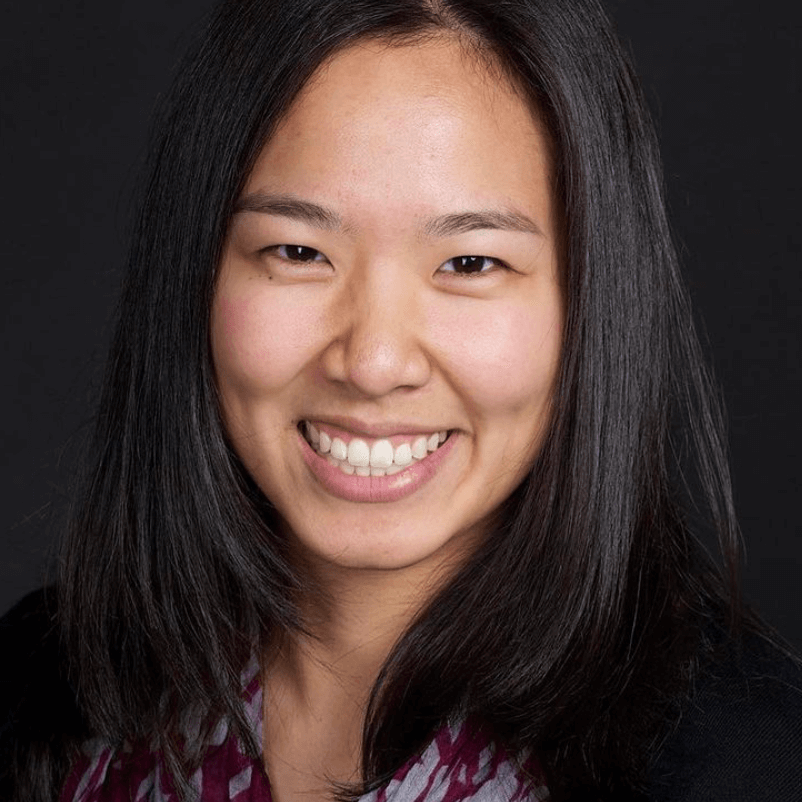
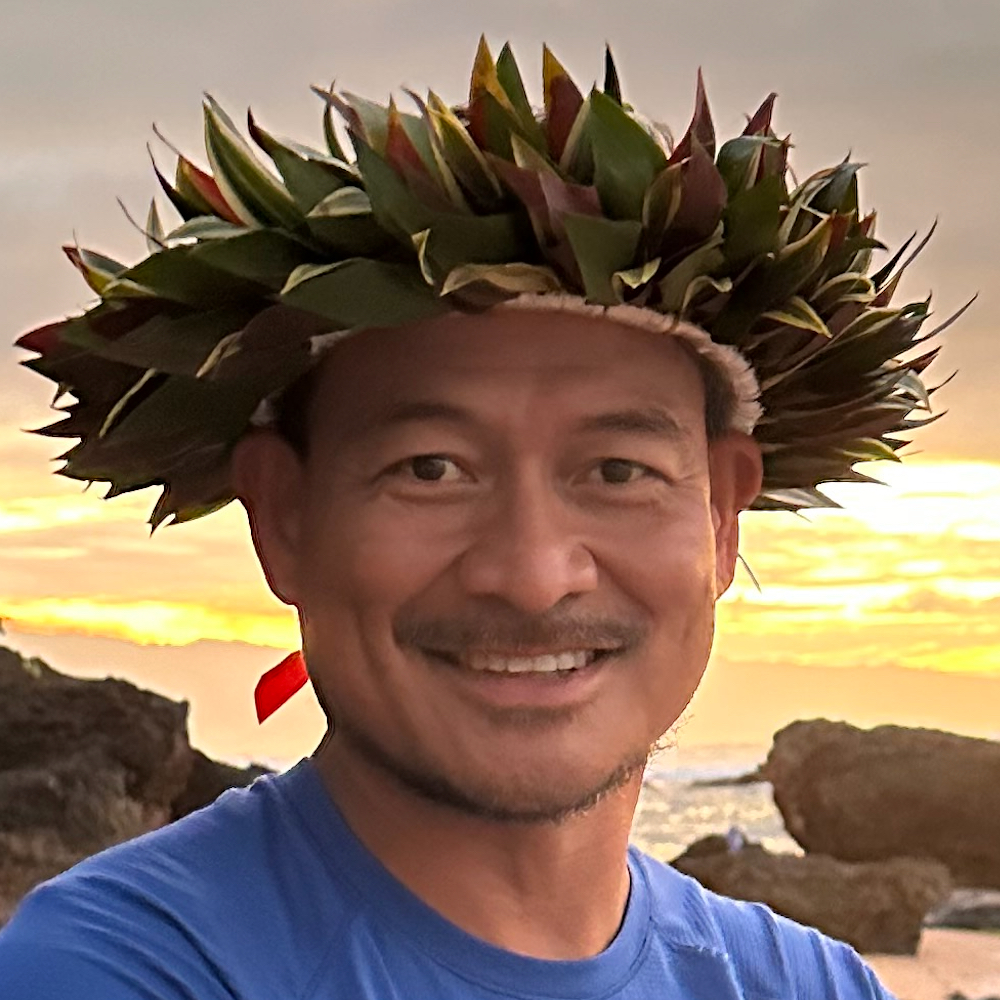
Camilla’s Story of Hope Beyond Terminal Stage 4 Stomach Cancer
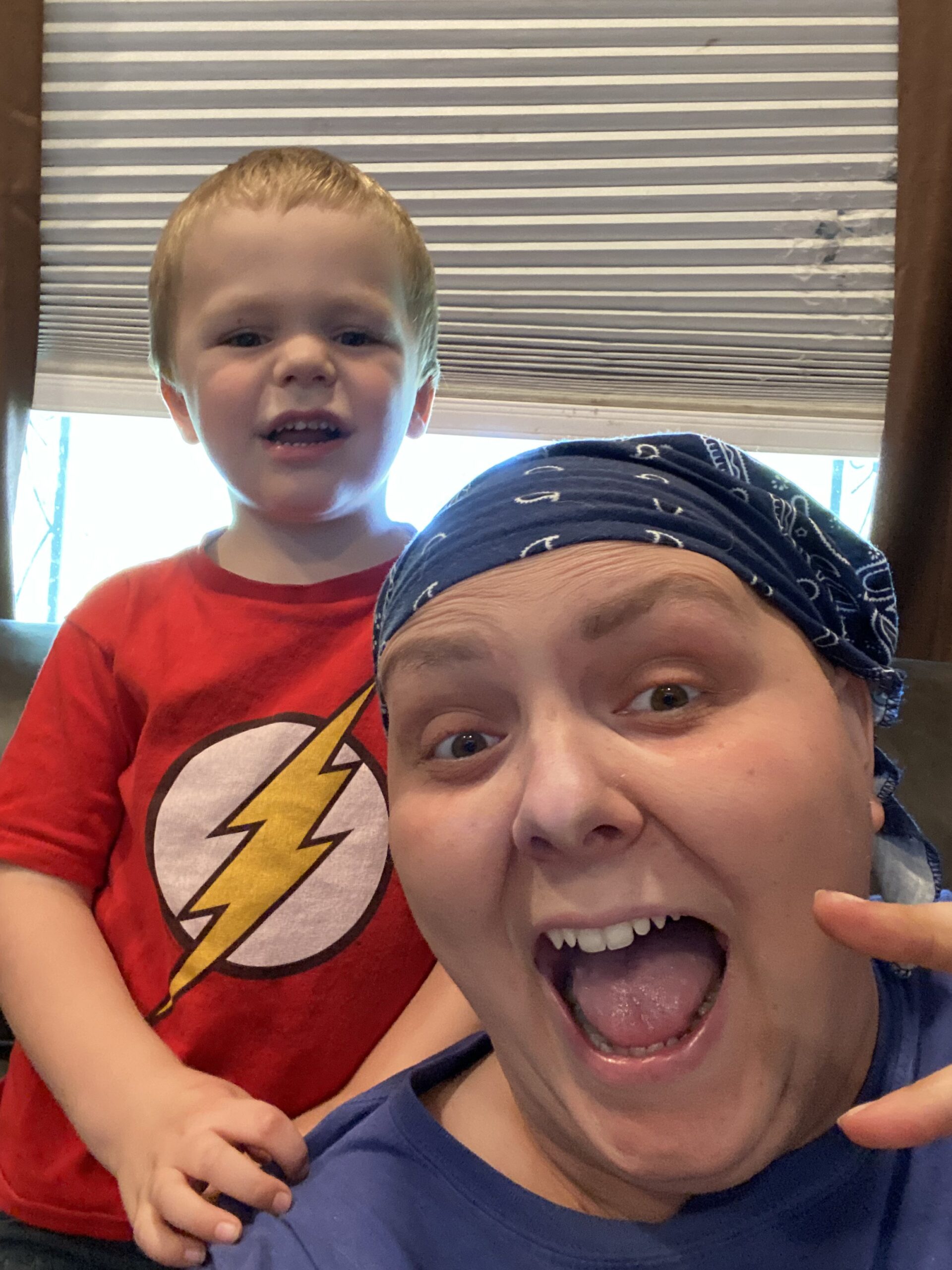
Camilla, a 40-year-old mother of four, was diagnosed with terminal stage 4 stomach cancer in February 2025. While the diagnosis was shocking, to say the least, she discovered an unexpected clarity and appreciation for life. She admits it sounds odd, but her diagnosis flipped her perspective entirely — refocusing on her health, family, and self-love.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez
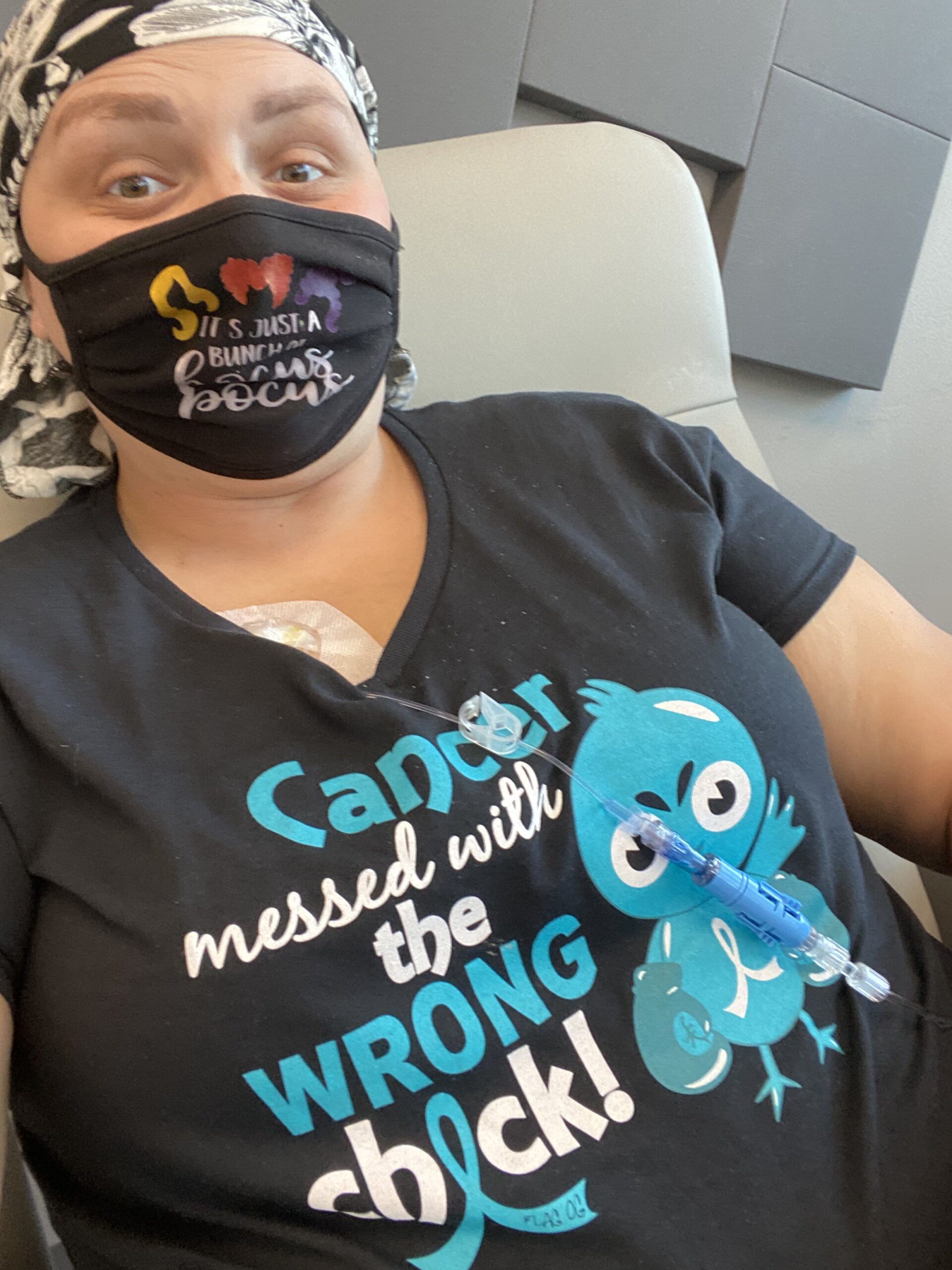
Before her diagnosis, Camilla sometimes had trouble swallowing and also discovered that a gland in her neck was swollen, something she initially dismissed as minor. It wasn’t until her symptoms worsened that she sought medical help, leading to an endoscopy that revealed a cancerous lesion. The CT scan results brought more devastating news: the stomach cancer had spread to her liver and lymph nodes. Despite being told that surgery wasn’t an option and only palliative chemotherapy was available, she chose a different path.

Camilla refused chemotherapy for her stage 4 stomach cancer and leaned into integrative health practices. She transformed her diet — cutting out sugar, dairy, and processed foods, and focusing instead on organic vegetables, fruits, wild fish, and whole grains. She incorporated fasting, yoga, meditation, and self-healing activities to support her mental and physical well-being.
Camila’s mental health has been a powerful part of her experience. She acknowledges that her emotional state directly affects her physical health. On down days, she feels the presence of her cancer more intensely, reinforcing the importance of maintaining a positive mindset. She embraces her feelings, allowing herself to cry, rest, and seek help without shame.
Planning her wedding for 2028, Camila embodies hope and determination. She refuses to accept her terminal stage 4 stomach cancer prognosis as her fate, believing that hope is vital for life. She is emphatic that one must never give up. Even when leaving the hospital with a terminal diagnosis, finding hope can transform despair into empowerment.
Watch Camilla’s video and learn from her about:
- Finding hope after a terminal cancer diagnosis.
- Why she refused chemotherapy and what she decided to do instead.
- How mental health can impact physical well-being during illness.
- The surprising ways her cancer diagnosis changed her life for the better.
- Her secret to living with a purpose beyond a terminal prognosis.
Note for Readers: Every person’s experience with cancer is unique. Camilla’s treatment decisions are deeply personal and based on her values and circumstances after having been told that surgery is not an option and being offered palliative chemotherapy. The Patient Story encourages anyone facing a diagnosis to explore all available options and consult with their healthcare team to determine what’s best for them.
- Name:
- Camilla C.
- Age at Diagnosis:
- 40
- Diagnosis:
- Stomach Cancer
- Staging:
- Stage 4
- Symptoms:
- Issues swallowing
- Swollen gland in the neck
- Treatments:
- Palliative chemotherapy was offered but declined
- Nutritional changes to support her comfort and energy
- Meditation and mindfulness practices
- Self-directed healing methods
What is palliative care? Palliative care focuses on helping people feel as well as possible when living with serious illness. Treatment is not about curing the disease but focuses on easing pain, managing symptoms, and supporting emotional and spiritual well-being. People can receive palliative care at any stage of illness, alongside other treatments, or on its own.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.

Inspired by Camilla's story?
Share your story, too!
More Stomach Cancer Stories
No post found