Drea Finds Identity and Strength with Stage 4 ROS1+ Lung Cancer
Drea is a video journalist who was only 26 when she was diagnosed with stage 4 ROS1+ lung cancer. It came as quite a shock. She never imagined that a physically active, young non-smoker who had never had any health issues, could ever get cancer.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez
Drea’s story began in early 2023. She began to experience some strange symptoms, including a swollen ankle from an unexplained deep vein thrombosis or blood clot, odd bruising, extreme weight loss, and persistent shortness of breath. She went to the ER several times, had some urgent care visits, and also saw specialists, but was reassured that what she was experiencing was due to stress or other such causes. She started to doubt herself even as her health began to deteriorate. Eventually, she succeeded in having a CT scan done. It revealed a large mass in her lung. Further tests confirmed that she had stage 4 non-small cell lung cancer that had already spread to multiple locations.

Drea’s experience has convinced her that self-advocacy is key. She explains why we always need to trust our instincts. “If you feel deep inside that something’s wrong, keep pushing,” she advises. Because she was persistent, she eventually had comprehensive biomarker testing, which identified the ROS1 mutation. This discovery opened the door to life-extending targeted therapies.
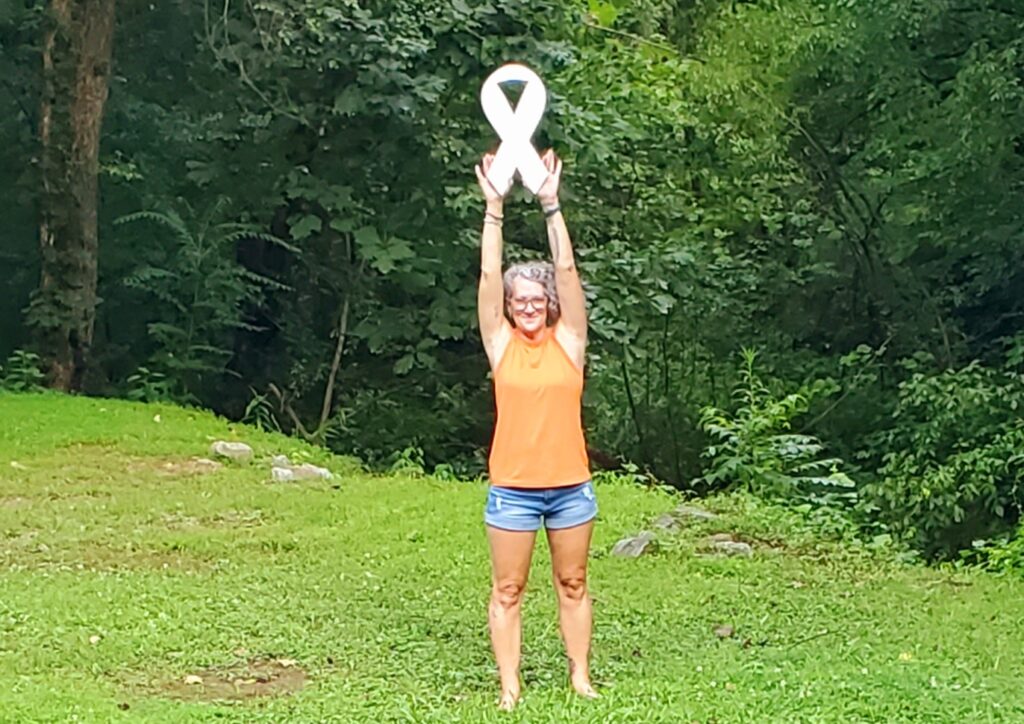
Living with stage 4 ROS1+ lung cancer has helped Drea redefine survivorship. It’s not just about existing; it’s about living fully. The targeted therapies she’s having allow her to enjoy climbing, biking, beach days, and gardening. She’s open and frank about her ups and downs, and acknowledges the chaos and struggle of having to navigate cancer in her 20s. But she’s decided to treat each day as an opportunity by focusing on what she can control rather than agonizing over the “what-ifs.”
Cancer didn’t strip Drea of her identity. Instead, it’s added new layers. She’s not just a video journalist anymore; she’s also an advocate, connector, and source of hope for others. She shares her story openly to help more people realize that “anyone with lungs can get lung cancer,” and, by doing so, to break the stigma that lung cancer is a smoker’s disease.
Drea urges others to be their own best advocate, seek second opinions, push for biomarker testing, link up with patient groups for support, and, most importantly, give themselves grace. Watch her video for more on:
- Her diagnosis at such a young age and how she became her own health advocate against all odds
- Drea’s struggle to be heard before her stage 4 ROS1+ lung cancer diagnosis
- How targeted therapies gave her her life back
- Why Drea names her cancer ‘Carl’, and how humor helps her thrive
- The advice she offers young people who don’t feel heard by doctors
Scroll down for the transcript of Drea’s video interview!
- Name: Drea C.
- Age at Diagnosis:
- 26
- Diagnosis:
- Non-Small Cell Lung Cancer
- Stage:
- Stage 4
- Mutation:
- ROS1
- Symptoms:
- Swollen ankle resulting from a deep vein thrombosis or blood clot
- Mysterious bruising
- Extreme weight loss
- Persistent shortness of breath
- Rattling sound coming from the throat while breathing
- Treatments:
- Radiation therapy
- Chemotherapy
- Targeted therapies
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
I’m Drea
My name is Drea. I was diagnosed with stage 4 non-small cell lung cancer at 26.
When I first felt something was wrong
I first started feeling off at the beginning of 2023. It began with the DVT, which is a blood clot that resulted in a swollen ankle, and at the time, it didn’t make sense to me because there were no known injuries; I hadn’t fallen, I didn’t trip or anything. I had gone to urgent care, which then sent me to the ER, and then they discovered that it was for sure a blood clot, so they put me on thinners. Following that, I kept having these sorts of mysterious symptoms, among them just bruising up and down my body, and extreme weight loss. It felt like I was in a pit of despair. I felt like there was something off, and I don’t know how to describe that feeling. And I think throughout the process of 4 or 5 months, the symptom that started scaring me the most was the shortness of breath. I think by the time they came around, I had this really weird, awful, rattling sound coming from my throat. Google scared me when I googled that one up. The entire five months of these symptoms, I had gone to urgent care a couple of times, I had gone to the ER, I had seen a specialist, and I kept getting sort of brushed off, getting told, “You’re young, you’re probably just needing a little more rest, you’re probably just tired or stressed.” Cancer or any sort of serious disease was never really mentioned. But then I remember in May, going back to that same urgent care that months earlier had prescribed me an inhaler for the shortness of breath, that same urgent care doctor had finally ordered a CT scan.
He gave me a call, and there was a sort of newfound sense of urgency in his voice. He told me I needed to go to the E.R. immediately. There was a mass that was found in the scan, and it did not look good. So I just drove myself over across the street and got admitted to the E.R. That was my first hospital visit that resulted in, I think it was like a 7 or 8 day stay.
They ran a swath of tests. My blood counts came back, not looking great, but nothing to signal cancer. But it was the imaging that scared doctors the most. They had found this huge lemon-sized mass on my right upper lobe, and sort of nodules scattered across it. They ended up doing a PET scan, and that’s when they found that there was also cancer up and down my spine and pelvis, and not even my noggin was spared, unfortunately. So they knew right away that this was serious and that it was likely cancer. And so I think it was maybe on day 4 or 5 of that hospital stay that they got me in for a bronchoscopy, and then I got the news.
The moment everything changed
Getting told that I had lung cancer at 26, as a never-smoker, never picked up a cigarette, or none of that, was shocking. I did not understand how that could even be possible. I never knew that non-smokers got lung cancer. My dad died of lung cancer in his 40s. He was a very heavy smoker, so I doubt he had any sort of mutations. But because of his lung cancer death, I had made the choice early on that I would never pick up a cigarette. I wouldn’t vape because I saw what it did to others. But then to find out that that didn’t save me from lung cancer was a shock.
Ten out of ten, I would not recommend getting your cancer diagnosis in the E.R. It is awful. So take that with you wherever you go. Try to establish care with the primary care physician who knows you and your history, because getting my diagnosis in the E.R. was not pleasant, to say the least. I think I was there anywhere between 5 and 7 days. It was complicated because after I got that diagnosis, I got discharged. I got sent home with no oxygen for some weird reason. Here’s a metastatic lung cancer patient who has cancer across both lungs, up and down the spine, in her noggin, and she still got sent home with no oxygen. And I just didn’t have anyone to check up on me in the way that I would imagine others would have if they didn’t get their diagnosis in the E.R.. It wasn’t until my at-home nurse noticed that my breathing was getting progressively worse, and she told me to head back to the E.R., that they found that my situation was getting even worse. And so the second time I got admitted, I had to get an emergency blood transfusion and start traditional chemo right away, the very next day, and that was the day that my oncologist told me, This doesn’t work.
We might have to put you in hospice. Because at this point, we had not gotten the biomarker testing results back. And so that was when things finally hit me that this was serious, that I don’t have my youth, I don’t have my young age to rely on, and that something needs to happen. And so I remember lying in bed with my mom by my side at this point, just panicking internally. And that was when I decided to just start calling around to see if there was a comprehensive cancer center that would take me right away, because I did not want to be put in hospice.
I took my health into my own hands
Hearing the word hospice just rattled me to my core. I knew that I had to do something to get myself from getting buried six feet under, and so I started crawling around trying to see what the next best option was. What is an option that is more familiar with these rare types of lung cancers? At the time, I didn’t know that I had ROS1 because we were still waiting on biomarker testing. But the oncologist at the time said that it was very likely, given the fact that I never smoked and I’m so young. I started calling around to this one major comprehensive cancer center in Florida. It was right after that conversation with the oncologist, and I think the call rep could hear the shakiness in my voice because I was trying to talk through tears, just trying to see if there was any sort of openings in the immediate couple of weeks. After all, things were serious, and as soon as I was discharged, I needed to seek care elsewhere to see what other options I had. Luckily, the lady found me in an appointment, and I was able to get in on time. I think it was two weeks later, and that’s how I ended up at my second hospital.
Learning my biomarker
I was actually very lucky that my oncologist at the time knew that there was a specific subtype of lung cancers that tend to impact younger nonsmokers. And he happened to be working that day and saw my case, and he ordered comprehensive biomarker testing right away. I think I got the results after just a couple of weeks. I consider myself very lucky because if it weren’t for biomarker testing, I don’t think I’d be here today.
It allowed me to take targeted therapies, which have been shown to work well with my specific type of cancer. Targeted therapies in general have truly revolutionized what it means to be metastatic and living with lung cancer. And it’s just unfortunate that there are people across this country, across the globe, who are not afforded that option because they’re doctors, or the hospital care system just may not be aware that comprehensive biomarker testing is a thing.
I was kind of all over the place, still trying to process the news. But when my oncologist at the time mentioned that comprehensive biomarker testing could open the window to newer forms of treatments, I was like, all right, let’s do it. And then when I finally got the news and I saw that I had ROS1, which tends to impact, I think it’s like 2 to 3% of all non-small cell lung cancer cases, I was like, great, so here’s to celebrating having a mutation, I guess, let’s do it. It was an interesting, interesting time. A couple of weeks later, my brother was doing some research on my behalf, and he found this incredible nonprofit advocacy group that does a lot to build community and share resources for people with ROS1. They’re called the Ross Wonders, and they have just been a godsend to me. They showed me how to be a better advocate for myself, they’ve connected me with those long-term cancer survivors, and they’ve shown me that you can still live a long and fulfilling life, although you have metastatic lung cancer.
My treatment plan
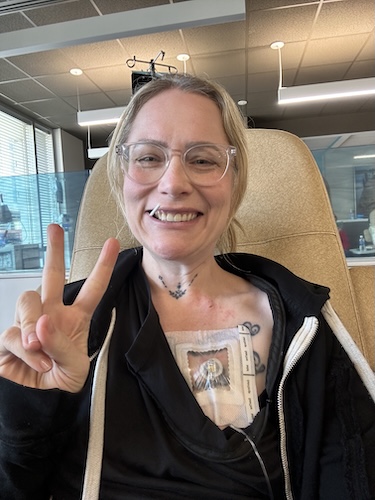
As soon as we found out that I had ROS1, it became very apparent that we had a better option than that platinum-based chemo that I had already gotten one round of. At the time, I had also gotten radiation. But there has been such incredible research out there about these targeted therapies that the best course of action at that time was to just stop chemo and go on a TKI pill, and so I was put on my first drug.
I got about three years of pretty great response, pretty great quality of life on what I like to call my beloved drug, and it was very good to me; it kept my cancer under control, and I was able to wrangle my control. And I was able to wrangle my life back from cancer in a way that I never envisioned, because I knew nothing about targeted therapies and what sort of quality of life that might have meant. It was great for me for about three years. Unfortunately, earlier this year, I had to switch to another drug, but thankfully, things have been going pretty well on this second TKI as well.
It’s gotten a pretty good control on some of the new lesions that have popped up, and I’m still able to live a relatively normal life. I have a couple of annoying symptoms, but they’re still manageable.
Everyone’s different. Everyone’s going to react differently to each drug. We may have the same cancer with the same lesions and other comorbidities, but we may still react differently to whatever drug we’re taking. I consider myself pretty blessed because I seem to be a fairly good responder to TKIs. I don’t deal with any sort of debilitating symptoms. I know that that’s not the case for a lot of other ROS1ers; unfortunately, I wish it were. But so far, everything that’s been thrown at me has been manageable. I’ve been able to get back to my old life. I climb a lot, I bike, I’m able to take my dog on long walks, I’m able to be out in the sun and garden, I’m a very big beach bum, true Floridian. And I have TKIs to thank for that.
How I feel about clinical trials
I will say a lot of people tend to fear the idea of clinical trials because they like to think, “I don’t want to be a lab rat, I don’t know what sort of outcomes I’m going to see if I join a clinical trial studying a very new drug.”
Editor’s Note: In cancer trials, no one is given only a sugar pill when an effective standard treatment exists. Instead, participants receive either the current standard-of-care treatment or the standard-of-care plus a new therapy being studied, and everyone is closely monitored for safety and benefit. Many of the oncologists we interview describe cancer clinical trials as "getting tomorrow's medicine today."
There are a lot of incredible treatments out there that are revolutionizing what it means to live with these sorts of subtypes of lung cancer, whether it’s ALK, EGFR, or ROS1, like what I have. These therapies are exciting; they’ve shown a lot of great promise. A lot of times, these drugs are being tested for years in a clinical trial setting, and there is early data that you can glean from and decide if that’s a good option for you at the time. If I’m ever at a point where I do run out of TKIs, I will gladly volunteer for science and to help the next lung cancer patient get access to even better drugs in the future.
How I’m navigating my diagnosis and being young
Navigating cancer in your 20s and 30s is incredibly messy; it is chaotic. It is a roller coaster you go through, so many loops, it’s complicated.
I’m not going to deny that, it’s not an easy feat. I’m metastatic, which has caused me to grow up in a lot of different ways. For people who have been diagnosed at earlier stages, it is life-changing. Just because treatment wraps up and your hair grows back and you’re in remission or you’re cured, does not mean that your life goes back to normal or that you’re even the same person you were the day that you were diagnosed. So it is complicated, and I try to remind every cancer patient that I meet to just give themselves grace. It is a work in progress. I am three years out, three years into survivorship, and I am still learning what it means to live with metastatic cancer, and to live each day as if I’m living, not as if I’m dying.
Honestly, I try to just make the most out of whatever time I have left. If it is three months, if it is three years, if it is six years. Let’s pray for six years, I will take six years happily. I like to treat every day like a new day.
And if I’m having a crappy day or just the type of day where you just don’t want to get out of bed and you’re just stuck doom scrolling on your phone, I try to remind myself that tomorrow is a new day.
I used to just get stuck on all the what-ifs. Like, what if I spoke up sooner? What if I pushed for answers sooner? Would my life have been different? Would my cancer have been when it was stage 2 or 3 instead of stage 4? But at the end of the day, what does that do for you? What are you thinking about, the crappy cards that you were dealt day after day? What does that do for you? And so I try to just remind myself to focus on the things that I can control. And that is what my life moving forward is going to look like. Whether that’s for three months, three years, or however long, I know that I just want to make the most of each and every day.
“Hope” is a complicated word for me
I am cautiously optimistic that I will be able to get a good chunk of time out of whatever TKI lines are currently available. And I hope that I will be able to respond well to those therapies until the next best thing comes out.
And there are a lot of really new and exciting TKI drugs currently being studied in clinical trial settings. I try to talk to my cancer from time to time and just be like, “Oh, Carl, can you give me three years of peace, until that next best thing comes out?” I know that next year there’s going to be another TKI out in the market, or at least that’s what my oncologist has said, and what we hope is that it’s going to get approved by the FDA. I try to count my blessings every day and try to beg Carl from time to time to just behave for a little longer, and just go from there.
I like to view my cancer as an insidious roommate that just does not pay rent, that has been uninvited. What is the most awful name you could give that imaginary roommate? And the first name that came to mind is Carl, so his name is Carl.
Carl used to be lemon-sized, around five centimeters. I think he’s down to two centimeters, and he’s been stable.
He’s been behaving this way this whole time. It’s just that I get random lesions outside of the primary tumor that pop up, but for the most part, he’s been good.
What I want others to know
My last piece of advice would just be not to take a lot of stock in survival statistics or prognosis. My first oncologist told me I likely had just three months to live; lo and behold, I’m still here. Three years later, and I’m still going strong, I’m still kicking.
And I hear it all the time in the lung cancer community, fellow patients who have been given months to live, a year to live, and they’re still doing well. And while that may not be true for everyone, there is reason to remain cautiously optimistic because newer therapies are coming out every couple of years, and science is advancing in a lot of incredible ways.
I want people to know that anyone with lungs can get lung cancer. You do not have to be smoking eight packs of cigarettes a day to get lung cancer. I was 26 when I was diagnosed, and I have not once picked up a cigarette or a vape or any of that stuff, but I still got diagnosed with stage four non-small cell lung cancer. It is something that is happening to more and more young people, year after year, and we don’t know why. It’s terrifying.
If you’re feeling out of breath, if you’re seeing a lot of troubling symptoms that don’t make sense, whether it’s back pain and then this weird rattling sound coming from your throat, and you’re getting told by your doctors you’re fine, it’s probably pneumonia or asthma, here’s an inhaler, don’t listen to them. Seek better care and keep pushing for answers, because lung cancer cases amongst nonsmokers are going up. And at the end of the day, you’re going to be your own best advocate.

Inspired by Drea's story?
Share your story, too!
More Non-Small Cell Lung Cancer Stories
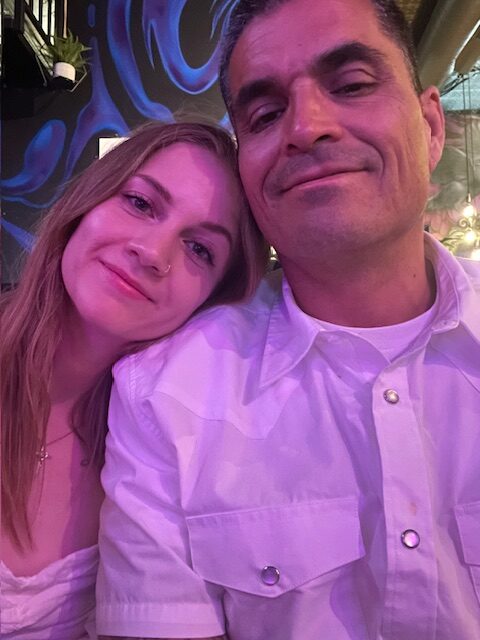
Lindsay W., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptom: Severe pain in her side
Treatments: Chemotherapy (targeted therapy), radiation
Leah P., Non-Small Cell Lung Cancer, EGFR 19del, Stage 4 (Metastatic)
Symptoms: Persistent dry cough, shortness of breath, heaviness in the chest, coughing up blood, weight loss, right rib pain, right shoulder pain
Treatments: Targeted therapy, chemotherapy, radiation (SBRT)
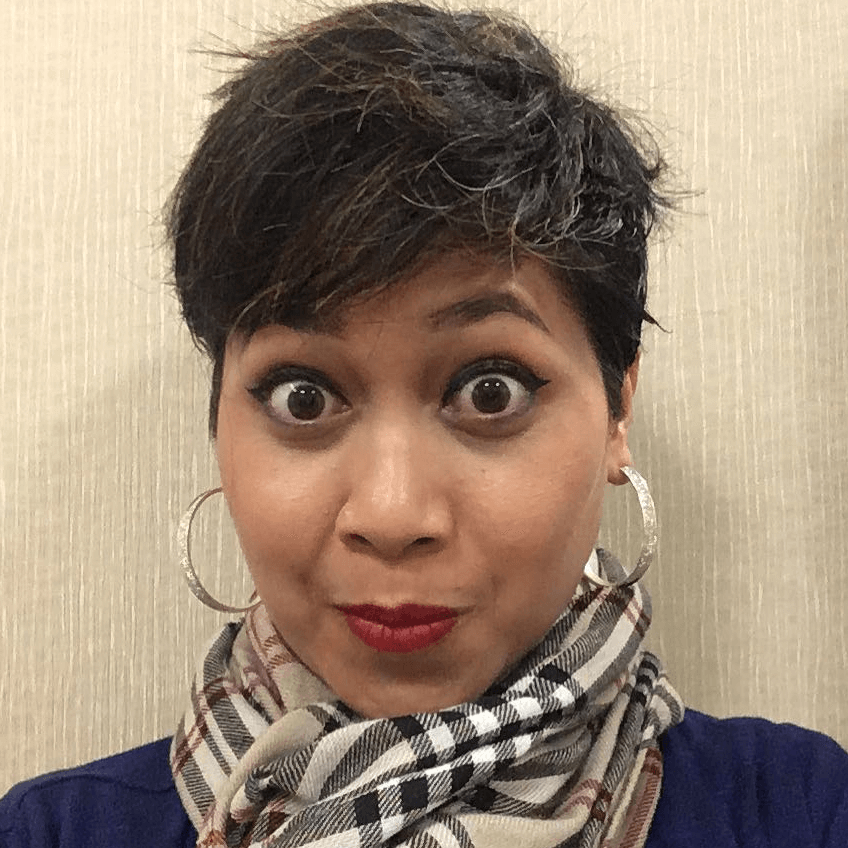
Shyreece Pompey, Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic) (Update)
Symptom: Shortness of breath
Treatments: Chemotherapy (carboplatin, pemetrexed & bevacizumab), targeted therapy (crizotinib & alectinib), AT13387 (HSP90 inhibitor)
Tiffany J., Non-Small Cell Lung Cancer, EGFR+, Stage 4 (Metastatic)
Symptoms: Pain in right side, breathlessness
Treatment: Clinical trial (osimertinib & ramucirumab)
Dan W., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Cold-like symptoms, shortness of breath, chest pains
Treatments: Radiation, targeted therapy (alectinib)