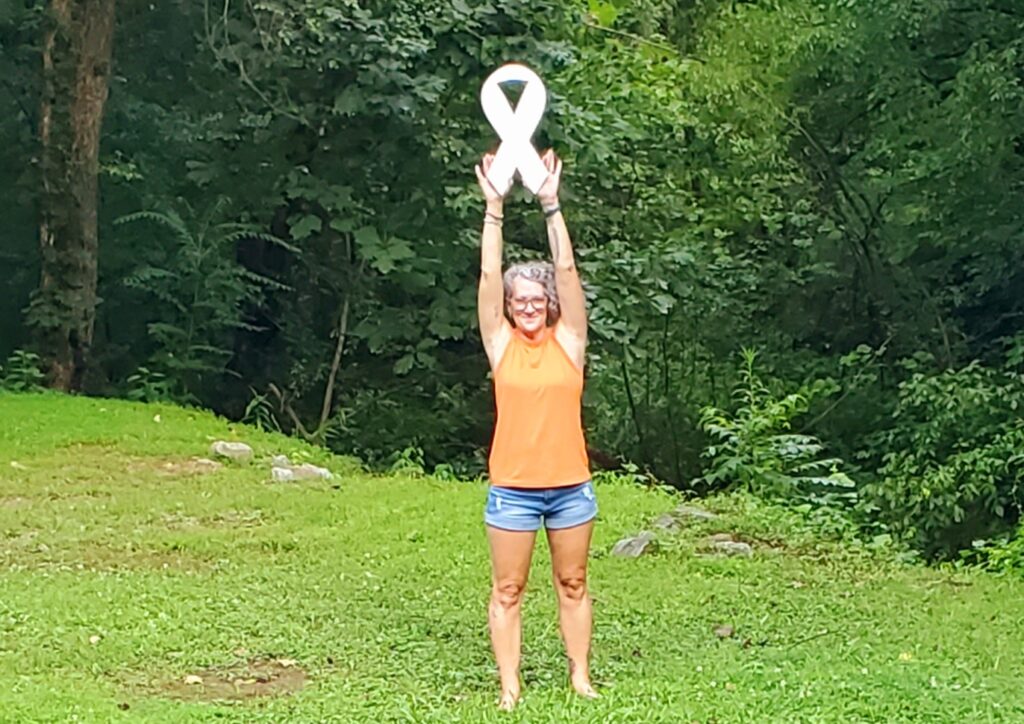
Laura’s Stage 4 ALK+ Lung Cancer Experience Balances Treatment and Quality of Life
For months, Laura managed a stubborn cough, but with a quiet pull from her intuition that something was not right. In South Carolina, where she ran a small handmade jewelry business, she also noticed deep fatigue and strange joint pain creeping into her days. These symptoms appeared slowly and at different times, so no clear connection was made. Intervention would come when, during a routine physical, she mentioned this year-long cough. A chest X-ray and CT scan were ordered right away and that’s when the truth emerged: a six-centimeter tumor and a diagnosis of stage 4 ALK-positive lung cancer.
Interviewed by: Carly Knowlton
Edited by: Chris Sanchez
Laura’s treatment for ALK-positive lung cancer initially focused on targeted therapies called tyrosine kinase inhibitors or TKIs. Laura cycled through several options, always balancing side effects against her quality of life. “If this is what my life is going to be like… it isn’t worth it,” she recalls, after struggling with the severe side effects of her first TKI. (Editor’s Note: TKIs work by blocking tyrosine kinases, enzymes that may be too active or may be found at high levels in some types of cancer cells. Blocking tyrosine kinases may help keep cancer cells from growing.)

Encouraged by her physician to prioritize what mattered to her, Laura took breaks, joined a clinical trial, and ultimately found a better fit with her current medication. “Patients should advocate for what works best; if side effects or treatments aren’t acceptable, speak with your doctor about changing things,” she says.
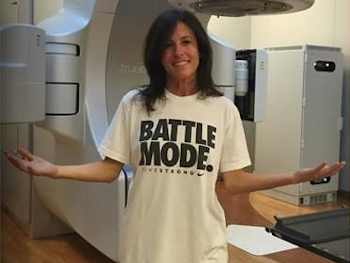
Laura’s ALK-positive lung cancer experience fundamentally shifted her identity and outlook. She speaks candidly about the grief and recalibration forced by advanced cancer, the evolving sense of self, and the acceptance of cancer as a chronic condition, if a life-defining one. Daily life is different, but Laura leans on support groups and prioritizes humor and connection.
“Given any type of tragedy, you either decide to learn from it, rebuild from it, or let it take you down,” Laura says. “And I think more of us decide not to let it take us down.”
Watch Laura’s video above, and scroll down to read through her edited interview transcript for more on:
- Why you should advocate for thorough diagnostics if your symptoms persist, regardless of smoking history or age
- How quality of life is essential; it’s valid to adjust or pause treatment if side effects outweigh benefits
- How proactive support in the form of family, community, mental health, and provider relationships can transform even the hardest experiences
- Why humor, connection, and redefining identity are key to sustaining hope and finding meaning
- How Laura has learned to accept new limitations, embrace choice, and support others through lung cancer community groups
- Name: Laura R.
- Age at Diagnosis:
- 37
- Diagnosis:
- Non-Small Cell Lung Cancer (NSCLC)
- Staging:
- Stage 4
- Mutation:
- ALK
- Symptoms:
- Persistent cough
- Fatigue
- Bone pain
- Treatments:
- Targeted therapies: tyrosine kinase inhibitors (TKIs), including through a clinical trial
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Laura
- My first symptoms and red flags
- Finding my care team
- My reaction to my diagnosis
- Genetic testing impacted my treatment options
- My experience with TKIs, their impact, and side effects
- My current work and support system
- The impact of cancer on my daily life
- Therapy experience and my quality of life
- My advice for others
My name is Laura
I live in South Carolina. I was diagnosed in May of 2023 with stage 4 non-small cell ALK-positive lung cancer.
It’s changed a little bit since my diagnosis, but before that, I owned a small handmade jewelry business. I still own it, but I do that part-time now. What I do for fun is horseback riding. I don’t get to do it as much as I’d like, but hopefully more so in the future now.
I try really hard to be funny. Whether or not I am, I don’t know, but I think I’m funny.
My first symptoms and red flags
It was hard because I overworked myself. I was very focused on work. I should have gone in sooner.
The first sign was a cough that wouldn’t go away. I’d been coughing for almost a full year, but it wasn’t bad. It was just a little bit in the morning. Sometimes during the day, I wouldn’t cough at all. It was just in the morning. Sometimes the cough would produce phlegm, sometimes it wouldn’t. Some days it got better, other days it got worse. It was a persistent cough that didn’t go away.
Over the years before my diagnosis, I became more fatigued, but gradually. I was approaching my late 30s, and I wondered, “Am I just getting old? Why am I tired all the time?” I also had a lot of joint issues, not debilitating, but pains in my wrist. I complained to my doctor, and she prescribed arthritis cream. I was in my 30s and wondered if that was normal. She said, “Yeah, it happens to some people.”
Those were the main symptoms: joint pain, fatigue, but the biggest one was the cough. I was lucky to have a cough because where the tumor was located, it was close to a bronchial opening, so the tumor caused almost an obstruction. I was trying to cough it out, but you can’t cough out a tumor.
I didn’t go to the doctor immediately. I lived with it, hoping it would go away. I was self-medicating. I’d always had allergies, so I kept taking allergy medications, switching between Allegra and others, but nothing helped.
At my yearly checkup, I talked about arthritis and back pain. I brought up the cough, and the doctor was concerned. She asked if I was from a region where there are common fungal infections in the lungs. I wasn’t. She thought a cough that long was unusual, so she sent me for a chest X-ray at the VA. The X-ray found a tiny nodule a few millimeters across. They said it’s common with service members and ordered a CT scan to monitor the size. After the CT scan, instead of a six-millimeter nodule, it turned into a six-centimeter mass, which is very large. That started the diagnosis process in May 2023.
Finding my care team
My first care team was a whirlwind, but I have healthcare through the VA, so it was all covered.
They told me to see a pulmonologist. I was referred to Dr. Nicole Tanner at MUSC in Charleston. She is amazing. She made me feel comfortable. She showed me the CT scan and explained the next steps with biopsy and diagnosis.
The VA is attached to MUSC, so I’ve received excellent care, and everything moved quickly. Waiting two days for a phone call felt long at the time, but the diagnosis from primary care to biopsy was within two weeks. I was given a pulmonologist and an oncologist.
At the VA, you can get a second opinion, so I got recommendations for a local thoracic oncologist. I also researched and found a specific ALK-positive specialist.
My reaction to my diagnosis
The news was given to me over the phone, which was fine. After the CT scan, my primary care doctor called quickly and said, “We’re going to do this.” I asked, “Why do I need to see an oncologist? Could this tumor be something else?” She said, “No, unfortunately, it’s cancer.”
It took me by surprise. I Googled possibilities, but didn’t think it was cancer. I said, “There’s absolutely no way.”
It took me a long time to believe it. I don’t even know when I fully recognized I had lung cancer.
I am a nonsmoker. We all went through COVID and had coping mechanisms, but that was rare and not a daily thing. Cigarette smoke? No.
Being diagnosed and treated for cancer as a woman in your late 30s is intense emotionally, hormonally, and mentally, because you’re aging and things are changing.
You think about childbirth, not being young anymore, friends with kids… it’s difficult to cope with all at once. I had to slow down after the diagnosis. It’s way too much for anybody to take on by themselves.
You have cancer, you can’t do this or that, you have to take medication, and then side effects prevent you from doing things. It’s too much.
Genetic testing impacted my treatment options
We waited to get my PET scan results to stage me.
Since I wasn’t presenting as poorly as some, maybe because of my age, there was no need to start chemo until genetic results came back. The genetic results [ALK positive] gave good news; there was a targeted therapy for me.
I started first-line therapy with my first TKI two years ago. Now I’m on my third.
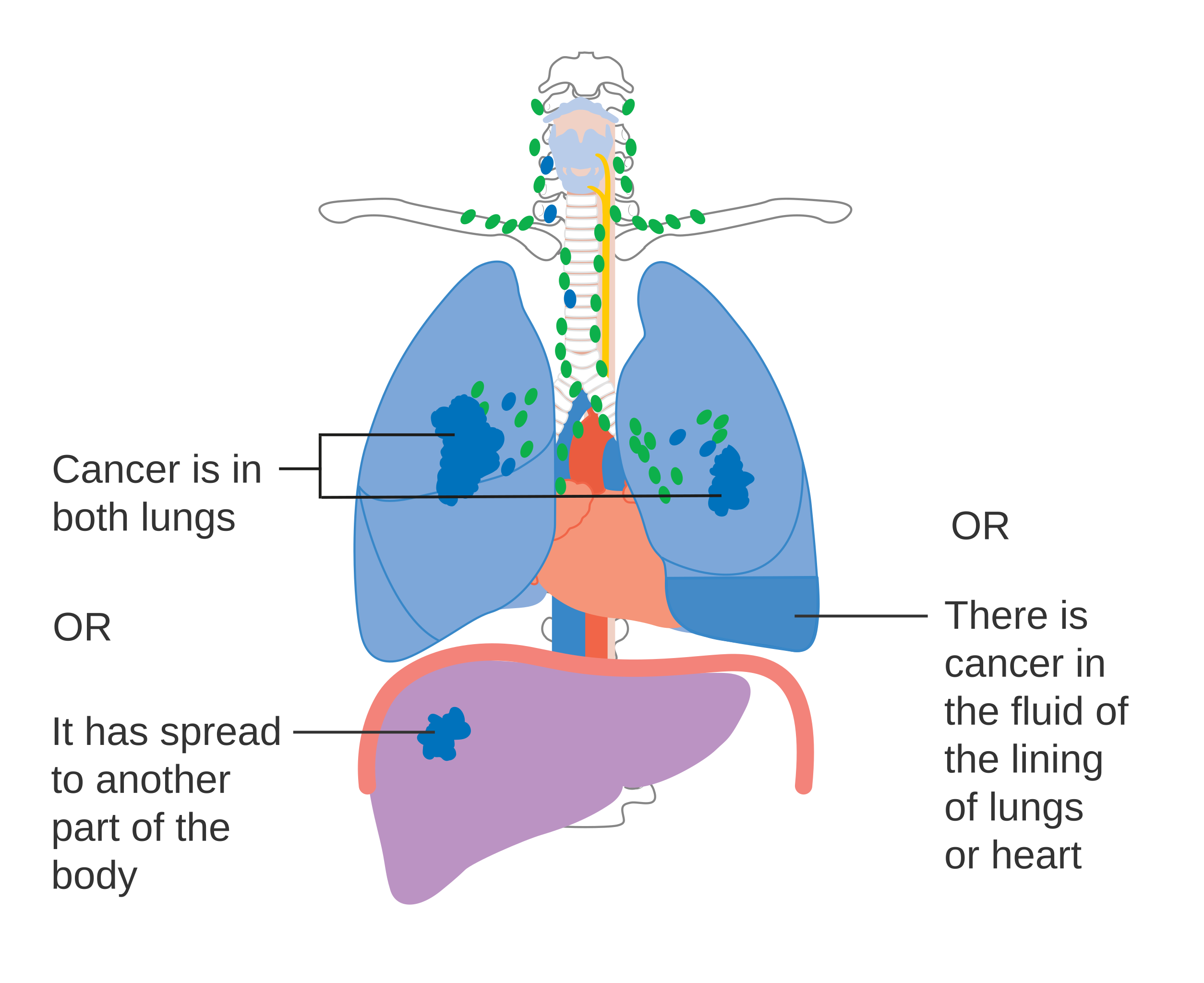
Surgery isn’t an option, since my cancer is stage 4 metastatic; it has spread to different areas. Some elect to have surgery, but for me, surgery isn’t curative, so it’s not an option.
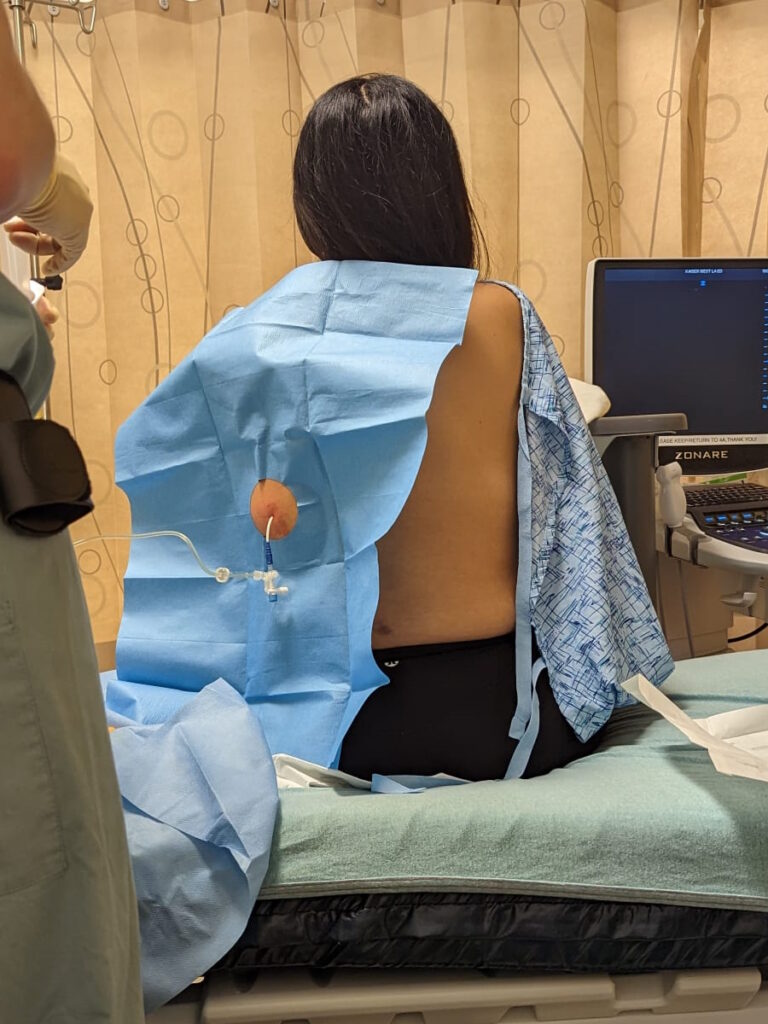
My experience with TKIs, their impact, and side effects
The first TKI wore me down. I lasted about a year, but couldn’t handle the side effects physically or mentally. I felt worse than before I had cancer, and I almost gave up. My specialist said that no one would force me to take it, which was freeing. I took a break, but the cancer grew back.
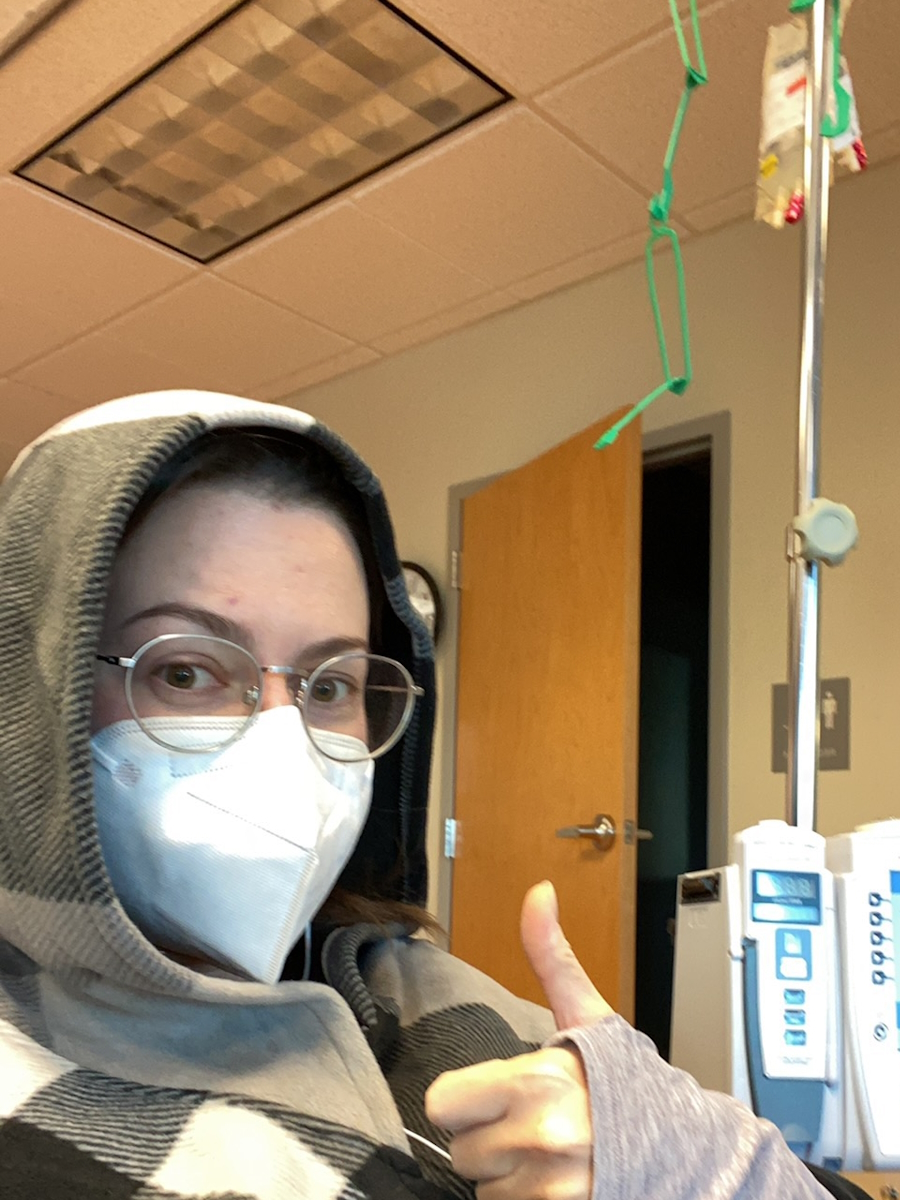
Then Dr. Lynn at Mass General told me about a clinical trial with cutting-edge medication. It’s rigorously tested and the latest available. I got on the trial, but my liver couldn’t tolerate the medication, which is common. I had some side effects from the clinical trial drug, but it was much better than the first drug. I loved the medication and was sad to stop.
I stopped and started my third TKI a month ago, and I’m doing pretty well so far. Hopefully, this one will stick. The drug I’m on now has minimal side effects. I increased my dose after consulting with my doctor because I had no side effects and wanted to see if the higher dose would hold.
There’s no end to it; treatment keeps going. TKIs are not a cure but must be taken until they stop working. Monitoring is constant with CT scans every three months to check tumor size. If it stays the same, that’s good news. Residual cells never go away. Researchers are working on vaccines and cures, but it’s a long process.
I kept my care at Duke University Hospital, where the clinical trial was run and supervised by an ALK-positive specialist. Instead of returning to Charleston, I now see the ALK specialist at Duke.
My current work and support system
I’m doing jewelry part-time and have stepped back a lot. Having my own business is great because I can return when I want. The connections are still there, just fewer. I pick when to work.
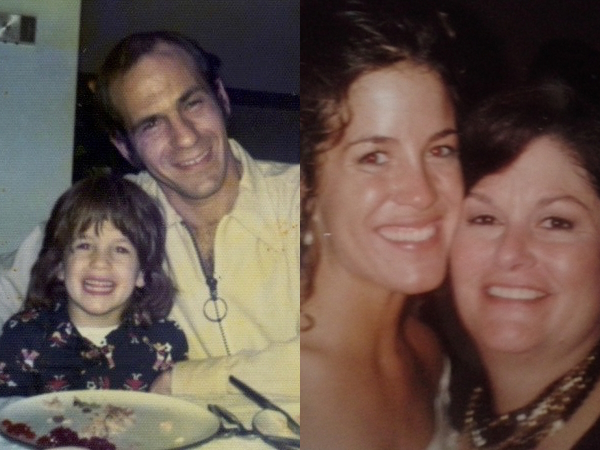
I have a lot of friends. My recently made friend, Emily, now lives in Washington state and has helped a lot. My sister, my only family member, left before, and our relationship wasn’t good. The diagnosis didn’t improve things, but we worked hard to rebuild our relationship, and it’s gotten much better. That’s one good thing about cancer; it brought my sister and me closer.
The impact of cancer on my daily life
The first year was the hardest; the second year was also difficult, mostly in finding a new normal. It’s like grieving loss, scrambling to survive, and rebuilding. It’s completely overwhelming, but you either do it or you don’t.
I have to do it. With any tragedy, you either learn and rebuild, or let it take you down. Most decide not to be taken down.
The hardest moment I’ve faced so far was deciding to stop the first TKI. I was going through a lot, dealing with side effects, life changes, and reflecting on a year of medication with a worse quality of life. I’d basically given up and stopped medication.
When I spoke to Dr. Lynn, she said, “What are you doing? You don’t have to take it.” I didn’t know that.
I’m fortunate to have supportive friends willing to help whenever I need it. Mental health is very important for people with this diagnosis since it’s life-changing. Some people aren’t sure what to do. There are many who care and want you to fight.
My identity has completely changed because I will always carry cancer; there is no cure. I think about death every day, almost like a built-in ticking time bomb. Not that I expect to die tomorrow, but it’s always there. At the same time, I appreciate life and can do what I want, such as take medication or not.
Therapy experience and my quality of life
I was already in therapy before the diagnosis and continued afterward.
I learned to speak up and eventually switched therapists, which was the best decision. If you don’t like your therapist or aren’t getting better, get another one.
Quality of life is often overlooked in cancer care, but it’s crucial that patients aren’t tortured to death. For me, quality is more important than length of life.
Everyone’s priorities are different. Some want to live at any cost. I think this changes how care should be delivered.
If you don’t like your treatment, talk to your oncologist. There are usually other options.
Advocacy is vital because your life won’t get better until you ask for change.
My advice for others
You’re not alone.
One of the best things I did was find a support group online. A friend recommended it, and connecting with others who understand made a big difference.
We all go through similar things, though differently. Having that support group has helped a lot over the past two years.

Inspired by Laura's story?
Share your story, too!
More ALK+ Lung Cancer Stories
Stephanie K., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent and intense cough, general feeling of sluggishness
Treatments: Chemotherapy, targeted therapy through a clinical trial, radiation therapy
Ruchira A., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Mild intermittent cough while talking, low-grade fever, severe nonstop cough, coughing up blood, collapsed left lung
Treatments: Surgery (lobectomy), targeted therapy
Laura R., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent cough, fatigue, bone pain
Treatments: Targeted therapies (tyrosine kinase inhibitors or TKIs, including through a clinical trial)
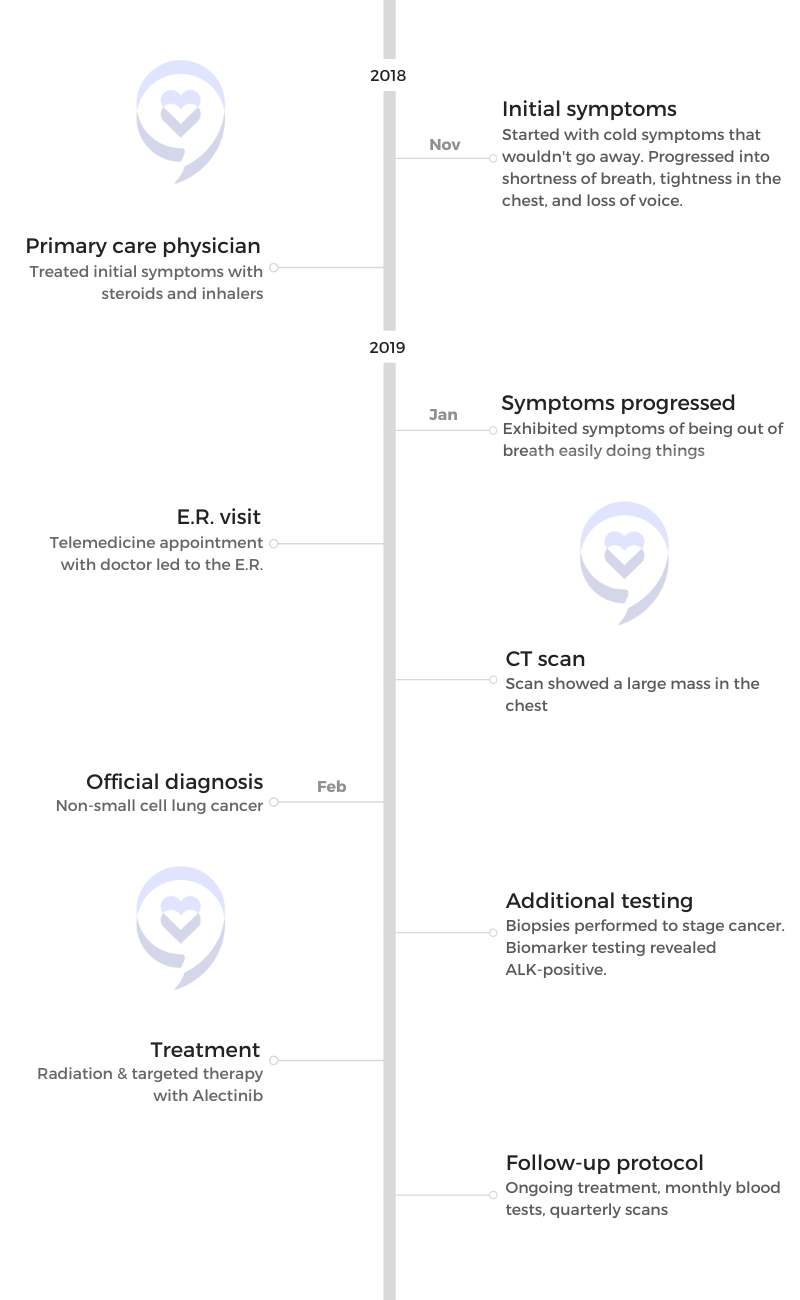
Shauna D., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptom: Persistent dry cough following a cold
Treatments: Targeted therapy (tyrosine kinase inhibitors), radiation therapy
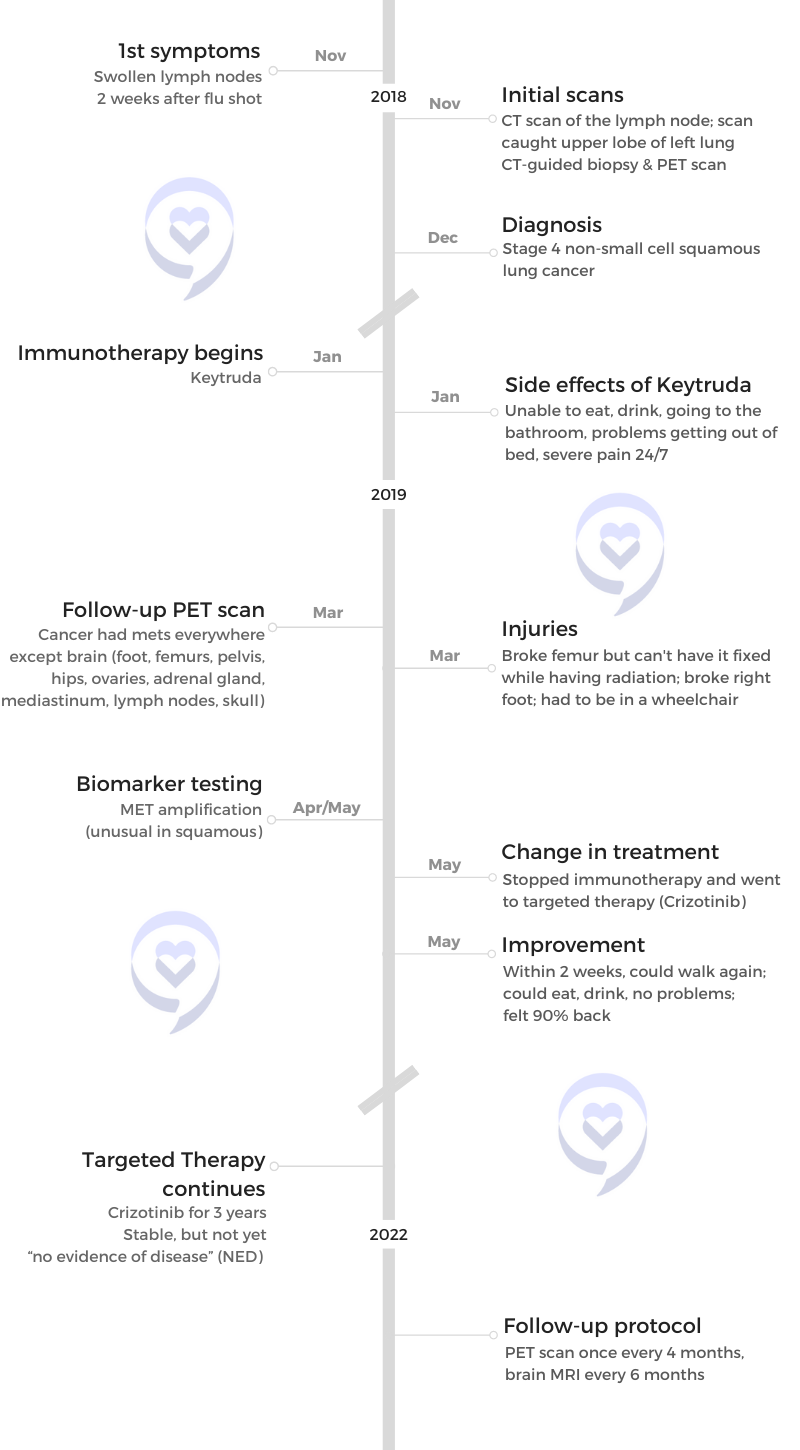
Allison Z., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptom: Severe back pain
Treatments: Targeted therapy (ALK inhibitors), radiation therapy