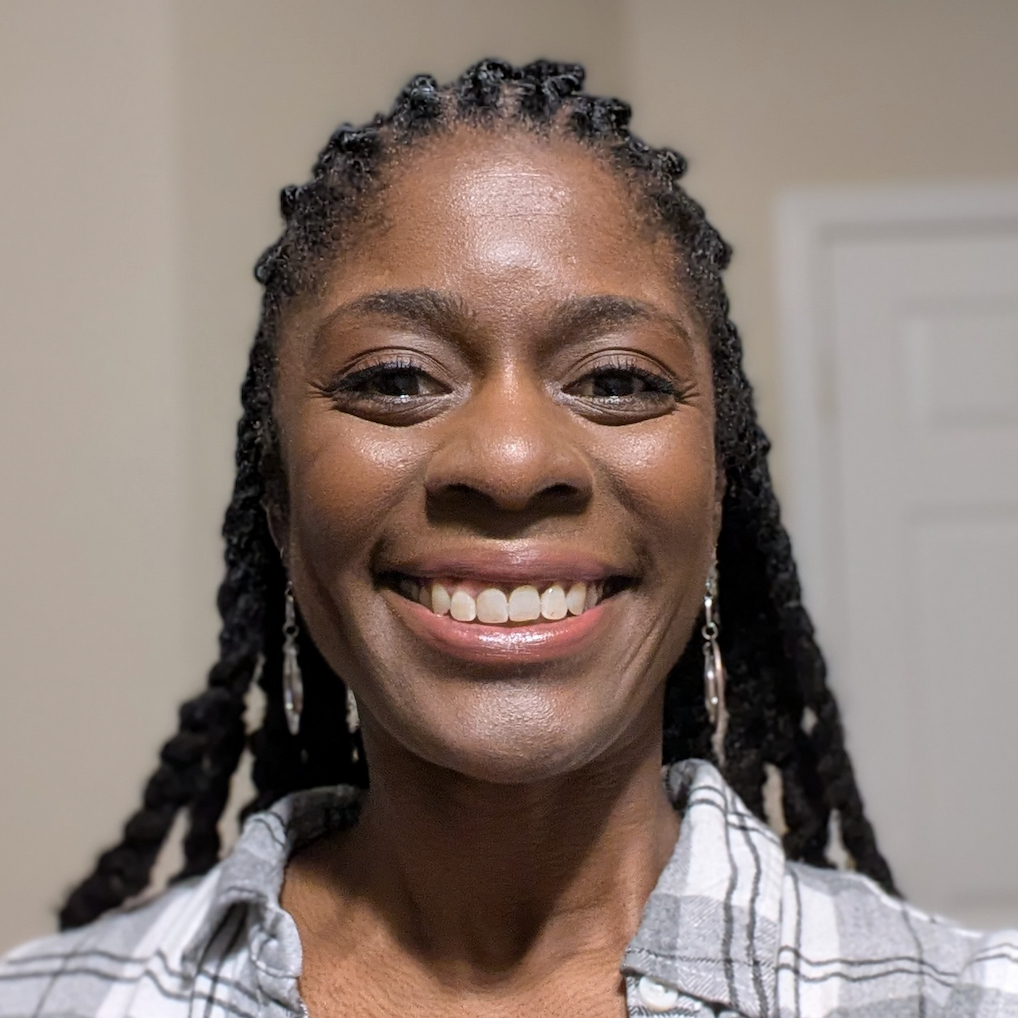
Resilience and Recovery: Dana’s Path to Living Fully with Crohn’s Disease (IBD)
In 2010, at the age of 15, Dana was diagnosed with Crohn’s disease (IBD) after experiencing severe gastrointestinal symptoms and significant weight loss. Initially mistaken for a minor issue following wisdom tooth surgery, her symptoms later on escalated, leading to a referral to a gastroenterologist. The diagnosis was ultimately confirmed via a colonoscopy after hospitalization due to severe anemia.
Interviewed by: Nikki Murphy
Edited by: Chris Sanchez
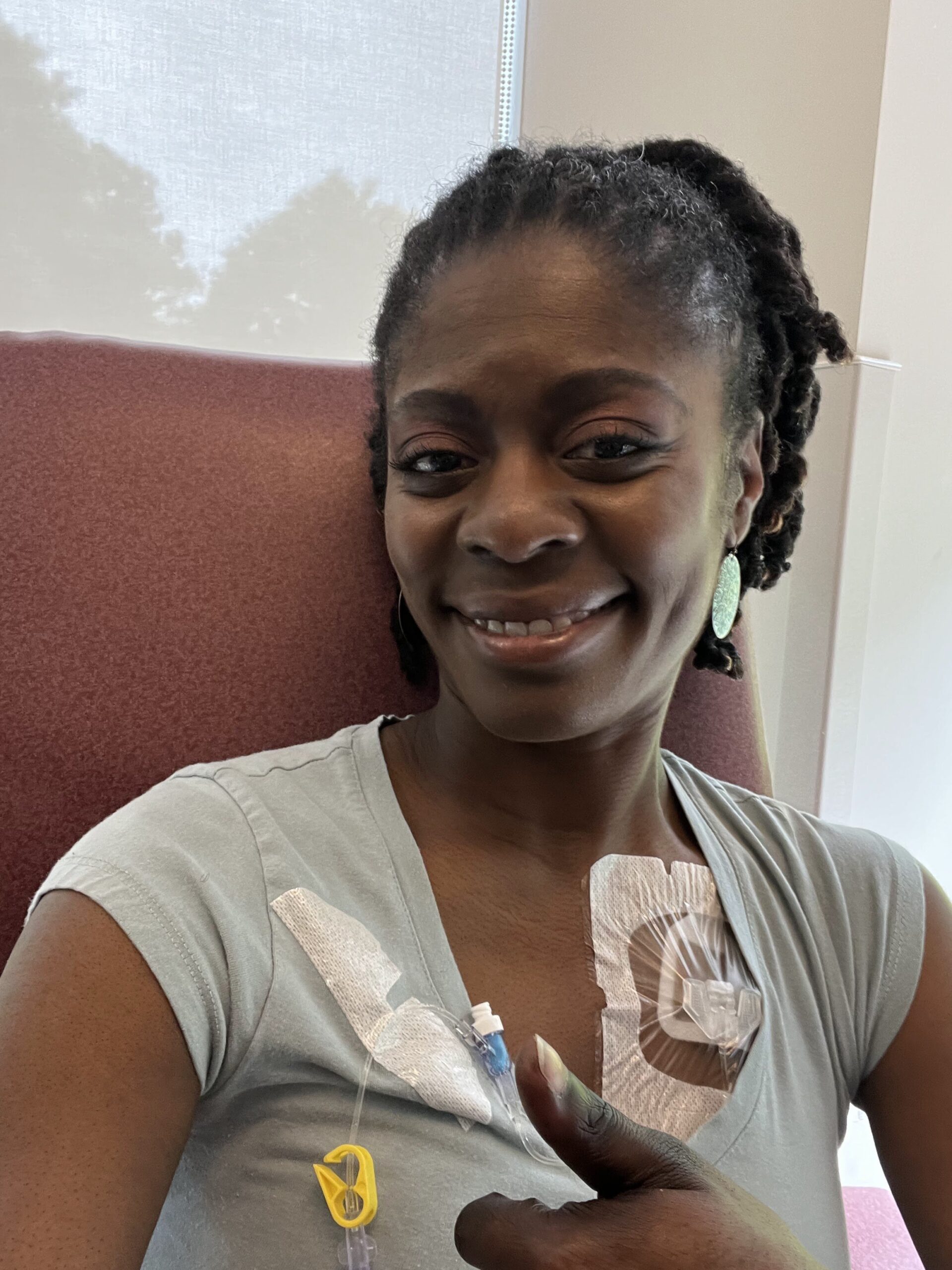
Dana’s experience with Crohn’s disease has been complex and difficult, involving various medications and surgeries. Early treatments began with corticosteroids to manage immediate symptoms, followed by oral immunosuppressants and, later, more intensive IV medications. While one of these medications induced remission for a few years, side effects later made it necessary to try different medications. Unfortunately, some of these proved less effective, resulting in her symptoms progressing.

Dana’s condition then developed a complication known as stricturing disease or colon stricture, during which the intestines narrow and scar during the healing process. This led to her first colon resection surgery in 2014. Despite trying newer medications called biologics, she faced increasing complications, requiring a visit to Mayo Clinic. There, specialists recommended another biologic similar to her initial successful treatment, but it also failed to deliver the desired results.
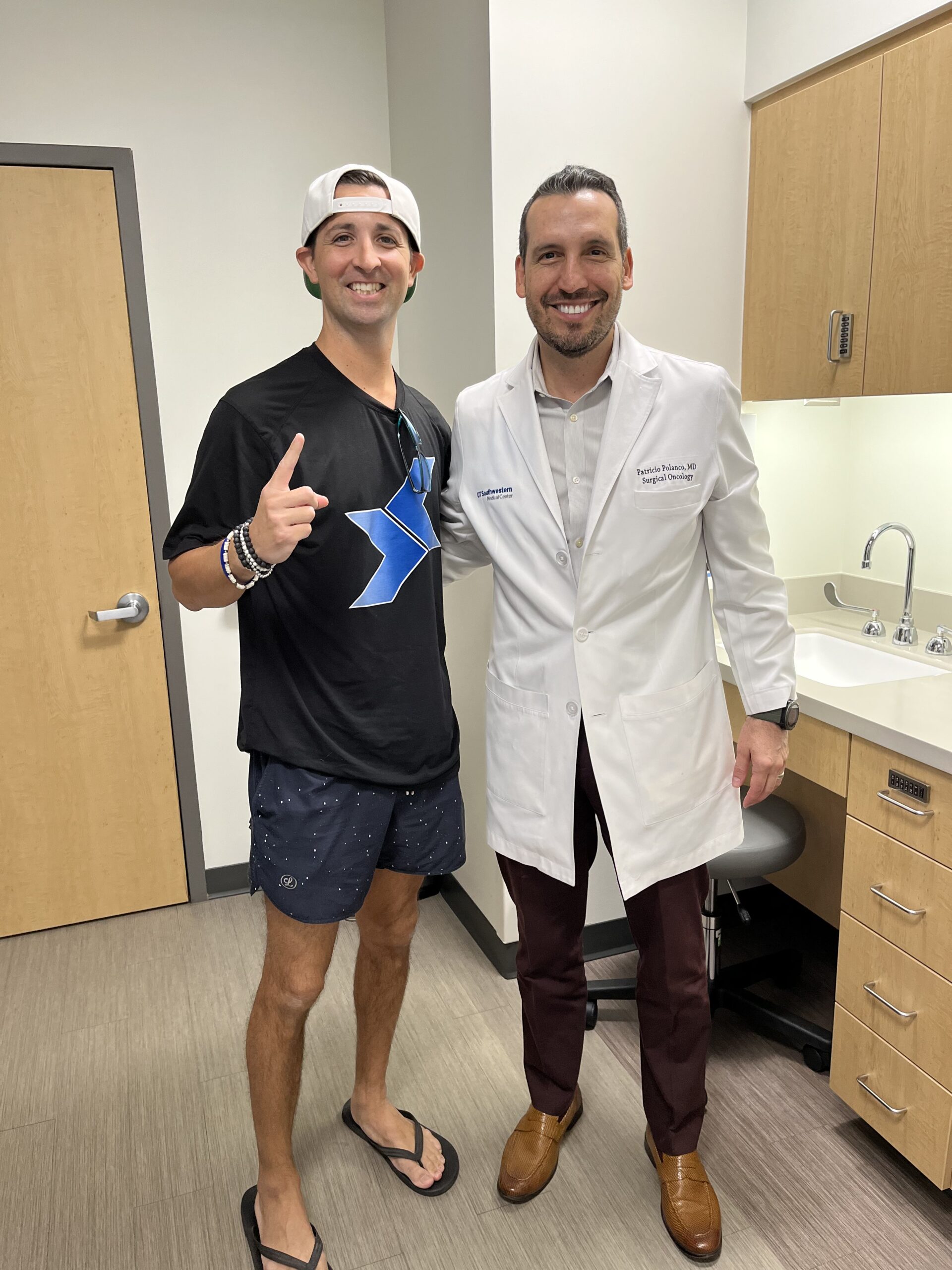
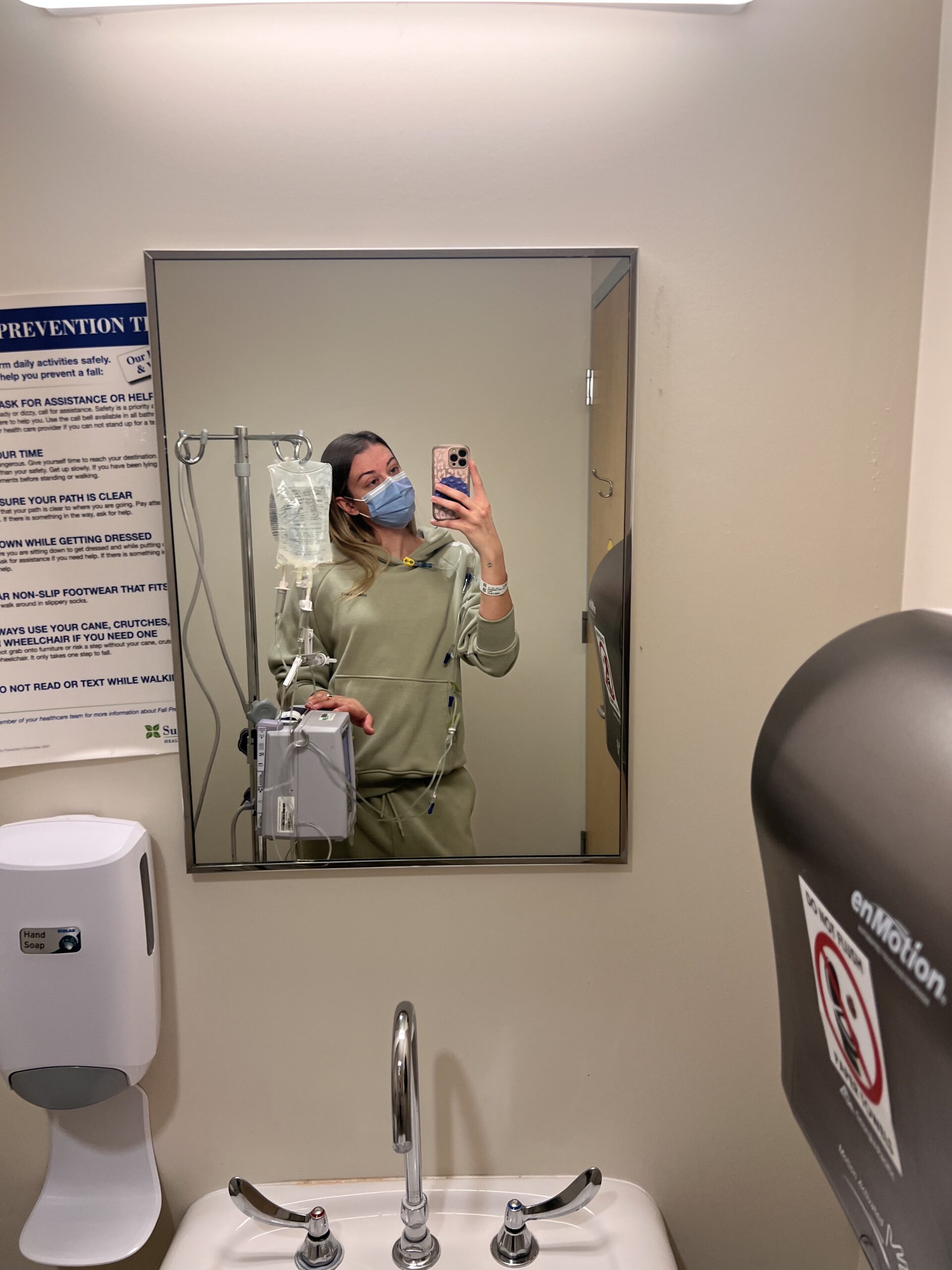
Dana subsequently faced fibrosis and severe narrowing throughout her colon and rectum. Her doctors then decided to perform an ileostomy, removing her entire colon and rectum. This significant surgery, involving a proctocolectomy and reconstruction of her pelvic floor, was daunting but ultimately transformative for Dana. It alleviated years of pain and allowed her to reclaim much of her life. However, adapting to an ostomy accordingly presented new challenges, including managing supplies and preventing leaks while dealing with skin reactions to adhesives.
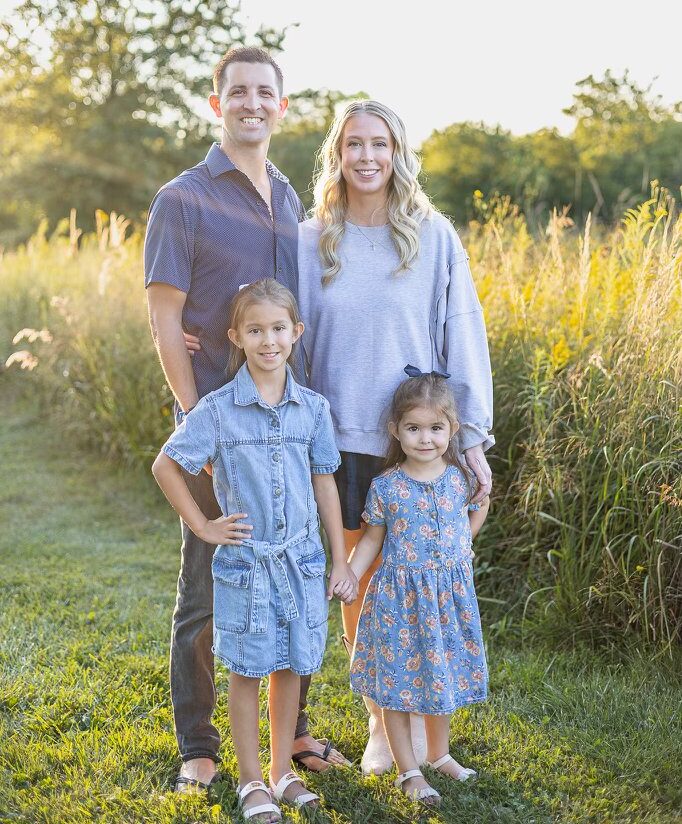
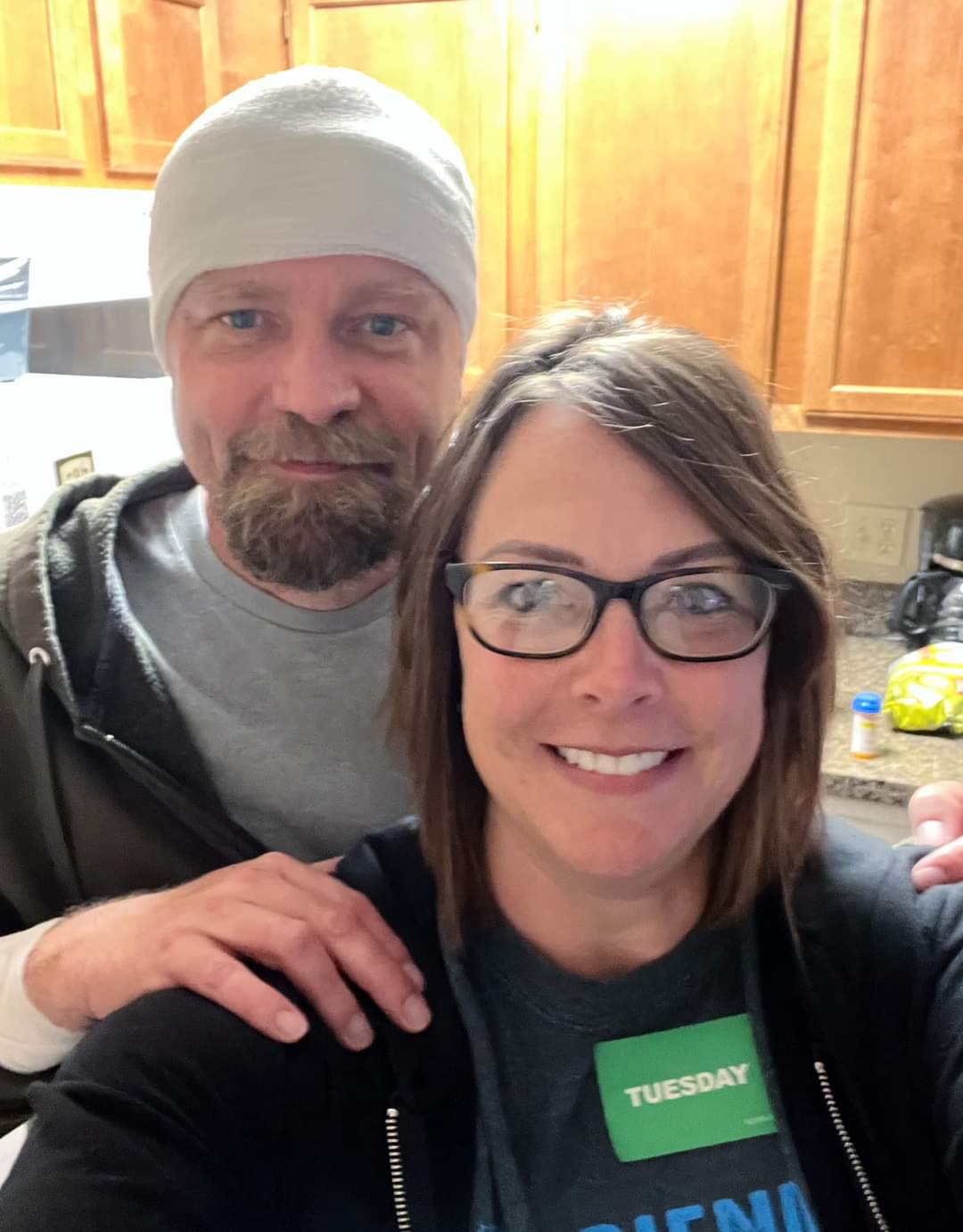
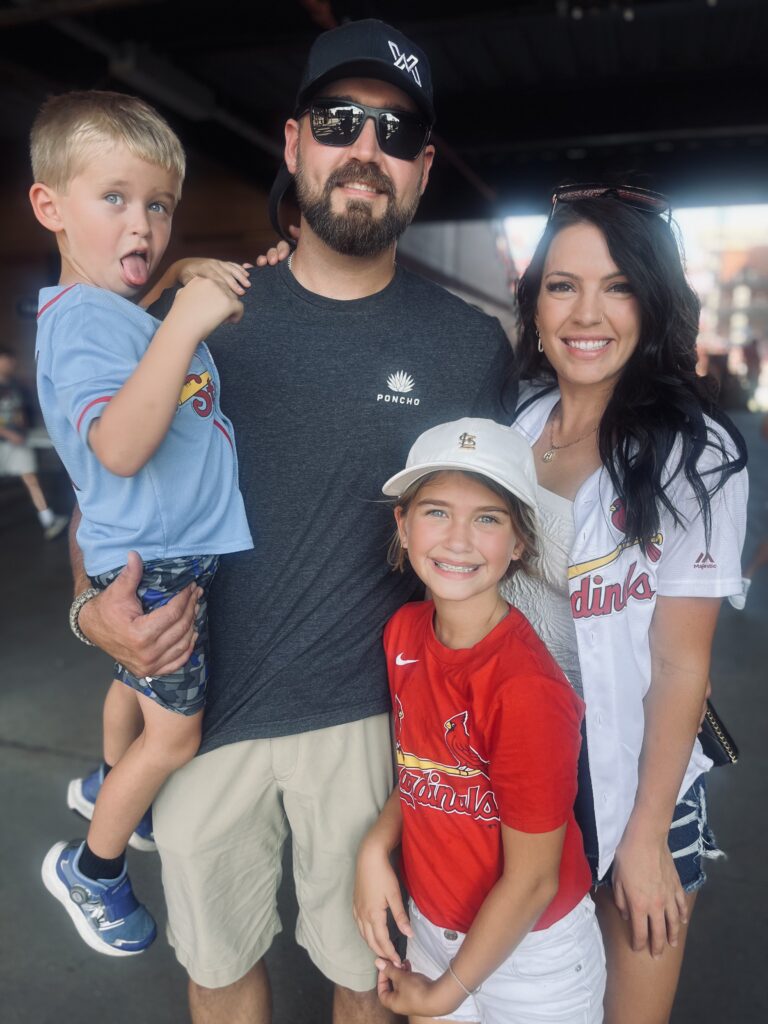
Dana acknowledges the lifelong changes and planning necessitated by Crohn’s disease, impacting spontaneity but ensuring she can continue participating in life fully. She emphasizes the importance of community and support networks, both online and locally, to combat the isolation that can accompany living with a chronic illness. Her relationship with her husband stands as a testament to resilience and ability to adapt, as it has grown stronger through their shared challenges.
Despite the difficulties she has faced, Dana remains hopeful, advocating for a positive mindset and the benefits of connecting with others in similar situations. She encourages those also facing Crohn’s disease and similar conditions to understand that life can continue meaningfully and fully, with even greater appreciation for health and connections.
- Name:
- Dana D.
- Age at Diagnosis:
- 15
- Diagnosis:
- Crohn’s Disease (a type of Inflammatory Bowel Disease or IBD)
- Symptoms:
- Abdominal pain
- Diarrhea
- Blood in stool
- Treatments:
- Surgeries: colon resection, total proctocolectomy with end ileostomy,
abdominal perineal resection, myocutaneous flap - Steroids
- Biologic therapy
- Surgeries: colon resection, total proctocolectomy with end ileostomy,
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Inspired by Dana's story?
Share your story, too!
More Crohn’s and Colitis Stories
No post found