Christine’s Relapsed T-Cell Acute Lymphoblastic Leukemia Story
Christine shares how she got through treatment and a relapse for T-cell acute lymphoblastic leukemia (ALL), including chemotherapy and a bone marrow transplant.
She also highlights how she navigated life with cancer, figuring out fertility preservation, how she managed work with cancer, and how the diagnosis impacted her marriage. Thank you for sharing your story, Christine!

- Name: Christine M.
- Diagnosis:
- Acute lymphoblastic leukemia (ALL)
- T-cell
- Staging: N/A
- 1st Symptoms:
- Enlarged lymph nodes
- Pain in abdomen
- Nausea
- Treatment:
- Chemotherapy
- Hyper-CVAD
- Cyclophosphamide, vincristine sulfate, Adriamycin & dexamethasone
- Hyper-CVAD + Nelarabine
- Hyper-CVAD
- Intrathecal chemotherapy
- 17 rounds total
- Bone marrow transplant
- Chemotherapy
- Diagnosis
- Treatment Decisions
- Chemotherapy Treatment
- Overcoming a Relapse & Complications
- Relapse Treatment Plan
- Bone Marrow Transplant
- Reflections
- How has your cancer experience changed your perspective?
- What helped you through your lowest moments?
- Fertility after cancer
- Paying for cancer treatment (financial toxicity)
- How has cancer impacted your work?
- How did cancer affect the relationship with your husband?
- Advice for someone who has just been diagnosed
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
One big thing is remembering that it’s okay to say no. Do not be a people-pleaser during this time of your life. If someone wants to come visit and you don’t feel up for it, say no.
Your job is to get better. Don’t feel like you have to say yes.
Stand up for yourself if you’re not comfortable with something. Be true to yourself and take care of yourself.
Christine M.

Diagnosis
What were your first symptoms?
I was on a week-long vacation. I felt fine. I didn’t notice anything different. The next day, I was pulling up my hair at work, and I noticed an enlarged, rock-hard lymph node.
I let it go. I was like, “I just took a week off of work. I don’t have time to be sick.” I ignored it, and I didn’t really feel different.
By the end of the week, I had a few more pop up along the back of my neck. Toward the end of the week, I developed a pain in my right abdomen. It was really intense, and it only came at night and in the morning.
Again, I ignored it. I thought I was just run down from a busy summer. It went on another week, and it was getting worse.
By the third week, I would wake up, vomit a little, put a heating pad on it, rest for about an hour, and go to work. I would do the same thing at night. At that point, I had 8 lymph nodes around my neck.
My husband said I needed to see a doctor. I called a regular family doctor. They talked to me and went through my symptoms, which were the lymph nodes and the pain in my abdomen.
What happened at the first doctor’s appointments?
They were not concerned with the lymph nodes at all. They didn’t think it was connected. They just asked me a bunch of questions, and they pretty much determined it was a gallbladder issue. They pressed on my stomach, and it was tender on that side, so they assumed that was the issue.
She set up an ultrasound for the next day. It showed a few lesions on my pancreas and nearby, but she really downplayed it. She said she wanted to do a CT just to be safe, so we did a CT scan.
I wasn’t really scared of anything because she was downplaying everything. When I got the CT done, the technician was asking if I had any history of cancer or cancer in my family.
That’s when I started thinking it might be a little serious.
I went to lunch after the CT. This was a Friday, and they said I’d probably have results by Tuesday, but I got a call an hour and a half later.
They told me I needed to come right away. I knew at that point that it was going to be bad, so I went and got my husband from work and brought him with me.
We went to the doctor, and we were in the waiting room. I knew I felt different somehow. I felt like people were looking at me differently.
We got called back, and I went to sit down. The doctor said, “I’m glad you brought your husband. I should’ve told you to bring him.”
She thought I had lymphoma at the time. Every organ in my abdomen lit up. I didn’t even know organs had lymph nodes. They were assuming it was a lymphoma of some sort, but we didn’t know what kind.
What happened after the preliminary diagnosis?
She scheduled an appointment for me. Her practice is next to the hospital, and there was an oncologist’s office connected to the hospital. She set me up with the oncologist.
Thank goodness everything happened so quickly. Plus, my doctor was taking care of setting everything up for us. The process was really smooth. It only took a week for me to get unofficially diagnosed and set up with the oncologist.
How were you feeling when she gave you the preliminary diagnosis?
I just took it like it was my path. I realized that I just had to get through it.
My husband was way more shocked than I was. He asked way more questions than I did. I don’t remember asking any, actually. I sat there and accepted it, but that was probably because I was in a daze.
»MORE: Patients share how they processed a cancer diagnosis
My best friend’s baby shower was the next day. I called my husband’s family, my family, and I let my 2 best friends know.
They offered to reschedule the baby shower, and I was like, “No way, I just don’t really want to talk about it. I want to try to be normal.” I went through the weekend feeling like things were up in the air.
First appointment with the oncologist
That was really nerve-wracking. My family says I was getting more and more tired by the day. My husband was super nervous, so my mom went with us. My husband tried on like 10 shirts that morning. He couldn’t focus on anything.
I was super sick by that point. My stomach was really hurting. We got to the appointment, and the oncologist was super nice and knowledgeable.
He immediately put us at ease. He let us know that the first step was to do a biopsy.
This was a Monday, and that was going to happen on Wednesday. He was going to take a lymph node out of my groin area and see what was going on. He was very reassuring, and he said the success rates are really high with this type of thing.
I don’t remember too much about the appointment other than him saying we would do a biopsy and make a plan from there.
Describe the lymph node biopsy
I went under, and they took a lymph node from my groin area. Everything went smoothly. The doctor who performed the biopsy went out and told my husband that they could tell right away that it was cancerous. She said it was probably cancerous, but they just didn’t know what kind.
Getting the biopsy results
I think we had to wait another week to get the results. I got a phone call from the oncologist himself.
He said, “I’m sorry to tell you, it’s acute lymphoblastic lymphoma.”
Treatment Decisions
Deciding where to go for treatment
They called it lymphoma at first. He said it was too difficult for him to treat and that I needed to go to a bigger center like Hopkins or George Washington University.
When I found out he couldn’t treat me because it was too aggressive and rare, that was hard. He offered to let us come in right then and talk to him in person.
We went in and were shocked. He told us it was going to be really hard and wished he had better news. He said it was treatable and can be curable, but it wasn’t going to be easy.
He had already set up an appointment for the next day. He had an oncologist friend right across the street from George Washington University. He told us to research some hospitals and make our own decision, but he wanted us to at least go talk to someone the next day.
He said we might want to pack a bag because they might want to keep us overnight. We thought that was absurd.

You were admitted to the hospital in D.C.
We went with my mom and my sister. They came to listen. At that point, it was really serious. I couldn’t stand. I couldn’t breathe. I was really tired and had bruises all over my body. Things were really progressing quickly.
We did not pack a bag, and that was a mistake because then I was in the hospital for 3 weeks. He threw me right into the hospital.
First appointment with new oncologist
I was super naive. He talked to us, but I can’t remember much except that I needed to be admitted for 4 to 6 weeks for induction chemo. He wanted me to get admitted right away because I needed blood and platelets.
Discussing preserving fertility
He also asked if we had kids. We said no, and he said we had the option to freeze eggs. He told us that I had a very strong chance of being infertile after the process, but he also told us he didn’t think we should wait.
My husband and I looked at each other, and he said, ‘She’s our priority. We’ll worry about that later.’
»MORE: Fertility preservation and cancer treatment
Checking into the hospital
They didn’t have a bed on the oncology floor at first, so they had to put me on another floor to get fluids and stuff. I got stuck about 6 times. They couldn’t find a vein. I was so bruised because I needed platelets.
It wasn’t until later that night that I moved to the oncology floor. The next morning, I had a bone marrow biopsy.
What was the bone marrow biopsy like?
A resident came in, and it was just me and my husband. They had me roll over. I got a local lidocaine shot. I was laying there on my stomach, and it was weird because the doctor was trying to make it casual while he’s drilling into my bone.
It definitely hurt, but I was so sick and tired that I remember not really caring. I was also pre-medicated for chemo, so I was out of it. I’ve had 4 more since, and those definitely hurt.
They didn’t really explain the process before they started. They just said, “We’re here for a bone marrow biopsy,” so I didn’t really know what to expect.
Bone marrow biopsy results
The results showed that about 97% of my bone marrow was affected. That’s how aggressive it was.
Chemotherapy Treatment
What was your chemo regimen?
The first week, I had chemo for 7 days straight. It was the hyper-CVAD regimen. One of the chemos was pumping 24/7. With leukemia, they just blast the induction chemo non-stop. You don’t get a break.
After the first week, I had a break. Because I had just had a week of chemo, they kept me to monitor me. After a couple days, they gave me more chemotherapy.
They waited for my counts to go back up. Then they’d hit me again, and my counts would drop again. Then, the last time my counts came back up, I got to go home.
During that first 3 weeks, I did what’s called an A round and then a B round. Then I was going to come back and do an A round and another B round.
It would be a week at a time, once a month. That was going to be my regimen until we were done.
You had intrathecal chemo
I was super nervous for that. I got platelets right before, during, and after the process. My oncologist was super sweet during the chemo. He held my hand and told me I was going to be okay because he knew I was really nervous.
Spinal tap side effects
If you’re going to have intrathecal chemo or a spinal tap, you have to lay flat for an hour after. I got a spinal headache for 24 hours after. It was really bad. I couldn’t sit up. I was pretty much on my back for 24 hours. That’s the only time I’ve ever had a bad headache that bad.
ALL can go to your brain. That’s why they do the spinal tap to check it and the intrathecal chemo. ALL is tricky, and it likes to hide and stay in your brain. I had 17 total intrathecals, but at this point I only had 2.
There was no cancer in my central nervous system when the results came back, so that was great news.
Chemotherapy side effects
Anxiety. I had a lot of that at night time especially. Physically, I was getting nauseous a few days after starting.
It stopped after a couple of days, though. My hair started to fall out 2 weeks after I started.
Describe your hair loss
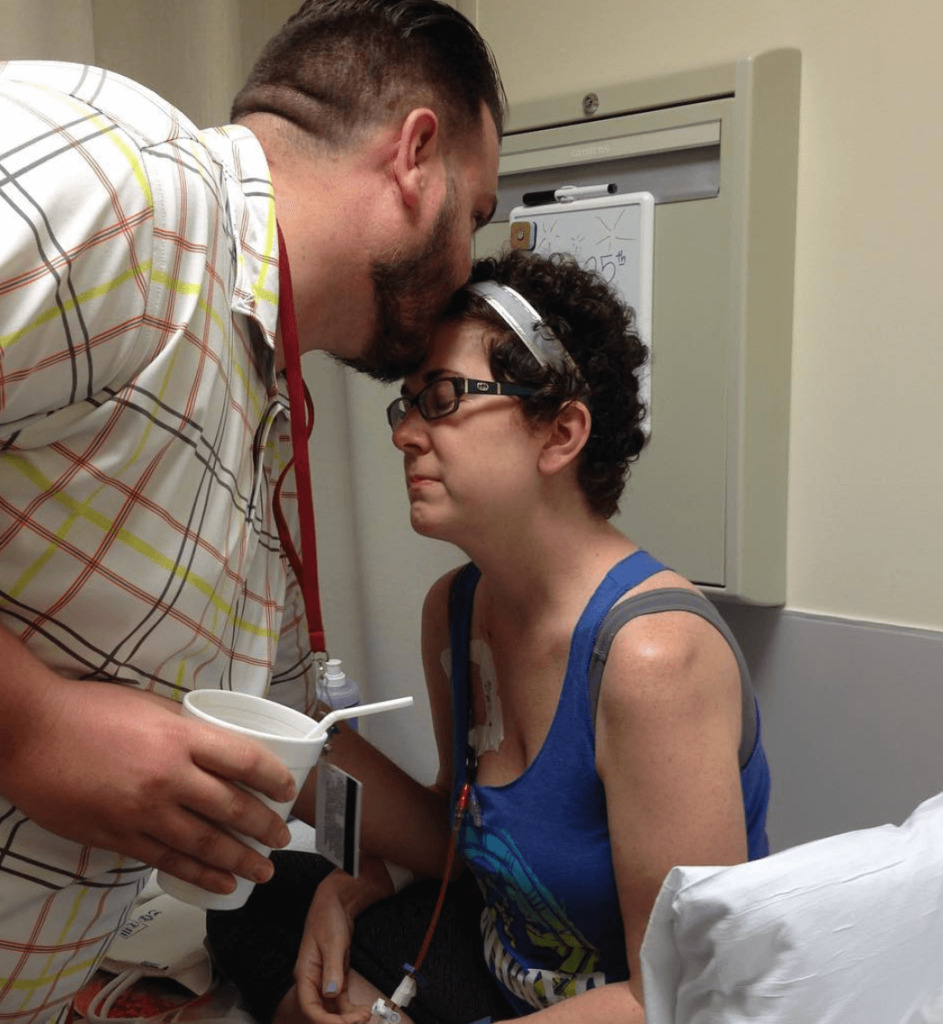
Two weeks in, my hairdresser came in and cut my hair really short. Then I had my husband shave it.
I was super tired. That was a big one. I was trying to walk around the floor. I would sit in the chair, but that was about it. I remember not being able to concentrate.
My appetite started going as well. Nothing sounded good. I was retaining fluid weight, though, and I was having to wear my husband’s clothes.
I was really positive about it, though. I didn’t have too many days during that first hospital stay that were awful, but I remember thinking I just wanted to go back to my normal life.
I stayed positive, though. My husband was with me, and that really helped.

How was the transition back home after the hospital?
After being in the hospital for 3 weeks, it was strange. I felt kind of nervous to be home away from the doctors. It was so weird. I left my house for a doctor’s appointment with hair, and then I didn’t come home for 3 weeks.
When I did come home, I didn’t have any hair, I could hardly move around, I didn’t have a job, and I was sick. I had no life all of a sudden. I was really tired and sore. I had really bad back issues to the point where I had morphine in a pain pump.
The hardest transition was not having anything to do. I went from being really active and having a career to not being able to really do anything because my counts were so low. I had to fill entire days with nothing.
The other thing was they put me in forced menopause. I had so many hot flashes. I couldn’t stop sweating. I was bored and sweating all the time.
»MORE: Mental and emotional support when leaving the hospital
How were you feeling knowing that the chemo was working?
They blasted me really hard at the beginning. I had another bone marrow biopsy after the first 3 weeks of chemo. They didn’t know if it was really there or not because the cancer cells can hide, but they did determine I had no evidence of disease after those 3 weeks.
I was excited and relieved, but I also knew I had a long way to go. I still didn’t really get how hard it was going to be to do more of the maintenance chemo, but I knew we were heading in the right direction.
At this point, my oncologist was still saying I may or may not need a transplant, but I think he knew I would need one.
What happened after you had no evidence of disease (NED)?
I still had to finish my protocol. From October to April, I was admitted to the hospital for 6 to 9 days each month for chemo. If it was an A round, I would usually be in for 6 or 7 days.
If it was a B round, it was more like 8 or 9. I spent almost 10 weeks in the hospital throughout those months because of chemo, fevers, and infections.

In December, I did a PET scan after 4 rounds, and nothing showed up. I had another scan after the full 8 rounds, and it was clear, too. They waited a month after I finished my protocol in April to do another bone marrow biopsy.
We found out the results 3 weeks later in June. They officially told me that there was no more leukemia to be found whatsoever. I went to my D.C. oncologist after that, and there were talks about doing the bone marrow transplant.
The transplant was the safest way to try and avoid a relapse. My sister was a perfect match, so we started taking steps towards the transplant.
I was feeling so much better. I didn’t even know why I needed a transplant anymore because I was starting to get back into a normal routine. I really didn’t want to even do it.
Insurance was holding up the process as well. There were so many roadblocks, but we finally picked a date. At this point, it was late July, and we set a date for the transplant finally in September.
Overcoming a Relapse & Complications
Relapse before the transplant
While waiting to schedule my transplant, I was having some pain in my arm and shoulder. I couldn’t really lift my arm without it hurting pretty bad.
I went to see my oncologist. He wasn’t too concerned about it, but he wanted to do an X-ray just in case.
When they did the scan, they saw fluid around my lung. My oncologist asked about a cough and how long I had had it. I told him I had been coughing for about 2 weeks. He decided to drain the fluid.
He called 2 days later and told me my leukemia was back.
Right when they scheduled the transplant, we found out we couldn’t do it. I was supposed to check in the next week for more chemo, but I got too sick and had to go to the ER.
At that point, my white blood cell count was like 470,000. I was so sick. It was a really bad relapse, and it progressed really quickly.
This was a rare situation
My doctor with more than 20 years of experience had never seen a blood count that high. I was admitted to the ICU right away. We had to do dialysis because they were scared that the chemo would blast my kidneys.
Relapse Treatment Plan
What was the treatment plan this time?
They started another 3 weeks of induction. They did the same chemo, but they added a drug called nelarabine. It’s common, but it wasn’t in my first protocol. We did 2 rounds of that, one in September and one in October.
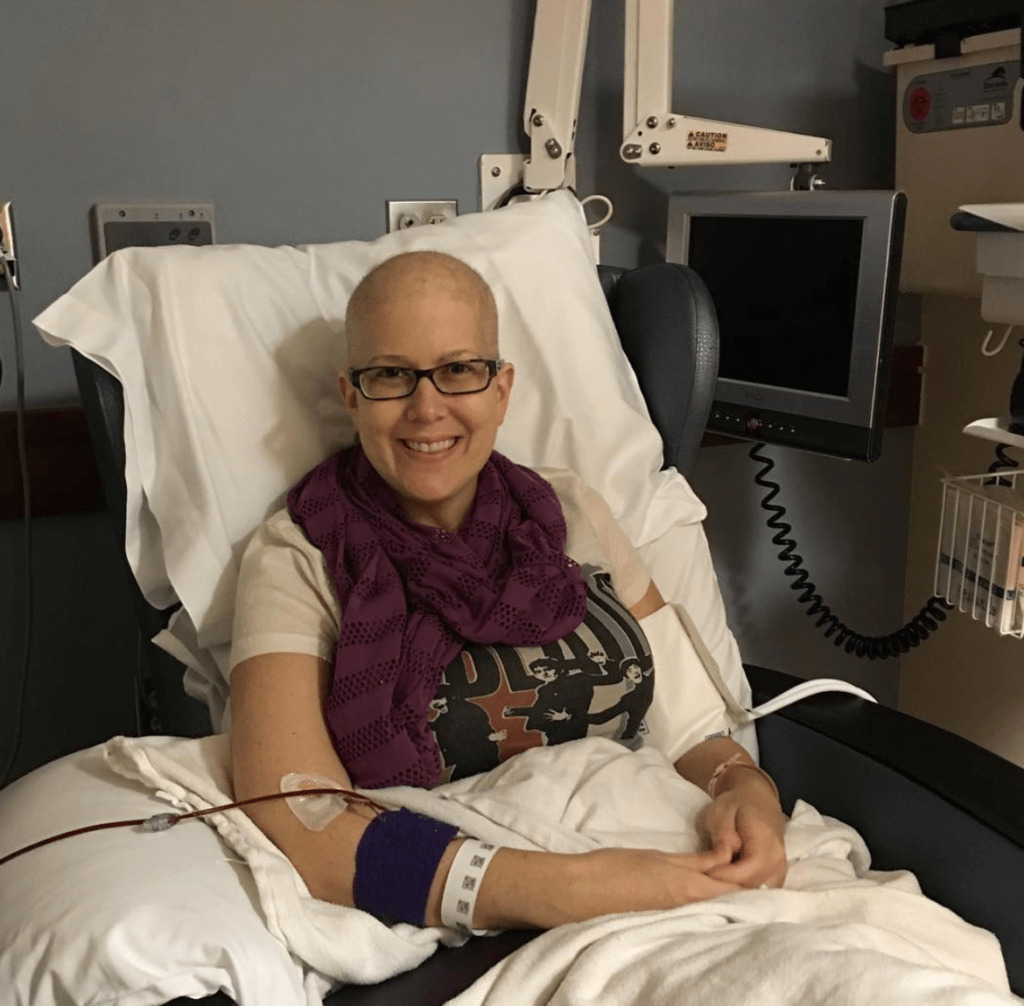
I was really surprised at how much better I felt compared to how I felt the first time around. I don’t think the nelarabine gave me side effects all that much. I didn’t even lose my hair right away. It was a different feel to the whole thing.
The relapse was harder emotionally, but I think physically I actually felt better on chemo just because I was so sick.
Instead of going through 8 rounds, my oncologist’s plan was to get into remission and do a transplant immediately.
I was supposed to do 2 rounds of chemo and have a bone marrow transplant near the end of October, but my counts weren’t coming up fast enough.
Processing the relapse
Relapse was hard because of the thought of having to do everything over again. I didn’t know if I could do it again.
By round 6, 7, and 8 the first time around, I was so tired. Every round was getting harder and harder to recover from.
After getting a taste of real life again, it was hard to comprehend that I was going to have to do it all over again.
Then I sucked it up and did it because I didn’t have any other choice. I felt a lot more up and down emotionally the second time around.

Complications
I found lymph nodes behind my left ear one night after doing my week in the hospital for chemo. They were all raised.
I called my nurse practitioner, and she said she could already tell me I should probably bring a bag because the oncologist was going to want to admit me.
We decided to go up there the next morning, but around 10 p.m. that night, we were watching TV, and I was like, “Ah, my face feels funny.”
It was fine, and then it wasn’t. The whole left side of my face was paralyzed. My husband looked at me and jumped up because he thought I was having a stroke or something, but then it went away.
I called my mom. She said it was really weird, but since we were already going, it was probably fine to wait. I woke up in the middle of the night, though, and I could feel my face paralyzed again. I couldn’t move it. I went back to bed. It didn’t go away, so we called my doctor, and we went in.
No standard procedure of care
They were worried that it had gone to my central nervous system. They did intrathecal chemo and a spinal tap right away, and that came back clear. They took out my lymph nodes right there behind my ear while I was lying in my hospital bed.
That was the hardest conversation we had with the oncologist because he said I wasn’t following any plan or normal disease course he had ever seen before.
He said he would figure it out, but we had to abandon what we were doing because my cancer was showing up for the third time.
They wanted to give me pegaspargase. It’s generally used for children, and no one had actually ever had it at George Washington Hospital before.
It has great success rates, but it comes with a lot of side effects. The nurse was reading the paperwork to me because no one had ever had it there before.
I did that in October and November. My face was still drooped, and I was almost more concerned about that than the cancer. November is when I lost my hair again.
On November 29th, I had a fever of about 101. It was really late at night, and I cried. I did not want to go to the hospital.
Pegaspargase side effects
My mom came over and dragged me out of bed. I could barely get dressed. I could barely walk to the car. We pulled up to a local ER, and they wheeled me in. I felt so sick.
I asked if there was a bathroom in my room, and I went into my bathroom.
Then I don’t remember anything for about 12 days. I was going in and out of coherent thought. I wound up going in septic shock.
There are texts from that time, and they’re coherent, but I really don’t remember any of it. The doctors there told me I needed to go back to George Washington because they didn’t have the resources to treat me. They never did any cancer tests, but they just assumed it was a cancer reaction and that I had cancer everywhere.
They put me in an ambulance and transferred me over to D.C. I got admitted back into my home cancer floor. To this day, medically, they don’t know what happened. I was in ICU for a few days because I was in a coma essentially for more than a week.
The ICU doctor told my family that they weren’t going to do any scans or anything because it was just going to tell them my prognosis, not my diagnosis. My oncologist didn’t have a say in my care at that point since I was in the ICU. He could only recommend, but he was pushing for the scan.
He knew I was a fighter, and he wanted to figure out what was going on.
Then 2 or 3 days later, they did an MRI. It came back completely clear. There was no cancer, so they were just waiting to see how I was going to do.
Eventually, I started to wake up and talk. I don’t remember any of this either, but I slowly became coherent.
On top of waking up and not knowing what was going on, I also couldn’t move anything. I was paralyzed. My doctor essentially said, “I hope you don’t have cancer because we can’t do anything about it since your body can’t take anything.”

Bone Marrow Transplant
Recovery before the bone marrow transplant
Luckily, there wasn’t any cancer, but I had to go to acute rehab. I was admitted to the rehab a floor down on December 22nd. I’m usually a positive person, but that was not a good time for me at all. I left the rehab January 19th.
I went home in a wheelchair because I still wasn’t walking. I was considered homebound for 2 months. I had physical therapy at home until April. I learned to walk again with a walker at the end of March. By April, I was walking well enough to go to PT outside of my house. I was in physical therapy in total for 14 months.
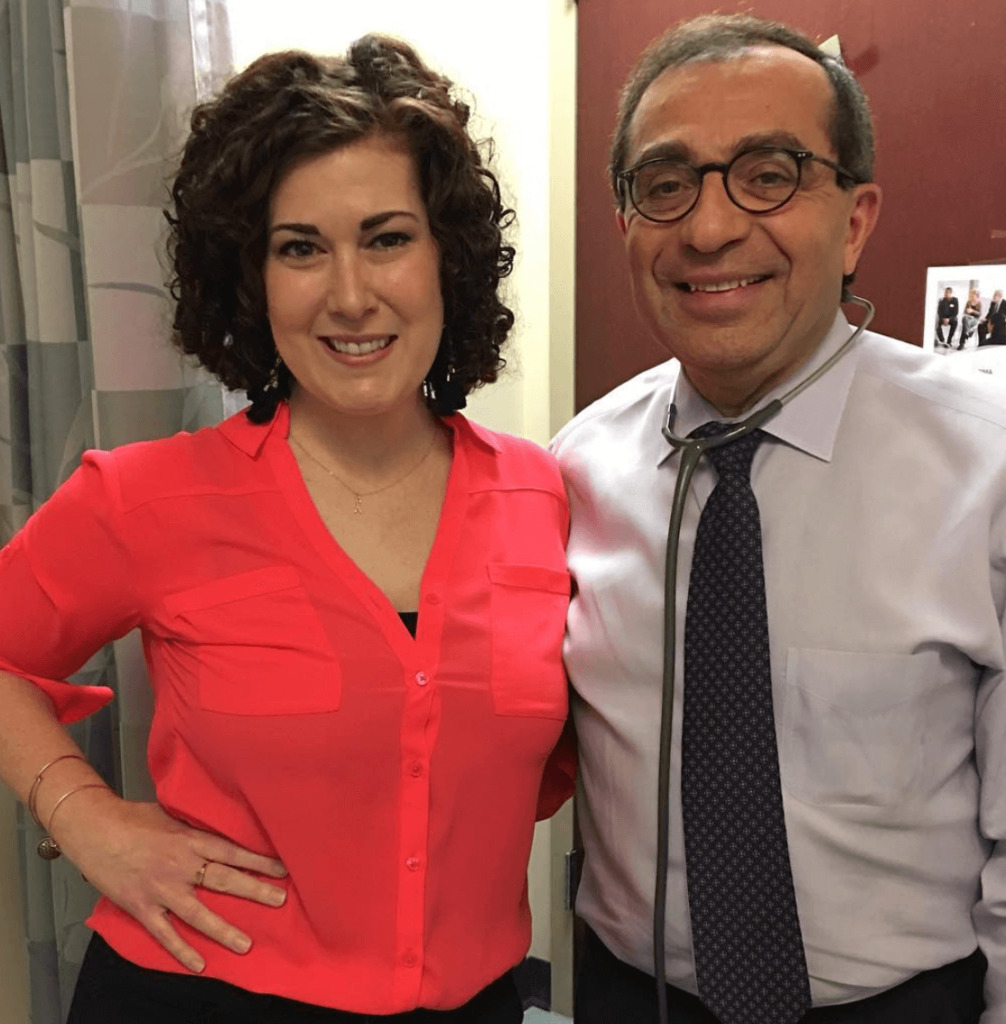
I’m still not physically where I was before everything, but I’ve made progress. After therapy, my doctor sent me to Johns Hopkins for the transplant because they have a whole program for transplants. From April to July was recovery, and then it was finally time for the transplant.
What happened with the bone marrow transplant?
I had 7 days of chemo before the transplant. I had a day of radiation, and then I had my transplant. It was outpatient, which was the first time I’d ever had outpatient treatment, so that was cool.
Johns Hopkins is so big that they have an entire floor of leukemia patients. They have a section called IPOP, or Inpatient/Outpatient. You go in for treatment, and you go back to your little apartment on the hospital grounds.
You never have to leave the hospital, but you get to stay in a little apartment. That helped me mentally so much. I felt like I could move around more, and it was nice to not be hooked up and monitored constantly.
It was harder than I thought it was going to be because of the fatigue, but the transplant itself was pretty uneventful. It looks like a blood transfusion.
It was a really hard recovery just because I don’t think I’ve ever been that tired before. I couldn’t pick up a spoon because I was so tired. I was not expecting that to be so exhausting, but around 3 weeks, my counts picked up a little. At that point, I was starting to feel a little better. On day 58, I got to go back home.
»MORE: Learn more about bone marrow transplants from a specialist
Reflections
How has your cancer experience changed your perspective?
It all sounds cliche, but I live every day to the fullest and appreciate every day. It sounds silly, but it’s true. I don’t really sweat the small stuff as much.
If I come across a new experience or something that’s hard, I think, “I don’t have cancer. It’s not gonna put me in the hospital,” and I feel better. Things aren’t as big of a deal.
The negative side of that is sometimes I get annoyed with people. When people get upset about small things, I’m like, “Wow, it’s really not a big deal. Just be happy and grateful.” I find that I sometimes have little patience when people are dealing with stuff.
I have to remember that their problems are important to them, but I wish everyone could appreciate life and how short it can be. I wish people knew not to worry about things.
I use my time more wisely than I did before. I have a unique experience and perspective on things, so I use that more than I did before. If I can use what I went through to help someone else, that’s great.
I wasn’t really an outgoing person before, and I feel like I’m way more outgoing and talkative now.
I share more personal things than I did before. I realized how little I knew about leukemia and cancer in general, and after connecting with people, I’ve been able to meet a lot of people.
Nobody really talks about it, so I decided to be open about my stuff. You can make so many connections with people by being vulnerable and real.
I’ve just realized that life is too short to be closed off.

What helped you through your lowest moments?
A lot of prayer. I’m from a Christian family, and we just used that and relied on that. I would love to say I prayed a lot, but I knew a lot of people were praying for me. I couldn’t function long enough to pray a lot, but I tried to sit there and pray. Having so many people around the country praying for me made me feel like I could rest.
I allowed myself to have a bad day. I would ask people to pray for specific things. I would go to bed, face the next day, and knew that other people were supporting me.
I zoned out a lot, I colored a lot, and I did mindless activities to turn my brain off.
Fertility after cancer
As of now, I’m medically in post-menopause. The transplant sealed the deal. There’s no fertility happening here, but they don’t want to tell me I’m infertile.
They told me that I’m in post-menopause, but my body is weird and there’s a chance it could come back. Since my infertility was from forced menopause, they’re never saying never.
There’s a small chance that my body could kick back into gear, but overall, the options are a donor egg or adoption.
I won’t be producing any eggs anymore. We could adopt, but we haven’t talked about that much. All of that is so expensive, and I’m still tired, so we haven’t made any decisions.
»MORE: Fertility preservation and cancer treatment
Paying for cancer treatment (financial toxicity)
My husband has really amazing insurance. I already had all my insurance through his job. That wasn’t a disruption. The transplant alone was like $800,000. Insurance covered a lot for us, but of course bills are expensive.
I was able to apply for disability because acute leukemia is one of those conditions with compassionate allowances within social security, so I started getting money from that in month 4 or 5.
They back paid me for the first few months, too. I’ve been on that since I got sick, and I recently got off of it.
Someone started a GoFundMe for us. When I was still working, people donated hours to me, so I was getting PTO some. I think it’s harder now because we’re playing catch up.
We’re still paying medical bills, but it could’ve been so much worse. If people don’t have the help that we had, it can be so expensive.
How has cancer impacted your work?
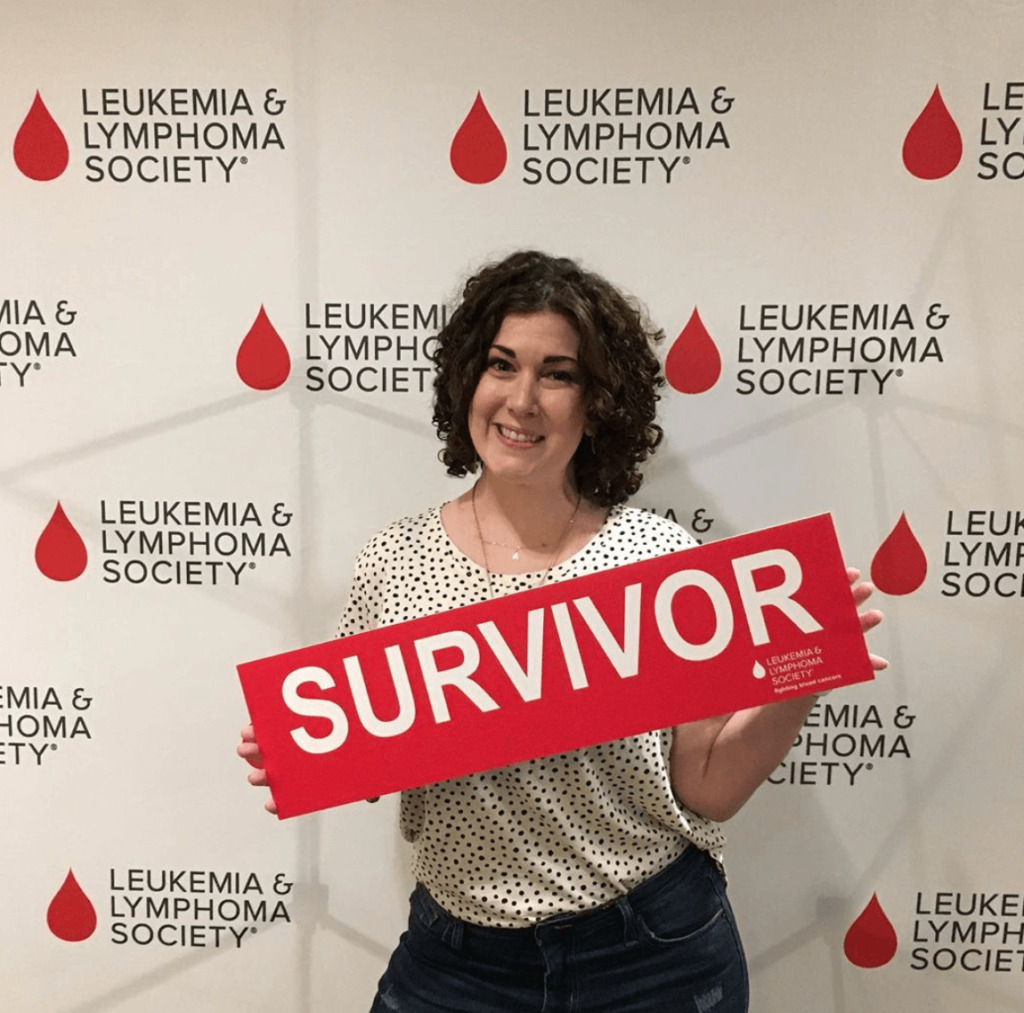
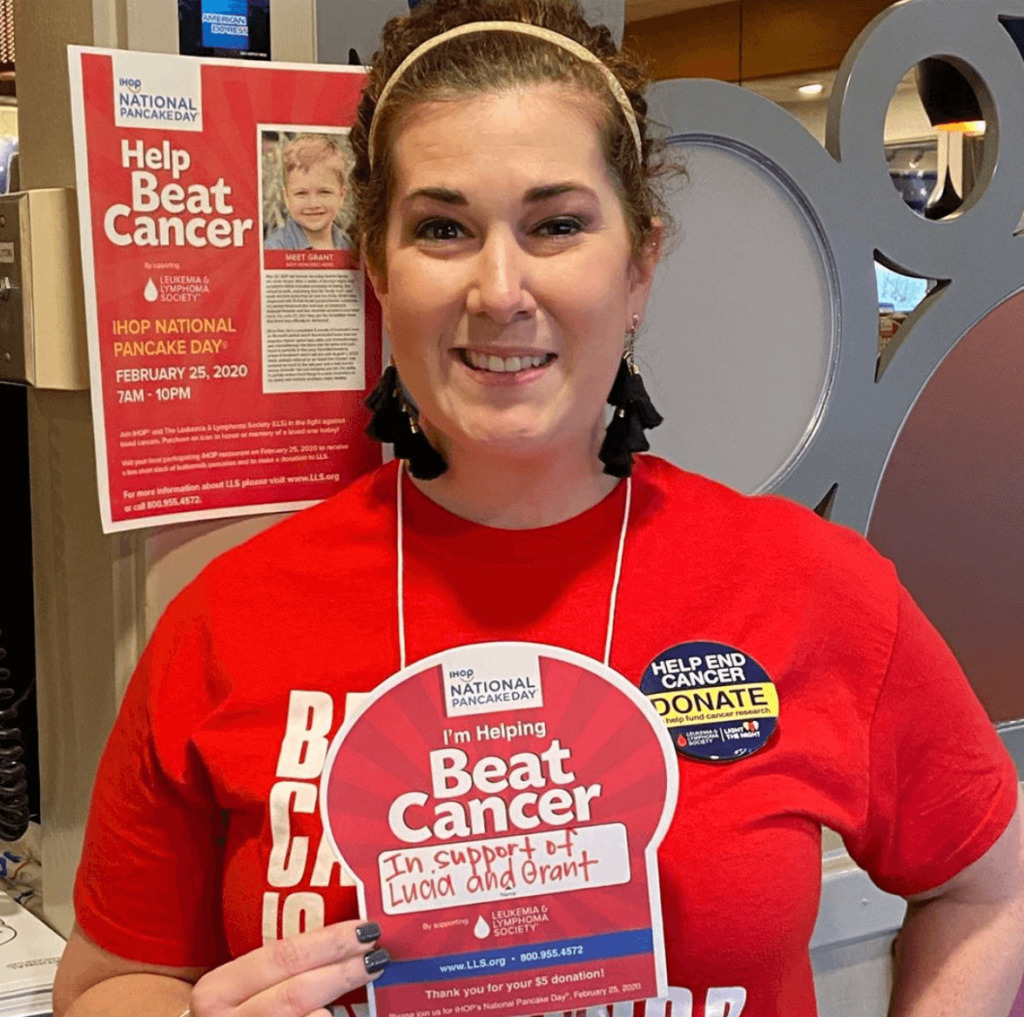
I ran for Woman of the Year, and I raised $84,000 for the Leukemia and Lymphoma Society. I started to meet people who worked there.
There was a position open, and it was a job I was able to do from home for 30 hours a week. It was a good entry opportunity back into real life, so I’m actually working for LLS now.
»MORE: Read more on how others dealt with work after a cancer diagnosis

How did cancer affect the relationship with your husband?
I would say we’re lucky that we went into this whole experience completely together and came out completely together. I feel like we’re stronger than we were 4 years ago. It never really affected us too much.
The hardest thing was when I was paralyzed. I felt like he was more my caregiver than my husband. He had to pick me up and put me in bed. He had to shower me. That was the weirdest part of everything, but he never acted any different. I didn’t look cute, but he never looked at me different.
Our relationship shifted a lot during the whole thing, and it took us a few months after my transplant for us to really get our groove back.
We got back to an adult husband and wife relationship, and now this year, we almost feel like we’re dating again.
We’ve reconnected and feel like we can go out and do things. We don’t talk about cancer every other conversation. We don’t have to update our families all the time. Life is getting back to normal. That’s been nice.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
Advice for someone who has just been diagnosed
Be patient with yourself. Don’t be so hard on yourself. It took me a long time to feel like my job was to just get better.
Be patient with the process. Be patient with family members who don’t know what to say.

It’s such a slow process, but there’s a rhyme and reason to everything. Let it happen. Don’t rush it. Try to remember it’s affecting you and everyone around you. Everyone might need some time to adjust.
One big thing is remembering that it’s okay to say no. Do not be a people-pleaser during this time of your life.
If someone wants to come visit and you don’t feel up for it, say no. Your job is to get better. Don’t feel like you have to say yes. Stand up for yourself if you’re not comfortable with something. Be true to yourself and take care of yourself.
Inspired by Christine's story?
Share your story, too!
Acute Lymphoblastic Leukemia (ALL) Stories
Lauren M., T-Cell Acute Lymphoblastic Leukemia (T-ALL)
Symptoms: High fever, trouble breathing while lying flat, bad cough, headaches
Treatments: Chemotherapy, radiation, lumbar puncture
Christine M., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Enlarged lymph nodes, pain in abdomen, nausea
Treatments: Chemotherapy, bone marrow transplant
Lauren J., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Extreme fatigue, easily bruised
Treatments: Chemo pills, chemotherapy, spinal taps, total body radiation, bone marrow transplant
Renata R., B-Cell Acute Lymphoblastic Leukemia, Philadelphia chromosome-positive (Ph+ALL)
Symptoms: Fatigue, shortness of breath, nausea, fevers, night sweats
Treatments: Immunotherapy, chemotherapy, TKI, stem cell transplant (tentative)



