From Shock to Strength: A Young Mom’s Follicular Lymphoma Story
Courtney shares her journey facing grade 3B follicular lymphoma, diagnosed in 2022, and her subsequent treatment and ongoing battle with the disease. Initially, she experienced severe back pain, sinus issues, and fatigue, which led to her diagnosis of follicular lymphoma after a visit to urgent care revealed a large mass in her chest. That diagnosis was a shock to her and her husband, with Courtney feeling overwhelmed while her husband took charge of scheduling appointments and managing logistics.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez
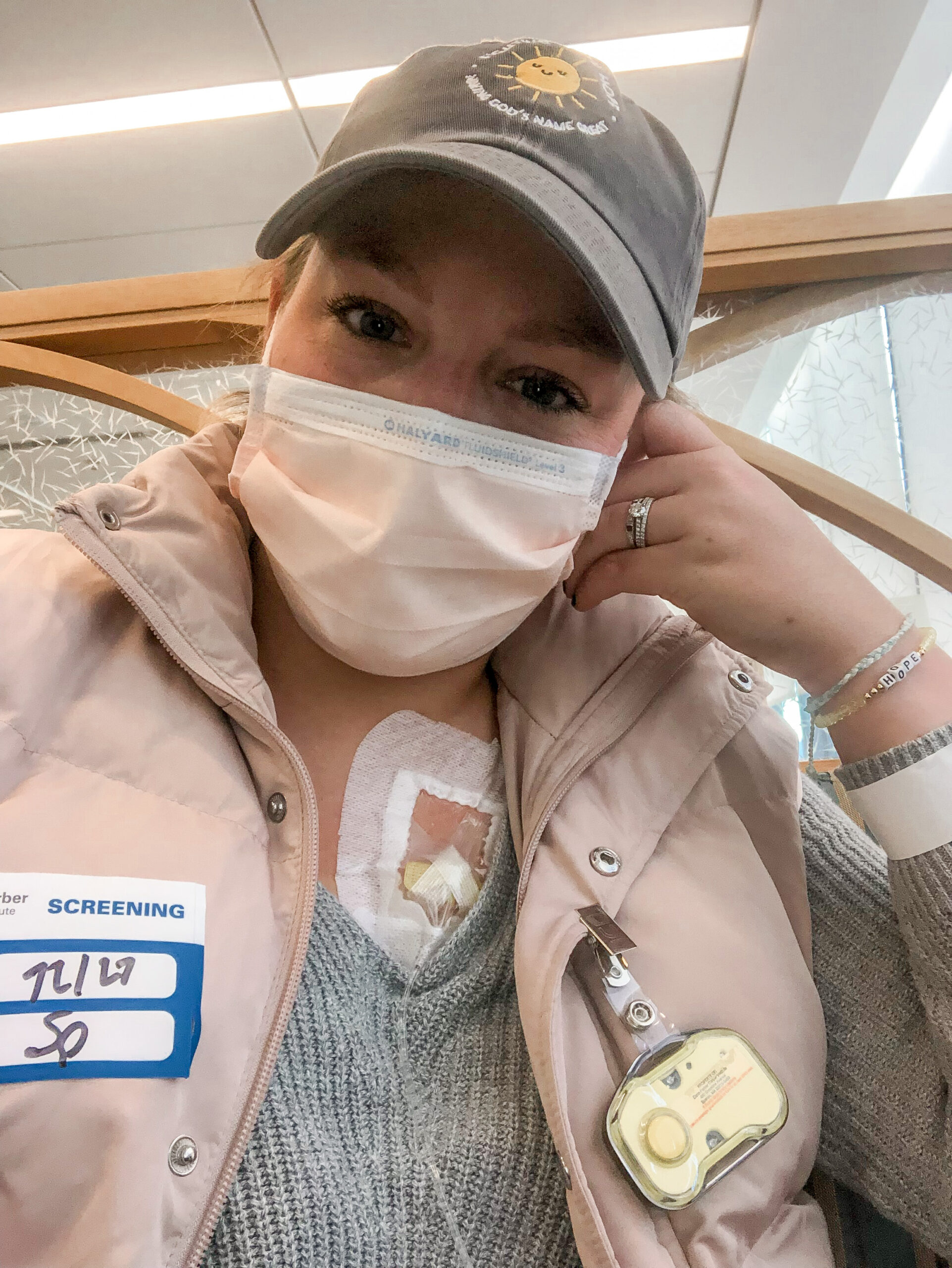
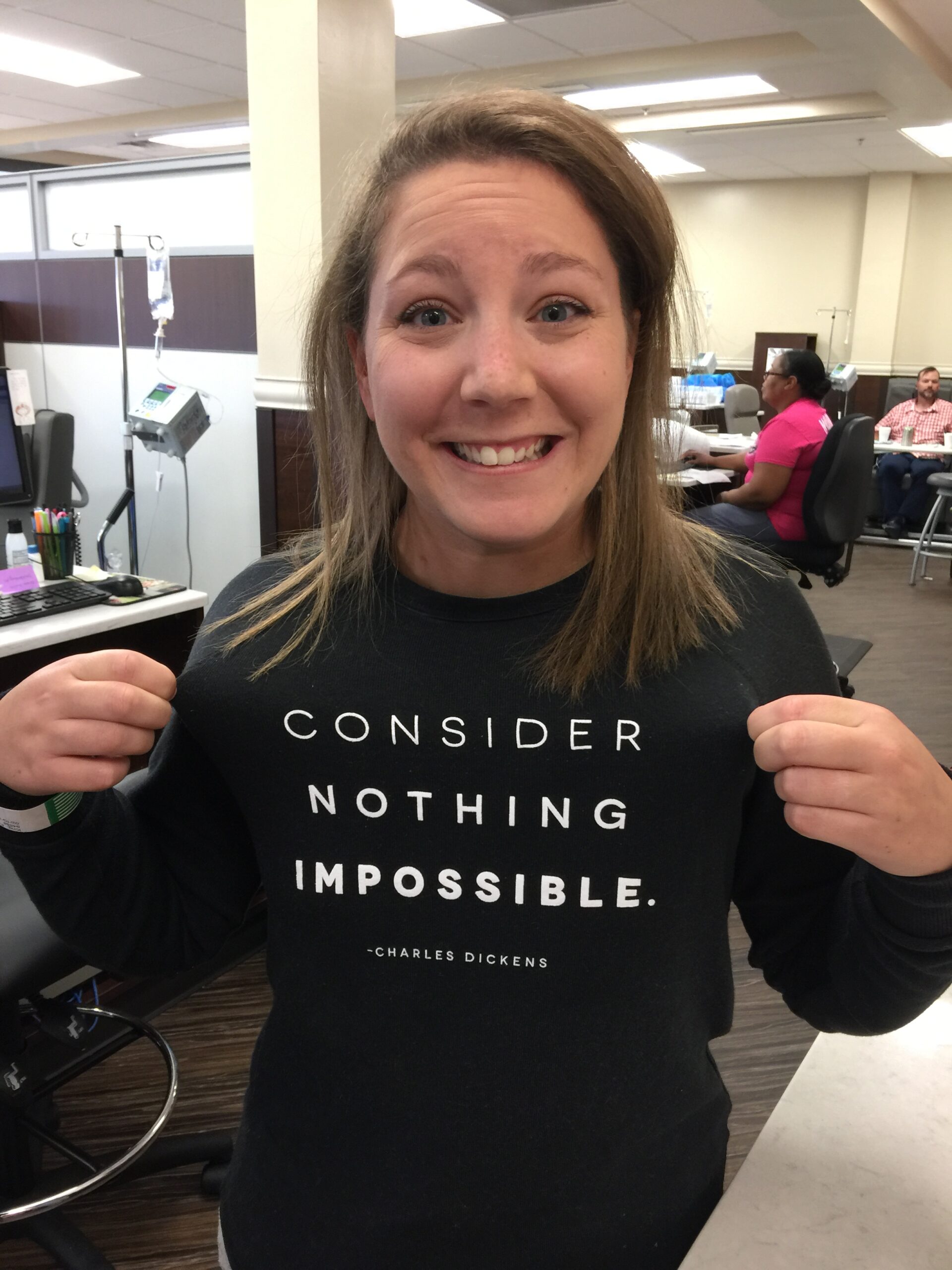
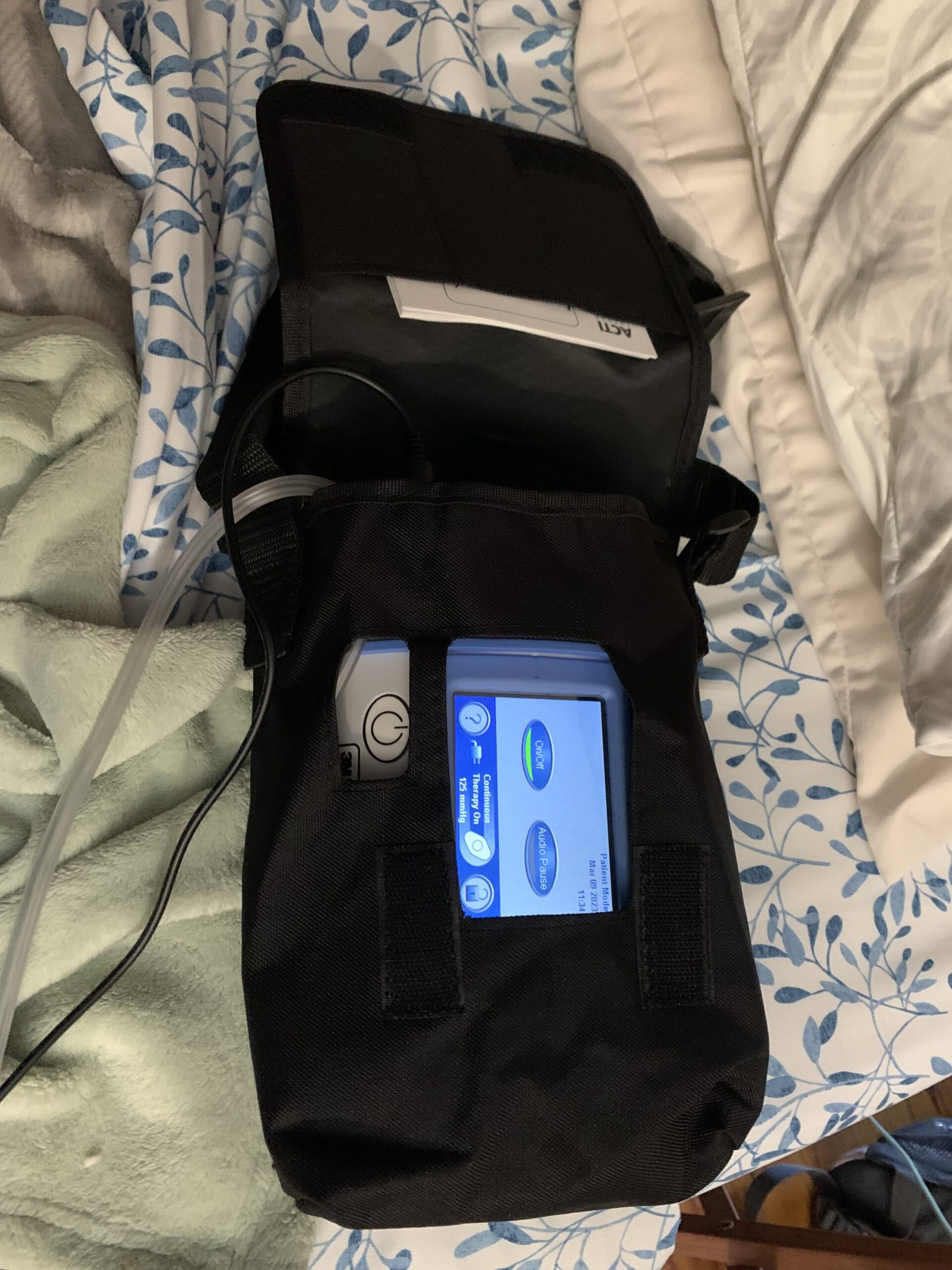
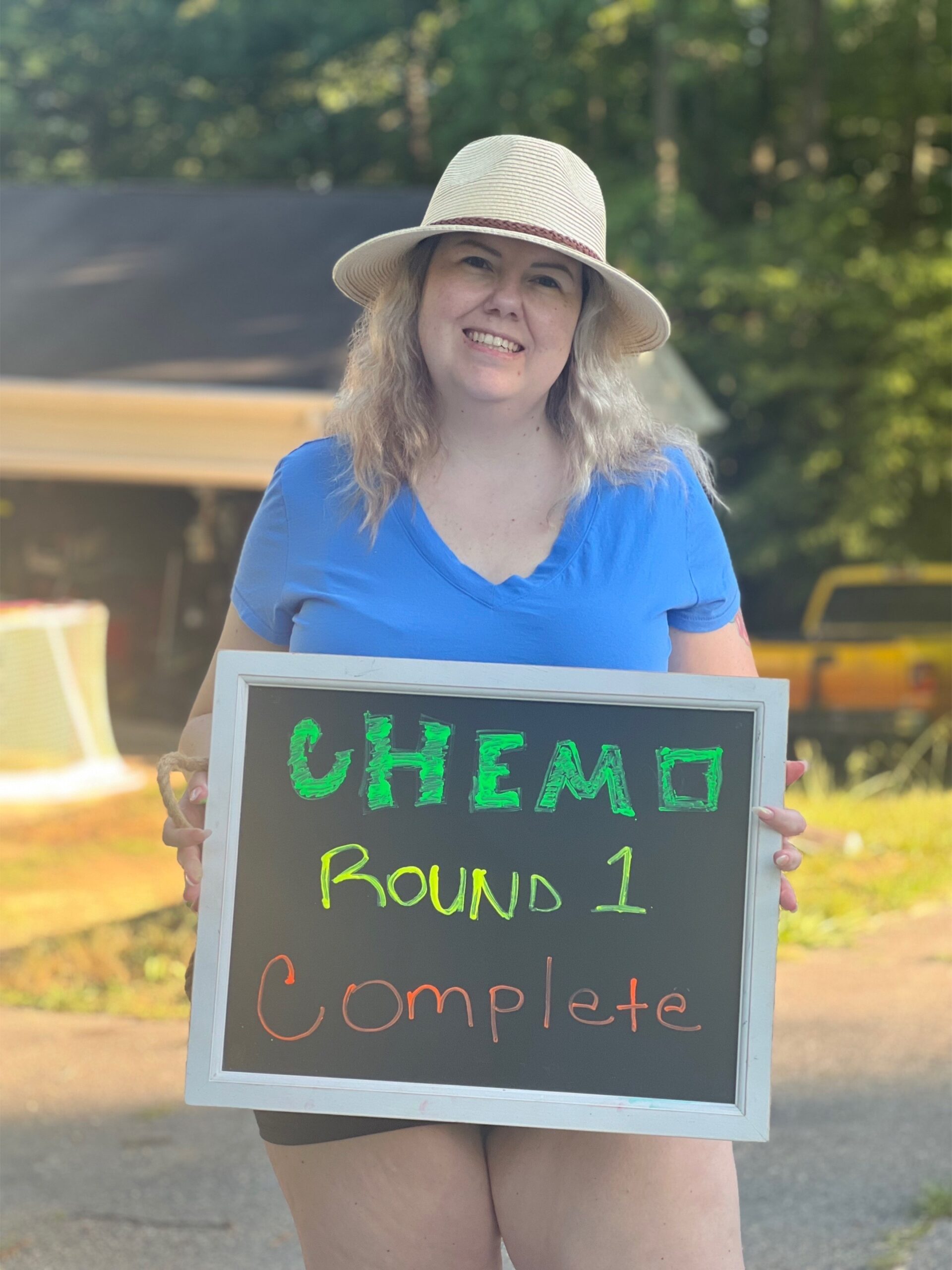
Courtney started chemotherapy soon after her diagnosis, enduring 6 rounds of treatment. The process was grueling, and she vividly recalls the emotional and physical toll it took, including the distress of losing her hair. Despite the hardships, she acknowledges the critical role her care team played, particularly her oncologist and the doctor from urgent care, both of whom provided essential support.

After treatment, Courtney reached remission, but the high-risk nature of her disease requires her to be vigilant about her health. She has regular check-ups and contemplates possible future treatments like CAR T-cell therapy. Throughout this journey, she emphasizes the importance of community support, expressing deep gratitude for her family and friends who have been there for her, and who have provided welcome emotional and practical assistance.
Courtney also discusses the psychological impact of her diagnosis, sharing her need to talk about cancer as a way to cope and bring awareness. She hopes that by sharing her story, others will understand that cancer can happen to anyone and stresses the significance of early detection.
Looking forward, Courtney remains hopeful, drawing strength from advancements in medical research and the support of her loved ones. She advises others in similar situations to document their journey, capturing every moment, because it becomes an integral part of their identity. Her message to others is one of resilience and hope: while cancer is challenging, it is not insurmountable, and individuals can find a way through it with the right support and mindset.
- Name:
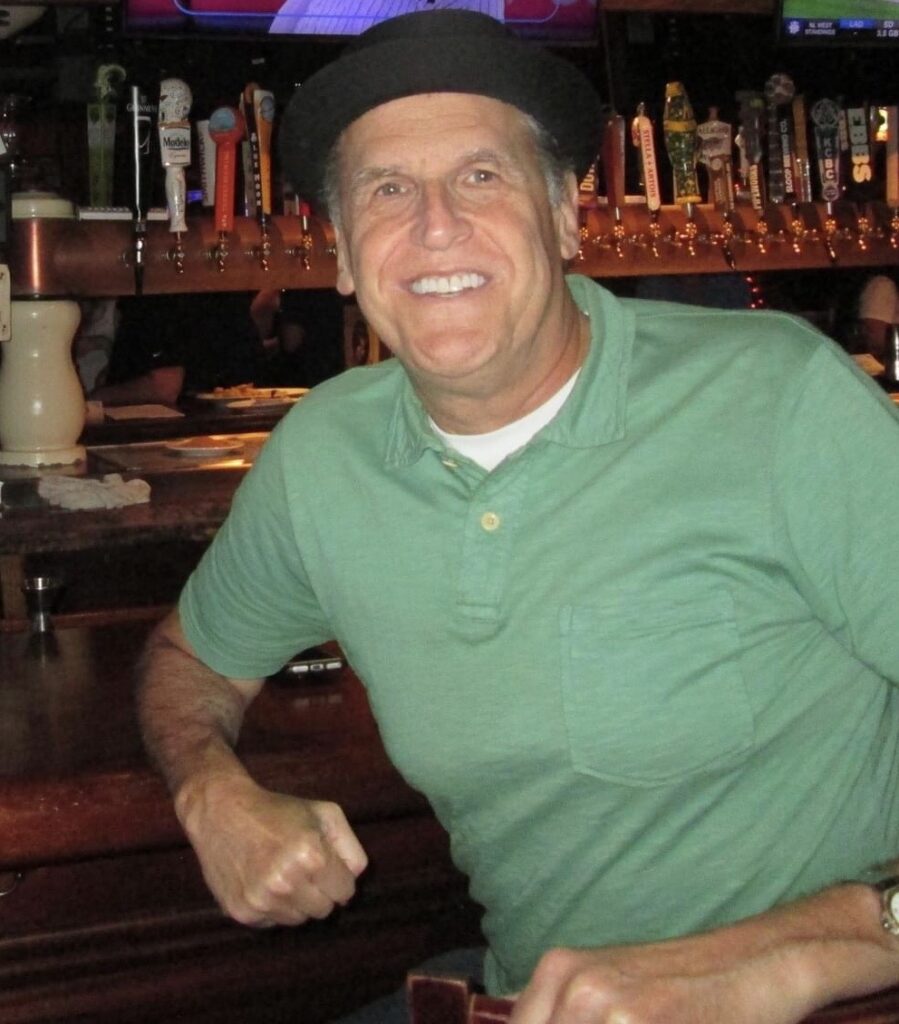
- Courtney L.
- Diagnosis:
- Follicular lymphoma
- Grade:
- Grade 3B
- Initial Symptoms:
- Intermittent back pain
- Sinus issues
- Hearing loss
- Swollen lymph node in neck
- Difficulty breathing
- Treatment:
- Chemotherapy

This interview has been edited for clarity and length. This is not medical advice. The Patient Story retains full editorial control over all content. Please consult with your healthcare provider for treatment decisions.
Follicular lymphoma is not the end of the world.
It might feel like it, but it isn’t.
Introduction
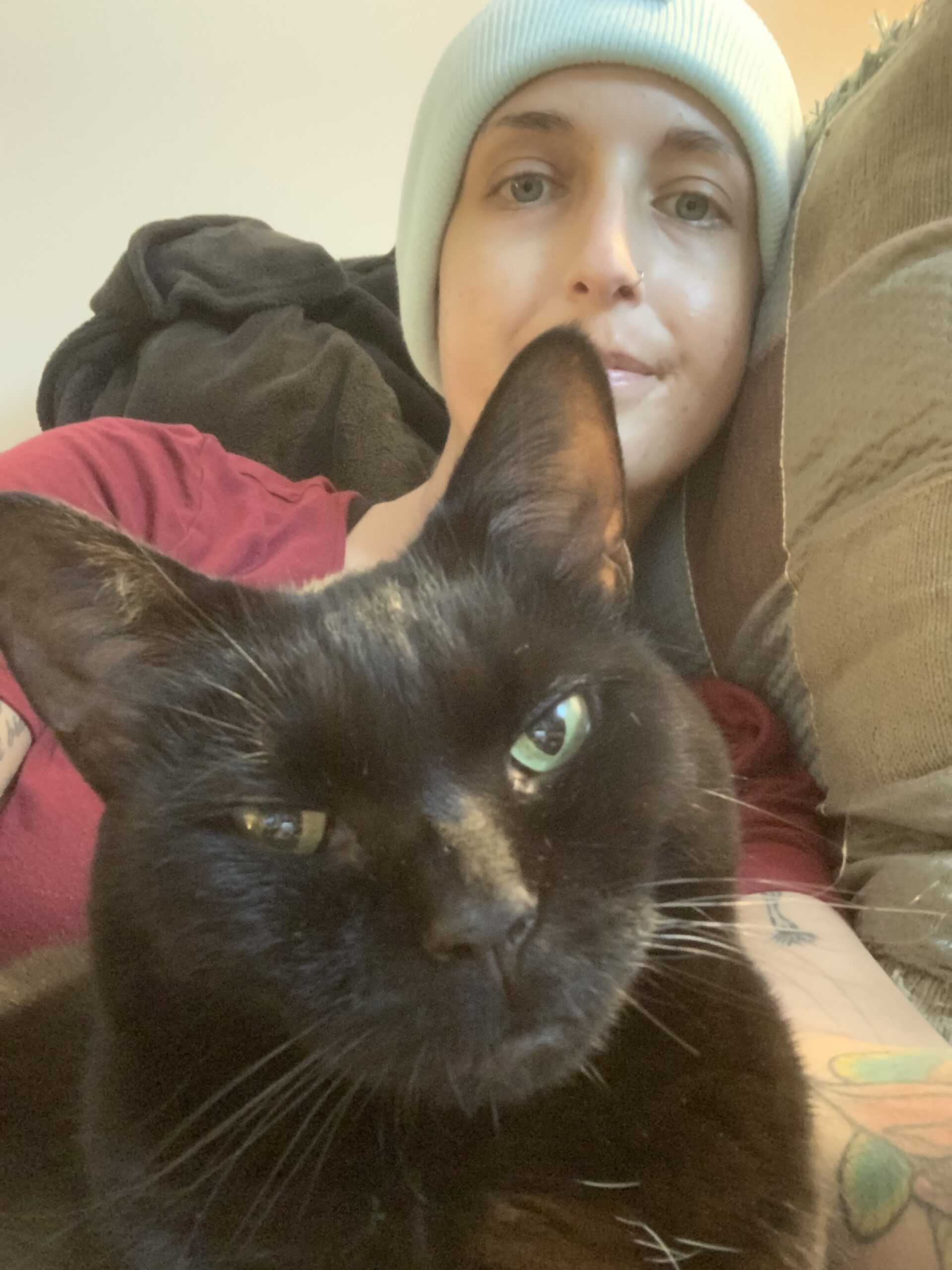
My name is Courtney and I currently live in Wisconsin.
I was diagnosed in 2022 with grade 3B follicular lymphoma. I also have a triplet mutation.


Pre-diagnosis
Initial symptoms
I really didn’t start feeling sick or off for too long. My first sign that something wasn’t right was just 2 months before my diagnosis, in December 2021. I started having really bad back pain. It wasn’t present all the time, but when I did have it, it was severe — sharp, stabbing pain in the shoulder area.
I also started having shortness of breath and a lot of sinus issues. My nose was draining constantly. No amount of blowing would stop it. I also began to lose hearing in my left ear. I’d wake up in the morning and would be basically deaf in my ear. And then it would take a couple of hours to get the hearing back. And then that cycle would just repeat.
I also started to feel very tired, and talked about it to one of my coworkers at one point. I said, really wish I knew what was going on, because I shouldn’t be this tired.
One night in January, I woke up out of a deep sleep, and I can’t recall what woke me up, but I remember thinking, oh my gosh, I think I had a stroke. The next morning, I told my colleagues about it, and one of them took me to the emergency room. There, they scanned my brain and head, and they diagnosed me with a complex migraine and a panic attack. Because I have a history of anxiety and migraines.
Some time after that, I took a trip to Mexico. I woke up one morning, and I had a huge swollen lump on my neck, and nobody knew what it was. And I spent that whole week Googling “swollen neck” and trying to find out what it could possibly be. Plenty of what I found online said it could be cancer. But I convinced myself that it wasn’t, because the internet is going to tell you the worst thing.
But then I began to struggle to take the stairs — even just one flight of stairs was a challenge. And then even when I got back to Chicago, the pain continued to be a concern. I told myself, I’m going to go to urgent care because I go back to work on Monday. If I don’t go now, I’m not going to go. So I went to urgent care.
Diagnosis
When I was at urgent care, the doctor did some lab tests, and then sent me to the hospital. She told me, you should just go get a scan so we can just see what it is. She added, I will call you personally in a couple of hours to give you an update. So my labs came back while I was waiting for the scan. My platelets were slightly high, and everything else was fine.
But she called me a couple hours later — and she said that there was a large mass in my chest. She didn’t even tell me about my neck. You have to go back to the hospital, she said. At that point, I still didn’t know that meant cancer.

So, on February 12, 2022, I went to a different hospital to be admitted. The radiologist met me in the lobby and brought me directly to my room. And there he told me, you have follicular lymphoma.
I went, I don’t know what that means. He explained it, and then tried to reassure me by saying that I met the criteria for Hodgkin’s lymphoma, “the good kind”, thanks to my age and gender, and he said that I could have the mass biopsied in the morning. So I had some sense of hope.
But as it turned out, none of that was accurate, and I ended up with a kind of non-Hodgkin’s lymphoma instead. Mine is an aggressive, rare, incurable kind of cancer.
I can’t not talk about cancer.
It’s a part of me now. It’s a part of who I am.

Reaction to the follicular lymphoma diagnosis
When we received the diagnosis, my husband and I were just in shock. But between the two of us, he’s the one who rallies when he receives tough news, and I’m the one that falls apart. I might not feel like getting out of bed or the shower, I might say that I’m down, I’m done, I need some time.
So rally he did. He was at the counter scheduling the appointments. He was taking time off from work to drive me around. I didn’t have to worry about any of that, which was good because I couldn’t do it at the time. So that was great. That was everything that I needed.
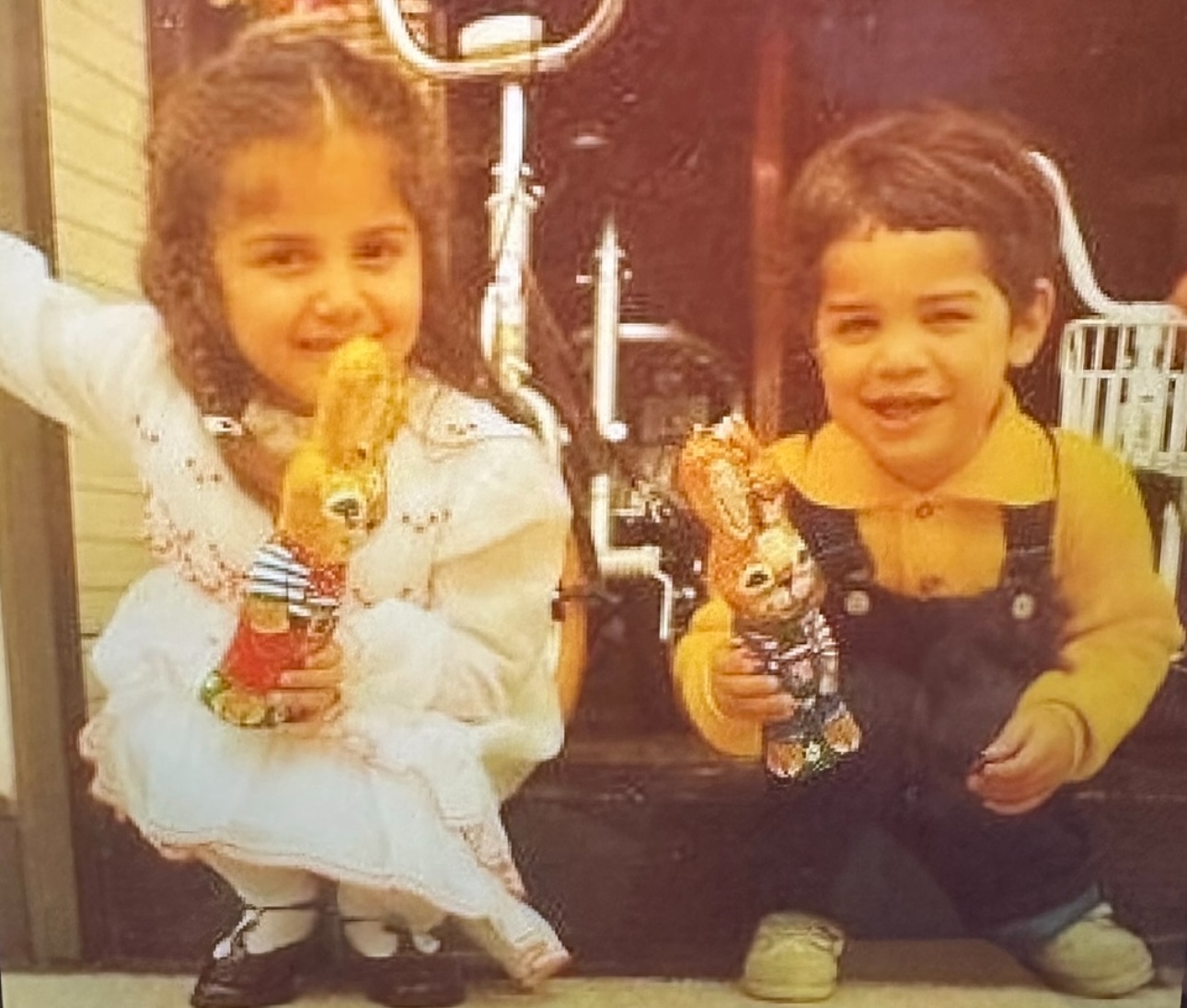
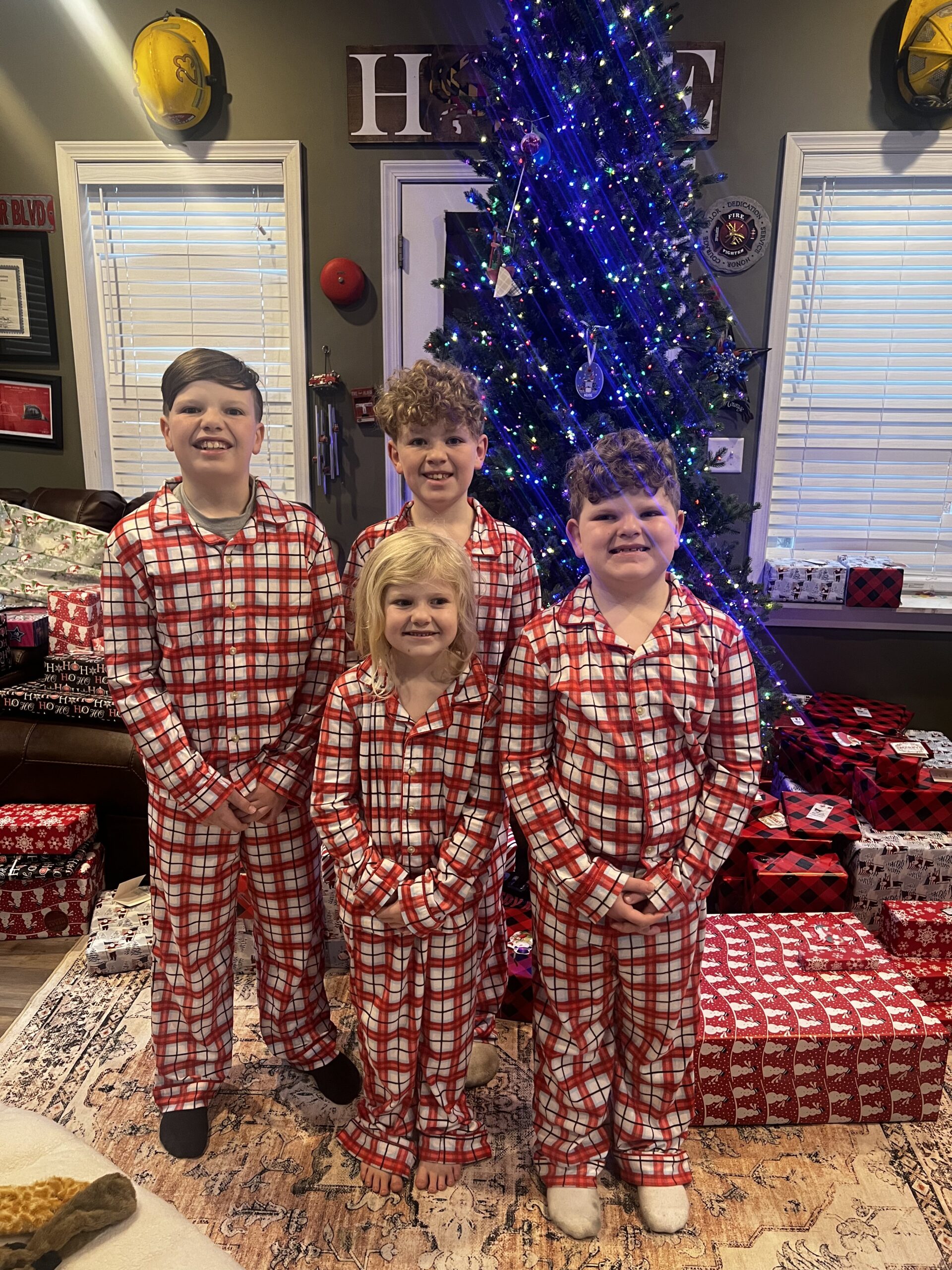
As for my kids, I hate that for basically their whole lives, I will be sick. They’re not going to know any differently. But it will be all they know because they were so young when this all began. To look at it like in a good light, they were so young at the outset that they didn’t really know the difference.
Treatment for follicular lymphoma
After my diagnosis, there was no time to waste. They told me I needed chemotherapy right away. And I didn’t really have a choice — I mean, of course I could say no, but if I did, I was going to die. Within the 2 months that they thought that I had cancer, it had spread over my entire body.
I only remember a couple of things about the initial appointment at the cancer center, because I was still on pain mediciness back then. I couldn’t retain anything from that time because of my meds. I’m so thankful for my care team, my oncologist and the doctor who initially saved my life in urgent care. She’s now my primary care doctor. They are my people, they are everything to me.
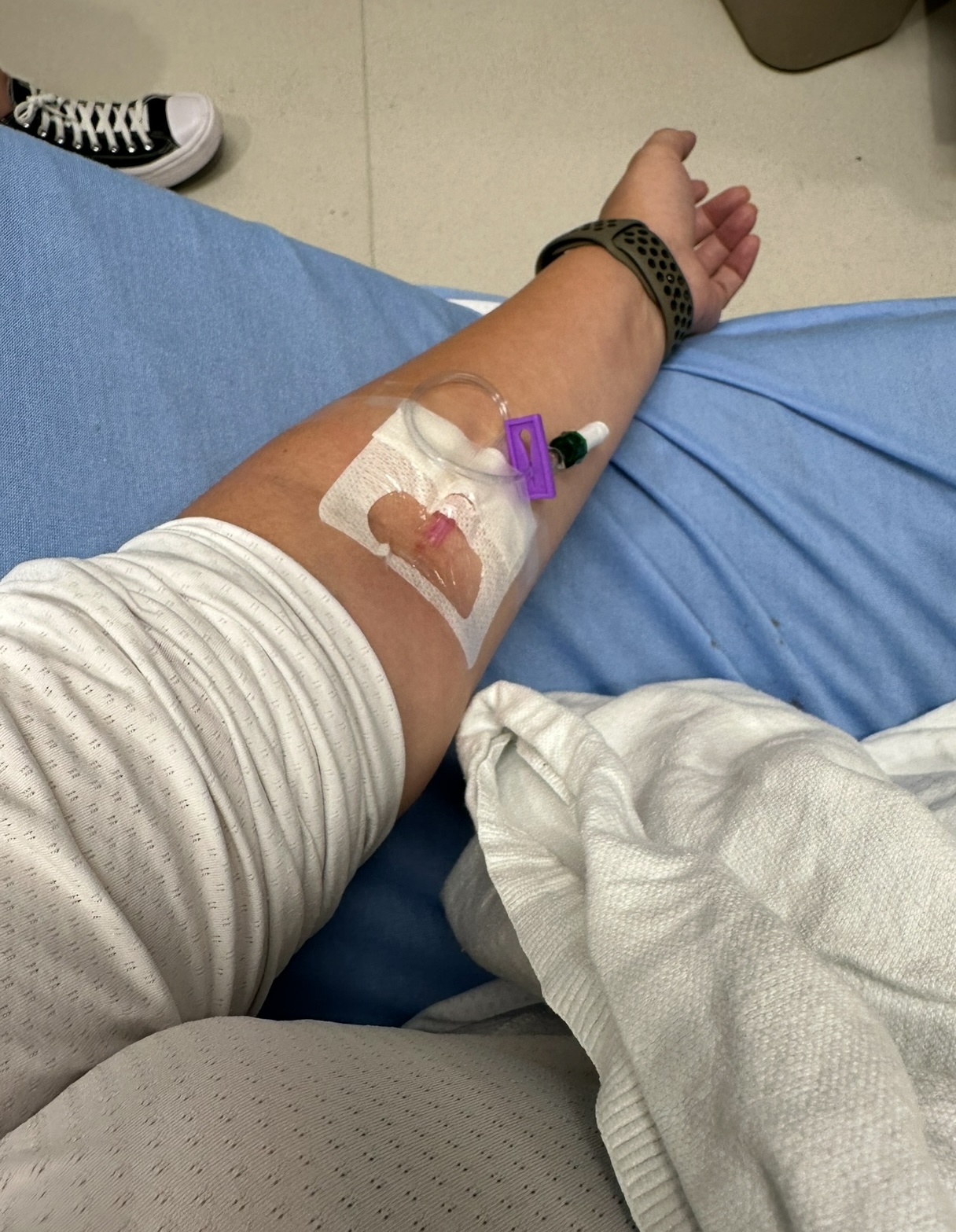
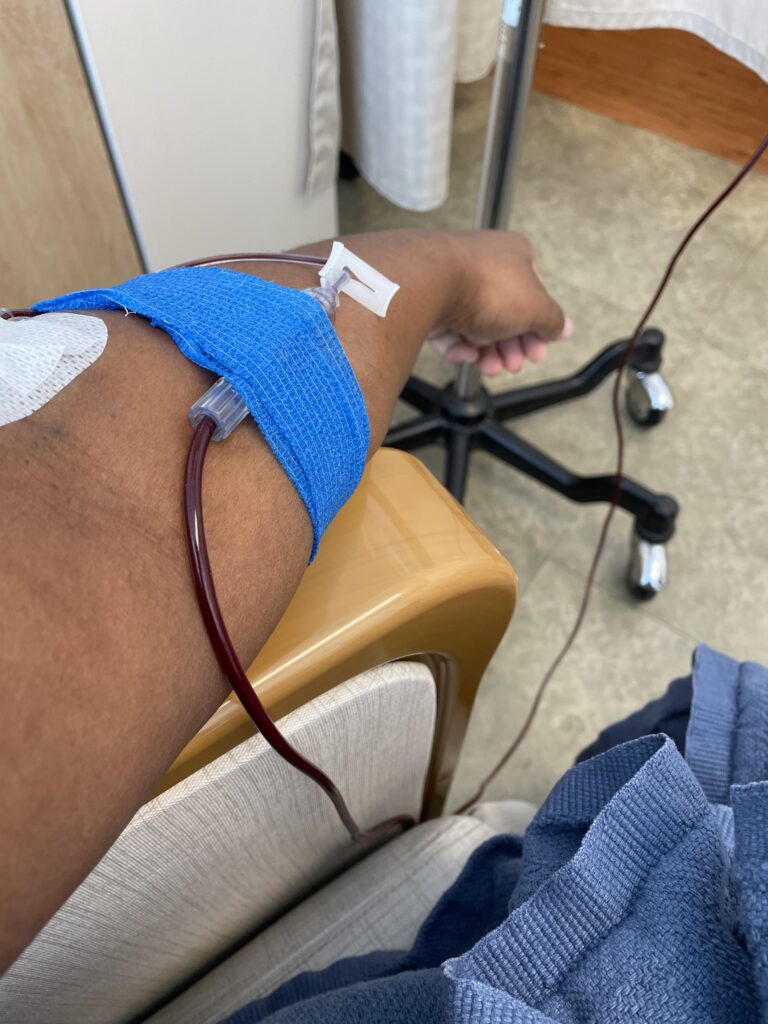
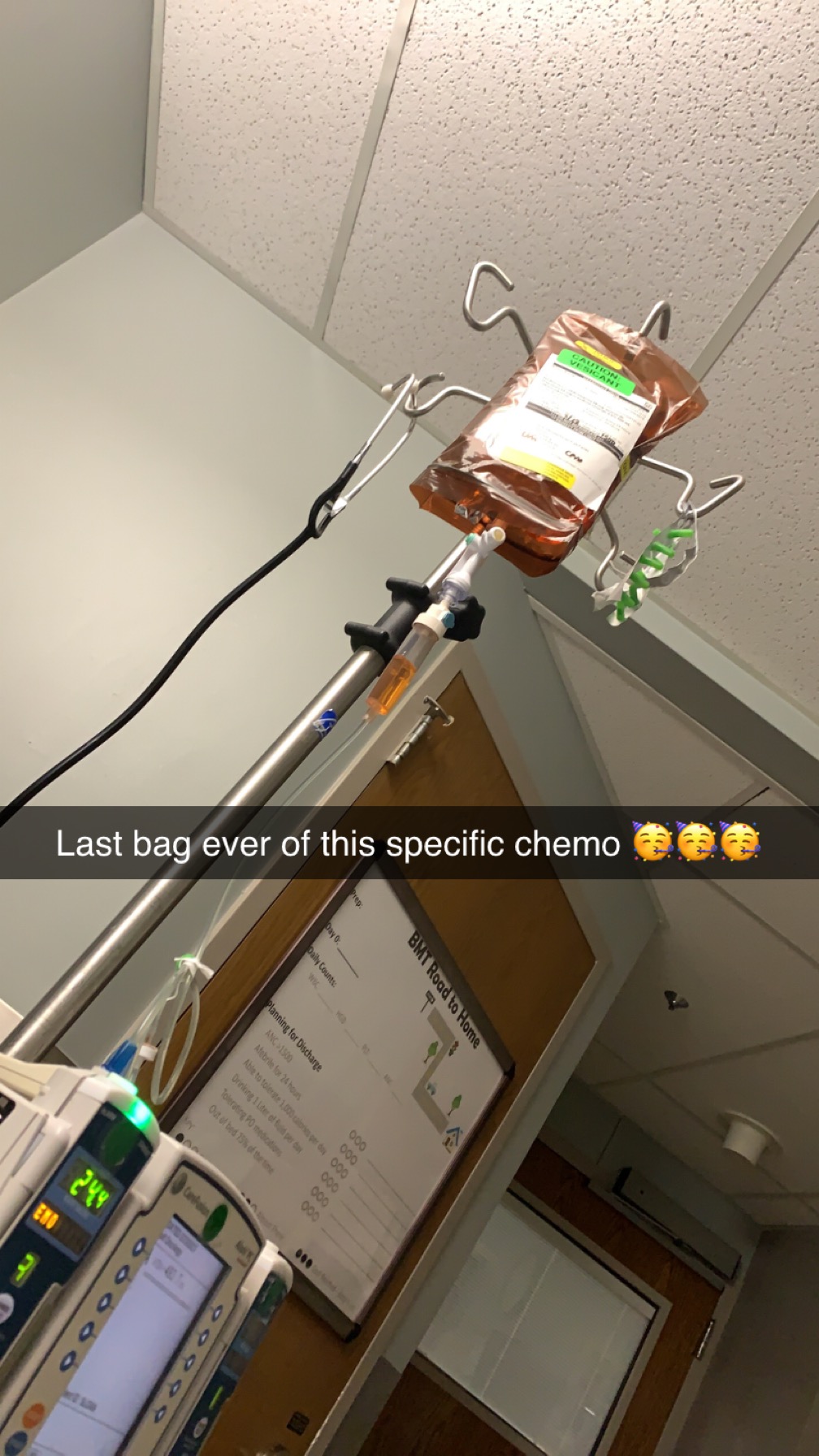
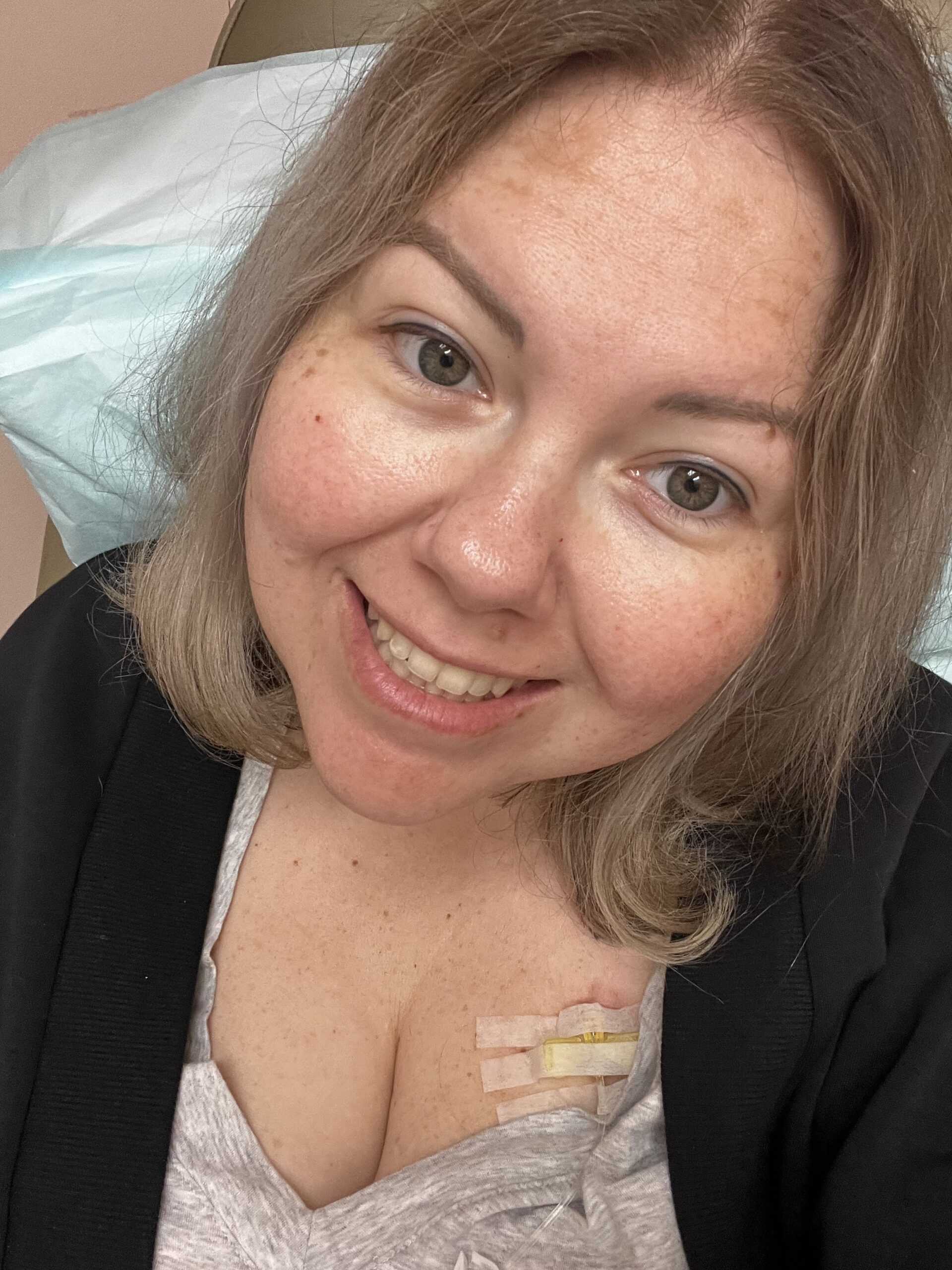
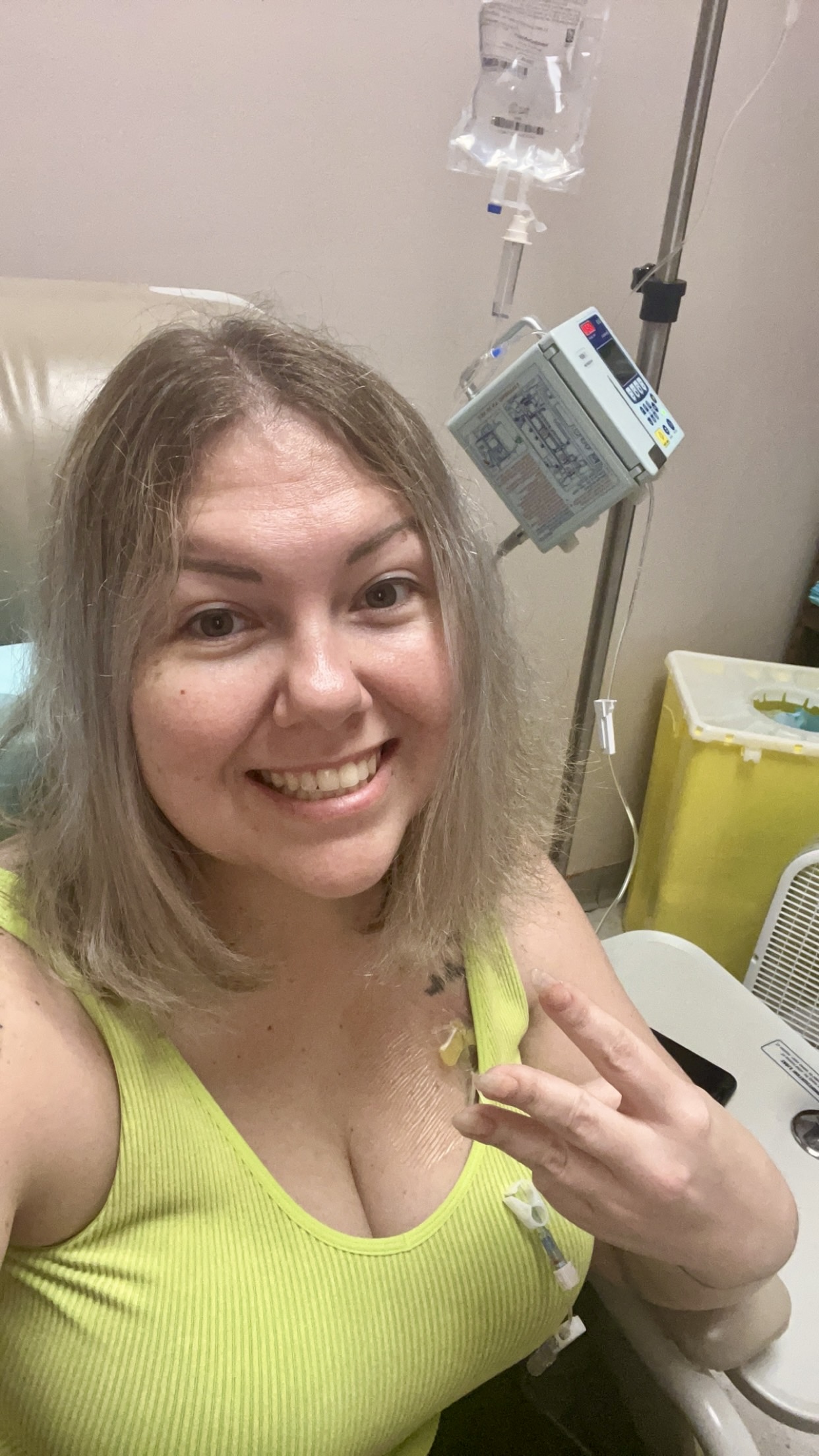
I had surgery on the 13th of February. I had my PET scan, my port placed, and my bone marrow biopsy done, all within days. And then I started chemotherapy within a week.

I did a total of 6 rounds of chemotherapy. And although it was okay at first, after that, it wasn’t fun. It didn’t feel good. I would go home after my treatment, and that’s where I would get pretty sick afterwards. If I wasn’t at the cancer center, I wasn’t getting out of bed. But I think everybody who takes chemo responds to it differently.
Looking back at it, I wish they could have given me a checklist, some sort of record that I can refer to, because you want to remember experiences like that, you want to go back and know what you went through. But I do recall looking back and realizing how distraught I was. I was a wreck. And I also remember saying — am I going to die? I do know now that cancer is not a death sentence if you catch it early enough.
I did ask for statistics, numbers, but the doctor didn’t have them. She did say, though, that I would lose my hair. And that made it worse.
Why me? And why at this age? I don’t think I’ll ever stop thinking and asking that.
But it’s not just about me.

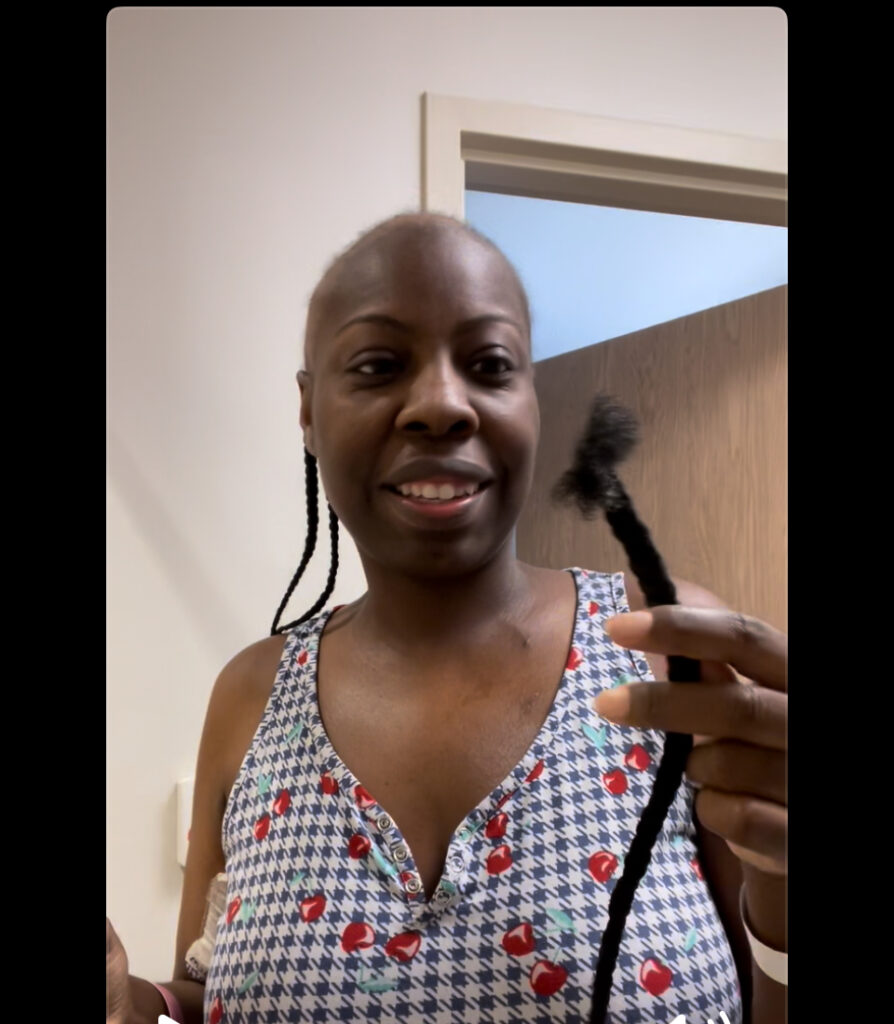
Loss of hair
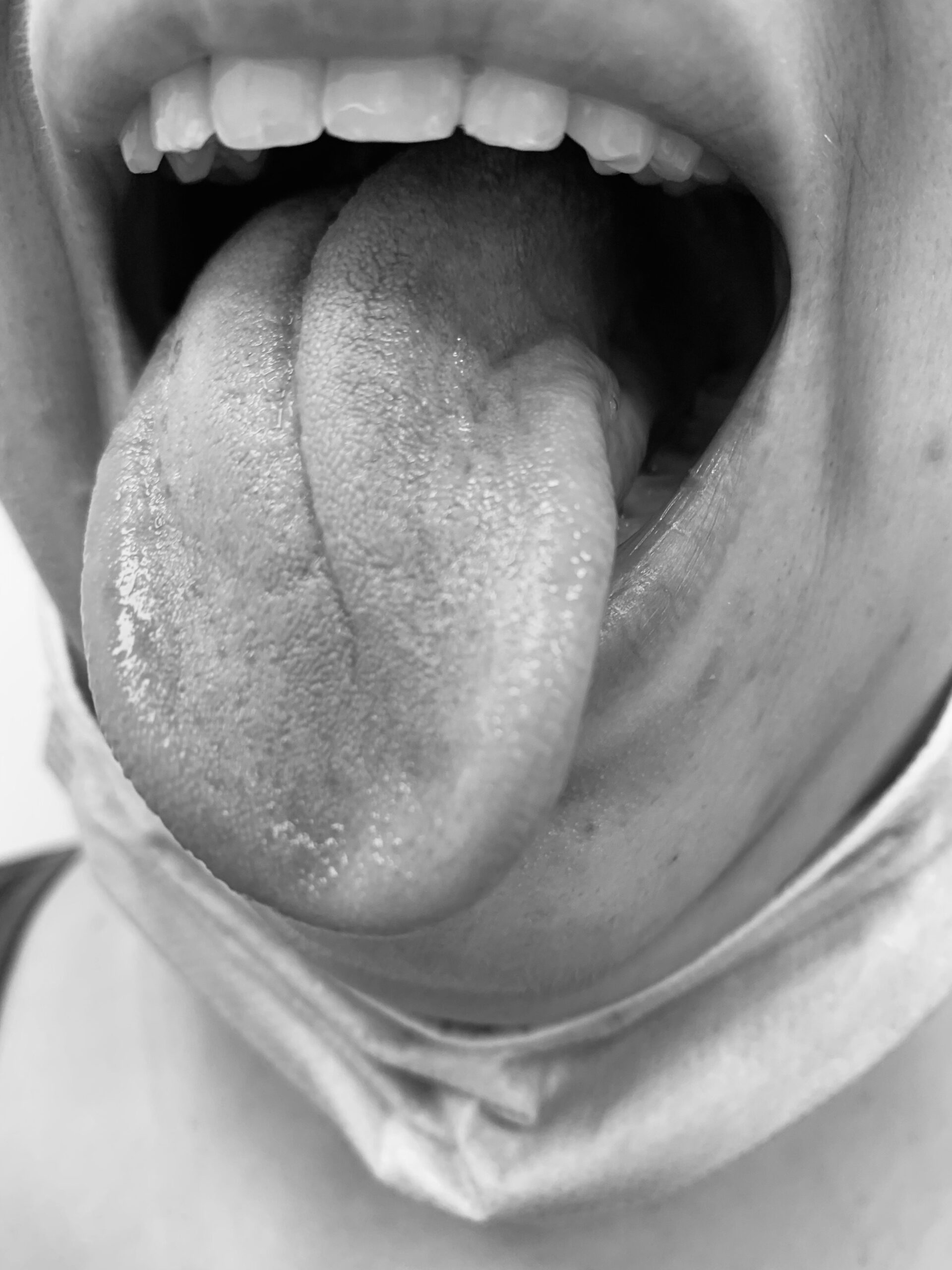
The nurse practitioner I spoke with did the cancer 1-on-1 with me. She said, you will lose your hair with this. And that’s exactly what happened.
I woke up one morning after the first cycle, and my hair was just coming out. All I needed to do was touch it and it would come out in clumps, just clumps at a time. And that was really difficult for me because I have a lot of long hair.
We ended up just shaving it off. If I didn’t, it would hurt like crazy.
It was one of the worst days. But the hair does grow back.
Post-treatment
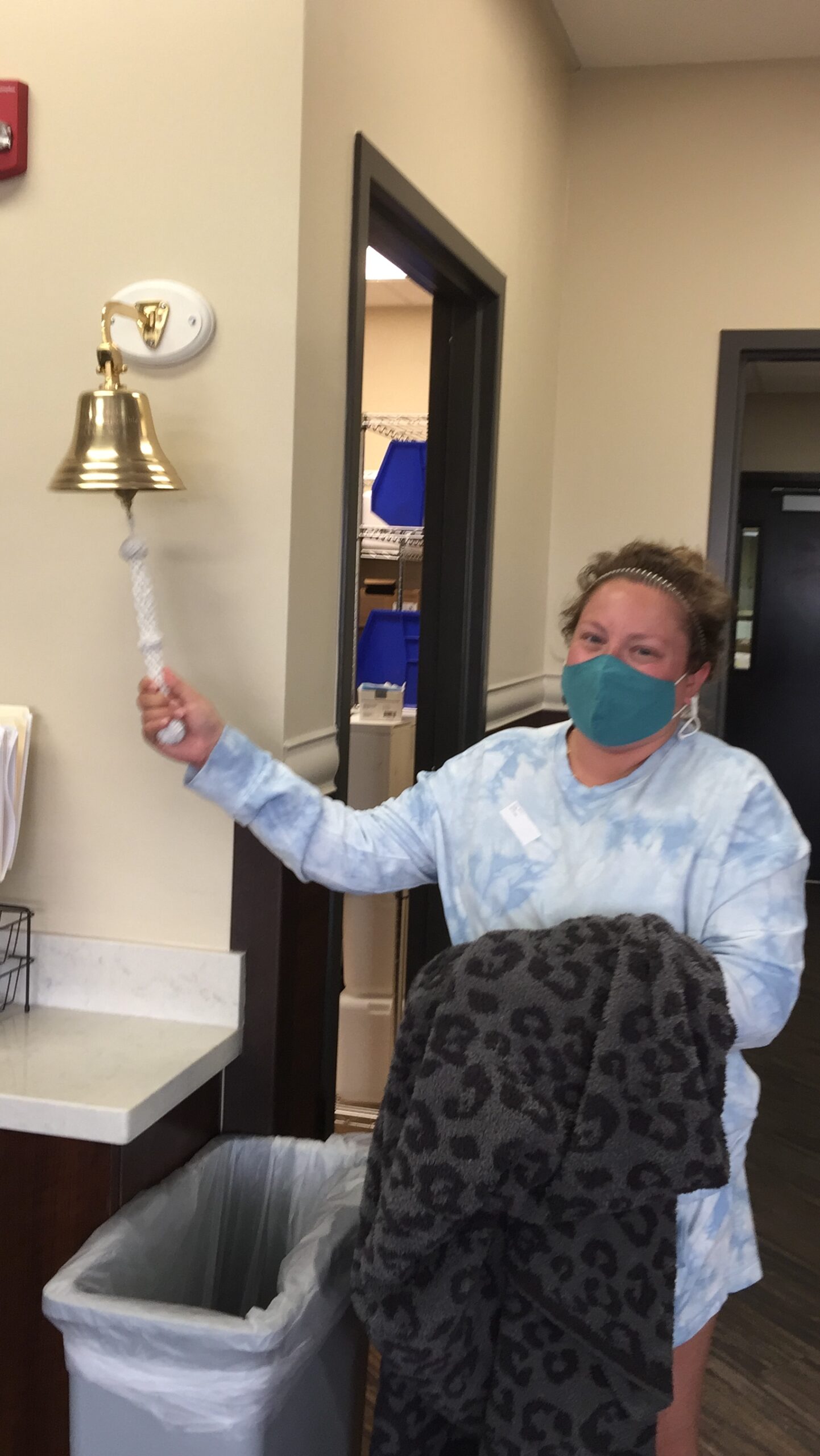
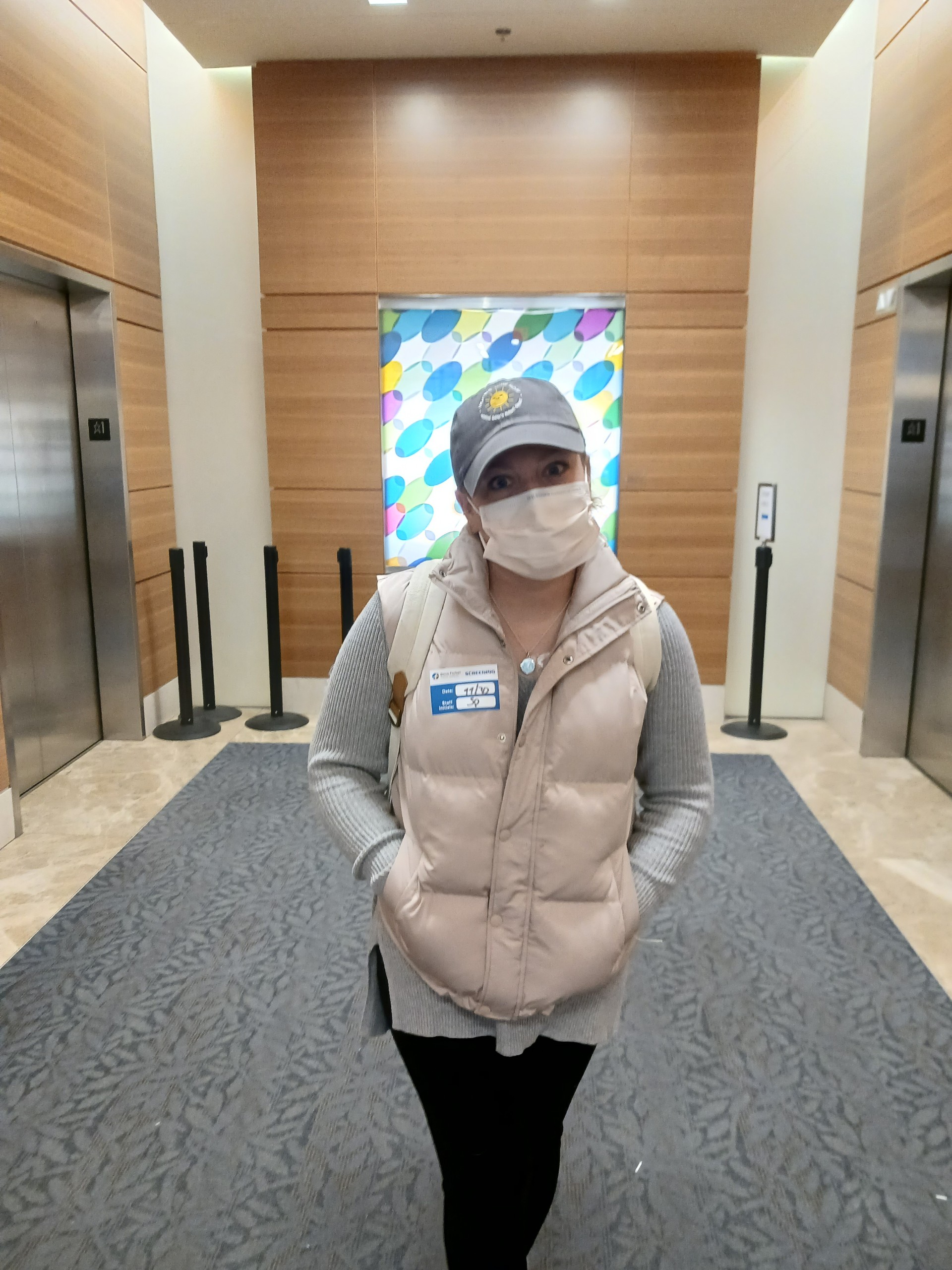
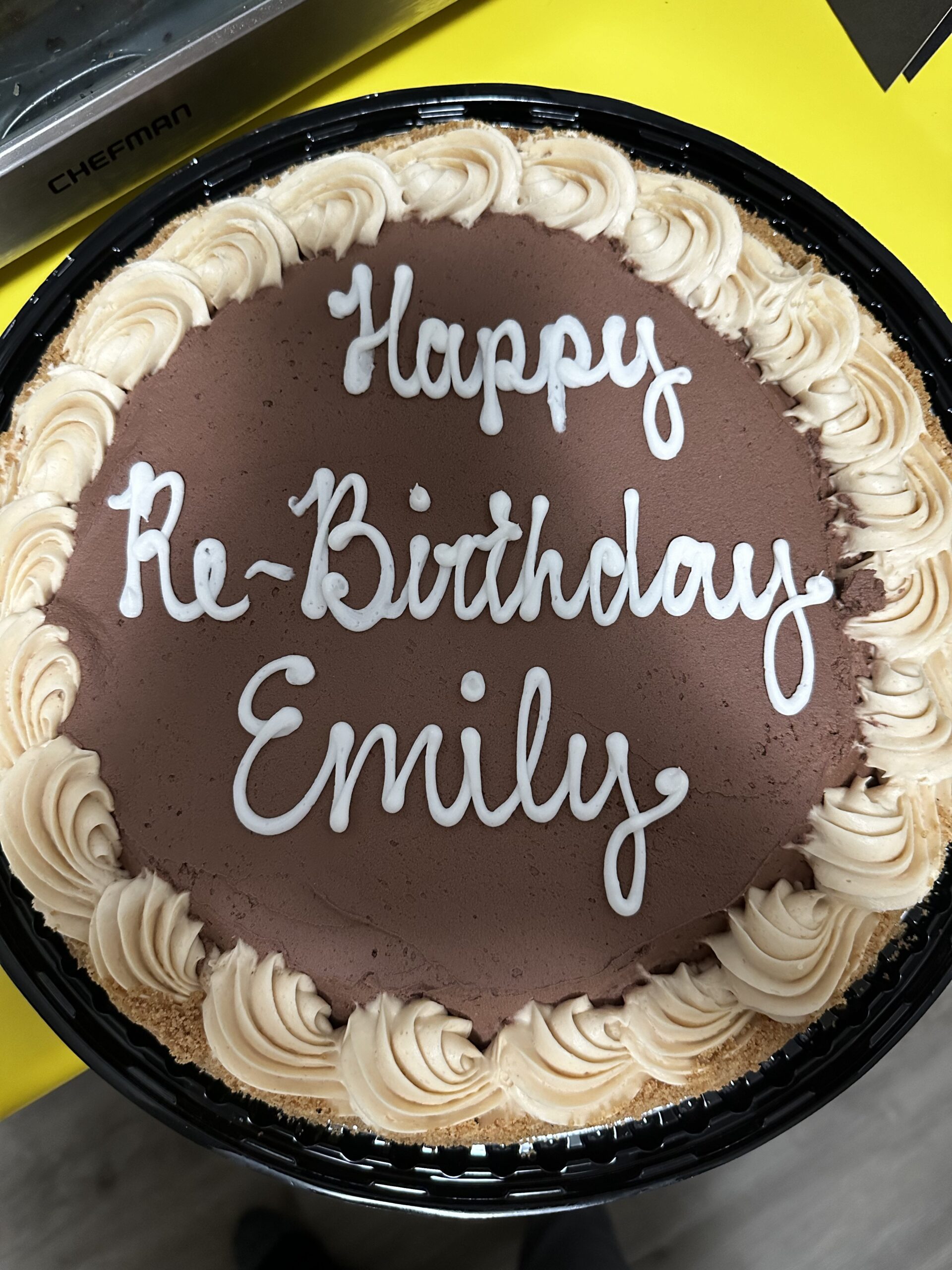
After my 6 chemotherapy rounds ended, I was thankfully in remission. But my follicular lymphoma is extremely high-risk, and this has affected my life even after my chemotherapy has concluded.
My last appointment or couple of appointments would have been 2 years out from the initial chemo session. My oncologist seemed to be on the verge of saying that we could start to space out the appointments since I was already at the 2-year mark, which is a big thing for us cancer patients, and maybe we could start seeing each other less. But then he checked himself and said, we can’t change your treatment schedule, because you really are too high-risk.

So now I’m 2 and a half years out from chemo, and that’s just great. But it does take a toll on me. Some days I feel that at my next check I’ll find that I’ve relapsed. Other days I’m more positive and I think, look, I’ve made it this far, I’ve beat all the odds.
It’s hard, it just depends.

Coping with her situation and helping others
When I’m having a really bad day, I let myself have a bad day. I know when my situation is overwhelming me. And when it comes to that, I just talk about it.
I can’t not talk about cancer. It’s a part of me now. It’s a part of who I am. And I don’t know if my need to talk about it is due to fear for other people or fear for myself.
The research out there says that it’s devastating for people my age. It’s a matter of catching it before it gets too late. So I want to bring awareness to the people around me who don’t think that cancer can touch them.
I used to not know what cancer was. Cancer is cancer, I thought, there’s no differentiation between the different sorts. Boy, was I wrong. There’s so much I don’t know about it yet.
So I try to talk about it in a way that can help other people, not just myself.
I have so many people around me whenever I need them.
I couldn’t ever have done this by myself.
Being diagnosed with cancer at a young age — and looking forward
Why me? And why at this age? I don’t think I’ll ever stop thinking and asking that.
But it’s not just about me. I also want to know why lots of people around me have been diagnosed with cancer recently, all different kinds of cancers. And none of them are better or worse than the other one. Some of my friends who have been diagnosed with different kinds of cancer have gone through worse treatments than I have. And hopefully, they will be cured.
I end up thinking, at least I don’t have to go through all those treatments like they are. But my case is different. The next step for me is a transplant, not more chemotherapy. I did ask about maintenance chemo and they said it wouldn’t be any more beneficial. I asked about genetic testing, too, because I’d also like to know if my kids need to be worried about this.

I’m young and I think my youth has helped me a great deal. My age has been on my side in this struggle. I also do know that grade 3B follicular lymphoma itself is extremely rare and is not treated as a normal lymphoma. And that’s where the difficulty lies. Determining the next steps and even navigating life itself now.
You don’t get many 30 year olds who have gone through this before. At my halfway chemo point, some people might have been clean at that point, and we were shocked that I hadn’t made progress. But I have hope that things will change. I see lots of research happening all the time across different areas. And though it is such a small percentage of people that have this, and the research isn’t being funneled my way, I hope that my time will come.
For example, I recently learned about CAR T-cell therapy. I got excited at the thought that maybe this would be my next step if I did relapse. It’s FDA-approved worldwide. It could work for me. So I have hope.

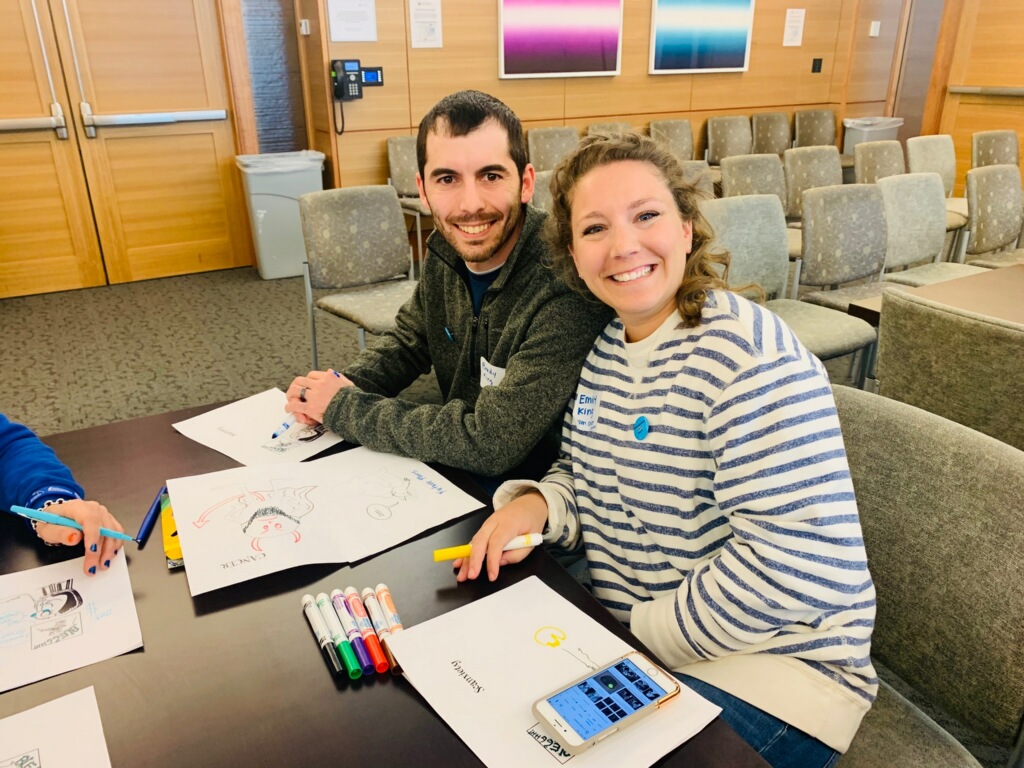
The importance of community
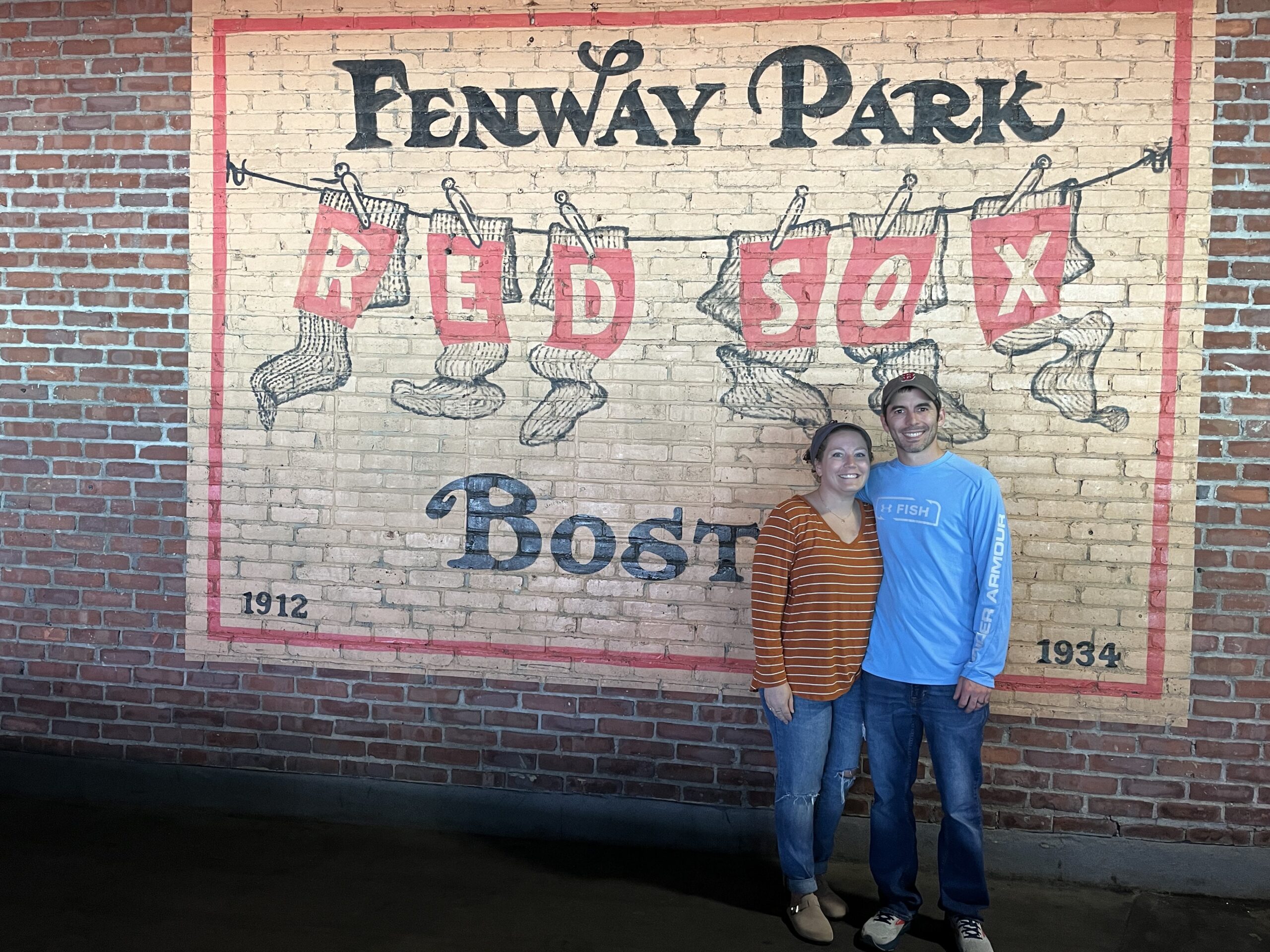
I have so many people around me whenever I need them; I couldn’t have ever done this by myself. I don’t think anybody can, so I just feel very lucky for all of it.
You can’t do this alone. And I am very lucky for everybody that I have around me, that listens to me, that lets me talk, lets me cry. That gives me a hug when I need it. That drops everything for me, takes me to appointments. My husband, my kids, my family, my friends, everybody.
I just I get emotional thinking about thinking about them all. I really am very lucky.
I don’t want to discount the things that I’ve gone through.
Because my experience wasn’t pleasant, but I’m all the better for it.
Advice Courtney offers
Record everything, including the first appointment, because you’re not going to remember it. Record yourself. Take photos. Even now, my brain doesn’t remember everything, so I keep on recording.
I don’t want to forget this part of my life, because it’s who I am now. I don’t want to discount the things that I’ve gone through. Because my experience with follicular lymphoma wasn’t pleasant, but I’m all the better for it.
I just hope that even 1 person hears me eventually and understands that it can happen to you, even if you don’t know what follicular lymphoma is and that there are different kinds of lymphoma, or even if you’re not aware of the basics of cancer.
Follicular lymphoma is not the end of the world. It might feel like it, but it isn’t. Yeah, you can be okay.


Inspired by Courtney's story?
Share your story, too!
Related Cancer Stories
More Follicular Lymphoma Stories
No post found