Amy’s Stage 4 Colon Cancer Story
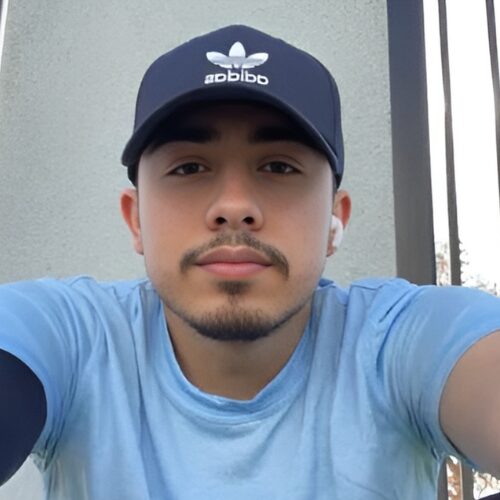
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal

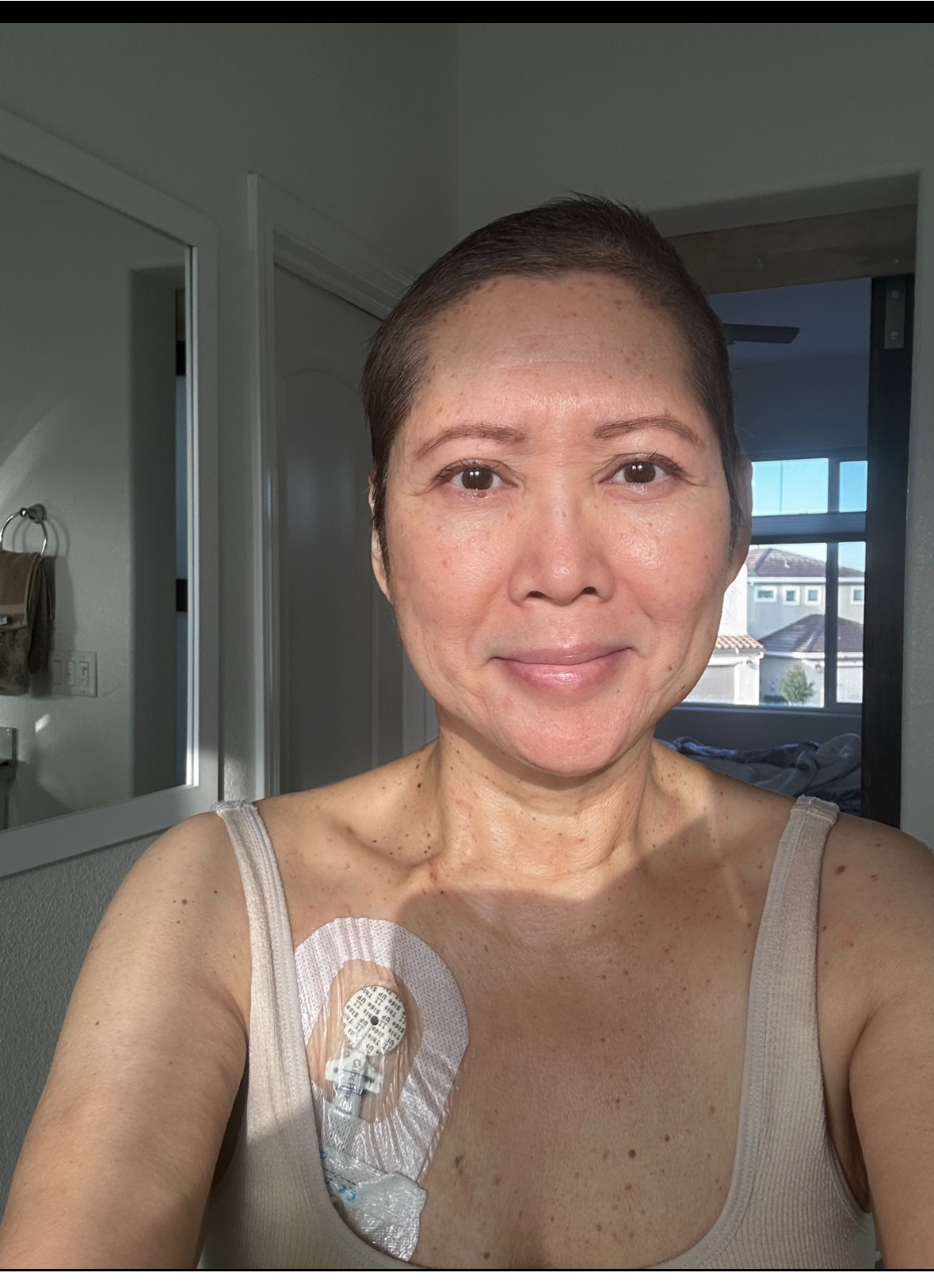
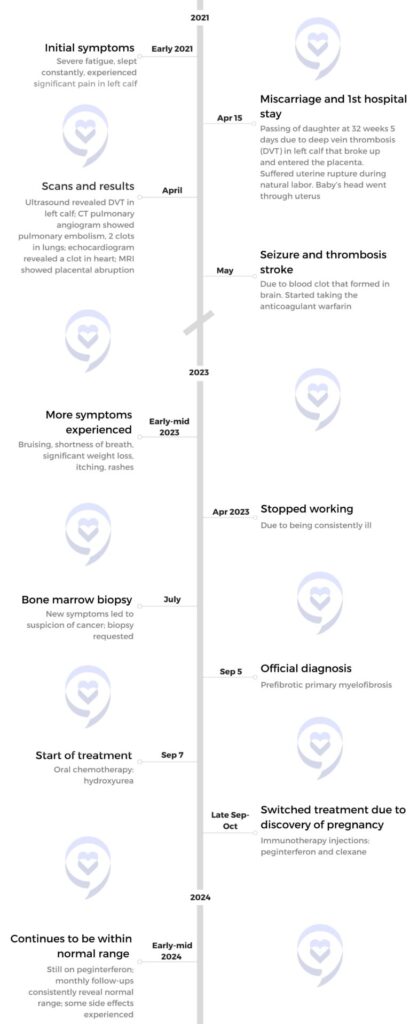
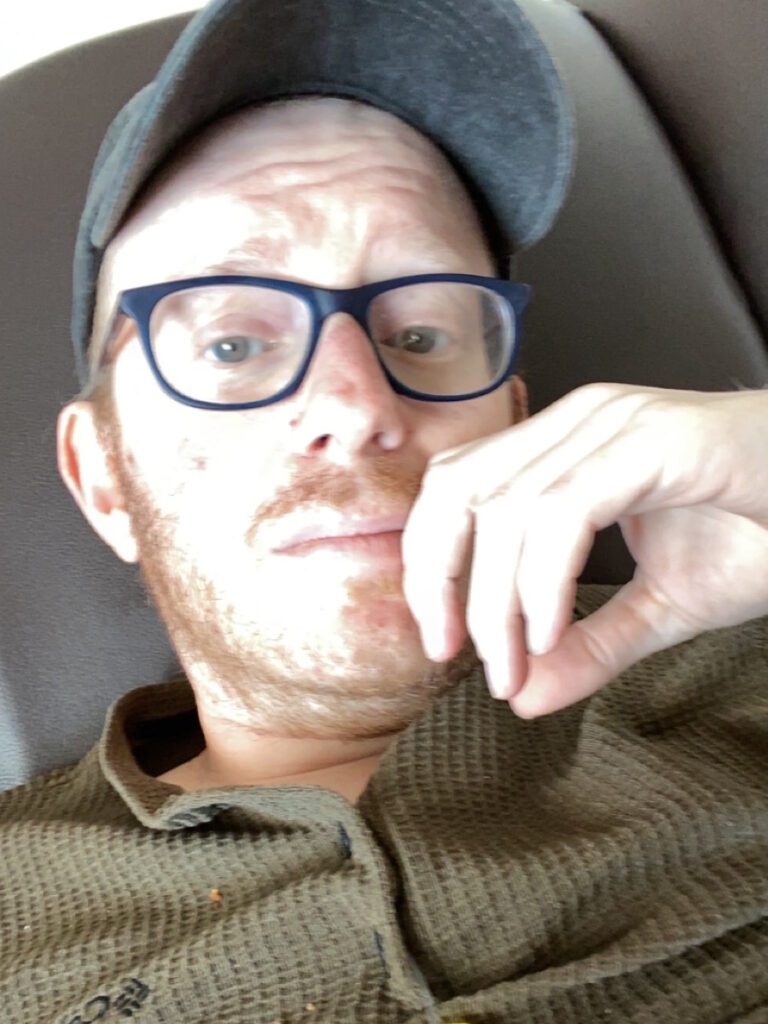
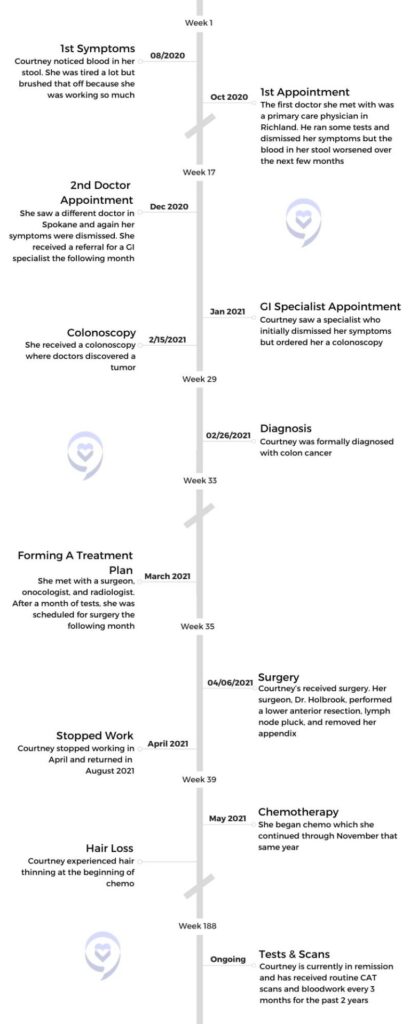
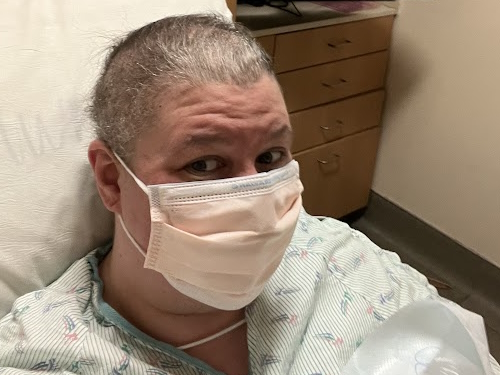
Amy initially noticed a slight change in her stool consistency, which persisted despite normal test results. After a year-long delay due to the COVID-19 pandemic, a colonoscopy revealed a 6-cm mass in her colon. Although the initial biopsy showed no cancer, surgery confirmed cancer in the tumor center and 11 out of 21 lymph nodes. It was stage 4 colon cancer.
She began treatment with FOLFOX, experiencing severe side effects like jaw pain, cold sensitivity, and neuropathy. Despite completing the regimen, a slight increase in CEA levels prompted further tests. A CT scan and MRI revealed cancer in her liver, leading to a relapse diagnosis. Unhappy with her initial oncologist’s pessimism, she sought a second opinion and switched to a more supportive doctor.
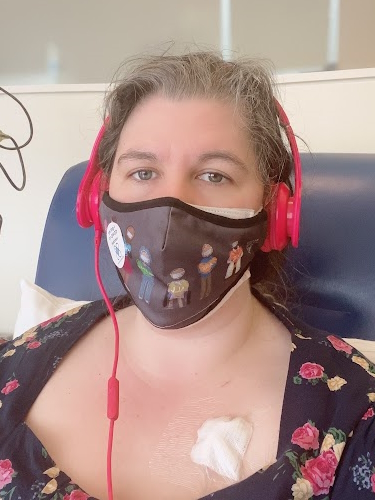
Her new oncologist initiated FOLFOXIRI, which shrank the tumors but wasn’t enough to eradicate the cancer, leading to surgery and an ablation. When the cancer resurfaced, she joined an immunotherapy clinical trial. The difference between chemotherapy and immunotherapy was substantial, providing her with a significantly improved quality of life.
Throughout her stage 4 colon cancer journey, Amy emphasized the importance of a supportive medical team, listening to her body, advocating for her health, and maintaining movement and proper nutrition during treatment. She also stressed the need for open communication with healthcare providers about side effects and health concerns.
- Name: Amy L.
- Diagnosis:
- Colon Cancer
- Staging:
- 4
- Symptoms:
- Slight change in stool consistency
- Treatments:
- Chemotherapy: FOLFOX, FOLFOXIRI
- Clinical trial: immunotherapy

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
What might be normal for somebody else might not be for you. If there’s a change, it’s important to talk to your doctor about it.
Introduction
I’m from the Seattle Pacific Northwest area and I was diagnosed with stage 4 colon cancer.
Pre-diagnosis
Initial Symptoms
I only had one symptom, which was a very small change in my stool. It became slightly looser, but it wasn’t consistent. For most people, that might not be a big deal, but I hadn’t changed my diet. The first time I noticed it was when I had just come back from Spain and I thought it was from traveling. I gave it a few weeks, but it wasn’t getting better.


PCP Appointment
I listened to my body and talked to my doctor about it within a month of this first symptom. My doctor at the time thought it was food sensitivity. They did autoimmune testing for Crohn’s and celiac disease, but those came up negative. They did an allergy panel to see if I developed any new food allergies. That came back normal. I also had my first CEA test, but I had no idea what that was and that also came back normal.
I was blessed to have a doctor who was very proactive and didn’t ignore my symptoms. They knew that I knew my body. What might be normal for somebody else might not be for you. If there’s a change, it’s important to talk to your doctor about it.
Unfortunately, they couldn’t get me in for a colonoscopy. They did the fecal immunochemical test (FIT) test. They did all these tests and everything was coming back normal.
He recommended me to a dietician who started looking at what I was eating and what we could change that might explain the stool change. My doctor said that since everything’s coming back normal, he wanted to do due diligence to make sure that there’s nothing they might be missing. He said, “Let’s get you in for a colonoscopy.” That was in the end of 2019.
They called in and said my procedure was non-essential and not COVID-related, so I needed to be put on hold… Unfortunately, I ended up waiting for a whole year.
Getting a Colonoscopy
They were booked back a few months. I wasn’t considered urgent. Nobody thought I had cancer. I was 39. They said they’ll get to me at the end of January or early February 2020. Then the COVID pandemic happened.
A week before my appointment, they called in and said my procedure was non-essential and not COVID-related, so I needed to be put on hold. They would call when they could make it happen again. Unfortunately, I ended up waiting for a whole year.
During that year, I was furloughed, so I was staying at home. My symptoms went away, which confirmed to me that maybe it was something I was eating since I wasn’t eating out.
By January 2021, I got a phone call asking if I wanted to schedule my colonoscopy again. I almost said no and that I didn’t need it anymore because the problem had gone away, but a little voice inside me told me to go ahead and do it. The “worst” thing that they could tell me is that nothing’s going on. I had nothing to lose, so I told them to go ahead and schedule it. They scheduled me for the first week of February 2021.


I didn’t have any other symptoms, like pencil-thin stools, bloating, or pain. Nobody was looking for cancer, especially colon cancer. Most people who get colon cancer are in their 70s and 80s. The first oncologist I had even told me that I was the youngest patient he ever had. Most of his patients were 60 and older, so it wasn’t on anyone’s mind that I could have cancer.
When I did the prep for my first colonoscopy, it was worse than the colonoscopy itself, but it’s a small drop in the bucket out of all the days in my life. On the day I came in, everything proceeded as normal. I got onto the table and they told my husband that the procedure could take up to 30 to 45 minutes. He couldn’t stay with me, so he dropped me off and left.
They put me in twilight sedation so I’m out of it, but the doctor’s voice and tone cut through. She turned to her nurses and said, “Where is her husband? Get him back here right now. Call him. We need him back here right now.”
She didn’t say anything, but because of her tone, I knew something was wrong. I felt my heart dropped to my stomach. I was half awake and the anesthesiologist was trying to put me back to sleep because my eyes were open and I was starting to ask questions. I didn’t feel anything, so it wasn’t traumatic.
The biopsy results showed there was cancer in the center of the tumor and 11 of 21 lymph nodes.
Diagnosis
Biopsy
When they wheeled me back into a curtained area, my husband was already there waiting for me. The doctor came and said they found a 6-cm mass in my colon.
I waited for the biopsy results to come back and when she finally called, she said they biopsied the tumor, but there was no cancer. However, they were extremely concerned given the size. It was either going to turn into cancer soon or there would be cancer in the center and not on the outside, so they wanted to get me in quickly. Everything was indicating that they had “caught this in time” and that I would just need surgery and might not even need chemo.


Surgery
They scheduled the surgery within three weeks of that conversation. They were on top of it and wanted to get it out.
The surgeon came in to talk to me. The biopsy results showed there was cancer in the center of the tumor and 11 of 21 lymph nodes. The tumor hadn’t broken through the colon, like they usually see with more advanced cancer, so they were not expecting to see cancer in my lymph nodes. He was very shocked it was stage 4 colon cancer.
I made an appointment with a doctor at Fred Hutchinson Cancer Center to get a second opinion because I wanted to know more.
Oncologist Appointment
My mom was an ER nurse. She also has leukemia, so she hasn’t worked while dealing with that. My mother-in-law is a hematology-oncology nurse at the Mayo Clinic. I’m fortunate to have knowledgeable people who helped me through the next process.
They referred me to my regular oncologist and said he’d go through my stage 4 colon cancer treatment plan. I had a meeting with him and it went okay, but I ended up switching. He told me that I would need clean-up chemo or adjuvant chemotherapy. Everything looked fine. He wasn’t hugely concerned.


Treatment
FOLFOX Chemotherapy
They said I was going to do FOLFOX (folinic acid, fluorouracil, and oxaliplatin) and then we would do a CT scan. They did a CT scan right after the colonoscopy where they found the mass, but they didn’t find anything else. He said it’ll be good.
Getting a Second Opinion
I made an appointment with a doctor at Fred Hutchinson Cancer Center to get a second opinion because I wanted to know more. I knew nothing. Is FOLFOX the standard treatment? What were my treatment options for stage 4 colon cancer?
Different doctors have different preferences and I wanted to ensure I was getting all the information. I made an appointment and brought all of my medical records to make sure. The doctor said they would do the same treatment.
I had a very rare side effect where I had jaw pain… This was a rare side effect of oxaliplatin.
Side Effects of FOLFOX
I did 12 and it was terrible. Before my second round, I had a very rare side effect where I had jaw pain. It was the most excruciating pain I’d ever experienced in my entire life. It radiated from my jaw back up around my neck and felt like somebody had put my head into a vice.
They didn’t know what was going on. I didn’t find out until I switched oncologists that this was a rare side effect of oxaliplatin. They sent me to a jaw specialist to make sure there wasn’t something else going on. I spent the rest of my treatment switching back and forth between morphine and oxycodone because the pain was so horrific.

On top of the nausea and hair loss, the cold sensitivity was bad. I like my drinks either really hot or cold. I don’t like lukewarm drinks. Chemo, especially oxaliplatin, made everything taste like pennies and dirt. I’m a big water drinker and I couldn’t drink water because the taste would make me gag. I started drinking electrolyte drinks to mask the taste. I don’t like sugary drinks, but I needed to get fluids in me so I don’t end up in the hospital. You have to do what you have to do to survive, I guess.
I also developed bad neuropathy in my hands and feet, and that came on suddenly. I was doing fine, but by cycle 10, the pain in my feet started to get bad. I was having trouble gripping things. I couldn’t wash the dishes. I would pick something up and drop it.
When the CT scan results came back, they found something in my liver… they didn’t think the cancer had come back, even though my CEA was up to 5 or 5.5.
Post-Treatment Follow-Up
After they finished, they did my scan and didn’t notice anything, so they sent me on my way and said they’d see me in six months. I wanted to see him in three, but he said he didn’t think that was necessary. I said I did, so he scheduled me for a three-month visit, which ended up being fine.
During my six-month visit, my CEA went up to 2 and that was my first flag. My CEA was still perfectly normal, but my CEA had never gone above 1.7. When I had the appointment with my oncologist, I told him this was concerning for me and he said it was a little concerning for him too. It’s a little bit of an increase, but it could still be normal, so he scheduled a blood draw after four weeks.
In four weeks, my CEA was 4.6 and that was abnormal for me. It was still within the normal range because anything under 5 is still normal, but I thought it was concerning. He said we could do another blood draw in four weeks.
By this time, it was around July and he said I wasn’t due for my CT until October. I said I didn’t want to wait until then.

Relapse
When the CT scan results came back, they found something in my liver. They thought it was a lesion because they said cancer usually looks like billiard balls but this looked like a zucchini. At that point, they didn’t think the cancer had come back, even though my CEA was up to 5 or 5.5, so something was going on.
They did an MRI and the results looked more like cancer. When they did a PET scan, the results looked even more like cancer. The biopsy confirmed it.
He said, “It’s looking more like it could be cancer.” They hadn’t done the biopsy yet at this point. He said, “If it’s cancer, there’s only a 20% chance you’ll make it to old age. That’s what the statistics tell us.”
I needed a doctor who I felt was on my side. I needed someone who I felt was going to fight for me.
Reaction to the Relapse
I walked out, got in my car, closed the door, and broke down crying. I was done with this oncologist. This is a horrific journey in itself. I needed a doctor who I felt was on my side. I needed someone who I felt was going to fight for me. I don’t care what the statistics say. There’s always somebody that’s on one side or the other.

Looking at Statistics
When you get these statistics, they mean something to doctors and researchers, but they don’t mean anything to people personally because you don’t know which side of that line you’re going to fall on. You could have the worst diagnosis and still survive.
I didn’t want to hear the statistics not because I was blind to it but because I knew it didn’t matter to me. The doctors are guessing which side of the line I’m going to end up on and I don’t want to hear their guess. I wanted to know if my treatment was working and if not, what my next steps would be.
She noticed the lymphatic system near my kidneys was getting larger so they thought that there was cancer there.
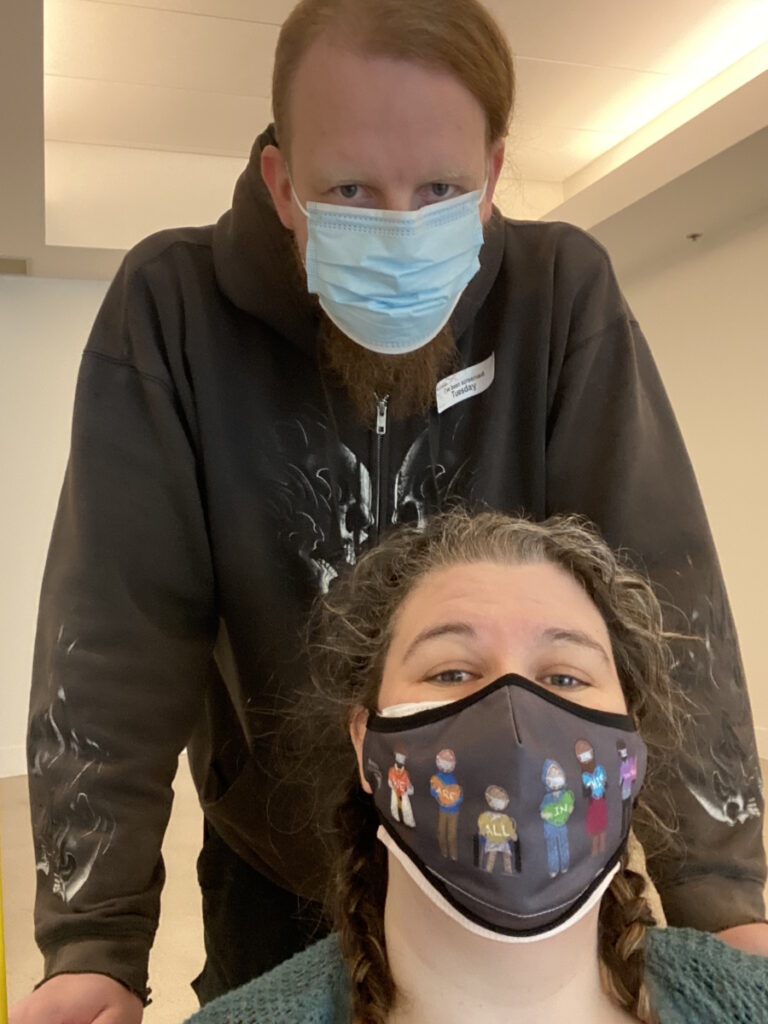
Switching Oncologists
I went back to the oncologist from whom I got a second opinion and she’s fantastic. She’s the best decision I ever made. One of the first things she did was get all of my scan results. She called my former doctor, requested all of my scan results, and sent them to a couple of different specialists so they could look at all of them. My new oncologist is on top of it and doing CT scans every eight weeks.
She noticed the lymphatic system near my kidneys was getting larger so they thought that there was cancer there. My first oncologist hadn’t even looked at that and it was one of the first things she noticed. It confirmed to me that I made a good decision.
I have this bad luck of getting things that look favorable but don’t end up being favorable. When I had my relapse, they looked at it and said I had a single liver lesion, which isn’t common. At that point, I was still considered curable.

Relapse Treatment
FOLFOXIRI Chemotherapy
She put me on FOLFOXIRI (folinic acid, fluorouracil, oxaliplatin, and irinotecan). I did FOLFOX a few times, but it wasn’t shrinking, so they added irinotecan and it started to shrink.
I went back on the full treatment for six months with very low node shrinkage but with slow growth.
Side Effects of FOLFOXIRI
I was miserable on oxaliplatin. It was terrible. I was sick all the time. The neuropathy in my hands had gotten better, but my feet had gotten worse. I could still do stuff with my hands, but my feet are pretty bad. I also had cold sensitivity, like not being able to eat cold food. Breathing in cold air was like breathing in shards of glass. My oncologist said they didn’t see any shrinkage with oxaliplatin, so she decided to remove it.
I had treatment until February 2023. It was shrinking and looking good, but it wasn’t going away, so they wanted to do surgery to remove the lymph system that had cancer in it. They did an ablation on one spot.

My oncologist wanted to do the ctDNA test to see if I had circulating tumor DNA in my blood. Four weeks later, that came out positive.
She said they usually wait 8 to 10 weeks before doing the first scan post-treatment, but she wanted to go ahead and do an MRI six weeks after surgery. She wanted to make sure because it looked like there was residual cancer.
Unfortunately, my liver lit up. They did a PET scan and there are a couple of spots now. I went back on the full treatment for six months with very low node shrinkage but with slow growth.
The difference between immunotherapy and chemotherapy is like night and day.
Joining a Clinical Trial
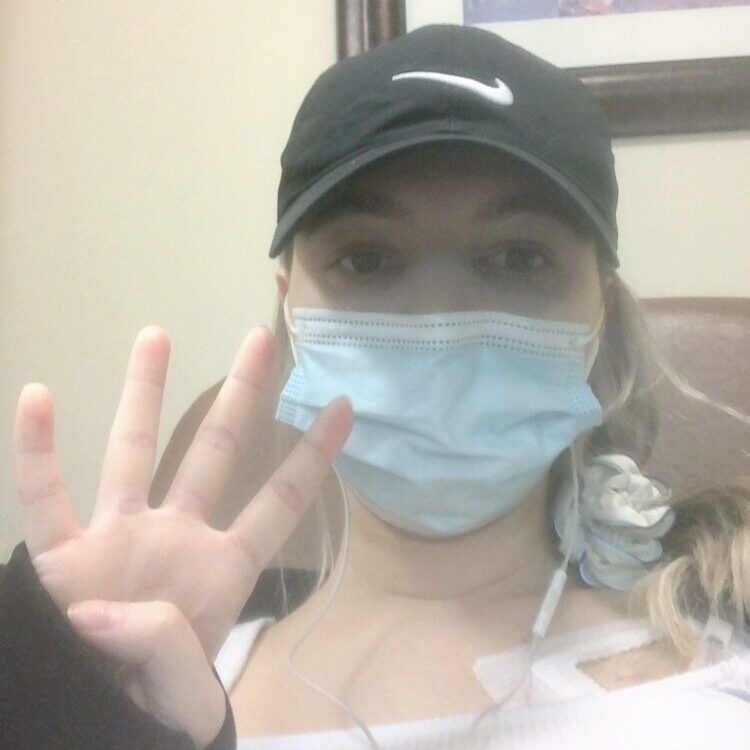
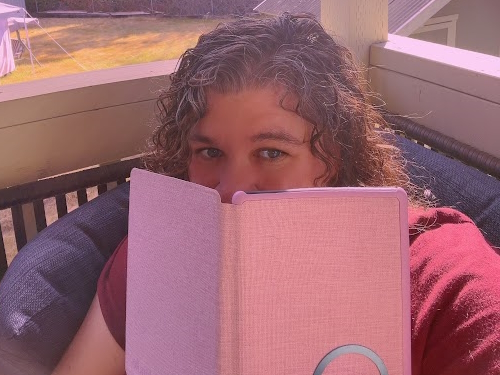
I started with an immunotherapy clinical trial in December 2023. The difference between immunotherapy and chemotherapy is like night and day. I’m not sick and tired all the time, so I’m able to go out and do normal activities. I feel like I’m able to have more of a normal life. It’s been fantastic, but I’m still fighting.
This is why it’s important to have a doctor who’s on your side. As soon as my recurrence happened, she went ahead and signed me up for every single trial that they offered. She didn’t ask me because she knew that these trials could have a year’s wait list. She figured that wherever I was, at least I was on the wait list. If a spot opened up, we could have a conversation about it.


When it comes to treatment, you do have a say. Your doctor may have a recommendation, but you have a say in what your treatment plan is going to be. You can tell them if you want an alternative.
A lot of people are intimidated, so they don’t want to tell their doctor what to do. It’s important to remember that your doctor is working for you. Find someone who’s working for you. My oncologist definitely was working for me.
Future Treatment Plans
My cancer is still growing. At any time, I can say I want to try something different. My oncologist and I have had those conversations. Because I’m on a trial, it’s not going to last forever. Unfortunately, I can’t be on this for the next five years. Having been off chemo, I’m hesitant about going back to it. I wanted to find out if there were non-chemo options we could explore, so we’ve talked about other options that are on the table.
With cancer, a lot of times, people sit and suffer in silence so by the time symptoms start rearing their big ugly heads, it’s often in the advanced stages.
Words of Advice
Know your body and trust your body. If something changes and there’s no warrant for that change, talk to your doctor. Don’t talk to your friends. Don’t go to social media. For everyone else, it might be normal, but if it’s not normal for you, it does warrant a conversation with your doctor. If it turns out to be nothing, you’re not out that much. I don’t think any doctor’s going to be mad that you wasted their time coming to them with your concern. Get rid of that fear. Know your body and know what’s normal for your body.
If anything comes up abnormal, don’t be afraid to go to your doctor and advocate for yourself. Tell them you want to find out what’s going on. With cancer, a lot of times, people sit and suffer in silence so by the time symptoms start rearing their big ugly heads, it’s often in the advanced stages.
People ignore the early symptoms. Maybe they’re busy, maybe they’re afraid, but I think primarily it’s because people think it’s not a big enough issue to warrant seeing a doctor. If it’s not normal for you, speak up and say something. The best thing that could happen is they tell you it’s nothing. The worst thing that could happen is they tell you it’s something, but maybe they found it before it’s something big and problematic.


Inspired by Amy's story?
Share your story, too!
More Colon Cancer Stories
Nicole S., Colon Cancer, Stage 3
Symptoms: Dull lower abdominal pain that sharpened and was focused on the lower left side, appearance of dark blood in stool, difficulty retaining food due to near-complete blockage of sigmoid colon
Treatments: Surgery (colectomy), chemotherapy
Ian D., Colon Cancer, Stage 3C
Symptoms: Fatigue, unusual blood test results during annual physical, blood in stool
Treatments: Surgery (partial colectomy), chemotherapy, clinical trial
Lauren G., Colon Cancer, Stage 4
Symptoms: Frequent urges to have bowel movements (up to 27x/day), incomplete evacuation, abdominal bloating
Treatments: Surgeries (colectomy, colostomy bag placement), chemotherapy
Jackson A., Colon Cancer, Stage 3
Symptom: Sharp abdominal pain
Treatment: Surgery (emergency transverse colectomy)
Jay W., Colon Cancer, Stage 4
Symptom: Occasional presence of blood in stool
Treatments: Chemotherapy, surgery (installation of port and liver infusion pump, colectomy, hepatectomy, liver ablation, removal of liver infusion pump)
Kelly C., Colon Cancer, Stage 4
Symptoms: Constipation, bloating, severe abdominal pain
Treatments: Surgeries (colectomy, colostomy, hepatectomy), chemotherapy