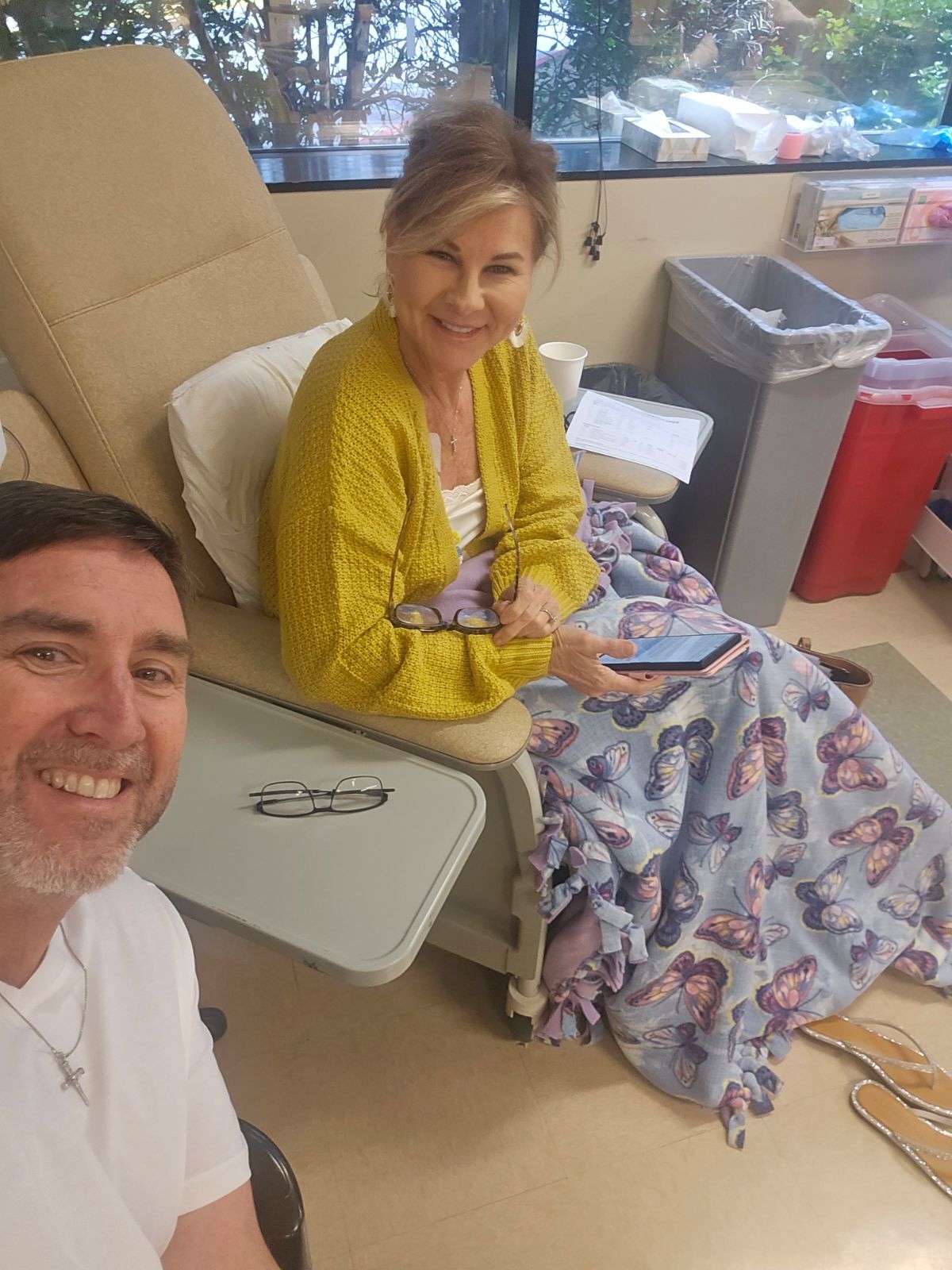
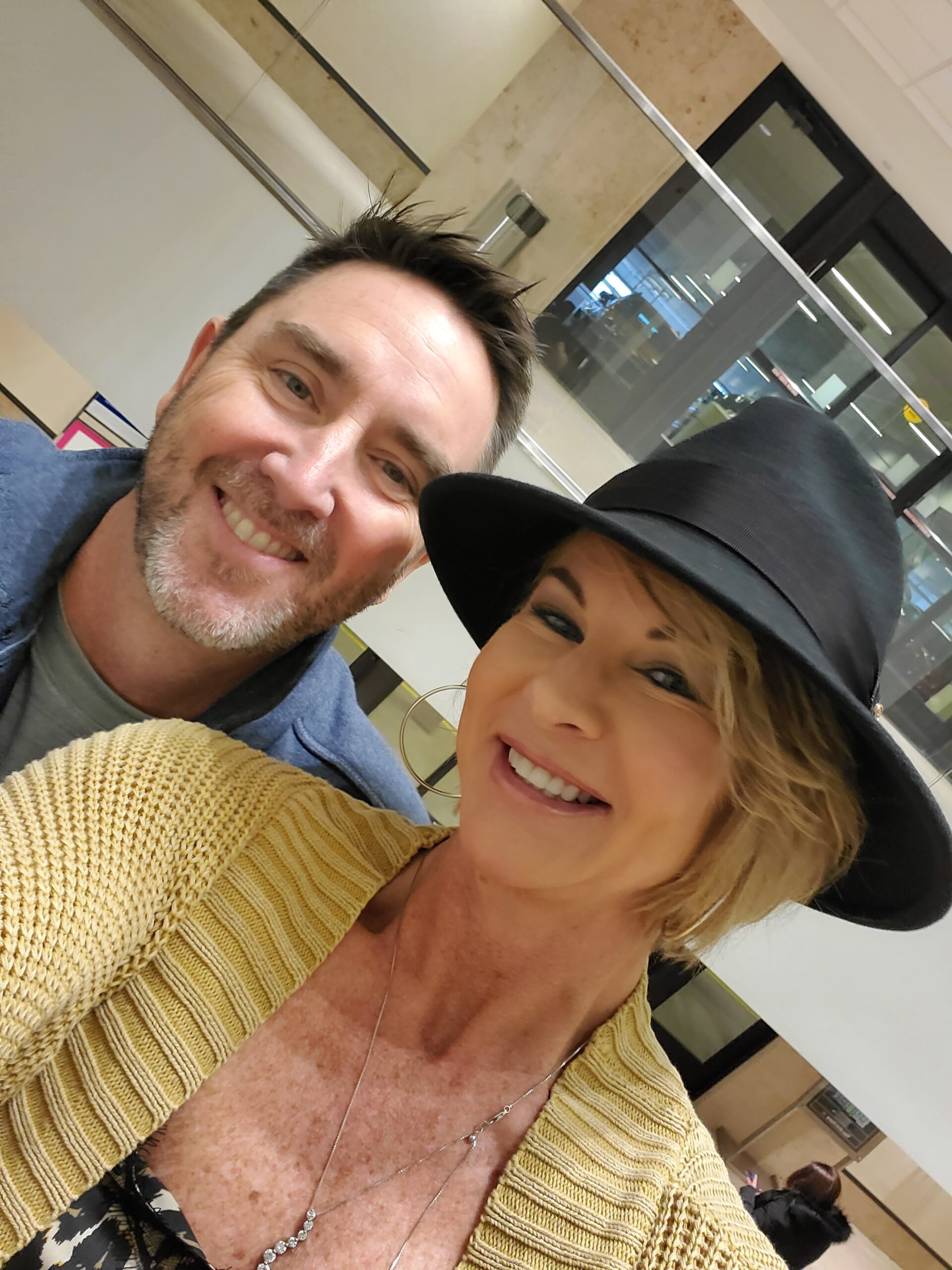
Traveling to Memorial Sloan-Kettering takes 2.5 hours; I’d go every other week for infusions. It’s a whole day affair. It’s worth it, and not too bad.
What my treatment has looked like
My treatment included chemotherapy and targeted therapy with panitumumab. Memorial Sloan-Kettering called it immunotherapy, but technically it was targeted therapy.
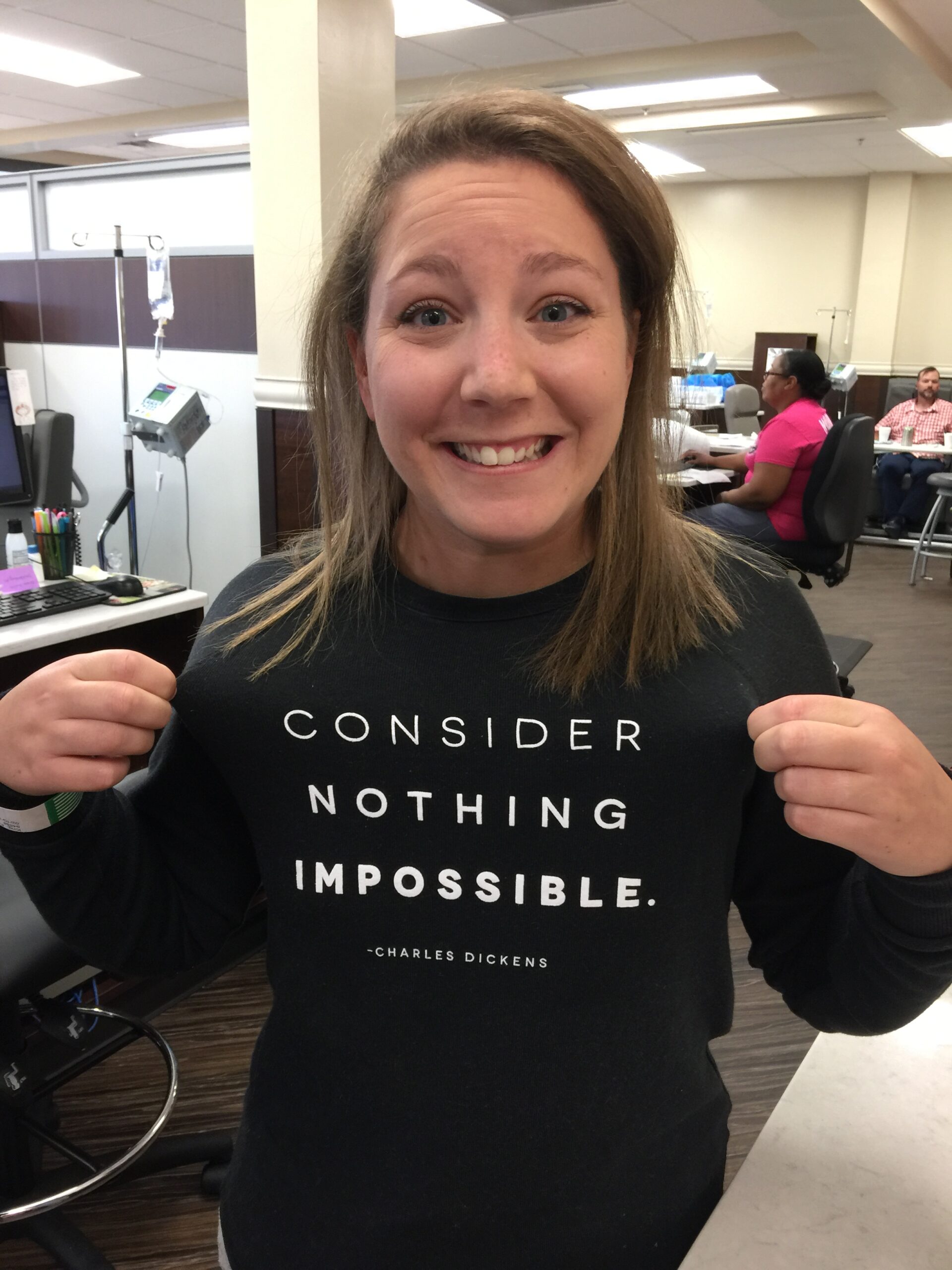
The targeted therapy changed my cells to kill bad cells. I received chemotherapy every other week. I just finished my last pump today.
For each cycle, I’d have an infusion for about 2.5 hours, then go home with a pump for two days.
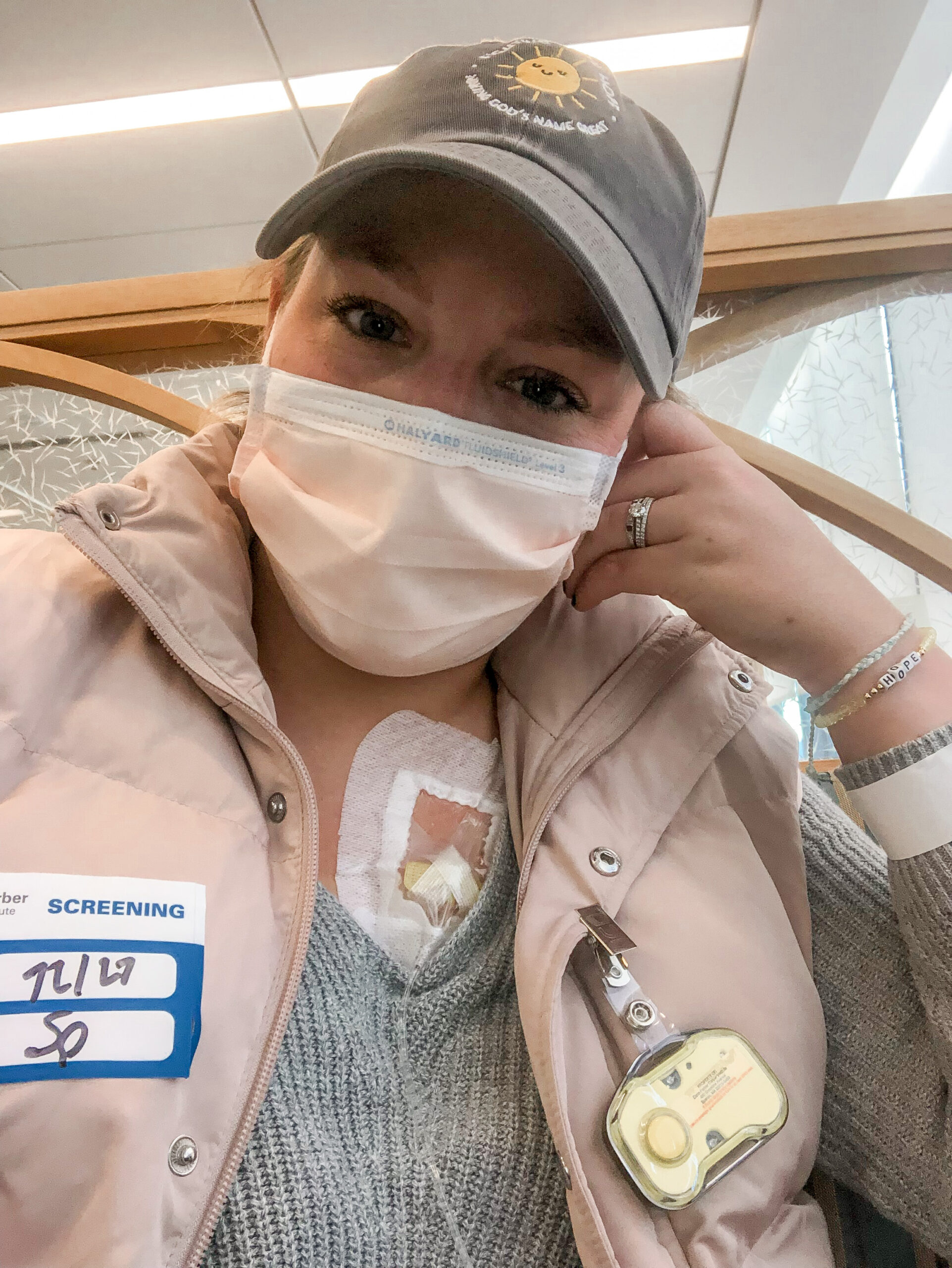
My treatments, including fertility treatment, and their side effects
The beginning was rough because after surgery, I immediately started physically overwhelming fertility treatments, four shots a day and no time to heal.
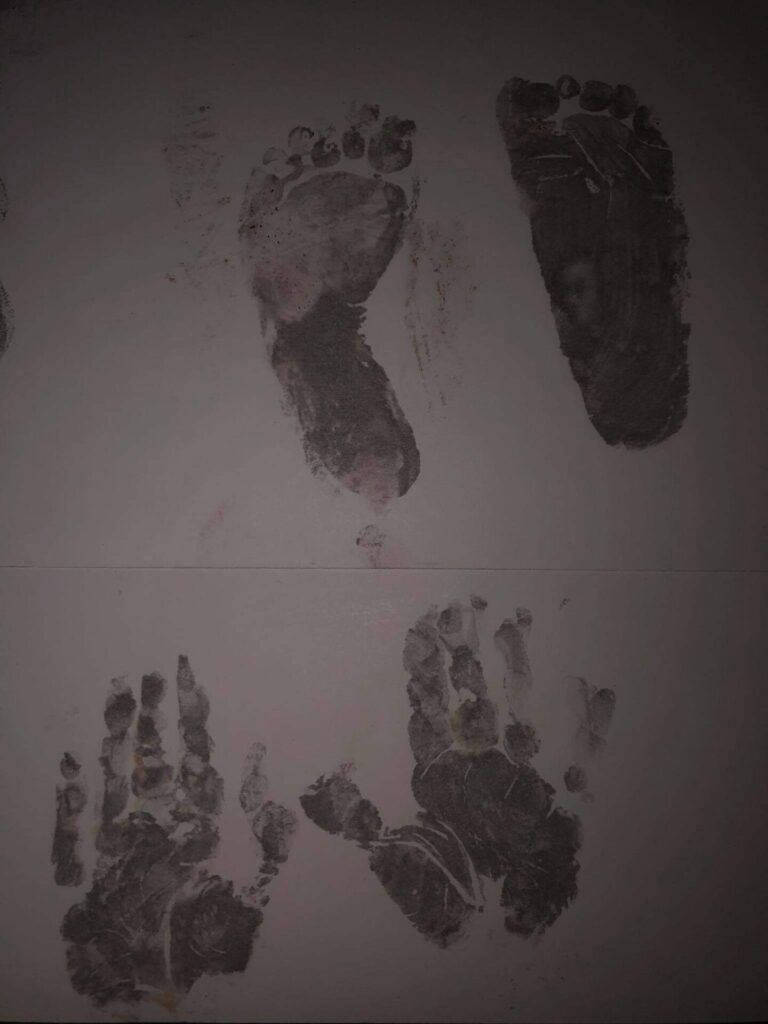
Two days after surgery, the team asked if I wanted to preserve my eggs. I had zero time to process what that meant. After hospitals explained it, I started shots for fertility treatments right after discharge, four shots a day for two weeks. The extraction yielded 40 eggs, with 36 viable. It was rough but worth it.
And then after egg extraction (Monday), I started chemotherapy (Wednesday). My body was still in recovery mode, and the first infusion landed me in the hospital because it caused severe pain. My ovaries were enlarged, causing pressure on my urinary tract, and a mass was pulled out, which was benign.
The first two treatments were rough due to back-up and pain, but after that, the treatment went well. I had some tiredness and a facial rash, but it was manageable overall.
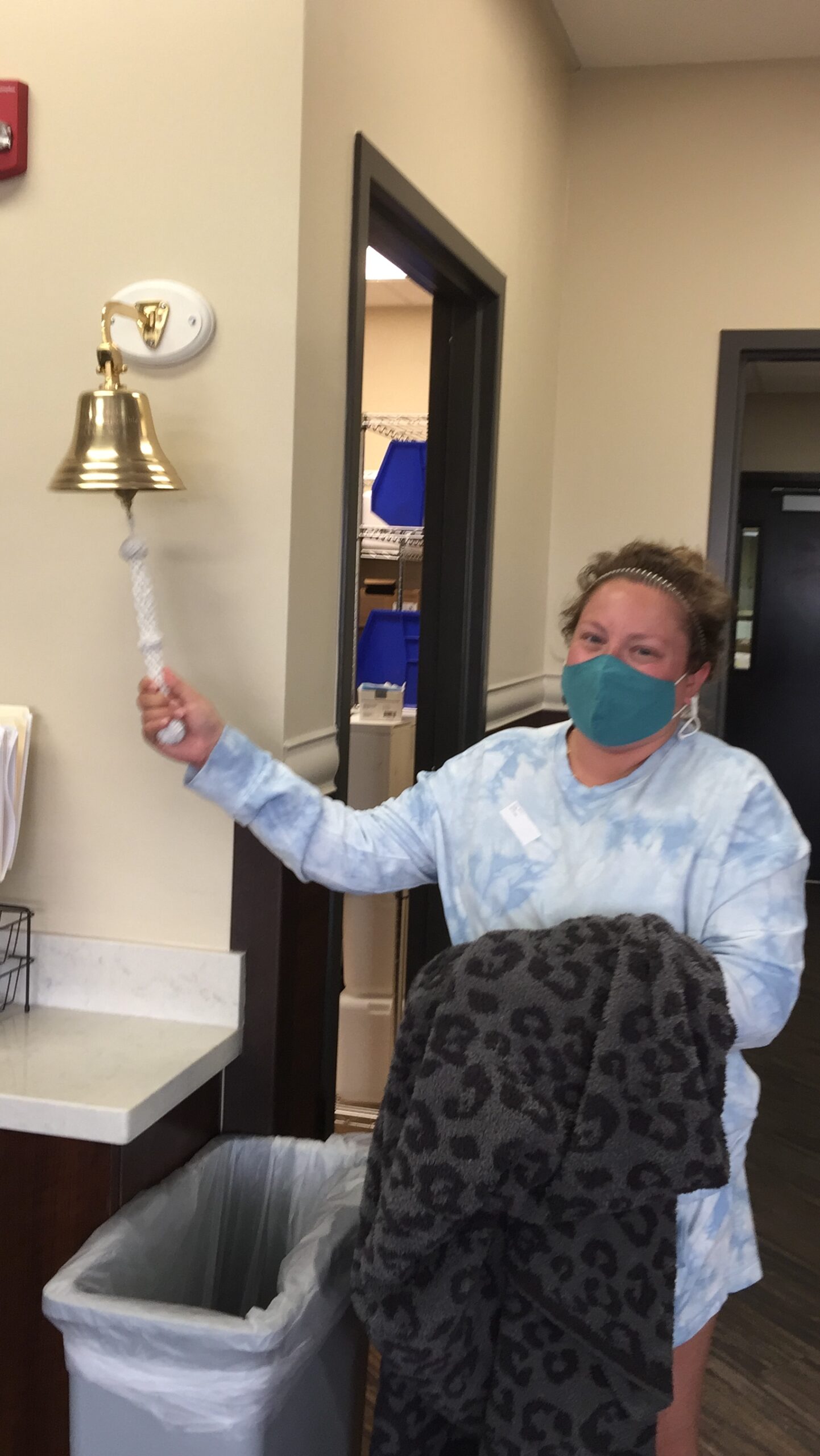
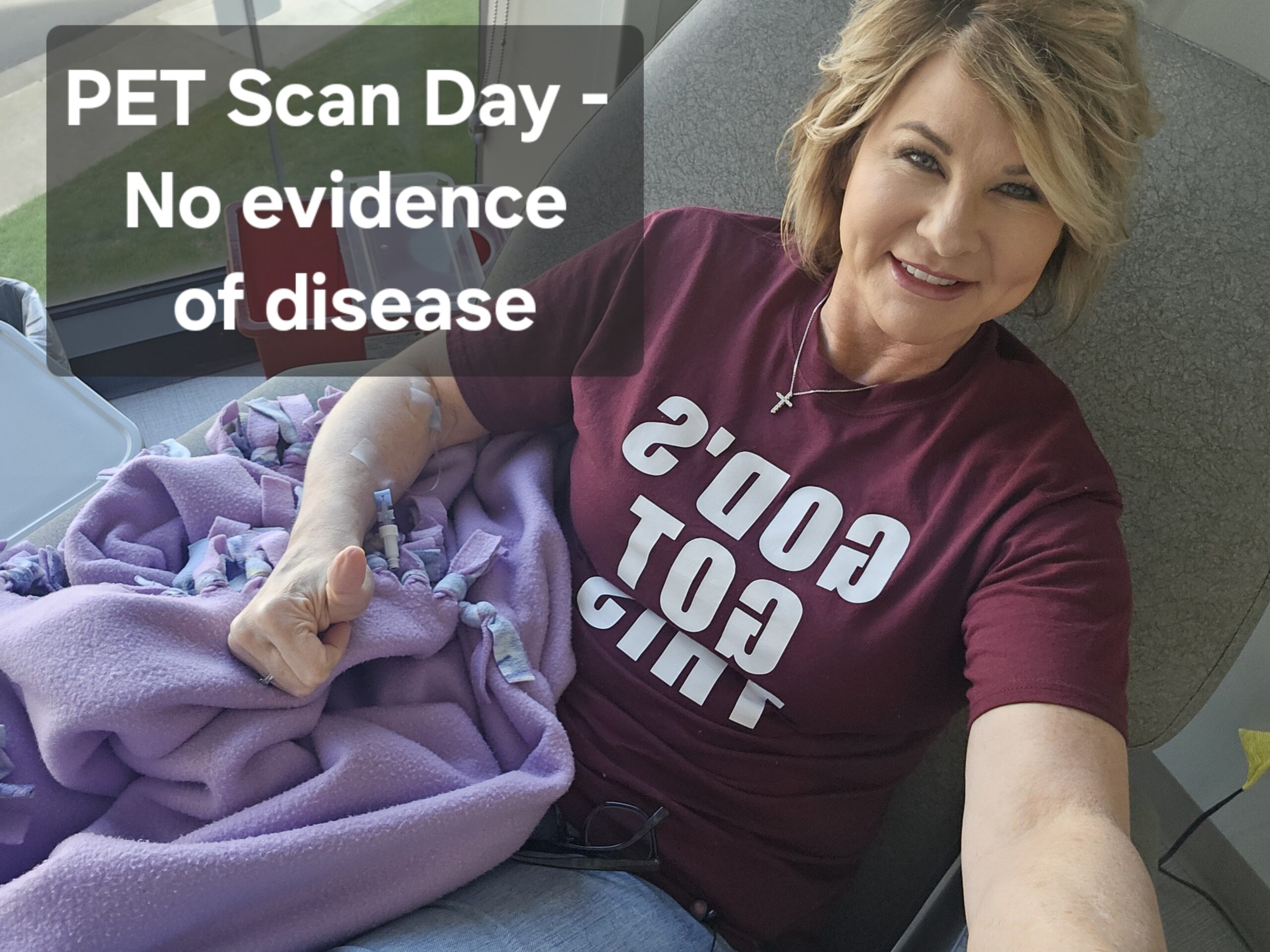
Scans, communication, and no evidence of disease
Two weeks ago, we were in a different emotional space due to miscommunication between surgery and cancer treatment. I had a scan, and the oncologist said the masses on my ovaries were shrinking. That was news to us.
After investigating, we learned these were cysts from fertility treatments, not cancer.
After an MRI and a CT scan, the team scheduled liver resection and ostomy reversal, and afterward, I’ll be in remission.
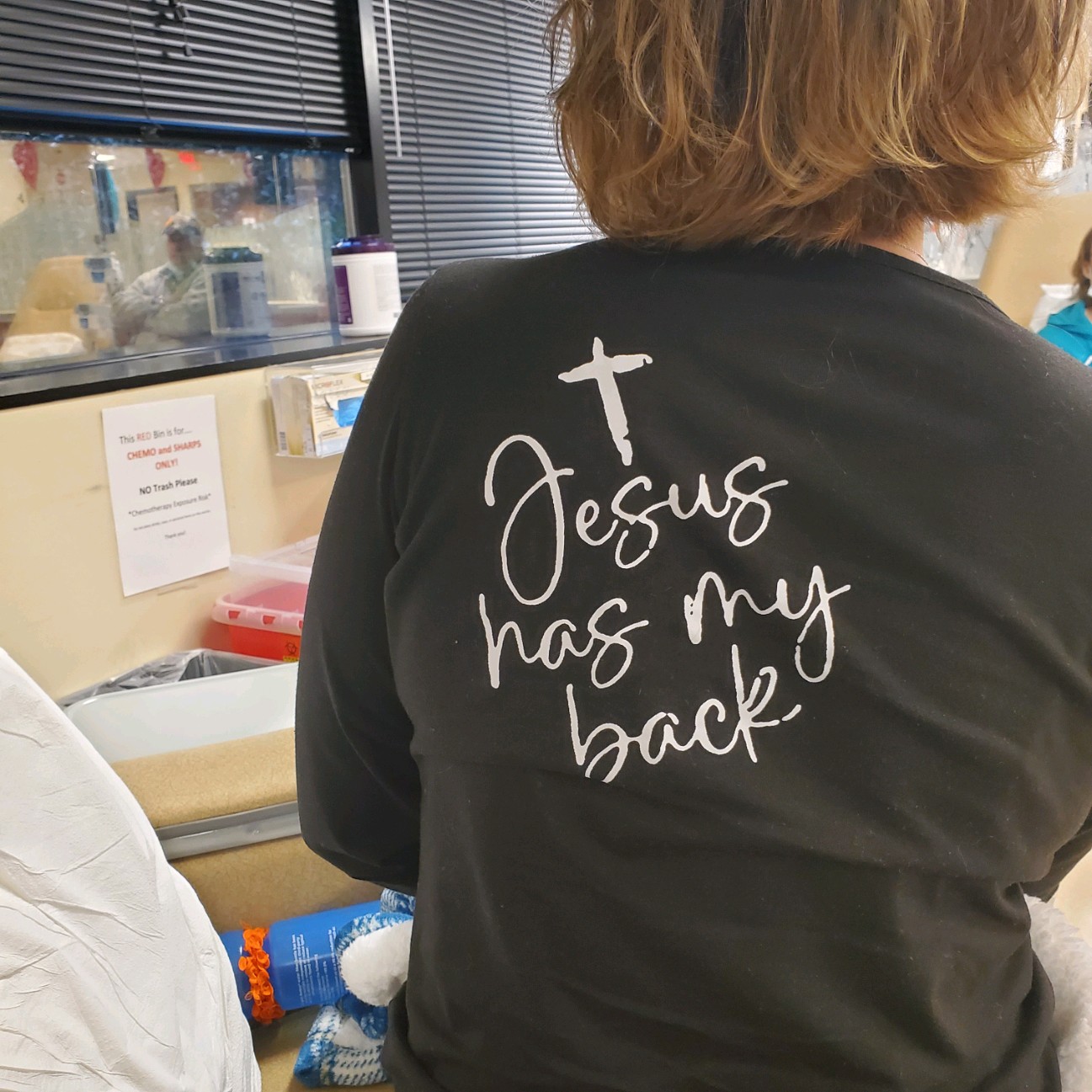
Hope and faith through cancer
I leaned heavily into my faith this year. God is the one who got me through this. He tested my strength but rewarded me in the end.
Without faith and my parents, I couldn’t have made it.
I try not to use the word “hope.” I want to be positive and manifest certainty that this isn’t coming back.
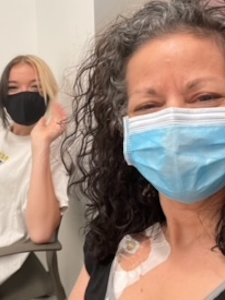
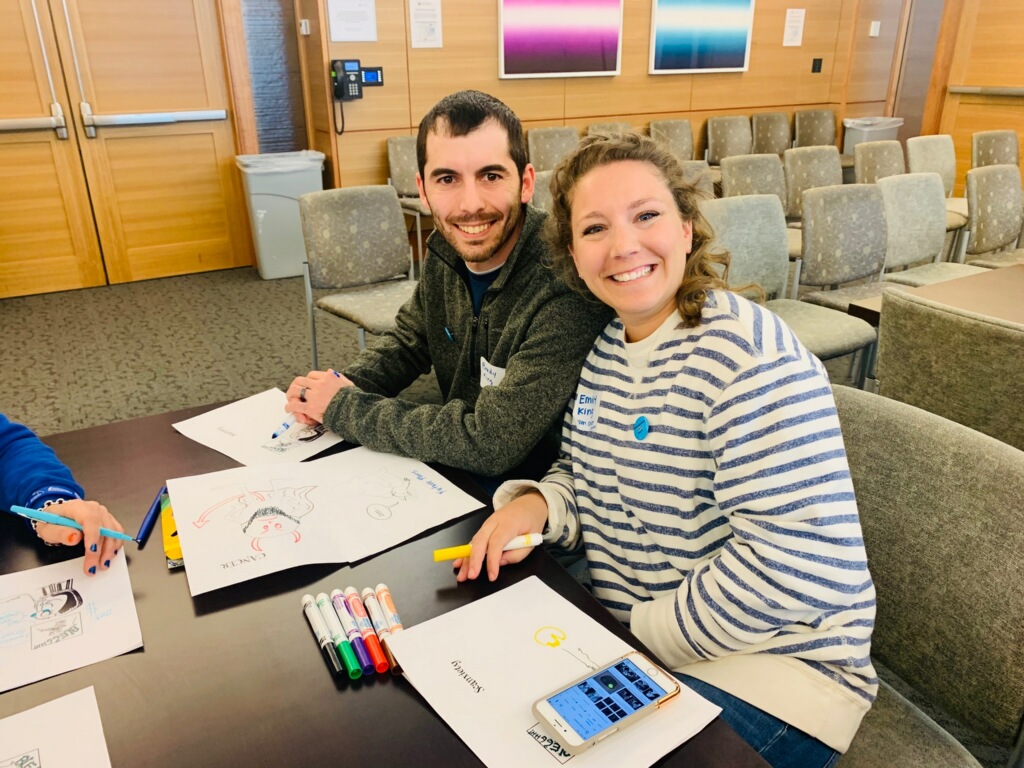
Support from the colorectal cancer community
It was hard to accept having cancer or an ostomy, so I avoided reaching out or telling people.
My mom sent me an article about a young woman going through the same thing: stage 3 colorectal cancer, has an ostomy, and runs marathons. I reached out. We quickly became best friends.
It made a huge difference to have someone who understands. I can always talk to my parents, but only she truly gets it.
What I want others to know
At first, I didn’t want to relive my journey, but I realized how important it is for young people to hear this. Colorectal cancer is often seen as an older person’s disease, but young people should still advocate for themselves.
I never would have been given a colonoscopy at 27, but if you have concerning symptoms, pay for the colonoscopy. It’s your life.
Lastly, you know your body best. Always advocate for yourself, no matter what.

Inspired by Rylie's story?
Share your story, too!
More Metastatic Colon Cancer Stories
Raquel A., Colorectal Cancer, Stage 4
Symptoms: Frequent bowel movements, pin-thin stools, mild red blood in stool
Treatment: Chemotherapy
Steve S., Colorectal Cancer, Stage 4
Symptoms: Blood in stool, changes in bowel habits, feeling gassy and bloated
Treatments: Surgery, chemotherapy, monoclonal antibody, liver transplant
Jessica T., BRAF Mutation Colon Cancer, Stage 4
Symptoms: Severe stomach cramps, diarrhea, vomiting, anemia (discovered later)
Treatments: Surgery (hemicolectomy), chemotherapy
Jennifer T., Colon Cancer, Stage 4
Symptoms: Weight loss, coughing, vomiting, sciatica pain, fatigue
Treatments: Surgeries (colectomy, lung wedge resection on both lungs), chemotherapy, immunotherapy
Kasey S., Colon Cancer, Stage 4
Symptoms: Extreme abdominal cramping, mucus in stool, rectal bleeding, black stool, fatigue, weight fluctuations, skin issues (guttate psoriasis)
Treatments: Surgeries (colectomy & salpingectomy), chemotherapy