Living With Stage 4 Stomach Cancer: How Lisa Balances Cancer and Life as a Mother
When Lisa had trouble swallowing a hamburger on her 35th birthday, she had no idea it would be the beginning of a stage 4 stomach cancer experience that would touch every part of her life. What started as difficulty swallowing and severe acid reflux quickly escalated to an endoscopy that revealed two tumors and a biopsy report labeled malignant. In January 2021, at age 35, Lisa was told she had stage 4 stomach cancer, with disease in distant lymph nodes, and suddenly the milestones she imagined, like visits to children’s museums, kindergarten drop-offs, and 10th‑anniversary trips, felt painfully out of reach.
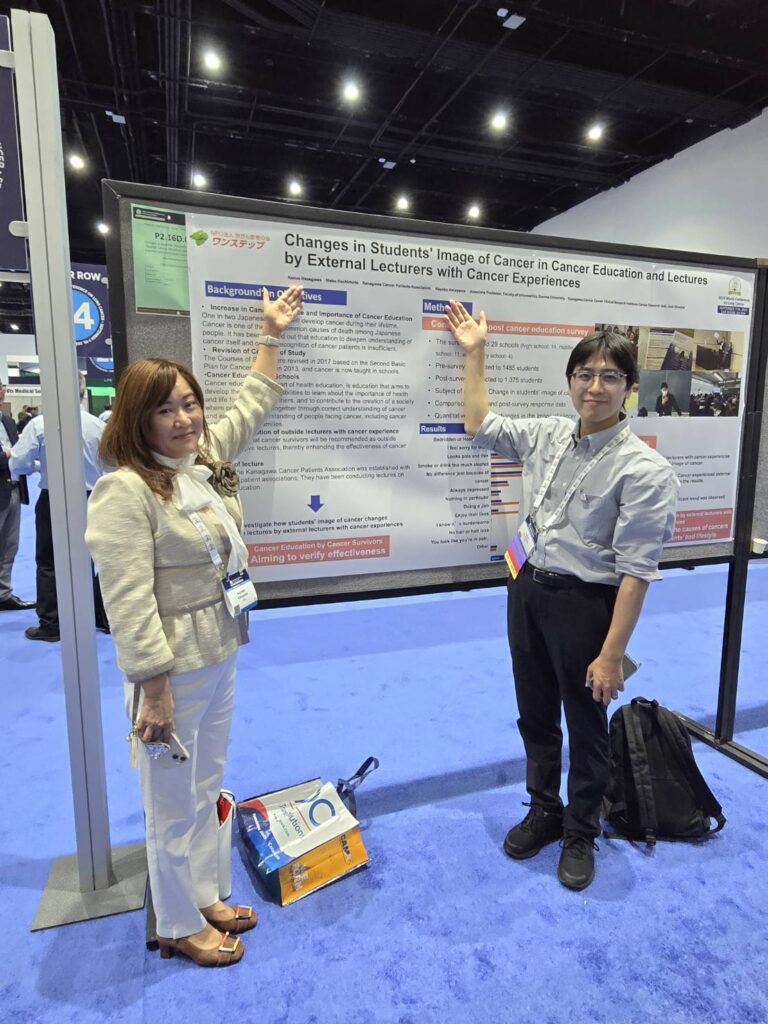
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez
From the start, Lisa trusted her intuition and insisted that something was wrong. With the support of a proactive primary care clinician, a responsive GI specialist, and an oncology team willing to think outside the box, she pursued aggressive stomach cancer treatment: chemotherapy, immunotherapy, radiation, and, eventually, a total gastrectomy. She describes trying to prepare mentally for losing her stomach as “a crazy thing,” especially the moment surgery was initially cancelled just three days before it was supposed to happen, because imaging showed progression. Still, she and her husband weighed the pros and cons and fought to reach the point where stomach removal became possible.

For Lisa, living without a stomach has meant relearning how to eat: tiny, frequent meals and careful pacing, knowing that overeating or too much sugar can bring her to the point that she needs to lie down. Her first year after surgery was especially hard, yet she emphasizes that it is possible to live without a stomach and that she now eats and drinks almost anything in moderation. Maintenance immunotherapy every five weeks, ongoing scans, and Signatera blood tests are part of her “new normal” as she focuses on staying stable rather than chasing the word “cured.”
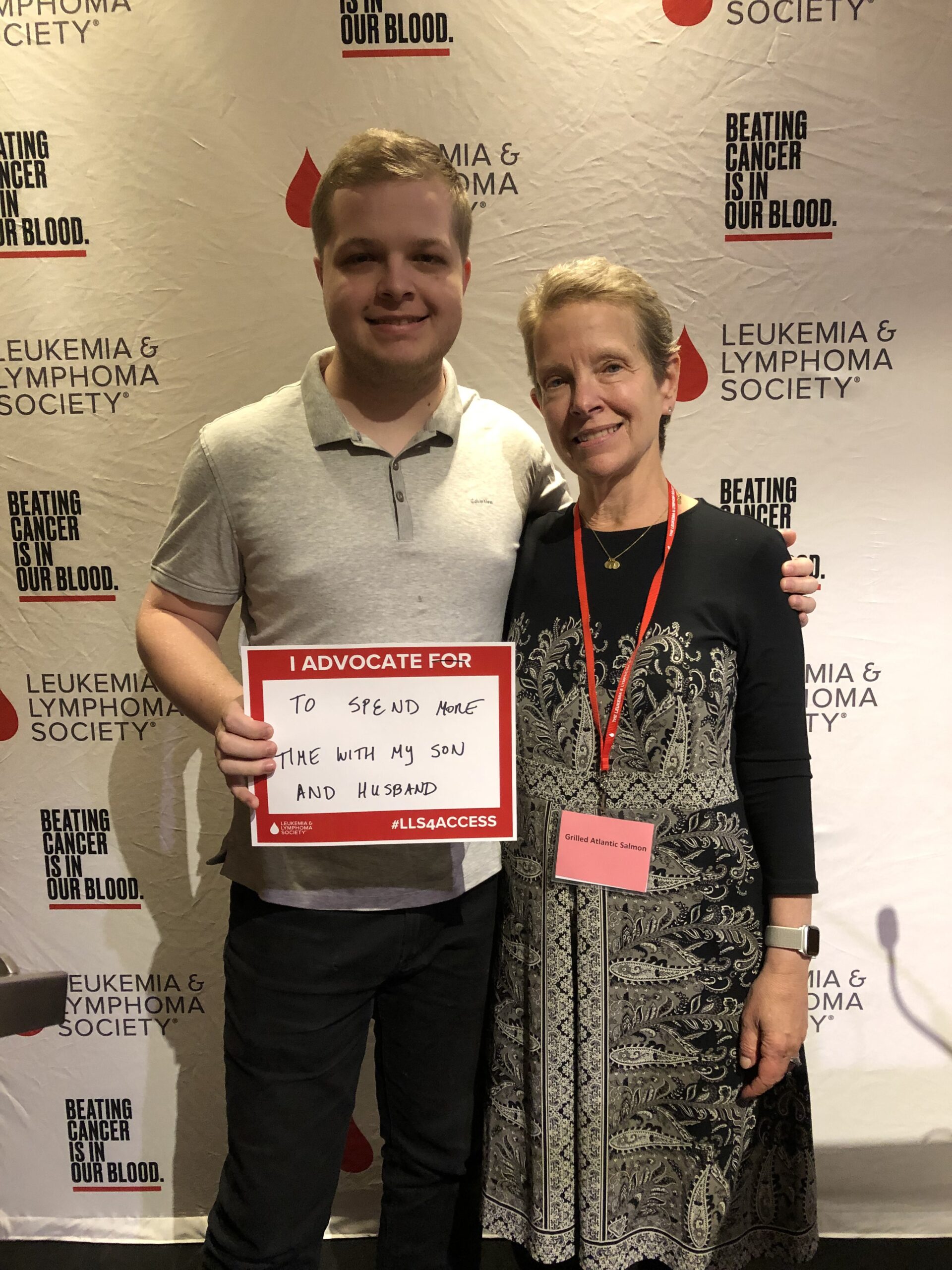
Five years into her stage 4 stomach cancer experience, Lisa has transformed from a terrified young mom who doubted she’d see her son start kindergarten into a powerful advocate. She co‑founded the Strides Against Stomach Cancer Walk in Wisconsin, travels to Capitol Hill for Advocacy Day, and proudly wears periwinkle, the stomach cancer awareness color, with her family. She urges others to trust your body, find your support system, ask for second opinions when needed, and keep living: one milestone, one walk, one day at a time.
Lisa’s video and the transcript of her interview below provide more details about her story.
- Trusting your own body and speaking up when something feels “off” can be lifesaving, especially when early stomach cancer symptoms look like common reflux or indigestion
- Patients deserve to ask questions, get second opinions, and seek care teams that truly listen. No one should feel guilty for advocating for their own health
- Aggressive treatment plans, including total gastrectomy, can sometimes open options even in stage 4 stomach cancer, but they require weighing risks and benefits based on each person’s goals
- Life without a stomach is challenging but possible; with time, support, and trial and error, many people, like Lisa, learn to enjoy food again in smaller portions and more mindful ways
- Lisa’s transformation from “just trying to survive” to leading fundraising walks and traveling to Advocacy Day shows how living with stage 4 stomach cancer can evolve into purpose‑driven advocacy
- Name: Lisa B.
- Age at Diagnosis:
- 35
- Diagnosis:
- Stomach Cancer
- Staging:
- Stage 4
- Symptoms:
- Trouble swallowing
- Acid reflux
- Treatments:
- Chemotherapy
- Immunotherapy
- Surgery: total gastrectomy
- Radiation therapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- I'm Lisa
- Parenting with stage 4 stomach cancer
- My first symptoms
- The endoscopy changed everything
- The importance of advocating for yourself
- Processing the diagnosis as a mom
- What we were told about my prognosis
- How we kept living
- How I balance everything
- What my treatment looked like
- Why we decided on an aggressive treatment
- Preparing for my stomach removal surgery
- Living without a stomach
- Why this surgery mattered even at Stage 4
- Helping people understand my diagnosis
- What I’m currently doing
- Balancing a “normal” life
- How much I’ve learned in these last five years
- Starting the Strides Against Stomach Cancer Walk in Wisconsin
- Why raising awareness matters to me
- What I want others to know
I’m Lisa
I was diagnosed in January 2021 with stage 4 stomach cancer, and I am from Milwaukee, Wisconsin.
A few of my passions: Our family really likes to stay really busy. We really like to travel. We like to see a lot of different new states. We have a state map that we scratch off when we go to a state together, which is really fun, just to help us go to new and exciting places.
We definitely like to travel. We’re the type of people who, when we’re on vacation, we are running. We’re seeing all the sights because we don’t know if we’re going to get back there. We really try to cram in as much stuff as possible. We’re not a huge lounging-around-vacation type of family.
In everyday life, it’s kind of the same thing. My son is seven right now, and we stay very busy with that. He’s really into sports. Then we each have extracurricular activities as well, so just managing all of that. I’m really into reading books and my book club, and just doing a lot of stuff together as a family and with friends.
Parenting with stage 4 stomach cancer
My son was two when I was originally diagnosed, so he’s kind of not known anything else. From the get‑go, a two‑year‑old doesn’t really understand what’s happening, but we really try to be as open as possible with him.
We’ve now done two fundraising walks, and I feel like that’s kind of a nice reminder. Even if I look okay all the time, it’s a reminder that we’re doing this because Mama still has stomach cancer. He knows when I go to the doctor — I go to the doctor about every five weeks at this point. So it’s just kind of a constant reminder of, nope, I still have stomach cancer. I am still sick. I’m still fighting this.
It’s something he’s just grown up with. To him, it’s very common. Also, just funny things: he’ll tell people, “Oh, yeah, my mom doesn’t have a stomach.” People are like, “Wait, what are you talking about?” They think he’s just saying crazy kid stuff, but he knows. He knows a lot of different things about stomach cancer that a seven‑year‑old really shouldn’t have to know.
I think when I was originally diagnosed with stage 4, it was really shocking and not what we expected. We have always been open with our son because we didn’t think we would be here at this point. We thought we’d only have a few years together.
January will be five years since I was diagnosed. We never thought I’d make it there, so I think it was really important from the start that we had to be open with him. We had to share that, just to be realistic.
Every once in a while, he gets really nervous. He’ll just say, “Well, I don’t want to die.” And I’m like, “Oh, honey, you don’t have to worry about that.” I think it has really forced him, as a young child, to have to think about those things.
He’s been really sweet, even through treatment. Every treatment has been kind of different in how it affects me, but there are some days I really can’t get out of bed. I’m just lying there, and he’ll be really sweet and come in. He’ll be like, “Good night, Mama,” and he just knows he needs to be quiet, and I’m not able to help with things and stuff.
So for him to pick up on that is awesome.
My first symptoms
In 2020, I was trying to get healthy, lose weight. I was working out a lot. I was eating healthier. Then it was on my 35th birthday in October 2020. I was eating a hamburger, and I had trouble swallowing it, which I had never experienced before. It got really stuck in my throat, and I was like, “Oh, that’s very weird.”
After that, I had about a week of really bad acid reflux, and I went to the doctor right away because, again, that’s not something I had ever had before. My primary care doctor really jumped on it right away, which was awesome. She got a lot of testing done. I started on Prilosec to try and see if that would help. It did help a little bit, but after two weeks, it still wasn’t back to normal.
I knew what my body normally was, and it wasn’t back to that yet. So we kept pushing for more testing. I did a swallow test. They thought I might have an ulcer. Ultimately, it was New Year’s Eve 2020. I had an endoscopy done.
The endoscopy changed everything
My husband didn’t come in with me or anything because this was in the height of COVID, but they called him and said, “We actually do need you to come in.” Then they told us they found two tumors in my stomach and that they had biopsied those.
It was not the news we were expecting to hear. It was not a routine endoscopy but something way worse than what we thought it would be.
After that, it felt like so long — it felt like weeks — but it was truly, I think, four days. We waited to get a call, and I received a call from the GI doctor that said the biopsies came back and they were malignant, which just kind of shattered us.
We were lucky enough to be working from home at that time because it was during COVID. That was one benefit — that we were there, my husband and I, to get the news together, process it together, have time to step away, which was helpful.
Everything moved really quickly after that: additional testing, meeting with doctors and oncologists, and setting me up for what the next steps were.
The importance of advocating for yourself
I feel like I’ve been really lucky along the way that all of my doctors have really taken anything I’ve said seriously. But I think it comes back to, you know your body the best. I knew this was something that was not right, because they easily could have brushed this off and just said, “Oh, that’s just getting older. That’s just being a woman.”
I knew it wasn’t that because I had never experienced it before. I was very lucky to have doctors who really did support me along the way. My primary care doctor and even my GI doctor really got me hooked up with an oncologist right away because it’s a scary thing, getting a cancer diagnosis. We wanted to jump on it.
He suggested one person. It really wasn’t a right fit for me. I did find a different oncologist. But even his saying, “I know someone who can get you in right away,” was very helpful from the start, and I’ve been really blessed with my care team at the cancer center I go to.
They have been so forward‑thinking the entire time because I was young. I was 35 when I was diagnosed. Basically, they were like, “You’re young and otherwise healthy. What can we do that’s maybe outside the box and give you the greatest chance?”
Processing the diagnosis as a mom
That’s definitely the toughest part — thinking back to the beginning and looking through old pictures. It reminds you because it becomes your new norm, just living with cancer. Looking back at pictures, I’m like, “Oh, wow, he was so young.”
The biggest thing we always laugh about is that I always said, “I’m never even going to be able to take my son to a children’s museum.” This was January 2021. Things were starting to open back up, but very slowly. Then we got hit with this diagnosis, and we didn’t want to put me at risk either. So I was like, “I’m never going to experience going to a children’s museum, going on vacation, seeing him get into kindergarten” — things like that.
So it was really tough from the start.
What we were told about my prognosis
They actually didn’t put a number on it. On the back end, my husband and I were definitely looking at statistics. Back in the day, five years ago, for stage 4, it was only about 4%. That has changed since then, but seeing that number, we could read that ourselves: okay, this is not a good chance.
Basically, they said, “You need to be prepared, but also don’t stop living either. There are a lot of different treatments out there and different things we can try.”
Research is always changing, which I feel I’ve really benefited from in the last five years. Things have advanced so much that I’ve been lucky to be able to do some of those treatments.
How we kept living
We did it in all the ways that we could, for sure. We try to — even now, whenever I’m feeling good, which is more often than not now compared to when I started. Whenever I’d be feeling up to it, we were always trying to do things together as a family, going to different things.
It’s nice that COVID kind of went away, and we could go and do more things. I was able to go to the children’s museum with my son. One of the big things when my husband and I got married was that we always wanted to go to Hawaii for our 10th anniversary. That was almost three years ago now, two and a half years ago, and we were able to do that.
When I was diagnosed, we never thought there was any way we’d be able to do that. We’ve gone on a family Disney trip. We’ve traveled all over and gotten to see a lot of great milestones with friends and family that we never thought would be possible.
We don’t stop, for sure. We are living it up as much as we possibly can because we truly don’t know. Things can change in an instant. A treatment can stop working, and I might be running out of options. We take that wholeheartedly, and we try and make the most of it.
How I balance everything
I rarely sleep. I feel like we were always a couple that burned it at both ends. Especially when we had our son, we wanted time after he went to bed to do things together or watch TV, play video games — things like that. That really has not changed.
We push it at both ends to get the most out of the time we have together, for sure. It’s still not enough time in the day. It’s very hard to balance.
I work full-time. My husband works full-time. Our son is in every sport imaginable, so we’re always running between something. Somehow, we just make it work, and we prioritize the things that are really important to us.
What my treatment looked like
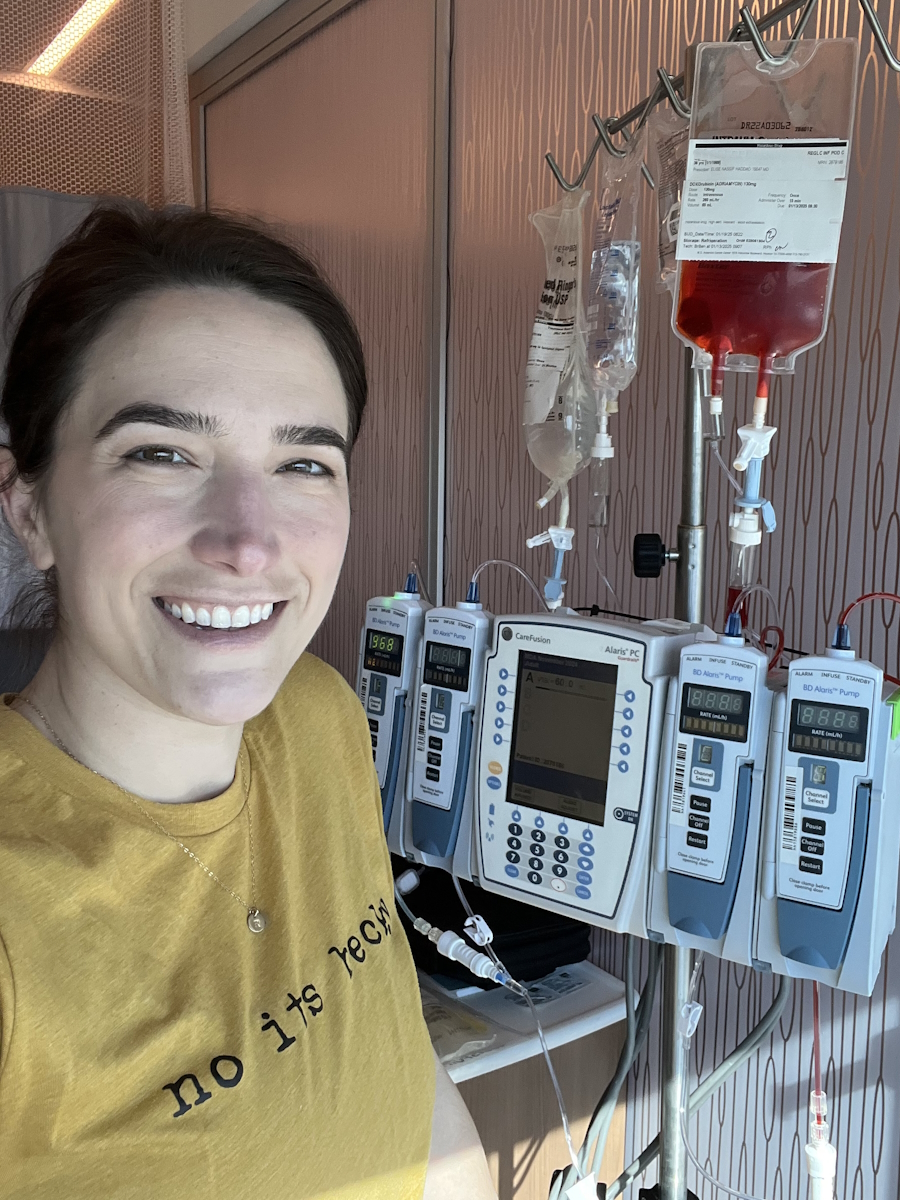
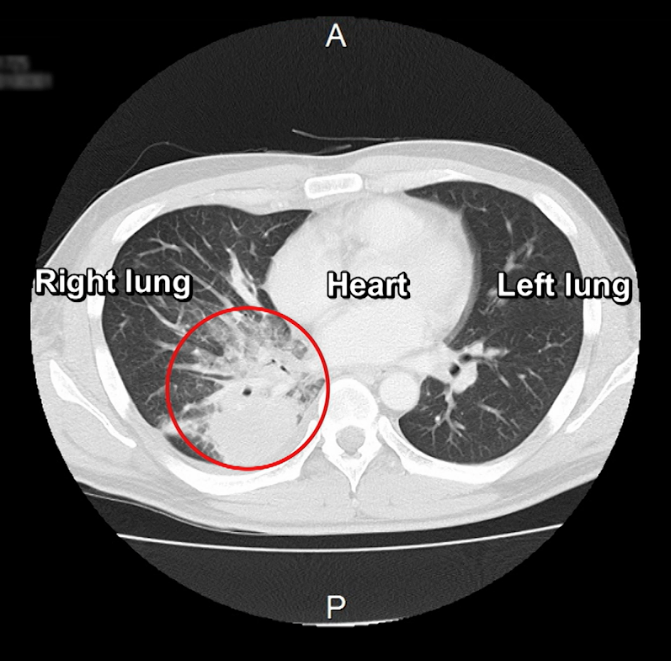
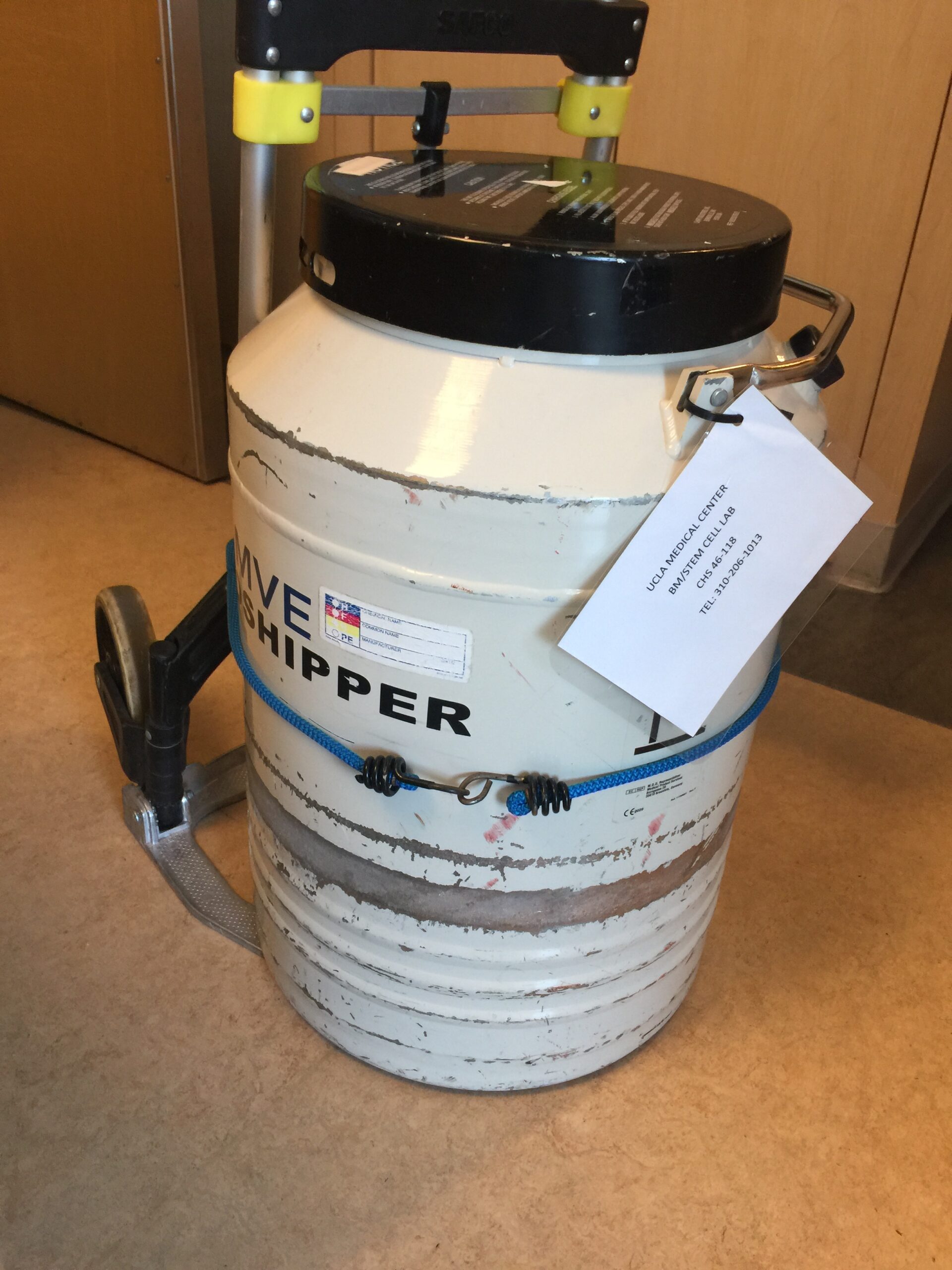
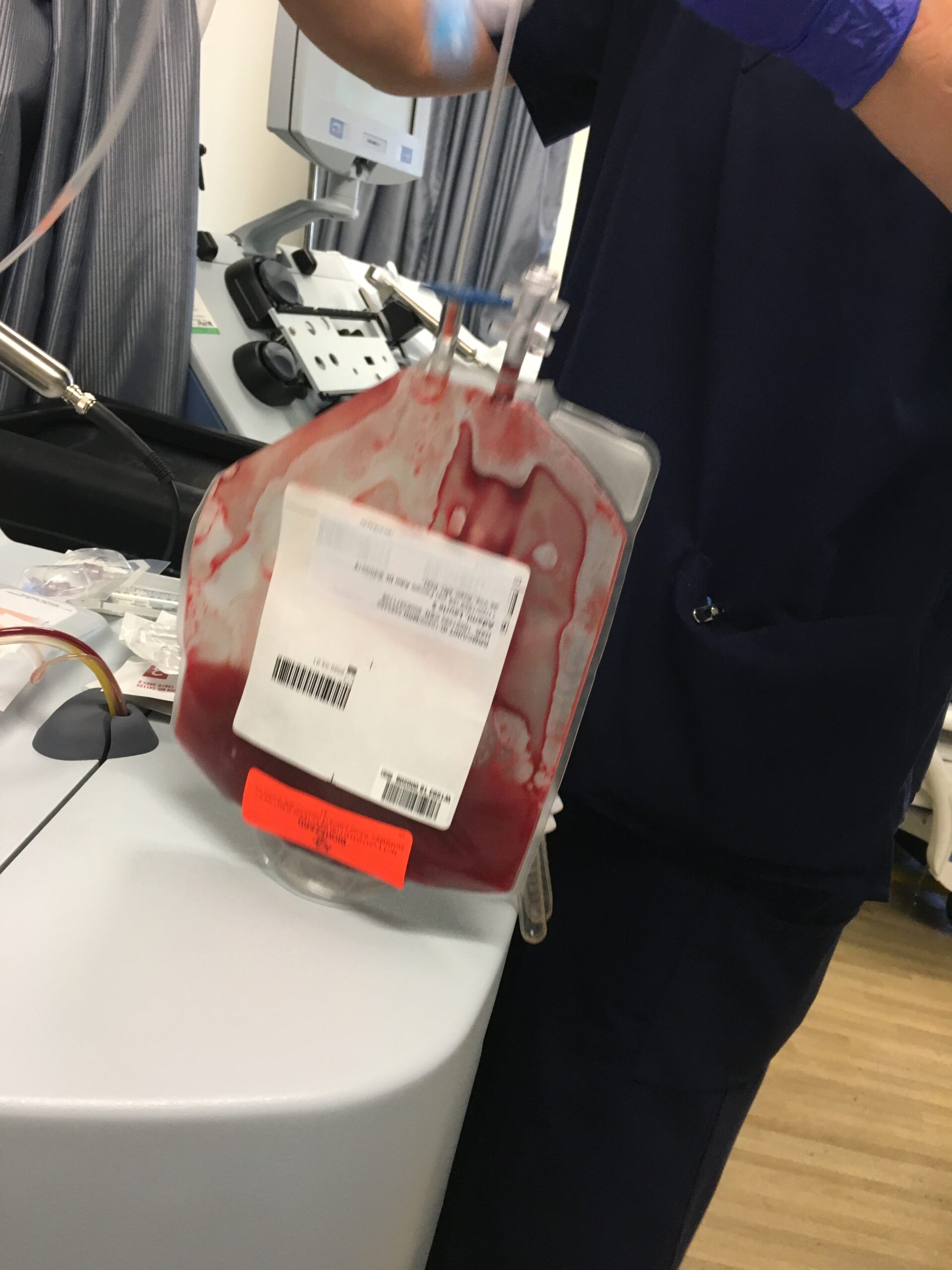
When I was first diagnosed, they found out that I also had a pulmonary embolism, and I was anemic right from the start. To start my treatment journey, I got my port placed really quickly. I received a blood transfusion. I received an iron transfusion. Then I started on a three‑drug chemo.
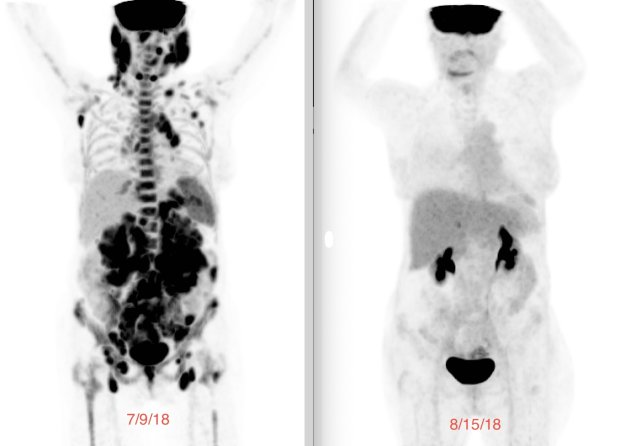
I did nine rounds of that. Our ultimate goal, even though I was stage 4, was to get a total gastrectomy, because my oncologist thought it would give me the best chance. After nine rounds, I had a great response. Everything was going well.
Then I did a CT scan or PET scan right before, and it showed that the cancer had progressed because we had to take a break from chemo. It was three days before my total gastrectomy surgery, and they had to cancel it, which was honestly one of the most difficult things.
Trying to prepare yourself to get a total gastrectomy is a crazy thing, because I didn’t know you could live without a stomach. I was getting excited, like, “This is going to be really good for me to survive.” Then, for that to be taken off the table was really tough. That was about July 2021. They said, “Okay, we’re taking that off the table for now.”
We started back on a two‑drug chemo with immunotherapy as well. They saw really great success with that. I did eight additional rounds. In November 2021, I was able to get my stomach removed because I had a really good response. That was in November.
After that, I started just immunotherapy, which I was on for about a year and a half. That treatment was keeping me stable. I was never cancer‑free, but I was always looking to stay stable. That worked for a long time.
I had to get off of that and took a little break. I did a full course of radiation to the abdominal area because they saw a few things they didn’t like cancer‑wise. I did a full course of radiation. Then I think it was the current treatment I’m on now.
Just before Thanksgiving, I received my 19th round of a new immunotherapy. It’s different from the one I was originally on, and that has been keeping me stable for almost two years now, which has been going really well.
Why we decided on an aggressive treatment
Yeah, it’s kind of funny because I feel like sometimes I can just name off, “Oh, yeah, I did chemo and immunotherapy and radiation,” and it kind of loses how actually crazy that is and how many rounds I did. It has become common knowledge to me now. It is crazy when I name off all the things I’ve been through.
It was really important to me from the start to have an oncology team that was in my corner and really wanted me to get the best results possible. A lot of stage 4 stomach cancer patients are not able to get their stomach removed because it has already spread, and it’s just not possible.
I’m stage 4 because it spread to my distant lymph nodes. Their thought process was: let’s get the majority of the cancer out that’s in that stomach/abdomen region, and then work on treating those distant lymph nodes. You can’t really go in and hunt and peck and take out all of the lymph nodes because, one, they’re all over your body, and lymph nodes fluctuate even for normal people when they’re sick. That’s not possible either.
So the plan from the start was to keep those in check. My husband and I were all for it. We wanted to give me the best chance possible.
I think the hardest thing to come to terms with was the total gastrectomy. It’s such a shocking thing. You don’t know: is this going to work for me? It’s a huge surgery, a big recovery. Maybe it knocks me down too much, and I’m not able to recover enough to receive treatment after that.
But the pros outweighed the cons when we were looking at it, and that’s why we really were trying to push for that as well.
Preparing for my stomach removal surgery
The biggest way I prepared for my total gastrectomy was connecting with other people who had gone through this. I’ve been lucky enough to connect with a lot of people through a few advocacy groups. I needed to know: What did you bring to the hospital? What do I need to bring? What do I need to prepare for? How is this going to go while I’m in the hospital? What tactical things are going to happen?
I’m such a planner, and I needed that. I talked with a lot of different people and got great feedback. They were like, “Here’s a list of things to try,” like slowly eating afterward and what worked for them.
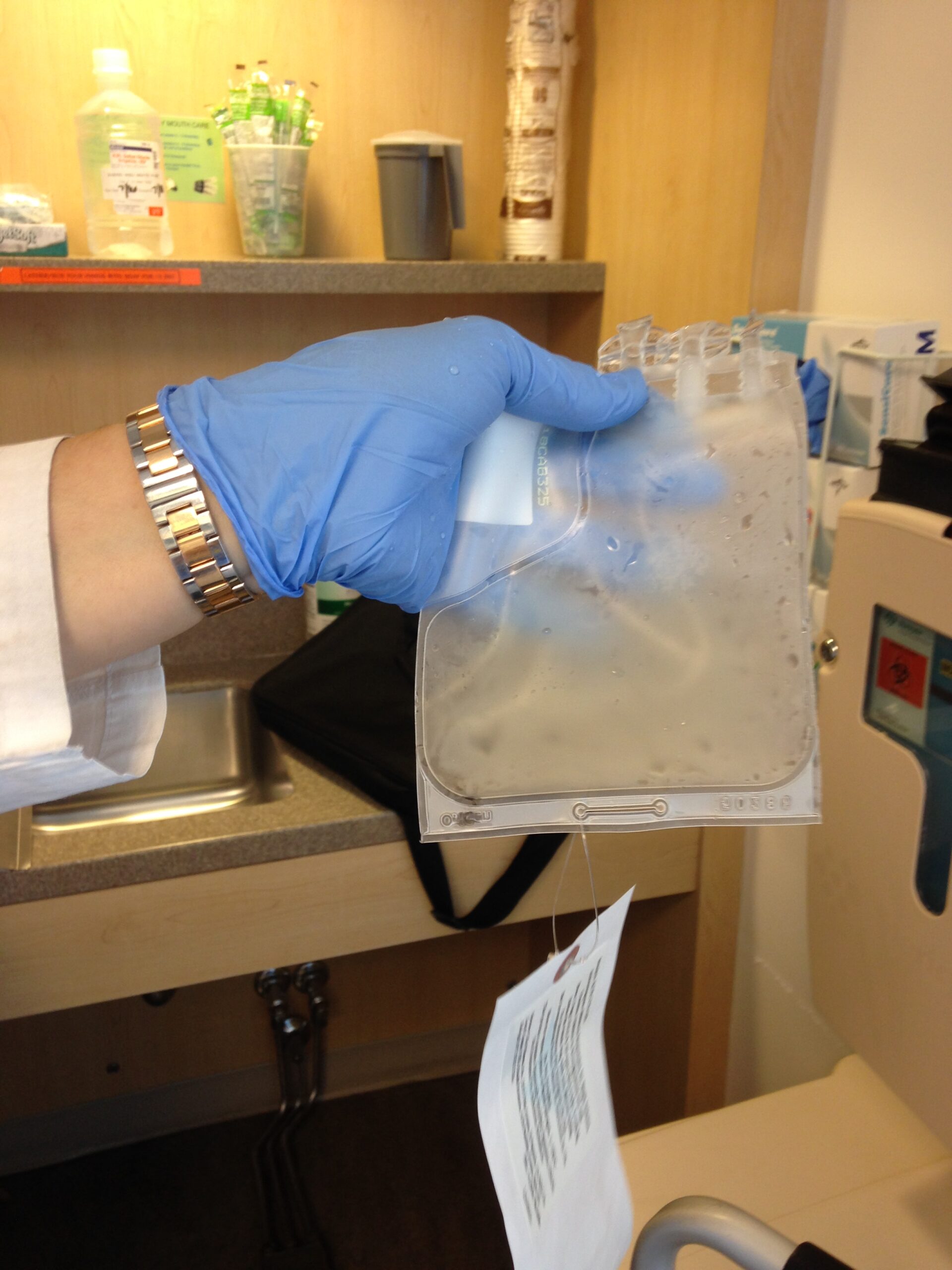
Right afterward, I received a feeding tube when I got my total gastrectomy done. Some patients do, some don’t. While I hated having it every single minute, it was a really nice safety net, just in case I wasn’t eating enough. The sheer volume of calories I could consume was so much less.
I had to constantly be eating, like every hour — “Okay, I’ve got to take two bites of yogurt, and I’ve got to drink my protein water,” things like that. So again, while I hated my feeding tube because it was such an annoyance, it was a really nice safety net to ease me back into it and not have me push it and maybe have complications.
Living without a stomach
The easiest way is that they cut out your stomach, and your esophagus is basically attached to your intestines. I really just don’t have that pouch where your food digests and sits for a bit. Things move more quickly through me, and I don’t absorb nutrients the same way. There are additional supplements you have to take when you don’t have a stomach.
Honestly, for me, the first year was really tough — learning to eat again and the amount. For me, going out and having food with friends has always been a big part of my life. I’ll go out and start eating and talking and forget about it, and then I overeat. It was something I probably did before, too, but now it’s even worse when I don’t have room for that. I know right away: “Oh, I really did push it.” Then I kind of have to go take a break or lie down a little bit, which is difficult.
It is possible to live without a stomach, which, again, I didn’t know before this whole experience. That first year was really tough, but now I’m really back to, I can eat and drink anything I want in moderation, I would say. Sugar is probably the number one thing that’s really hard on a lot of people. I love sweets, so I try and push it sometimes, but I know sometimes I’m going to have to pay the price for that.
Everything in moderation, just like everyone else, but just a little bit smaller.
Why this surgery mattered even at Stage 4
It was really big because, as I said, a lot of stage 4 stomach cancer patients are not able to get their stomachs removed. For me to have this opportunity felt like something I really needed to try and get to.
We didn’t know if it was going to work, if there would be complications, or if the recovery would be too hard and my body would be too weak to receive treatment after that.
We didn’t know those things, but we took an educated chance and weighed our pros and cons to determine that this was really the right decision.
Helping people understand my diagnosis
I think at the beginning, there was so much support around my diagnosis and helping with things. After a while, people kind of forget. They just assume that you look great and you’re doing well, and they assume you’re cancer‑free, which is something I deal with all the time.
Especially in my job, new people will start, and you never know the right time to drop that bomb on people because it’s not the first thing I want them to know. There were people I had worked with for quite some time, and this past November, I stood up in front of everyone to let them know I had this walk happening and that I was a stage 4 stomach cancer patient. Some people were shocked. They were like, “I had no clue, and I work with you daily. I don’t understand.”
I think it’s encouraging and good that people don’t notice it, but also, you want people to understand that it is still a hardship, and going through treatment is really tough. I’m lucky I don’t have a ton of side effects, but I honestly probably have more side effects from not having a stomach — overeating, not eating enough, eating too fast — things that will put me down for the count.
It’s hard when people don’t realize it’s a daily thing. There’s not one day that goes by that I don’t remember I have stage 4 stomach cancer because of some random symptom or pain that rears its ugly head.
What I’m currently doing
I’m on immunotherapy right now, and I go every five weeks to receive that, which is nice. It’s not very disruptive to my schedule. It’s just one Wednesday every five weeks, and then I’m back to work the next day, which is great. I’m pretty lucky that I don’t have a lot of side effects at this point, and the ones I do have are really manageable.
It’s a full day that I spend at the cancer center. I go in, I get labs. They check all of my levels to make sure it’s okay for me to receive this treatment. It’s a good double check to see where things are. I go to that, I meet with the doctor, and he reviews everything. If there’s a CT scan — I get those every three months — we talk through anything new that popped up.
I also get a Signatera test, just to see where my levels are. A lot of people get Signatera, and they want their number to be zero. Mine has never been zero because I’ve always had cancer in my body, but we make sure it’s still a lower number. If that number starts to spike, we want to jump on it.
I’m lucky that I have a port, thank goodness, because my veins are so tired and small from being poked so many times. I got a port right away when I was diagnosed. This is actually my second port; I had to get it changed out. I go to the hospital and receive immunotherapy for over an hour. It’s pretty short, the treatment itself. Then I’m pretty much back to normal after that. You would never know that I received treatment that day.
I’m currently on maintenance immunotherapy. Our goal is really just to keep me stable for as long as possible. I’ll continue to do that until either the side effects don’t work for me or the cancer progresses and we need to look at other options.
Balancing a “normal” life
There’s not a lot of balance when you’re a mom, for sure. I’ve got to jump back in, and I need to parent right away — picking up my son, doing bedtime, doing laundry, doing the dishes, doing all those things. It never stops.
It gets exhausting, for sure. My husband and I would agree: our house is never in the state that we once would want it to be and have always wanted it to be. But it’s the trade‑offs. You do have to have balance, and the dishes can wait till tomorrow, and my house can look messy for a day, and it’s fine.
Sometimes it gets a little too overwhelming. Between treatment and family life and work and everything, sometimes it’s too much. We’ve kind of — as much as we don’t like it — said, “You know what? The house can wait, or that other thing can wait, and it’s fine.”
How much I’ve learned in these last five years
Oh, I’ve learned so much over the last five years. It’s crazy. So much about cancer in general — just all the jargon and language you need to learn when you’re in the cancer world — has been a lot.
Also, I had so many mentors when I first started this experience, looking to them as inspirational stories because I thought there was no way I was going to get through this. Talking to some of those people, who have become some of my closest friends, was so inspiring. I was like, “Well, they can do it. They live without a stomach. It can be done.”
Now I’ve shifted to really wanting to give back and pay it forward.
Starting the Strides Against Stomach Cancer Walk in Wisconsin
I plan events in my job. So in 2024, one of my friends — she’s always wanted to do some kind of walk to raise money for stomach cancer because there’s really not anything local in the area. It’s a lesser-talked-about form of cancer, so we don’t have anything already set up. She said, “Let’s just start a walk,” and I was like, “I don’t think you know exactly what that means, but sure, let’s do it.”
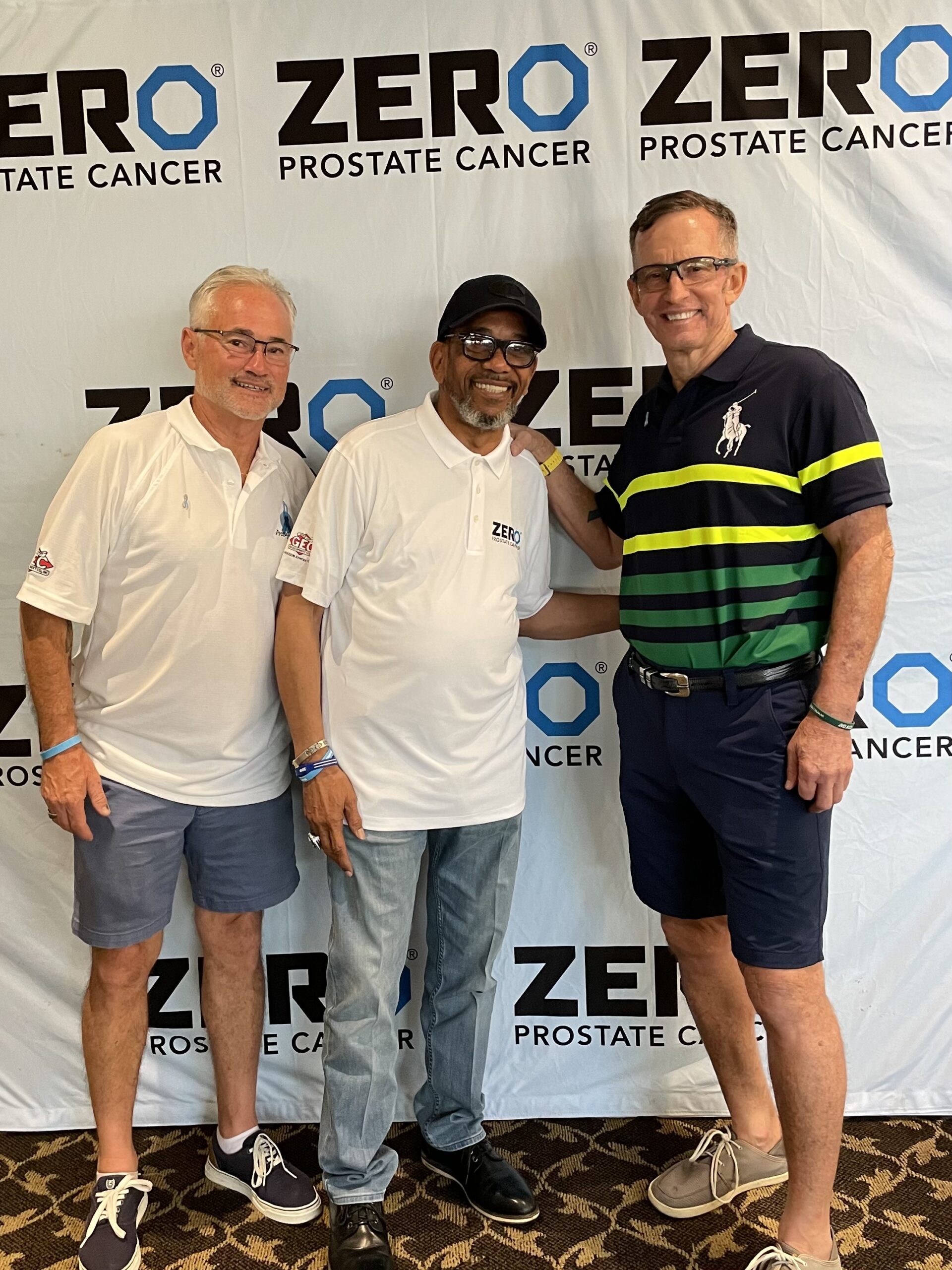
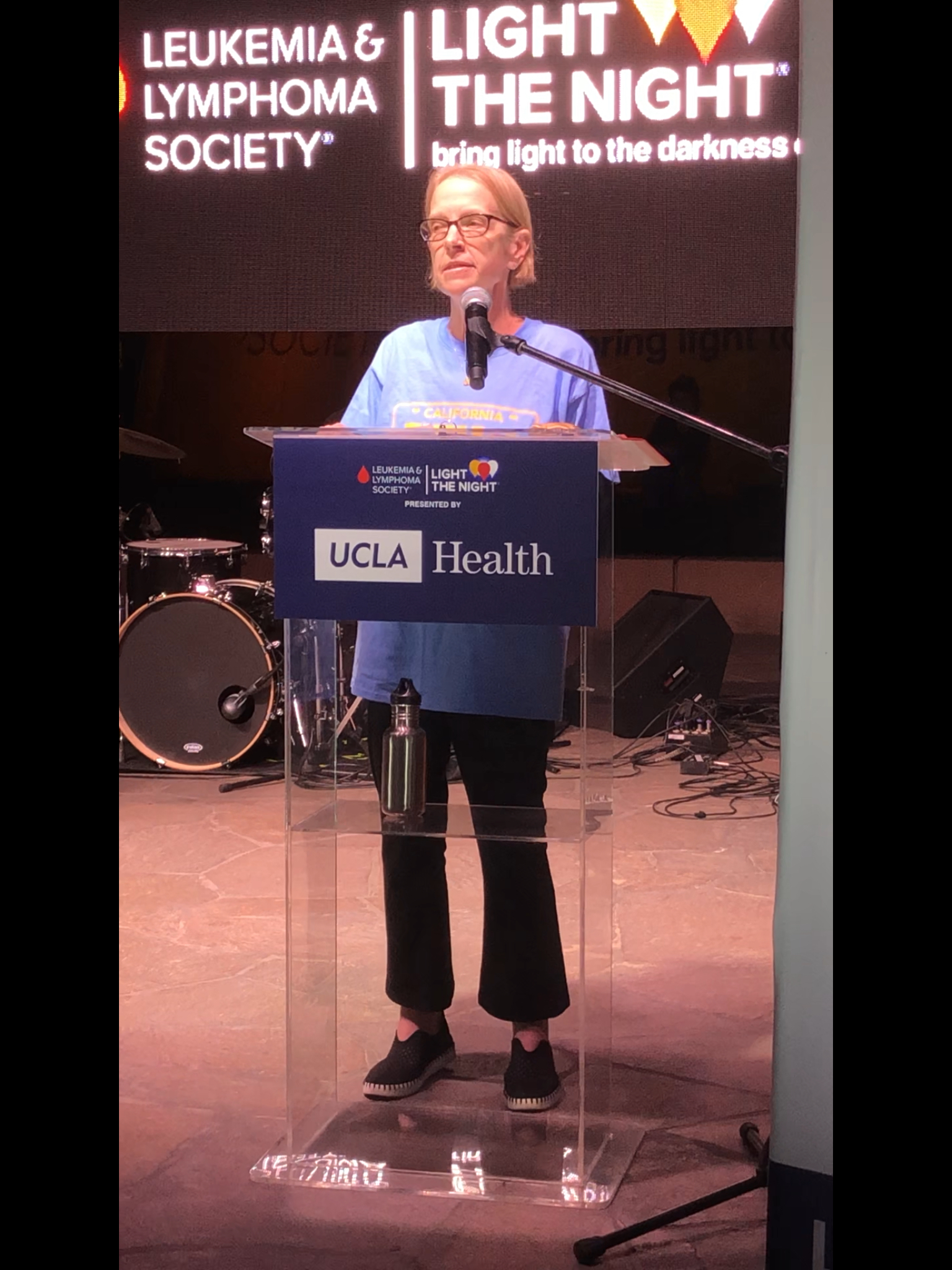
In 2024, we started the Strides Against Stomach Cancer walk in Wisconsin. We had a pretty minimal goal. We wanted to get 100 people — everyone bring your friends and family — and raise $10,000 to support stomach cancer patients. We were blown away. We had 200 people come that first year and raised over $20,000.
We learned so much along the way, even with that. While I do events at a university, this is very different from doing a big fundraising walk, which I had never really done. We learned a lot along the way.
This past year, in 2025, we had our second year, and again, I was blown away. We had over 300 people and raised over $30,000. The support and awareness we’re bringing to stomach cancer in the local area has been so important to me.
One exciting thing this year: last year, five stomach cancer survivors came to the walk, and I knew every single one. I had talked to them all before. This year, we actually had three new‑to‑me stomach cancer patients register, which was awesome.
It’s really important to me. I want to connect with people and share my story and help them along the way if I can — just to share that not every treatment will work for everyone, but maybe there’s another option someone hasn’t thought about. I’m looking to connect with other stomach cancer patients locally and across the country.
It’s been really special to start some of those relationships and find the weird coincidences of, “Oh, yeah, my aunt passed away from stomach cancer.” Finding those little connections has been really special. When someone says they know someone with stomach cancer, I’m like, “Tell me everything.” I don’t know many people who have it.
I feel like I’ve switched gears now, and I really want to pay it forward and keep advocating, obviously for myself, but for the full stomach cancer community as well.
Why raising awareness matters to me
It’s really important to me, especially for current patients — sharing my story with them — but also bringing awareness to stomach cancer. It’s one of the most deadly cancers and definitely one of the most underfunded.
We go to Advocacy Day with an organization. We go to the Hill every year to ask for more funding for research, just to keep pushing that. I feel like treatment options are getting better and better, but they really need those research funds.
I don’t think people know about that because stomach cancer is a less talked‑about cancer. Just bringing awareness to it is definitely something that I’m looking to do.
It’s definitely a family effort, for sure. This past year, my husband was lucky enough to get a media spot to talk about the walk, and he’s so passionate about it and being such a champion for me as well.
It has become our personality, I would say. Every single day, you’ll probably catch one of us in a periwinkle color, because that’s the color for stomach cancer. One of us is wearing a walk shirt or periwinkle, or we’re talking about it. It is our lives, for sure, and we’re very passionate about it because it is so personal.
I truly never thought when I was diagnosed that I would be where I am right now. Honestly, from the beginning, my husband found an organization online and was like, “Hey, you can get a mentor through them.” At the beginning, I was not interested. I was just trying to survive. That was really what I was trying to do.
It was a slow process for me — reaching out to people and connecting with them. Then it was, okay, I’m going to participate in an online forum or an online support group. Then we decided we were going to go to D.C. and participate in Advocacy Day. It has been a slow build. I was really hesitant at first.
Now, as I said, it has become our personality. That is just what we are always talking about or doing because we are so passionate about it. I never once would have thought I would be where I am right now, five years later.
What I want others to know
I think a message I would leave with people is that cancer is a tough, tough experience. You need to find your support system, whether that be family, friends, or online. I’ve found some really deep, amazing connections with friends online. We’re always like, this is the best group to be in, but the worst group to be in because we all are affected by cancer.
Find your support system. Reach out. Make sure you’re talking to people. Make sure you’re advocating for yourself — that’s probably the biggest one. If you don’t like what your oncologist is saying or you don’t agree with them, get a second opinion. No one’s going to be offended if you get a second opinion on this because it is a rare cancer.
So definitely push for some of those things and find your support system.
I think the biggest thing for me — there were so many milestones I never thought I would reach. I uploaded a lot of photos that reflect it as well.
I talked about it at the walk this year. I never thought I would see my son going to kindergarten. He’s in first grade now. My sister told me, I think it was a year after I was diagnosed, she got engaged. They were going to have a long engagement, and I was like, “That is not good for me. I want to see you get married.” I was able to see her get married last year, which was super special.
This past October, I celebrated my 40th birthday with a bunch of friends in Las Vegas, which was so much fun. In January, it will be five years since I was diagnosed. All those big milestones are very meaningful for our family, for sure.

Inspired by Lisa's story?
Share your story, too!
More Stomach Cancer Stories
Andy G., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Stomach pain, back pain, chest pain, extreme exhaustion, shortness of breath after short walks
Treatments: Chemotherapy, immunotherapy
...
Alyssa B., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...
Brittany D., Stomach Cancer, Stage T1b
Symptoms: Choking suddenly while eating and attempting to speak, neck and right shoulder pain, neck tightness, trouble swallowing certain food items
Treatments: Surgeries (subtotal gastrectomy, D1 lymphadenectomy, gastric bypass)
...
Camilla C., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Issues swallowing, swollen gland in the neck
Treatments: Palliative chemotherapy was offered but declined, nutritional changes to support her comfort and energy, meditation and mindfulness practices, self-directed healing methods
...
Emily D., Stomach Cancer (Gastric Adenocarcinoma), Stage 4 (Metastatic)
Symptoms: Persistent postpartum stomachache, early satiety, difficulty swallowing, vomiting
Treatments: Chemotherapy, immunotherapy
...
Alyssa B., Stomach Cancer, Stage 4 (Metastatic) (Hospice Update)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...