Living With Incurable (Not Terminal) Stage 4 ALK+ Lung Cancer: How Stephanie Redefines Hope
When Stephanie was diagnosed with stage 4 ALK-positive lung cancer at 44, she was a busy mom of two teenage daughters, working full time and spending weekends skiing, traveling, and cheering from the sidelines at club sports. The first signs that something was wrong showed up as a stubborn cough after COVID and repeated “pneumonia” diagnoses. Even as she cycled through antibiotics and inhalers, she kept pushing through work and parenting — until she had a coughing spell violent enough to break a rib, which finally sent her to the emergency room.
Interviewed by: Keshia Rice
Edited by: Chris Sanchez
In the hospital, imaging revealed tumors in multiple parts of her body, and a biopsy confirmed non-small cell lung cancer that had already spread, making the diagnosis stage 4. Stephanie, a lifelong nonsmoker living outside a city, had never imagined that lung cancer could be possible for her. Like many, she had absorbed the stigma that lung cancer is an “old person’s” or “smoker’s” disease. Learning that her cancer was driven by an ALK mutation completely shifted that narrative and opened the door to targeted therapy and a very different kind of long-term experience with cancer.

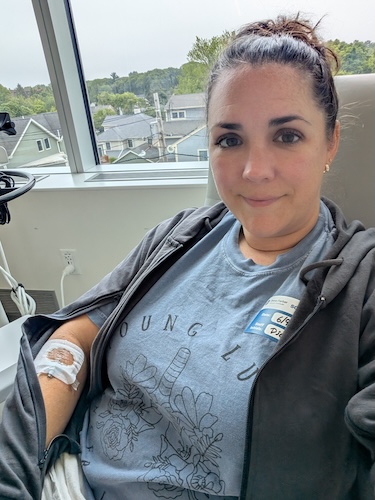
While waiting on genomic testing, Stephanie started chemotherapy. She received the call confirming ALK-positive lung cancer while she was literally in the infusion chair and with an IV already in her arm. Her doctor explained that, in the world of lung cancer, being ALK-positive was considered “good news” because there were effective targeted therapies and active clinical trials. Stephanie chose to enroll in a clinical trial designed to match standard-of-care results with fewer side effects and better protection against brain metastases. She describes that decision as both an act of “paying it forward” and a way to potentially spare herself from harsher side effects.
At home, Stephanie and her husband faced the emotional logistics of sharing the news with their daughters. They first mentioned only that she had lung cancer, intentionally holding off on the stage 4 details until scans began to show real treatment response. Months later, after multiple scans showed shrinking tumors, they sat each daughter down individually to talk about what “incurable but not terminal” would mean for their family.
Today, one year into treatment, Stephanie describes her cancer as a chronic, managed disease, and herself as an advocate who now centers her time and energy on what matters most: her health, her family, and helping other people living with stage 4 ALK-positive lung cancer feel less alone.
Watch Stephanie’s video and browse the edited transcript of her interview to learn more.
- Persistent or changing symptoms like a chronic cough or unexplained pain deserve follow-up and imaging, even when they are initially labeled as “just pneumonia” or a lingering infection
- Lung cancer can affect younger, active nonsmokers; anyone with lungs can develop lung cancer, which is why genomic testing for mutations such as ALK is so important
- Clinical trials and targeted therapies for ALK-positive lung cancer can offer effective treatment options, sometimes with fewer side effects and additional benefits, like better protection against brain metastases
- Asking for help from loved ones, care teams, and communities is not a sign of weakness; it is a powerful form of self-advocacy that can make the experience more manageable for both patients and families
- Stephanie’s transformation includes shifting from a fiercely independent, always-last-on-the-list mom to someone who prioritizes her physical, emotional, and mental health and channels her experience into advocacy and education
- Name: Stephanie K.
- Age at Diagnosis:
- 37
- Diagnosis:
- Non-Small Cell Lung Cancer (NSCLC)
- Staging:
- Stage 4
- Mutation:
- ALK
- Symptoms:
- Persistent, intense cough
- General feeling of sluggishness
- Treatments:
- Chemotherapy
- Targeted therapy through a clinical trial
- Radiation therapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- I'm Stephanie
- My early symptoms: coughing and feeling sluggish
- I was a young nonsmoker: how risk factors were missed
- I confronted lung cancer stigma as a nonsmoker
- Hearing “Stage 4” at 44, and redefining terminal vs. incurable
- Learning about ALK-positive lung cancer and targeted therapy
- I found hope in the ALK-positive lung cancer community
- Telling our teen daughters about lung cancer and the ALK mutation
- Why I chose an ALK-positive lung cancer clinical trial
- Hip radiation, pain, and learning to advocate for my body
- Losing independence: oxygen tanks, mobility issues, and asking for help
- How lung cancer changed my marriage
- Mom guilt, teen sports, and white ribbons
- One year after my stage 4 ALK-positive diagnosis: reflection and advocacy
I’m Stephanie
I’m from Massachusetts, and I was diagnosed with stage four ALK-positive non-small cell lung cancer in December of 2024.
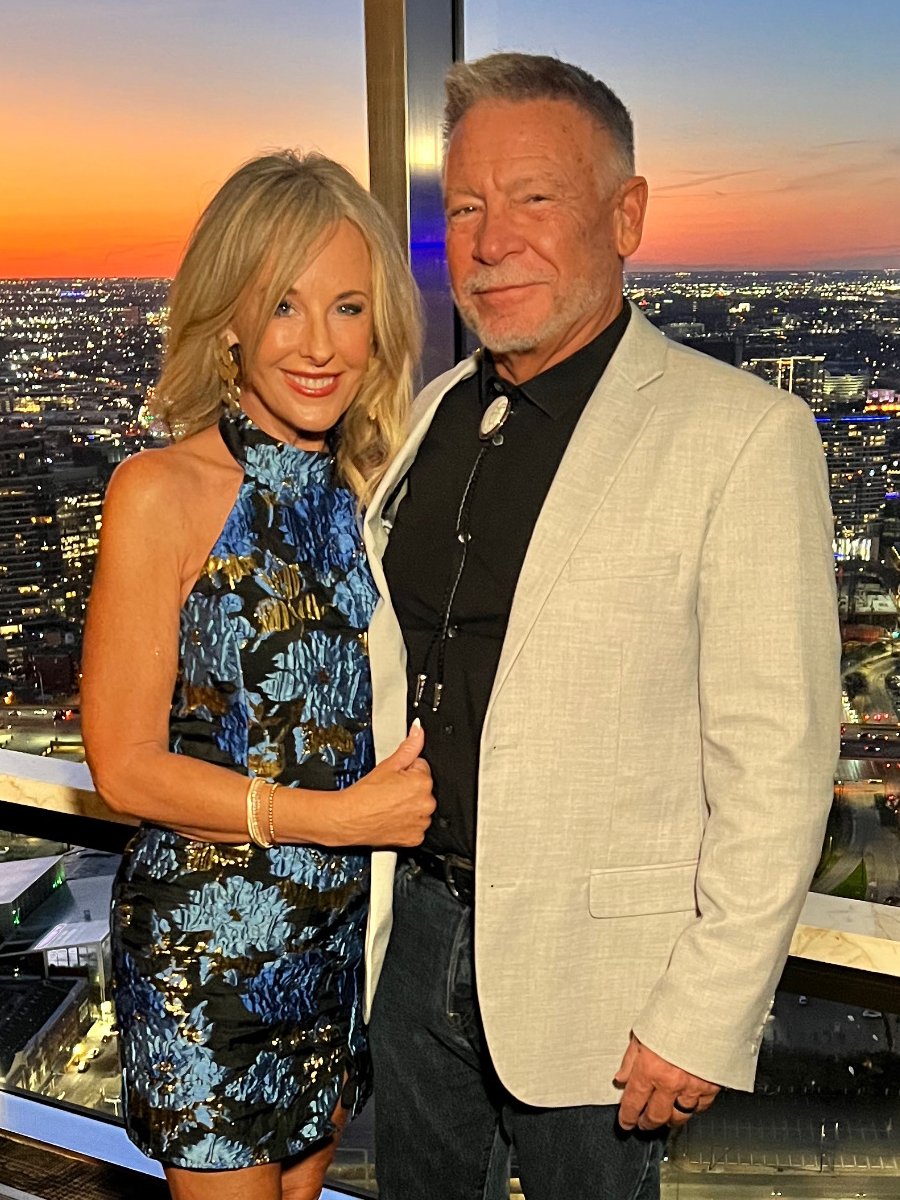
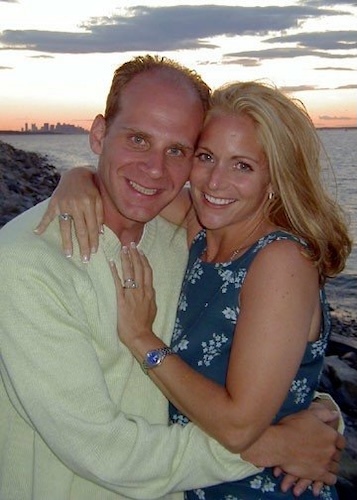
My life before cancer was a life full of hope and fun. I have two teenage daughters, and I’m married to my high school sweetheart, and we have been doing all kinds of great things. We go skiing. We travel. We both work full-time, while the girls are in high school and doing their thing. Right before diagnosis, I was very sick, and we thought I had pneumonia. So the right before diagnosis was a lot of coughing and a lot of inhalers and things like that. But the before life was one of more travel, adventure, activity, things like that.
My early symptoms: coughing and feeling sluggish
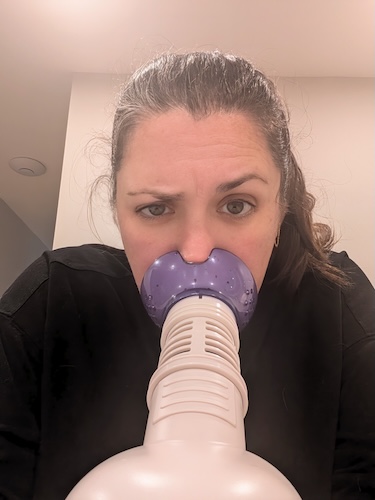
As a mom, we put ourselves last. So when I was sick, I just thought it was a quick cold. I had just gotten over COVID, actually, and then I had a couple of great weeks, and then I started coughing again. So I thought it was just a little residual congestion from having COVID, and it just escalated, and the cough just wouldn’t go away. I didn’t really have other cold symptoms. I had just a terrible, hacking cough. It wouldn’t be resolved with any over-the-counter medication. Using cough drops didn’t help. I used an inhaler, like a steam inhaler, at night for some kind of relief, but nothing was doing the trick.
So I did brush it off for a while and figured, “I’ll just deal with this later because I’m working full-time.” It was a busy time for me at work, and eventually I hit up the urgent care and figured that’s good enough. We’ll just get some kind of antibiotic and move along my way. After a few more weeks with antibiotics, nothing changed. It got worse. I went through more antibiotics and had a chest X-ray. The second time, they said it was pneumonia again, and we had new antibiotics. But again, I was still going to work every day, just going through the cycle of trying to pull yourself together and get everything you need to do done.
It wasn’t until maybe eight weeks later, from my first visit to an urgent care, that I was coughing so hard that I actually broke a rib. I felt it snap as I coughed, and when that happened, the pain was actually what finally sent me to the hospital instead of an urgent care. The pain of that coughing was intense. I wasn’t going to the hospital with the concern of the cough. I was going because I needed pain medication that was stronger than ibuprofen.
When I got there, they took a look at me and were like, “Did you have imaging done recently? Because we think it’s important that we do that again.” The ER doctor came in fairly quickly and decided he was going to admit me, which I thought was strange because, again, I still just thought I had a cold. I had pneumonia. I figured he was just admitting me because of the pain from the broken rib. It was actually a couple of days before I realized he was admitting me for more than pneumonia. I think they danced delicately around what they were testing me for at first, maybe to not scare me.
On my second day in the hospital, when they told me I’d be getting a biopsy the next day, I was like, “Why would I need a biopsy for pneumonia? This is silly.” That was the reality for me of just how I pushed it aside for a long time. I mean, not very long — eight weeks maybe — that I was kind of just pushing it aside as a cold, and then it became real very suddenly for me.
I was a young nonsmoker: how risk factors were missed
Absolutely, my age played a role, especially not having a history of smoking. That really was part of the lack, I think, of pushing quicker to get the diagnosis because I didn’t have your typical risk factors. I live in a pretty wooded area. I’m not in a city, so they weren’t thinking about air pollution. I don’t use a wood-burning or coal-burning stove in my house, so they weren’t thinking about it like that. I don’t smoke, and I was, again, 44 years old and fairly healthy. So we didn’t go there very quickly.
What they saw in my lungs on the X-rays at urgent care looked like pneumonia to them. Without those other risk factors, they really didn’t say, “Well, it could be something else, so we should test just to make sure.” They said, “Hey, it’s the season. It’s September, October, November. People get sick. A lot of pneumonia is going around right now. You’re young, you’re healthy. It’s just that. Let’s treat it.”
I wasn’t diagnosied until that hospitalization. But also very randomly in November, I had a couple of blood clots in my leg. Having the DVT in my leg finally made my PCP say, “Something doesn’t sound right here,” because that shouldn’t be happening. You don’t have any other reasons for that either. She referred me to a pulmonologist and a hematologist, whom I wouldn’t be able to see until February or March because they were booked so far out. Since I didn’t have your typical risk factors, they didn’t see it as urgent.
For me, it was like, “Well, if you think something’s going on and there are some other puzzle pieces, I’m concerned.” I actually did start making calls to see if there was anybody I could meet with earlier. It was probably a two-week span between when she sent me a referral for hematology and when I actually went into the hospital and found out it was, in fact, lung cancer. I certainly wasn’t thinking lung cancer, though. I was more concerned with, like, why do you want me to see a hematologist? For whatever reason, I wanted to get there faster because, whatever you think this might be, I want to tackle it and get a solution in place quickly.
I confronted lung cancer stigma as a nonsmoker
When you tell people you have lung cancer, the first question is, “Do you smoke?” I knew nothing of lung cancer before having it myself. I didn’t have any experience with anybody who’d had it before. I also believed in the stigma of, “It’s a smoker’s or old person’s cancer. It’s not something that you can just get out of the blue.”
I’d never heard of a genomic test for any sort of cancer other than breast cancer and the BRCA gene. That’s the only time I’d ever heard of some kind of cancer test you could get to find out if you have the gene.
When I was first diagnosed in the hospital, I had tumors on each of my ovaries, lesions in my spine, on my liver, and in my lungs. All I knew, though, was my ovaries, because I had a little sensitivity on my side. When they pushed on my stomach, I’d say, “Yeah, it hurts.” When they said I needed to do a biopsy, it was like, “Oh, it’s got to be something on my ovary.“
They came back and said, “It’s cancer.” They just said, “It’s cancer.” I obviously was upset. But then my nurse was like, “Yeah, but if it’s ovarian cancer, that’s a quick and easy thing that we’ll just take out. You don’t want to have children anymore, so we can remove all of the parts that could be affected right now. I promise you, you’re going to be in great hands.” So I had this really different hope that it was just a tumor situation. We’d just remove it; we’re going to be fine.
The following day, I was told that it was actually lung cancer and that they had biopsied my liver. The liver is what showed the lung cancer on the slides. Because I didn’t have the classic risk factors, the concern was that it was probably a genomic defect, a mutation. As we were starting to figure out what this was, the doctor mentioned that there could be these genetic tests that we needed to do, and we needed to button up whether it was just straight-up non-small cell lung cancer or if there was an actual mutation that we were up against, because you treat them differently. I also didn’t know that. In my head, you have cancer, you get chemo. That’s as far as I’d been aware of it.
I was the first person in my family — my parents, my aunts, my uncles, my grandparents — to get cancer. It’s been a very healthy bloodline to date, and I was just shocked at what we’ve learned. I would say that what I learned about, “Every person with lungs can get lung cancer,” was only once I was one of those people, one of those lungs with lung cancer. That’s when I learned it really can be anyone with any risk factor. All you have to do is be breathing, basically, and you have that risk factor.
Hearing “Stage 4” at 44, and redefining terminal vs. incurable
Hearing “stage 4” was terrifying. It was shocking. I think shock was probably the first thing, because I didn’t even know I was that sick. I knew I was sick with a cold. I knew I was sick with pneumonia. But to think you’re going to tell me I have cancer and it’s stage four already — how in the world did I not know? In my mind, you must have cancer for a really long time for it to get to be at stage 4. Unchecked cancer for a really long time, for it to grow.
It was probably a matter of months, to be honest, because I was well in the summertime. To think about the fact that I started coughing in the fall and was diagnosed in early December — that was only a matter of months. It was a horrible shock at 44. When you’re not exposed to cancer with other people you know and your family members, you hear the word “stage 4,” and you immediately go to the word “terminal.” At 44, that’s a really scary thought because you just immediately think, “How long do I have? I am halfway through this existence that I thought I had. How are you telling me I’ve got a limited number of, I don’t know, months? Weeks? What are you even going to tell me?“
The best thing that my doctors did was they never gave me a date. They never said, “You have an expiration date.” When we got to the point of understanding the mutation that I do have, because I’m ALK-positive, there are so many advancements and treatments that I can have, that people are living longer and longer at the stage four level. We’ve changed our language here at my house. We do not use the term “terminal” at all. We say “incurable cancer.”
Even if I get to a point where there is no evidence of disease, I will always have this gene that’s just kind of waiting in the wings to come back out and scare me again. I recognize that I will be on medication for the rest of my life, making it more like a chronic illness. I need to keep that gene at bay. Keeping it under control, making sure it doesn’t come back and come up bigger by taking these medications, makes this something for me that I will never beat. It’s always in my system. I will never beat this cancer. That’s why it’s incurable, but not terminal. Because it’s not a timeline for me. It’s not a deadline. It’s not saying you only have so long to go. It’s just saying we’re going to work really hard to keep you as healthy as possible for as long as possible. It’s incurable, but we can manage this.
Learning about ALK-positive lung cancer and targeted therapy
Because of the timing of when I was diagnosed and how fast it had already gone to so many areas of my body, the doctors felt it would be best to have one round of chemo while I was waiting for the genetic test to come back, because it’s not always guaranteed how fast it’s going to come back for each patient. It was just coming up to Christmas time, so there was also something about not being sure of where that test would end up on a lab bench somewhere, how fast it would get there. We scheduled my first round of chemotherapy for December 23rd last year.
As I was sitting in that chair with my husband across from me, the phone rang, and I ignored it because it was some weird number from Pennsylvania. Then it rang again, and my husband was like, “That’s weird. Come on, why don’t you just pick it up? It’s probably not a telemarketer.” So he picked it up, and it was the doctor who originally diagnosed me at the hospital nearest my house, because we had gone to a cancer center at this point.
The doctor called and said, “I wanted to be the one to tell you your genetic test came back. Have you started your chemo yet?” I was literally in the chair, and the nurse had the medicine right here, ready to go — are we doing this or not? He said, “It’s an ALK mutation, which, in this general area of conversation, is the best possible news I could give you, because there’s so much treatment out there and so much research, and you’re going to be okay in the sense of, you’re not going to need to stay with chemo, which can be very hard on your body. We’re going to be on targeted therapy.”
He told me to go ahead and get that first round of chemo because they wanted to knock it down as much and as fast as they could. “Let’s do one round of chemo today, and then we’re going to see you back in the office in a week after you start to feel a little bit better post-chemo.” The way they explained it to me gave me a lot of hope, and it gave my husband a lot of hope to start to really dig in.
The IV was in my arm. I’m getting the chemo. We’re both on our phones immediately Googling, “What in the world is ALK-positive cancer?” Not knowing anything about this, we were learning about cancer itself, the word “metastasized,” understanding what that even means, what stage 4 means, what ALK-positive means, and what the different types of treatments are. I was getting chemotherapy at that moment and wondering, “What’s the prognosis for the future?” Nobody was telling me, “You have this many years,” or “You have this many months.” Neither of us was ready to Google that. That’s a scary thing to ask, and neither of us wanted to get that answer because you just don’t know what you’re going to see.
I found hope in the ALK-positive lung cancer community
We started to learn there was a great big community out there of ALK-positive patients, and they are so kind. They talk to each other about what’s going on. Sometimes the questions are, “I’m having a hard time with something — has anybody else experienced this?” But a lot of the time, it’s super positive. A lot of people are saying, “Hey, I just hit my anniversary. It’s been this many years since I’ve been diagnosed,” which was incredibly hopeful for me — to think that I could receive a stage 4 diagnosis, and here are people who are years into their stage 4 diagnosis.
It helped us really reframe how we think about it, to think about it as the “incurable” phrasing, because we’re seeing so many other people who are successful in their treatment. Unfortunately, there are a lot of people who are not as successful, and that’s super hard to see. But the majority of what I’m seeing, at least through these communities that I’m a part of now, is just people wanting to help each other, people celebrating the lives that have been through it before, and the treatments that are on the horizon.
There’s a lot of very promising activity in the space of ALK-positive lung cancer.
Telling our teen daughters about lung cancer and the ALK mutation
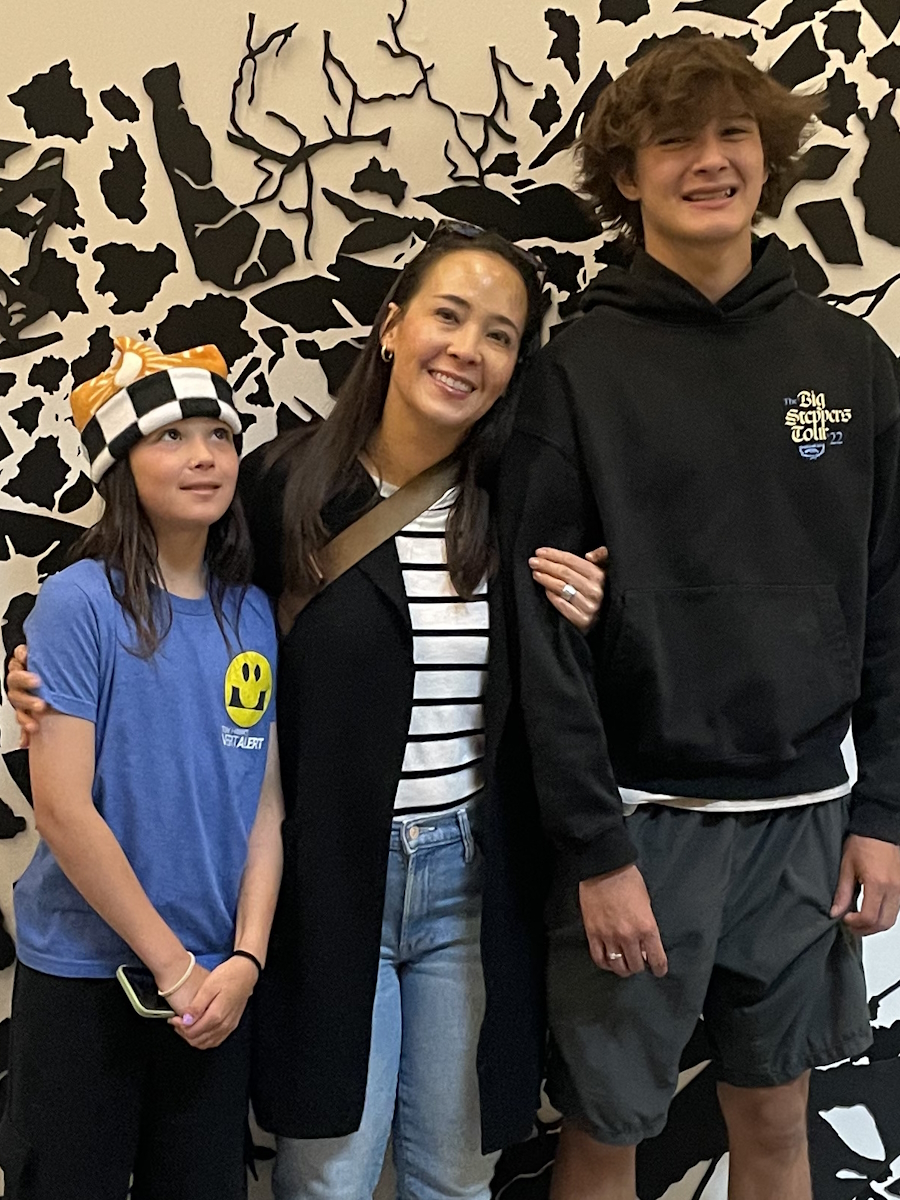
The poor kids. I was in the hospital for a week, so they knew I was sick, but they also knew I had pneumonia. So they thought I was dealing with pneumonia this whole time. It was a Friday that I was discharged. They both had some activities that they had to go to on Saturday that were, believe it or not, fundraising events for childhood cancer at their school that they were helping to run.
I certainly was not telling them before that. We just told them, “Mom’s better. She’s going to be okay. We’re out of the hospital. We have a plan. We’ll talk about this more later. Go have fun at your event, and we’ll talk.” We sat them down the next morning and said, “The reason I was out and what we found was that I do have cancer.” We did not tell them staging. We told them only that it was lung cancer. We didn’t tell them that it had spread anywhere. We told them just enough, I think, to make them feel included in the conversation but not to overwhelm them, because my husband and I didn’t have answers yet either.
When we told them, it was before actually meeting with my now treatment team, my oncology team. We had met with the emergency room oncology team. We didn’t have a plan. We knew we were going to get chemotherapy in a couple of weeks. That was about all we knew. So we told them just enough to let them know, because they were 13 and 15 at the time. We said, “Mom has cancer. It is lung cancer.” They were as baffled as we were. We had to explain that there are different ways people can get lung cancer, and we’re going to learn all about it together, and we’re going to figure out what it means for us as a family.
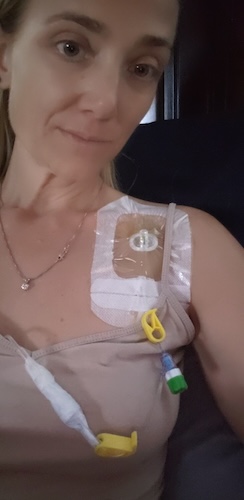
The next couple of weeks, it was a lot of cuddling, a lot of movie watching. I was sent home with an oxygen tank, so the poor kids had to see me with this thing strapped to me all the time. It was scary for them. Absolutely scary. My older daughter is very interested in becoming a nurse, so she was already tracking to be in the healthcare field prior to me being sick. She was in an anatomy and physiology class as well as a biology class that year. I didn’t want to overshare because I didn’t know quite how much she might actually understand and look up on her own, and panic, to be totally honest. So telling them just “lung cancer” without staging was very intentional.
We let them get through the school year. We also let them get through a few rounds of me getting scans, and each time I got scans, it was better and better and better. We decided to wait until the school year ended in June. I had been six months into treatment at that point. We’d all celebrated a couple of rounds where I’d had a reduction in my tumor mass. We sat them each down individually to talk about what it really was, which was the hard part. This was telling them it had actually been in all these different areas and was considered stage four.
We gave them the spiel about “incurable versus terminal.” We told my older daughter first, and she said, “I kind of knew.” She knew it was ALK-positive lung cancer and had started to do her own research, which I knew she would. She started to do a project in her anatomy class around ALK lung cancer, so she was learning a lot about it. What she learned is that one of the first things you see, and I didn’t realize this when we told them it was ALK, is that a majority of patients find out late stage that it’s ALK, because most of those patients don’t have risk factors. They are surprised by their diagnosis because of this mutation. So she sort of knew what was going on but kept it to herself for a while, and she was very strong about it throughout the year.
When we told my younger daughter, she’s a very different person. She’s the artsy, English-major type versus the sciencey type. She said, “Okay, okay, I hear you, and I am just going to believe that it’s going to be okay because I’ve seen you over the last six months, and you went from having a gray face and being on oxygen and looking sick all the time to being who you are today, which is you seem like yourself again. You seem normal. You do what you normally do. We go on our little adventures again, and everything is going to be fine.” So she basically moved on. My older daughter was like, “Okay, I’m going to think more about this and do research, and I’m going to really understand it.”
Since then, they’ve both become part of my little advocacy group because I have advocated for people to understand ALK-positive lung cancer better and to help with funding, because it’s a very unique cancer. We need to make sure that as patients, we’re part of the community that’s driving the research.
So, about testing them. Luckily, this is one of those things where it’s a gene that in me just broke. It just broke on its own and decided to become cancerous. So it’s nothing that they can inherit, nothing that they have a risk factor for — other than being a person with lungs. Thankfully, that’s what we’ve been learning more about and understanding, that it’s very different from the BRCA gene with breast cancer. Anybody can, unfortunately, just have this kind of genomic mutation where it’s not hereditary, but it’s just something in your body that goes awry.
Why I chose an ALK-positive lung cancer clinical trial
When I met with my oncology team the first time, it was overwhelming because there was so much I still didn’t really understand. I didn’t understand what my options were. I didn’t understand what ALK-positive was. I just didn’t know how to feel about it. To go in there and be presented with options, I thought, was really unique. I didn’t realize that would even be the way this conversation would go. I thought it would just be, “Let’s pick your chemotherapy regimen, and we’ll move along.”
When they presented me with the different trial versus standard-of-care options, I think my personality is that I want to pay it forward. I’m a person who wants to be a part of what makes things better for more people, coming up with this. Receiving this diagnosis is not fun, but if I can be part of a medication that makes it better for people, because it has really great effects on the cancer but has fewer side effects than some of its predecessors, I want to be part of that movement. That was part of why I decided to be in the trial.
The other part was very black and white. Part of it is that the drug that’s on market now does A, B, and C, but you’re going to have X, Y, and Z as side effects, and that’s not going to be fun. The clinical trial drug is the same drug that does A, B, and C, but it may have X, and that’s about it. You’re not quite sure; it may have none of those side effects. It felt to me like an obvious choice, almost like, why wouldn’t I take the drug that’s the same as the one on the market, but maybe has fewer problems?
They told me it is just as good as what’s on the market right now. It is not a placebo. It’s not half as effective or anything like that. It is just as good as what’s on the market today, but hopefully better because you won’t have the side effects. So, between wanting to do the right thing to help others coming after me and, selfishly, not wanting the side effects, I thought, let’s go for it. It also came with a third thing: it was hopefully going to block the ability for this cancer to reach into my brain. ALK-positive cancer very frequently travels up into the brain.
This new trial drug helps to block that, or that’s what they hope to find at the end of the trial — that it really does a good job of blocking that brain barrier. That’s what I fear every time I have scans: “Oh God, please tell me it didn’t go all the way up to my brain.” That being one of their selling points, in a sense, was worth being on the clinical trial.
One of the benefits of being on a trial is that my care team felt a lot bigger. There were clinical trial nurses also keeping track of everything I was doing, as well as my standard oncology team. I had more frequent check-ins and scans because of it, and I felt really well cared for in my first year of treatment. Being on that trial meant that I had a dedicated person, on top of my care team, that I could talk to about the drug itself, to say, “Hey, this thing came up. Do you think that’s a side effect worth reporting, or is that just normal stuff?” For me, it felt like a no-brainer.
Hip radiation, pain, and learning to advocate for my body
One of the lesions I have is at the top of my femur, called the femoral head. It’s right in the socket where you walk. That lesion was really bothering me a lot. It could never get rest because it was always being rubbed. I had been complaining of hip pain for a long time, not realizing it was because there was a lesion there. That was one of those things that was in my initial diagnosis, and I just never read that full-length report. I don’t think, at the time, I could have even digested it if I wanted to.
Having hip pain that wasn’t really being helped by any medication, I started to ask more questions about what else could be done, because it was getting to the point where it was unbearable. The doctor mentioned that radiation might help. It might; it may not. It might not work, and it might work. Hopefully, it would zap that one lesion, and it would die or shrink, and maybe it would be easier as I walked.
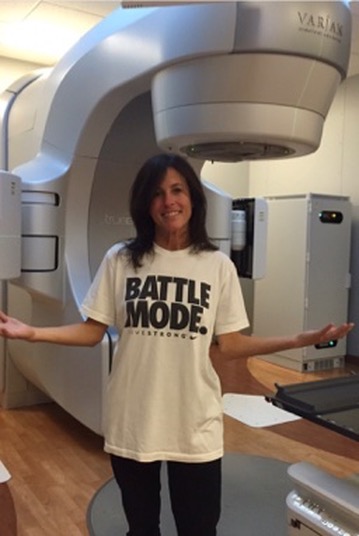
I found the radiation process to be less scary than I imagined. I think I was more scared going into it because I don’t understand radiation. Then it was super easy. I went for five days in a row. Luckily, the center is very close to my house, so it was about a 20-minute ride back and forth. I’d go, and I’d have the same care team every day, the same people to say hello to. They played nice music while I was in there. The lights were dimmed a little bit. It felt comfortable. They made it feel very casual, which was really helpful if you’re going somewhere every day to get this done.
The first time was maybe 20 minutes or so, and it was the longest appointment. The rest were maybe 10 minutes after that. At the end, it was a wait-and-see to see if it worked or not, because it also causes inflammation which can itself cause more pain in that area. It was unclear for about eight weeks if it had actually worked or not. Right after having radiation, I had a spike in pain, which was not typical. I was walking with a cane and called the radiation oncologist to ask if this was normal. I knew there was going to be some pain, but this felt like more than “some pain.” This felt scary, like too much.
Thankfully, she saw me right away, took an X-ray, and looked at everything. They wanted to make sure nothing was fractured, because radiation can also cause some bone brittleness. They confirmed nothing was fractured, so we were just doing the wait-and-see game again to see if maybe that was just more inflammation coming through. For me, I stopped using my leg as much because I was so nervous that maybe it was fractured, and that if I was on it a lot, I was going to suddenly break something, like osteoporosis. I was afraid it was going to just break out from under me.
What I ended up doing was a disservice to myself, because all the muscles and ligaments around it got super tight. My physical therapist mentioned it was like leather: it gets harder, like leather, and it doesn’t move as freely. I caused myself to have less mobility because I was so afraid of hurting myself more. Now I’m at a point where I’m done with my cane. I don’t have the pain as frequently, but it didn’t resolve what I was hoping it was going to resolve when I initially went for radiation.
It’s a very individual thing for every patient, how your body reacts and what it does for you. For me, it was trial and error, and I kind of wish I hadn’t done it. I don’t know if it’s the type of thing where I learned a bit about my body, too. After the fact, I asked for a physical therapy script so I could get moving again, get loose again, and that has helped me a lot. The biggest thing for me is learning how to advocate, because I advocated to do the radiation, but then I also advocated to get physical therapy to loosen myself back up.
Losing independence: oxygen tanks, mobility issues, and asking for help
That loss of independence is tough. It’s really tough to understand that at 44, I was incredibly independent. I was the type of person who, if you went to the grocery store, I’d bring every grocery bag in one haul because I don’t want to go back out and do that. Or if I decide I’m going to move the furniture, I’m just going to do it myself. I don’t want anybody’s help. I was fiercely independent before this diagnosis.
The way it sidelined me was dramatic. I was literally tethered to an oxygen tank for probably four weeks after my discharge. Talk about the opposite of independence. I was dependent on this machine following me around. I was dependent on anybody helping me carry the stupid thing if we went out and about somewhere, because it got heavy and was arduous to have with me. I wasn’t able to drive at the beginning because everybody around me was nervous that something was going to happen, and I wasn’t able to drive myself because of that.
Every time I wanted to go anywhere, it was a huge project because somebody would have to drive me. They were kind to do it, but I didn’t like being dependent on somebody else. I want to be able to just go when I want to go. I had a lot of help. I had a lot of wonderful friends and my family who helped me with everything. If there was an appointment, there were a lot of appointments in the beginning.
My oncologist said at the very beginning that this treatment, especially because it’s a clinical trial, is like a sprint. You’re just going from thing to thing to thing, and over two weeks, you’re going to be in appointments constantly. Then once that’s all done, you turn into marathon mode. You can get into a cadence, and your appointments will normalize. In the beginning, there were so many appointments. My husband also works full-time, so he was trying to juggle his job. I was out on leave from work, focused on my health.
My parents were really kind. They drove me to appointments just to keep me company and to make sure I wasn’t struggling if I needed help with something. It was nice just to have company. It’s nice to be there with somebody who you can talk to or don’t have to talk to, but they’re there, so you feel that comfort.
It was also hard because my daughters play club sports in the winter, and that’s my thing. I enjoy going to these club sports. It’s not a tax on me. I enjoy going. That would make us drive all over tarnation, going to tournaments. We’d be driving two hours away. I couldn’t do that anymore. It was disappointing to have to coordinate a ride for her or ask somebody if they’d be willing to come with us. My husband went to all of them because it’s his daughter, of course. But normally, I would just take off and go with her, and maybe he would meet us there halfway through. It was annoying to me to always have to ask for something, to ask for help. I’m not used to doing that.
Over this past year, I’ve learned it’s okay to ask for help. Nobody’s upset about doing it. People actually want to help; they just don’t know how to. If you’re able to actually ask for the help, then people will happily give you a hand. If they don’t, then those aren’t the people that maybe you need in your close circle at that time. Right now, I just need the people who are going to matter the most when I’m going through the hardest thing I’ve ever gone through. That’s what my circle is to me. They’re the people I would call no matter what.
How lung cancer changed my marriage
It’s weird to say, but I feel like this has been harder on my husband than on me. I think he internalized a lot of this pain, and I quickly tried to move into “What’s next?” mode. I don’t like to wallow in what’s happening. I’m just, what can I do next? How can I get better next? How can I get to the next thing? What’s the next landmark I can get to?
In the very beginning, my husband was emotional. I think he just looked at me and was sad. When you think about your future with someone — we’ve been together since we were 15 years old — to be 44 and still together and in love, it’s hard to look at your future and imagine it not with that person. We haven’t known a life without each other. That’s really hard.
It has probably made us closer, but we were already so close that it’s hard to say we’re closer now. There’s a difference in the kind of respect. I think he sees me as a fighter, and I see him as a fabulous caretaker. Once I started to feel better and feel like myself, we went back into our old roles, which was really nice, but with an extra layer of care. I don’t know that you really get that without having something like this in your family.
You care for each other and your spouse when they’re sick with a cold, but there’s a whole other way of caring for someone when they’re sick with a chronic illness or with cancer. That deepened the love and care between us.
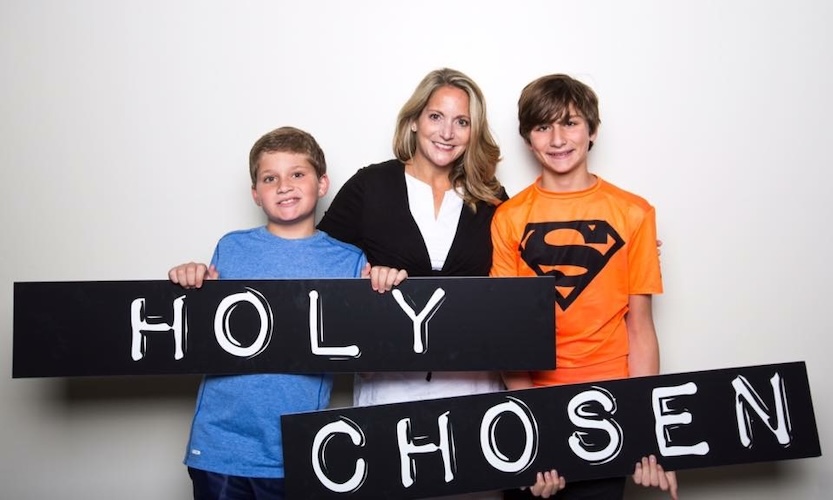
Mom guilt, teen sports, and white ribbons
I’ve never put myself first, and that was a very big wake-up call for me — to put my health, my emotional health, and my mental health at the forefront. Those things all needed attention. I took nine months off work while I was battling my first year. During that time, once I started to feel better, I was prioritizing myself. It was the Stephanie Show. I was going to yoga twice a week. I was grabbing lattes with my friends. Whatever made me feel good and filled my bucket, that’s what I wanted to do.
A lot of what I wanted to do was spend time with my girls. It was amazing to be home for the summer with them. I got to say things like, “Let’s just go run to the beach today because it’s a Tuesday and we can.”
Part of my mom guilt was that I felt guilty in the beginning, which was silly because I couldn’t help it. I felt guilty that my daughter was on a new team. She didn’t really know anybody yet, and her mom was dragging around an oxygen tank to the games. Her mom was the one who maybe couldn’t be social with people, because I didn’t have it in me. I was exhausted, or I had masks on, which made me look very “don’t approach.” I did feel guilty for that.
I felt like, “I hope I’m not alienating her with these new friends because they don’t really understand what we’re going through.” I wasn’t sure if she was telling them what we were going through. I might just look weird to other kids. I had that guilt until she showed me something that makes me emotional even now. She showed me that they had all tied white ribbons to their sneakers, the whole team. The white ribbon is for lung cancer. They all tied white ribbons to their shoes, not even knowing me and barely knowing her.
That let go of that guilt because I realized she wasn’t embarrassed by it. She had told them, and they see me showing up still. So I’m okay. I’m going to be okay. She’s going to be okay, and we’re going to get through this. By the end of her club season, I was great. My tumor burden was down almost 55 percent within those first three or four months. I knew I was on track to become healthy and be myself again. I let go of a lot of that guilt because I recognized quickly that they’re going to be okay. The girls are good. They accept me for who I am, and they understand the diagnosis now. They can explain it to other people, and it doesn’t hold me back from being a good mom for them.
One year after my stage 4 ALK-positive diagnosis: reflection and advocacy
It has helped me prioritize what’s important to me. I actually had my first anniversary this week, and I spent it at the spa because that’s what I wanted to do. Again, I’m prioritizing what makes me feel good and what makes me feel whole. I took a day to relax and reflect, and unplug from work so that I could really focus on myself and my family.
At the one-year mark, I recognized that what’s important to me now is my family and myself, but also advocating. I need people to understand that people do not get cancer maliciously. When people look at you and say, “Oh, it must be because you did A, B, or C,” whatever people think a risk factor you’ve “caused” might be — nobody’s asking for cancer. We need to do a really good job of researching and continuing to advocate for those who are fighting it and for those who are living with the people who are fighting it, because those people need to be heard and seen as well.
My work is in corporate philanthropy, and I have been in that field for about 20 years. Over time, I hadn’t really found my deep connection with one particular nonprofit that I get behind. Mostly because of the kind of work I do, I tend to support whatever I need to in the moment — something I’m running for work or something I’m affiliated with because of work.
Now I am very clearly driven by my own diagnosis. This is something that I work on communicating about. I want people I know to understand ALK-positive cancer, and I want people to understand lung cancer in general, especially in younger people, more and more often. For me, it’s been an eye-opening experience to turn this into something positive. I have a real driven purpose and mission in life about ALK-positive cancer now.
My kids have been great about trying to find ways to affiliate themselves with volunteering and getting involved in things. They support a lot of groups and clubs that have to do with cancer in general. What I’m really excited about is a future where I have more time because of the research being done and the drugs and treatments being manufactured now. They will give me more time with my family and more time to advocate on behalf of those who will eventually find out that they also have ALK-positive lung cancer.
It’s important to me that people who are coming into this and who are young and just starting their families know that they have time with their families. It’s not as terrifying, perhaps, as what we all thought it was when we first got diagnosed. Rather quickly, you learn more about ALK and how you have hope.

Inspired by Stephanie's story?
Share your story, too!
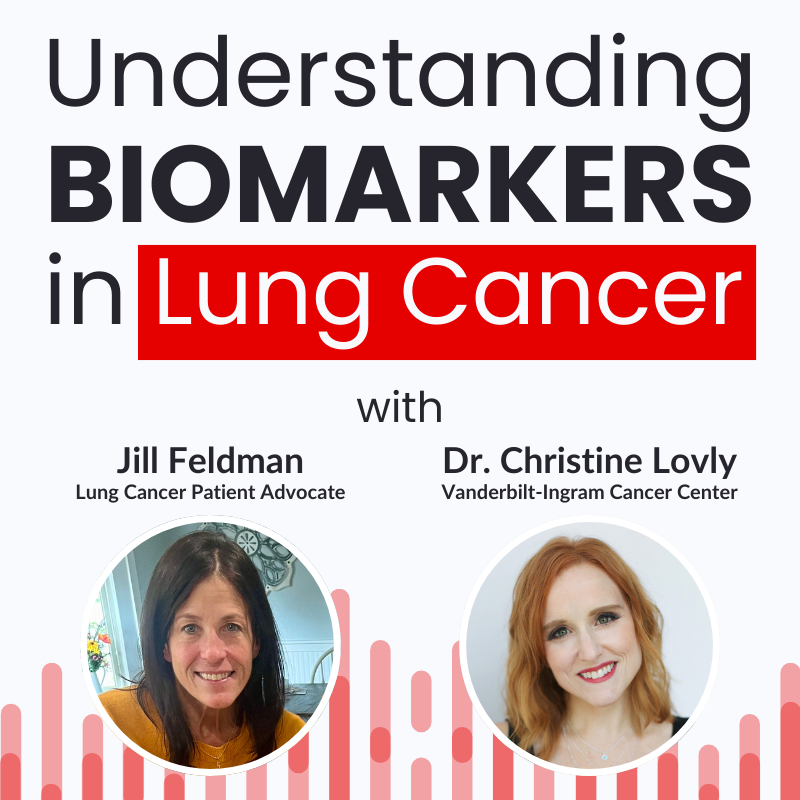
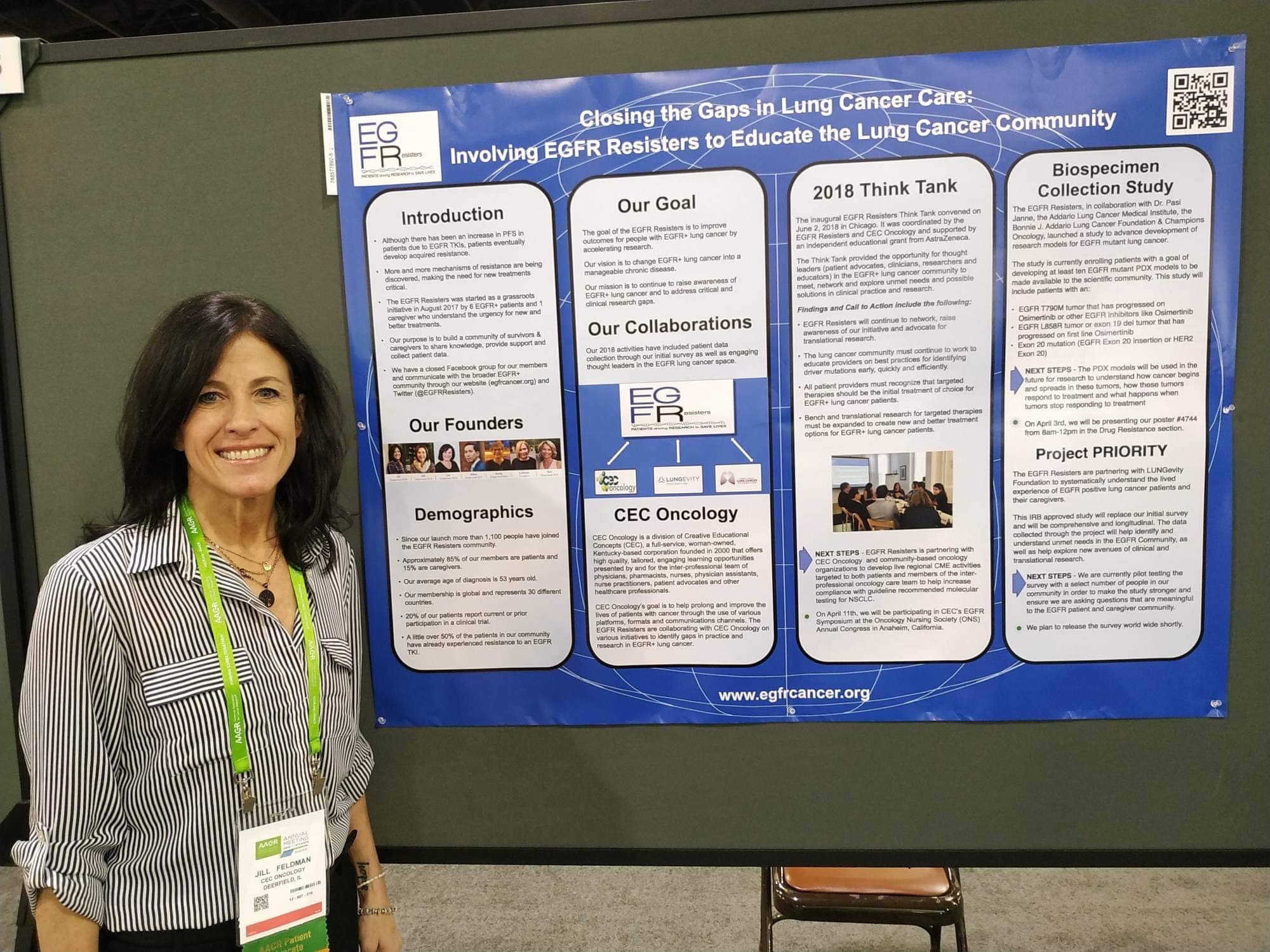
Learn about Lung Cancer Biomarkers
What does “biomarker testing” actually mean in lung cancer? How can it change your treatment options? Jill Feldman and Dr. Christine Lovly explain it in plain language, including tissue vs. blood testing and questions to bring to your next appointment.
More ALK+ Lung Cancer Stories
Stephanie K., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent and intense cough, general feeling of sluggishness
Treatments: Chemotherapy, targeted therapy through a clinical trial, radiation therapy
Ruchira A., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Mild intermittent cough while talking, low-grade fever, severe nonstop cough, coughing up blood, collapsed left lung
Treatments: Surgery (lobectomy), targeted therapy
Laura R., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent cough, fatigue, bone pain
Treatments: Targeted therapies (tyrosine kinase inhibitors or TKIs, including through a clinical trial)
Shauna D., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptom: Persistent dry cough following a cold
Treatments: Targeted therapy (tyrosine kinase inhibitors), radiation therapy
Allison Z., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptom: Severe back pain
Treatments: Targeted therapy (ALK inhibitors), radiation therapy