From Life with a Newborn to Stage 4 DLBCL: Anna Navigates Her Diagnosis Through Positivity
Anna was just settling into the sweet spot of life, running a coffee business with her husband, enjoying her new home, and parenting her toddler and newborn, when she found an unusual lump while breastfeeding. Though it was initially dismissed as a common milk cyst by her OB and even after an ultrasound, Anna’s persistence led to a biopsy that revealed a shocking diagnosis: diffuse large B-cell lymphoma (DLBCL). It was stage 4, an advanced presentation that initially terrified her family and friends, but was quickly clarified by her oncologist as a highly treatable blood cancer.
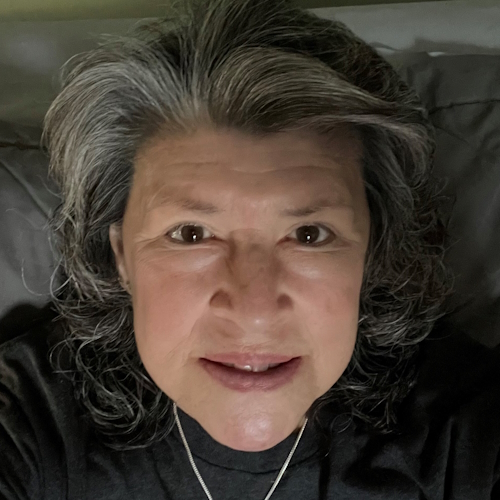
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez
Facing aggressive chemotherapy and hair loss while caring for an infant and a toddler presented immense emotional challenges. Anna had to stop breastfeeding abruptly and navigate the physical changes of treatment, including shaving her head, a moment she feared would scare her children. Instead, her two-and-a-half-year-old son’s reaction was pure love: “Oh, mommy, you look cute.” This moment, along with seeing a contestant rock alopecia with confidence on The Great British Baking Show, helped Anna embrace her new look and focus on the present joys of motherhood rather than the fears of the future.

Throughout her DLBCL experience, Anna has leaned into her natural optimism, reframing her diagnosis not as a tragedy, but as a challenge she is uniquely equipped to handle. By taking life one day at a time and refusing to wish away her baby’s first year to get to the end of treatment, she has found profound strength. Her story underscores the power of a supportive “village,” the resilience of young mothers, and the importance of advocating for yourself when your body tells you something isn’t right.
Learn more about Anna’s story by watching her video or scrolling down to read her edited interview transcript.
- Trust your instincts. Even when medical professionals suspect a common issue like a breastfeeding cyst, push for answers if something feels wrong in your body
- Stage 4 isn’t always the end. In blood cancers like DLBCL, a kind of non-Hodgkin lymphoma, stage 4 indicates where the cancer is located, not necessarily a poor prognosis; it remains highly treatable
- The “candle” analogy. Chemotherapy treats systemic blood cancer (multiple candles) just as effectively as it treats a single spot (one candle); the “water” extinguishes them all
- Children can be resilient anchors. As Anna’s kids show, young kids often accept physical changes like hair loss with surprising ease, and can keep you grounded in the present moment
- You are stronger than you think. Adversity often reveals a depth of resilience and toughness you didn’t know you possessed until it was tested
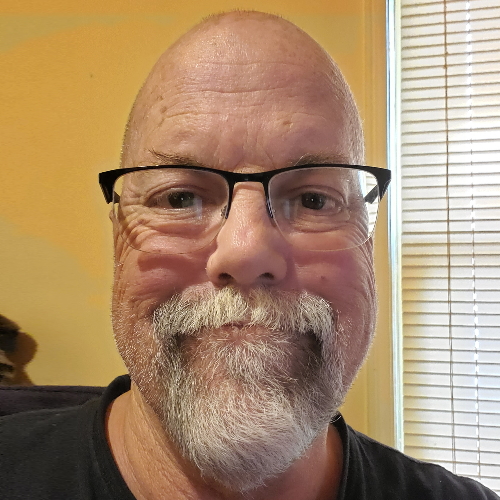
- Name: Anna M.
- Age at Diagnosis:
- 31
- Diagnosis:
- Diffuse Large B-Cell Lymphoma (DLBCL)
- Staging:
- Stage 4
- Symptom:
- A rapidly growing, painless lump on the breast
- Treatment:
- Chemotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- I’m Anna
- Life before my diagnosis: new motherhood and business
- Discovery: finding a lump postpartum
- Diagnosis: from breast cyst to non-Hodgkin lymphoma
- My initial reaction and the silver linings
- Sharing the news with my family and friends
- Understanding stage 4 DLBCL: the candle analogy
- Coping with hair loss and finding confidence
- Parenting through cancer: navigating my diagnosis with my kids
- Finding silver linings in adversity
- Looking to the future: one day at a time
- Advice for patients and loved ones
I’m Anna
I have diffuse large B-cell non-Hodgkin’s lymphoma, stage 4. I was diagnosed this year in October, and I am from Arkansas.
At this point, my biggest passion, purpose, and what I’m doing every single day is I’m a mom. I have two small boys. I have a two-and-a-half-year-old and an eight-month-old. I worked full-time before having children, but once I did, they were obviously the most important priority. Being able to spend time with them has become my life’s work, now that they exist and are alive. Before that, I worked in journalism, in storytelling, in instructional design. That was my career before children.
My husband and I also own a coffee company. We do events. We take coffee catering to events like weddings, corporate events, and birthday parties. We basically get to be at people’s greatest times, serving coffee and talking to people in the community. It’s really fun. It’s been a really good way to stay connected while I am a stay-at-home mom. I would say my number one passions are my children and then being in the community in some aspect, getting to be involved with people, especially on people’s wedding days. That’s just the most fun thing ever because it’s their happiest day, and getting to witness that, even if I’m just serving coffee, is really cool.
I have kind of always been this way, smiling. I actually had to learn in my adult years how to be angry and how to deal with negative feelings because I had some. At times, it might be toxic positivity, just always being so positive and kind of ignoring and shoving those other feelings to the wayside. But I think as I’ve grown, and especially as I’ve dealt with adversity, I’ve learned that you can have both at the same time. You could recognize the bad and still feel the good and the joy and the positive, which I think has been really important to learn. Cancer has been another thing that has taught me that.
My mom instilled in us when we were little to be able to laugh at ourselves and not to take ourselves too seriously. I think that has just made me always find the silver lining or the brighter side, or to help other people feel that. If it’s kind of like — I’m sure you saw some of my videos making fun of my no hair or bringing light to my baldness — I will make myself not the butt of the joke, but I will make a joke out of something if it means somebody else is going to laugh. If it can bring some positivity and some joy to someone else. I think I can turn situations into that for myself. It’s just always kind of been ingrained in me since I was little.
Life before my diagnosis: new motherhood and business
Right before diagnosis, I had a baby, this April. We were just in the sweet spot of postpartum. We have the happiest baby. He is just the smallest little guy. So we were just really soaking up being second-time parents. We kind of know a little bit more about what we’re doing. We’re not as terrified because we’ve already done it once. Our older child was really excited to be a big brother.
Our coffee business is doing really well. We ordered a coffee roaster so that we could spread our reach; we wanted to be able to sell coffee to people, to be able to ship it, and spread the people that we’re able to serve, rather than just locally. We were kind of just in the groove. We were flowing. Being parents, being business owners — my husband’s also a teacher. So we were balancing all of these different things. Really getting into the groove of being new parents again and just enjoying life. My children and I were going out on adventures in town and playing outside, and just getting ready. I think whenever we found out about cancer, we were prepping for Halloween and getting the costumes ready.
Life just seemed like we were in a really good, sweet spot, which we were. A new baby brings so much joy and positivity. And as I said, he’s a really happy baby, too. We’ve owned this business for four years. So we were really in the flow of that. We were doing some renovations to our home as well because we’ve lived there for four years now. Everything was just kind of in a really sweet spot in life. We were thinking about when we’re going to do some camping trips and traveling because we’ve got the hang of being second-time parents. We weren’t as scared to take our baby out. Everything just seemed like life is good. Nothing’s really wrong. I was getting into the groove of working out again and just starting to feel like my normal self after having a baby. And then everything kind of changed. There’s still a lot of goodness, like I said. But that was life before, just a few months ago.
Discovery: finding a lump postpartum
The main symptoms of the cancer that I have are fatigue, night sweats, a fast-growing, painless lump in one of the lymph node areas (or outside of, in my case), and unexplained weight loss. For me, I was postpartum. Obviously, I was fatigued. I’m not sleeping through the night yet. I had lost weight because I had just had a baby. So that kind of explained it. Nursing and having a new baby and hormone changes — sometimes you do have the occasional hot flash, night sweat, whatever. So any symptom that I was having, I was unaware of because they were all kind of masked as just being a new mom, postpartum, and hormonal changes.
There was one night when I came back to go to bed after putting my son down, and I told my husband I felt a lump. I said, “Does this feel weird to you?” I found a lump in my breast. He was like, “Yeah, that definitely seems like kind of a big lump. Maybe you should call your doctor and get that checked out.”
I called my OB, and she was like, “Oh, we’ll get you in. It’s probably just breastfeeding-related because that happens a lot of the time.” She expected it just to be a cyst of sorts. Then she sent me to just get it double-checked. She was like, “I’m pretty sure it’s just a cyst from breastfeeding. But let’s go ahead and get somebody else who specializes in this to look at it.”
She sent me to get an ultrasound and a mammogram. They said the same thing: “It looks like it’s probably just a cyst from breastfeeding.” I think looking back now, that was probably because it wasn’t breast cancer, so it didn’t present as a typical breast cancer would. Anytime they looked at it, they were like, “Yeah, I don’t know. It’s kind of in the gray area, but most likely a milk cyst.”
Diagnosis: from breast cyst to non-Hodgkin lymphoma
They ended up deciding on a biopsy. Then once the biopsy came back, of course, this all happened in two weeks from when I first discovered it to finding out. They called me. The doctor who did the biopsy called me, and he said, “Your results came back, and they’re very interesting, a little unexpected.” I was like, “Okay, go ahead.” And he said, “Well, you don’t have breast cancer.” I was like, “That’s great news. Thank you. I’m so thrilled.” And he was like, “But you do have cancer.”
I just felt chills and the wave of… I think I started trembling, just thinking, You just told me I had cancer. Did I hear that right? He said, “You have non-Hodgkin’s lymphoma. It’s called Diffuse Large B-Cell Lymphoma. Do you have any questions?” I was like, “Well, yes, but I can’t think of any of them right now.” I think I asked a question that was just the first question that came to my mind, and he was like, “Actually, this is not my area of expertise. I’ve already sent this over to an oncologist. They’ll reach out, and they’ll be able to answer more questions.”
Really, truly, I didn’t notice any symptoms. Even when my blood work was drawn, it was relatively normal. There was no indication that there was cancer. It was really just that fast-growing, painless lump that I felt. Thank goodness I didn’t brush it off or just think, Oh, we’ll see what it does in a few weeks or anything like that. I’m really glad that people took me seriously when I showed, “Hey, I think this is a little abnormal,” because I know sometimes people will do that, and they’ll say, “Let’s just watch it for a little bit and see.”
My initial reaction and the silver linings
In a way, I thought our life was derailed at first. I was talking with a good friend from college the other day, and he was asking me all of these questions and really getting me to think about things I hadn’t thought about yet. I gave him back an answer, and then he said, “I’m not glad that you have cancer by any means. But I am so glad that you are you if this was going to happen to you.” I think what he meant is really just the way I have always just kind of been able to turn something into that silver lining to look for it.
Looking back, I’m just seeing all of these things that set us up for this diagnosis. Yes, we were in a sweet spot, but we were also so set up for this to happen. I bought a house right next door to my mom four years ago, so I have help right next door. I just had a baby, which is like the most joyful thing you can see every day. It reminds you that there is good even when bad is happening. As I said, I have the happiest baby. Anytime I would feel sadness or start to think about what was going on, I would look over, and he’s just smiling at me. It’s like, Okay, this sweet spot that we’re in, this place that we’re at, really sets us up for this to happen.
I also think in my family, not that I would ever want anybody to have cancer, but if somebody in my family was going to have to have it, I’m glad it was me. I feel like that sounds so weird to say, but it definitely feels like if it had happened to anybody else, it would have been harder emotionally for me. I’m looking at my family members and I’m like, I’m so sorry that you have to feel this because I know watching someone you love go through something like this is really hard. Being a mom now, I look at my mom and she’s been so positive and so helpful and so encouraging, but I know that there are times when it’s just really hard to watch your kid go through something like that. I can’t even imagine. My kid has a fever, and I’m like, The world is ending. So it’s definitely been a 180 from the sweet spot. But I know that it set us up to have the best experience that we could if something like this was going to happen.
Sharing the news with my family and friends
Telling people was really hard because I kept trying to find a convenient time. When I found out, I immediately went and told my mom and sister because they work close by. So I was able to get my kids in the car and drive to where they were. I waited until my husband got home that day because I didn’t want him to hear that news while he was in charge of other people’s kids. That is not a good time for that.
I definitely felt a lot of vulnerability and a lot of emotions and a lot of fear right away. You hear the words, and then you don’t know. I didn’t even know what lymphoma was before I was diagnosed. I didn’t know staging yet, or treatment, or what anything was going to look like. That was hardest for me: to not know what was going to happen and to just have so many questions. That’s when I think I showed a lot of my vulnerability and a lot of fear and anxiety. Everybody else kind of met me with their emotions, too, which I think was probably the best response to know. A lot of times, certain medical revelations or diagnoses can almost make you feel like you’re overreacting. When my emotions of fear and anxiety were met with the same, I was like, Okay, this makes me feel validated and like we’re ready to fight together. It was good to be met with that in the beginning. Once I started to know that there was a plan and it’s very treatable, I started to feel more positive, and then in turn, my family felt the same way.
As far as telling friends and other people, I was really nervous. I just didn’t want to inconvenience anybody or cause them to have a bad day. I was looking at people’s locations, like, Okay, are they at work? Are they at a friend’s house? I would text people and be like, “Hey, what are you doing?” And they’re like, “I’m just working. Why? What’s going on?” And I was like, “Oh, nothing. Just, you know, I have a funny story to tell you, but just let me know what you’re doing later.”
No one tells you how to break bad news to somebody else. I tried to make light in a lot of the ways that I told people. I’d be like, “Turns out I have cancer.” And my friends are like, “What? Wait, what did you just say?” And I’m like, “Yeah, I know, crazy, right?” Probably not the best way to do it, looking back, but you don’t know what to do. I had never had anybody personally break that news to me about them. I just really had no way to know how I should go about it. So, typical me, I tried to make it a lighthearted thing. Telling people was hard for sure. But once I started to, I felt like it really just helped me know how many people were on my team. And it was even further reinforced. Okay, I can do this. Like, there is nothing that I can’t handle with this village backing me.
It makes people feel better, too, if they have some facts, some information they can kind of hold on to. I had people who I knew were going to start Googling, and they’d end up on WebMD. I’m like, “This is what I know. Don’t Google it because it sounds scarier on Google than what the doctors told me. If you have questions, ask me, and I’ll make sure we address any concerns. Don’t go on Google.”
Understanding stage 4 DLBCL: the candle analogy
Initially, when I told my husband, he was terrified. The word cancer — he was like, “You’re going to die. This is the end of everything. This is the worst news.” I was like, “Okay, wait, let’s get some more information. We don’t know anything yet.”
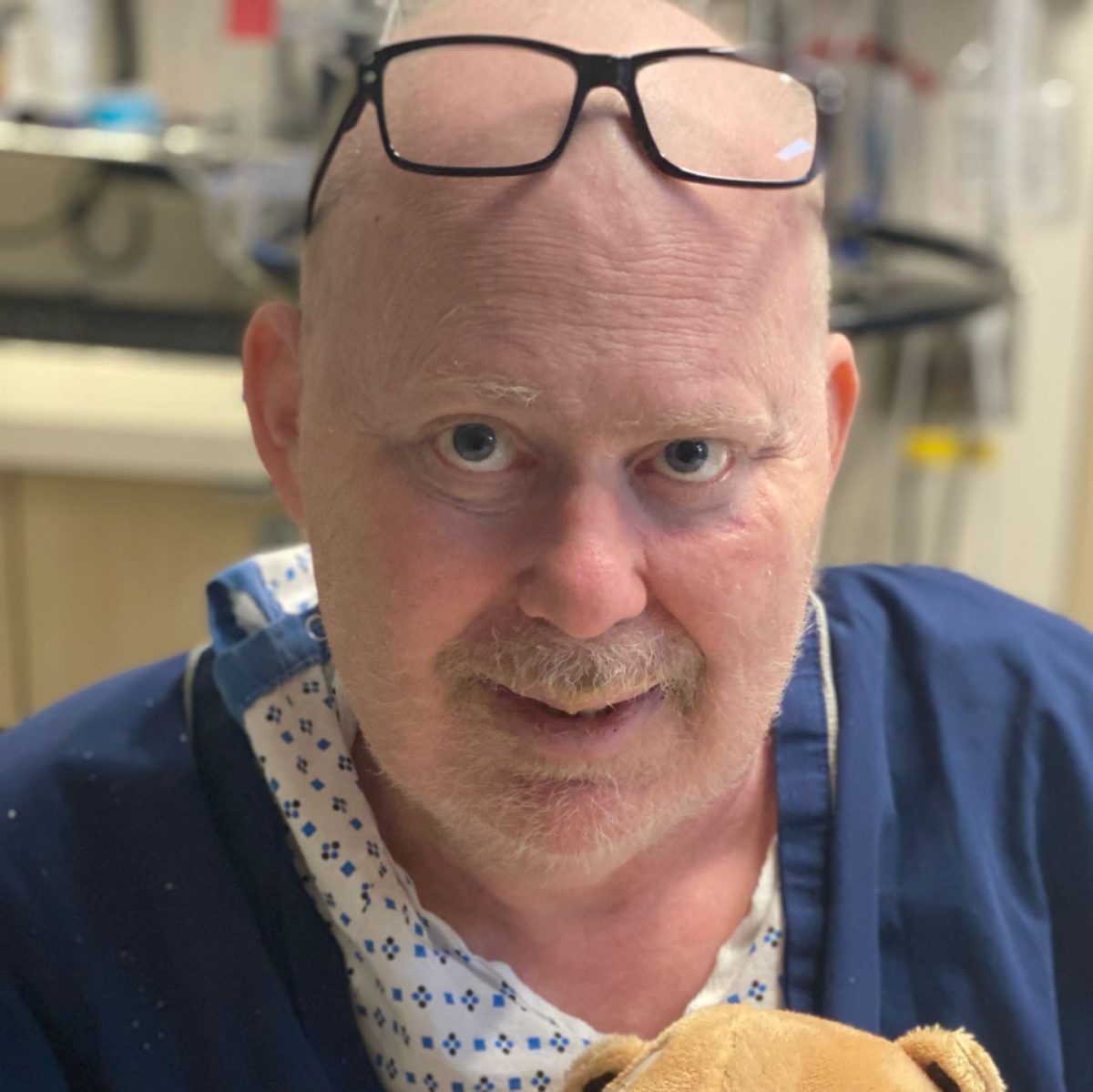
We met with the doctor. Initially, it was before the PET scan. He did blood work and an initial exam, and he was like, “You’re not symptomatic. Your blood work looks really good. I think it’s probably stage 1 or stage 2. We’ll get your PET scan next Friday, and then you’ll come back and meet with me again, and we’ll get a plan.” He told me that he would not call me unless it was bad news.
I was the only one who knew that if he called, it was going to be bad news. Nobody else knew that. I was by myself that day because I had a PET scan, so I couldn’t be around my children. My husband’s taking them out to keep them away from my radioactive self. I get a call while I’m in the shower. I miss it, of course. It’s my doctor. He leaves me a voicemail, and he’s like, “Hey, give me a call back. I want to talk to you about your PET scan results.” I was like, Oh, crap. I immediately called back, and it was after 5:00. I don’t get him. I’m like, Oh my gosh, I’m gonna have to wait till Monday to know. I was trying to talk myself into… maybe he just wanted to tell me, “Stage 1, like you’re good.” But I knew he had said, “If I call, it’s probably just because it’s a little bit more serious.”
On Monday, a scheduler called me first, and they were like, “We’re going to move your appointment from Tuesday to Thursday.” I was like, “Why?” She said, “Well, insurance hasn’t approved your treatment yet.” I was like, “My treatment? I’m just supposed to meet with the doctor.” She was like, “No, no, no, you’re starting infusions on Thursday.” I was like, “Wait, what? What are you talking about?” She was like, “I think Dr. Lopez is going to call you soon.”
He called me shortly after, and he was like, “Hey, I just want to let you know. The PET scan came back. It is stage 4.” And he was like, “But blood cancer is different from tumor cancer.” He immediately told me that information. For anyone that doesn’t know, when you hear stage 4 lung cancer, that’s very different from lymphoma stage 4. That just means that there are lymph nodes that have the active cancer in them on both sides of the diaphragm. That’s stage 3. Stage 4 is also in somewhere other than a lymph node. I had a spot on my mediastinum and also a spot in my breast, which were not lymph nodes, and then a spot behind my abdomen.
He told me that, and he said, “The treatment changes only slightly. There’s one different chemo that we use from 1 and 2 to 3 and 4. The prognosis is still really good, almost the same. It hardly changes.” I had that information right away. I was like, “Okay, so this is different.” I tell my family, and they’re all still like, “Stage 4…” And I’m like, “No, no, no, listen.”
I tried to give the analogy — I just made this analogy up — and then I told my doctor, and he was like, “That’s actually really good. I’m going to use that.” I told my husband, “Think about a candle on a table, and you pour a bucket of water on the candle. The candle is going to go out. Now you fill the whole table with candles, and you pour the same bucket onto the table with multiple candles. All those candles are still going to go out. That’s kind of how the treatment is working. The chemo is going to go to all of the cancer just as efficiently as it would to one spot, stage 1, stage 2.”
He was like, “Okay, it makes me feel a little bit better.” Being super informed right away did kind of make that feel better. But it still did feel like, Oof, it’s kind of a little bit scarier than what we thought it was going to be. It just kind of felt like things kept happening like that, where we were like, Okay, we think it might just be this. And then it was like, Actually, it’s this. But we are still positive. We’re still hopeful. Treatment’s still going to be really good. I’m thankful that my doctor has the personality that he does. I told him from the get-go, “I am a hypochondriac and medically anxious, so you’re gonna have to give me all the information. You’re going to have to give it to me straight. No beating around the bush. No softening things. I want to know everything.” He was like, “Okay, sounds good.” And he has done that throughout.
Coping with hair loss and finding confidence
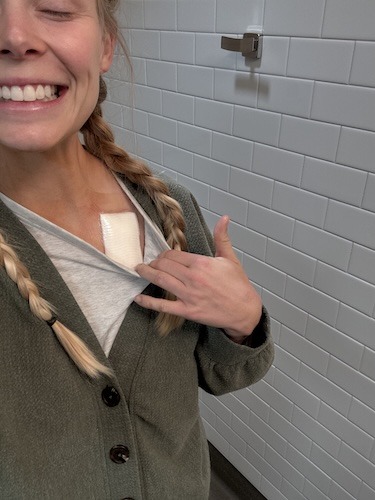
If you had told me, probably a year ago, that I was going to lose all my hair, I probably would have absolutely lost it, freaked out, just because it’s all I’ve always had. The long blond hair. It’s kind of been like, if someone didn’t know me, they would say, “Oh, the girl over there with the long blond hair.” You see me in a supermarket, you know it’s me for sure.
The doctor told me the first time we met that chemo was the treatment for lymphoma, no matter what stage, and that I would lose my hair because of one of the chemos. That’s just what it does. The “Red Devil” — I can’t remember the proper name for it at the moment. “That’s one of your chemos, and you will for sure lose your hair.” I asked him about cold capping, and he said, “You can do it. It’s not super successful. It’s not super great for lymphoma, especially with the breast presentation.” I had a higher likelihood of central nervous system involvement. So there was a treatment that needed to go all the way through, the whole body. He said it extends treatment, and it’s really expensive, not covered by insurance. I was like, “Okay, that’s fine, no worries.”
I was prepping myself from the very beginning, but something that actually helped me be okay with the fact that I was going to lose my hair — a lot more so than I thought I would have been — I watched The Great British Baking Show. Have you ever watched that? This season, the winner had alopecia, and she was open about that throughout the show. So she’s bald as well, doesn’t wear wigs or anything. She talked about that early on in the season. She said she used to wear wigs, and she doesn’t anymore. She’s really found her own style, confidence, and beauty. She was a med student on this baking show. Really successful, really good. I was just like, Okay, she has found the confidence to do this, and she looks wonderful. She’s unique, and she’s rocking it. Watching her prepped me. I was like, “If Jasmine can do it, I can do it.”
I was still a little emotional when I cut my hair because it’s always been really long. It’s really short. I don’t think it’s been that short since I was a little kid, and it was growing from my head for the first time. Shaving it obviously was a little emotional. My husband was shaving it, and he was like, “I’ve never seen your scalp.” And I was like, “I’ve never seen my scalp.” I was born with more hair than this. So it definitely was shocking and emotional. Sometimes I still forget that I don’t have hair, and I’ll see myself, and I’m like, Whoa, that’s me. I’m bald.
People are really kind about it and tell me, “You have a smooth head, like that looks pretty good.” Sometimes little kids will look at me, and I can tell they’re like, What’s going on there? And I just smile at them. I know that they just don’t know any different. It doesn’t bother me. It is a reminder for sure that I don’t have hair anymore. Making jokes out of it as well helps. I don’t know if you saw that video, just me being silly. But it definitely has helped me process losing it. I have a wig too, which I can wear sometimes. That was gifted to me by a really good friend. I’m thankful to have been prepped and to have different ways to make me feel best in my body, how it is right now, and to feel confident if I need them.
Parenting through cancer: navigating my diagnosis with my kids
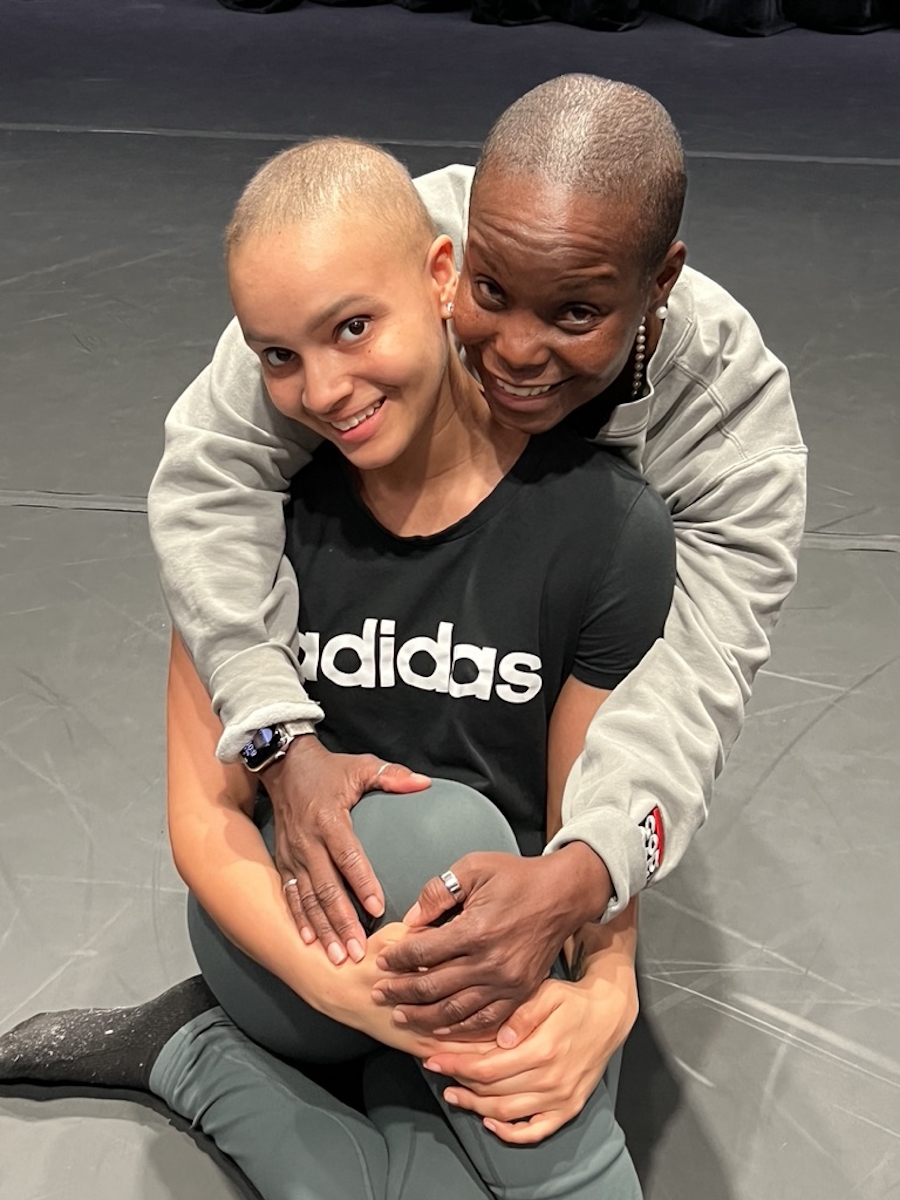
My two-and-a-half-year-old would always play with my hair when I would hold him. He does the same thing with his own hair. He’ll play with it as he falls asleep. It’s always how we know that he’s getting tired. But when I would hold him, he would play with my hair and just kind of pull it and take the really long piece. He loved to brush it. He thought that was the most fun thing ever. So we were really nervous that he was going to look at me like, Oh my gosh, who is that?
We let him watch. He was with my parents. Both my kids were there when my husband shaved it. And when I cut it too, I thought, Oh no, he’s not gonna like that. Big change. And I think his response was, “Oh, mommy, you look cute.” He’s just the sweetest thing ever. Everyone was there. He got to see it being cut. I think that helped him to be like, Okay, I see it actually falling off. Mom’s getting a haircut. It put things in place for him.
When we actually shaved it, he was with my parents, and I put a hat on after it was done. So when he saw me for the first time, it wasn’t just a stark difference. Then he kind of noticed. He was like, “Mommy, where’s your hair?” I said, “Oh, well, buddy, I’m taking some medicine. And it made it all fall out.” He was like, “What? Where is it?” And I said, “It’s in the trash.” And he was like, “Oh, is it going to come back?” I was like, “Someday. Yes.” He said, “Can I see?” I was like, “Okay, sure.” I took the hat off, and I said, “Do you want to touch my head?” He was like, “Yeah.” And he just kind of rubbed. I was like, “Isn’t that so silly?” He was like, “Yeah.” And then that was it.
He didn’t talk about it anymore until I got a wig. I came home with a wig on, and he goes, “Are you a different mommy?” I was like, “No, the same mommy, just different hair.” He was like, “Your hair came back.” I said, “No, buddy, it’s a wig.” I took it off and showed him, and he said, “Oh, so pretty.” Anytime I put the wig on and come out, “Oh, mommy, you look so cute.” He has handled it beautifully. Better than I could have ever imagined. We were really nervous about that. One of my friends is a child life specialist, and she was like, “I need to talk to him. If there’s anything you want me to explain to him or talk to him about, let me know.” I was like, “Yeah, we might need to do that, especially with this big physical change that he can see because he can’t tell otherwise that something’s going on with me.” But no, he handled that great.
My youngest… I think he looked at me kind of funny the first time. Then I smiled at him, and it was like, Okay, that’s it. We’re good. Same mom. My wig is a little darker than my natural hair, so I’m sure he was like, Oh, there you are. That’s what I think when I smile, they’re like, Those are my mom’s teeth. All right. Cool.
There is some sweetness to it because it is a good distraction all the time. Anytime I’m feeling down about what’s going on, I have a great reminder of happiness and joy and lightness. Kids keep things so upbeat, and they kind of keep you busy enough that a lot of times you’re not really thinking about it anyway. But there have been some moments where I have just compared my experience with my youngest this time to my experience with my oldest. I didn’t have anything taking me away from being a mom to a newborn or to an infant before. Now I’ve stayed away from them longer than I ever have before. I had to stop my breastfeeding experience because of chemo. I’ve had to do bottles, and that’s been really different.
My husband has been really great about taking things on. He said, “I hate that this is why we’re doing this. But I’m really thankful that I’ve gotten an attachment to our youngest, Shepherd, so much earlier than Harrison, our older son. He was so much more attached to you for so much longer.” I’ve kind of had a different experience with him, which has been really cool for me. And then my experience has given me some independence sooner than I would have had with my oldest. So there’s been some goodness to the hard as well.
I had to stop thinking, Oh, I’ll be so glad when treatment is over. I’ll be so glad when I’m on the other side of this. If I can just get to being cancer-free, then I can start enjoying life again. I was thinking about that. I was like, Okay, so that’ll be next May or June if we stay on track with everything. I have a one-year-old and a three-year-old. I will have wished away the whole first year of my youngest son’s life. So again, they are really keeping me in that mindset of I still need to enjoy every single day, despite the hard stuff.
There are days when I’m tired and anxious, and I need to just kind of step away and take a moment. Luckily, I have a support system to be able to do so. But most of the time it’s a reframe. It’s just this constant flipping in my mind of feeling the anxiety, feeling the sadness from it, but then remembering, Look what you have right in front of you. Don’t let these other things that are going on take over the good parts of life that are happening right now, too. My husband even said at one point, “I hate that this is happening, but why did it have to happen when we have small children?” I was thinking the same. Why couldn’t it have happened before we had kids? And then I was like, Well, you know, now that I say that though, they make every day so much better, no matter how I’m feeling. Maybe if this was going to happen — of course, again, thank God it’s happening at this time because I do have these constant little smiles at me all the time. You can’t be upset when these little faces are smiling back at you. It’s been different, but so good to be able to have this experience and to be able to treasure them even more. Once you hear those words, cancer, you’re looking at things so differently.
Finding silver linings in adversity
For sure, getting out of the house with both of them helps. Even when I am feeling really tired, leaving the house helps with that a lot. Having family so close is really helpful, even just to get in a different space with another person, with the kids. It’s like, Okay, I’m remembering that we can be normal while these things are happening, too. My husband can be home anytime I am not feeling well. That’s really helpful too, to be able to know that I have certain days where if I need extra rest, I can take it. But for the most part, it’s like, Okay, this is my sweet spot to be with them.
I think prepping for the holidays, whether it be Halloween, Thanksgiving, or Christmas, has really helped as well to have those moments. I want to make this really magical for them. I want to make things exciting and happy for them. Filming my experience and sharing that has been really helpful, too, to just kind of talk about it to make it less scary for other people. I know it can be really daunting. Before I had my first PET scan, I was like, Oh, that sounds terrifying. I’m going to be in one of those little tubes and being enclosed. Things just seem so much more daunting when you don’t know anything about them. So that’s been really helpful too, to have that outlet. I’ve had so many people say things back to me like encouragement and say that, “I was just diagnosed and watching your videos, I hope that I can stay positive as well. Thank you for sharing. You gave me the courage to go and get something checked out.” Even though I have little kids, just things like that… just little reminders that when I am feeling positive and happy and absorbing those moments, it really is making a difference.
I think I gave you the little phrase, “There’s nothing that I can’t handle.” I think that I have learned that over this amount of time because I think I downplay who I am and what I do a lot of the time. Oh, I’m just a mom. Oh, I don’t work. I just stay home. Or I just help my husband with his business. I think dealing with something like this and just thinking, Okay, this is what happened. I’m going to face it head-on and keep being positive. I didn’t realize that I was doing something kind of different here or that I was taking such a positive take on it. When I first heard about cancer and realized what kind it was and how treatable it was, I was like, Okay, there are so many people dealing with heavier things. Things could be so much worse. I think I try to always look at things like that anyway.
Even after my first chemo, I didn’t feel super bad afterward. I was tired, but I was thinking, Okay, that was pretty smooth. I can do this for sure. But then I had friends and family members being like, “You have cancer. Like, this is a big deal.” Not everyone will experience that. I remember my husband telling me that after I had a C-section, he was like, “You are a lot tougher than you give yourself credit for, mentally, physically.” I’m a small, petite woman. I’m not super muscular or strong or anything like that. I don’t think of myself as tough. But I have realized, especially in the past few months, that I am pretty tough and there is a lot that I can take and a lot that I can handle. If I can go through this, there’s absolutely nothing that I can’t handle past that, which is a good reminder.
Sometimes it’s the little things in life that get to you, and then a big thing happens and kind of gives you perspective on, Okay, why did I get so upset in traffic? Or why did I let that sleepless night with my kids make me have a bad day the next day? That’s nothing. I faced this, now everything else seems so small. I’m really grateful to have that perspective now. I’m more resilient than I thought. I hate for anybody to have that tested with adversity, but I feel like that’s the only way you really know how strong you are, is for your strength to be put to the test.
I’ve learned how much people care about me, which is a really unique thing to get to actually hear from people. Once I was diagnosed and started sharing my experience, people reached out. I had a teacher that I had in high school reach out and tell me, “You were always one of the most positive students that I’ve had.” It’s really cool to be able to hear what people think about you. It’s kind of reminded me to do the same for others. If you feel like you want to tell somebody something about what they mean to you, do it, because you never know how it will make them feel.
Looking to the future: one day at a time
That was hard for me, and I felt that was going to be the hardest part: to think about things a few months out or even to think about life after cancer. I feel like I’m always going to be thinking, Is it back? Is something else going on? But I’ve heard a lot of people who have also had cancer or dealt with a large adversity: take it a day at a time. And I think that is the best advice that you could receive. Take it a day at a time, and when you take it a day at a time, it allows you to be more present in that day because you’re not thinking about the future.
So that’s really just a day at a time — sometimes a week at a time, if I know what’s going to happen a week from now. But I try not to push too far forward because I feel like I can kind of get a little bit too in my head if I think about the hospital days that are coming up, or if I try to just digest everything that’s going to happen. But if I take it a day at a time, I mean, I can handle that for sure. One, just one little day at a time. No big deal.
Advice for patients and loved ones
For anyone going through something similar or anyone loving someone who is going through something similar, there are no dumb questions. Getting a second opinion is great. Lean on people who love you and whom you trust. And if you are someone loving someone else going through something like that, show up and be present and show people that you care, even if you feel awkward or if you don’t know what to say. You don’t have to say anything. Just being there is so special and helps people know that they can do anything and they can handle anything.

Inspired by Anna's story?
Share your story, too!
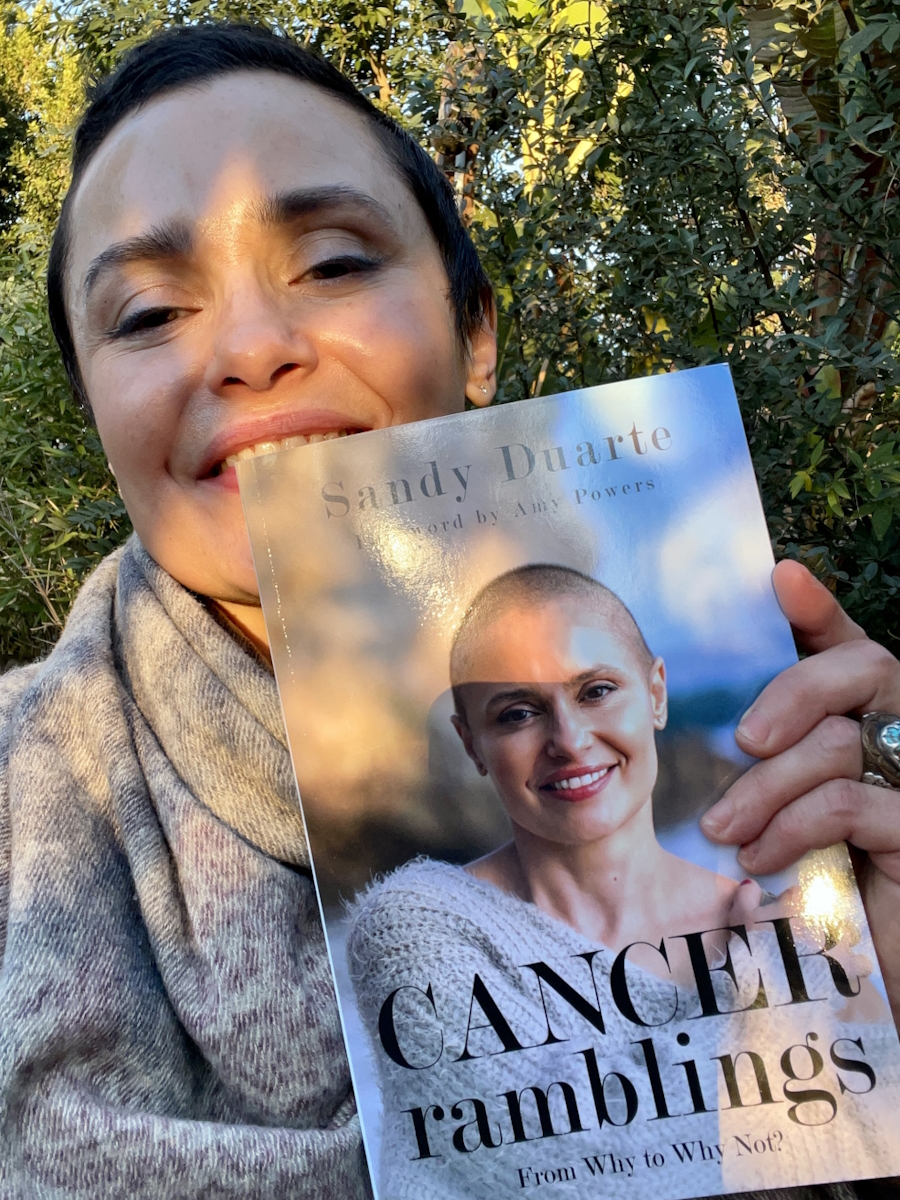
More DLBCL Stories
Anna M., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: a rRapidly growing, painless lump on the breast
Treatment: Chemotherapy
Ashley P., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Feeling like holding breath when bending down or picking up objects from the floor, waking abruptly at night feeling “off,” one episode of fainting (syncope), presence of a large mass in the breast
Treatments: Chemotherapy, bridge therapy of chemotherapy and radiation, CAR T-cell therapy
Melissa B., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Lump in the left breast, persistent rash (started near the belly button and spread), intense fatigue and energy loss
Treatments: Chemotherapy (R-EPOCH), Neulasta, radiation therapy, surgery (to remove scar tissue and necrosis), autologous stem cell transplant
Jen N., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4B
Symptoms: Blood-tinged phlegm, whole-body itching, shortness of breath, lump near collarbone, night sweats, upper body swelling, rapid weight loss
Treatments: Chemotherapy, immunotherapy, lumbar puncture, autologous stem cell transplant