Matthew’s Stage 4 Pancreatic Cancer Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

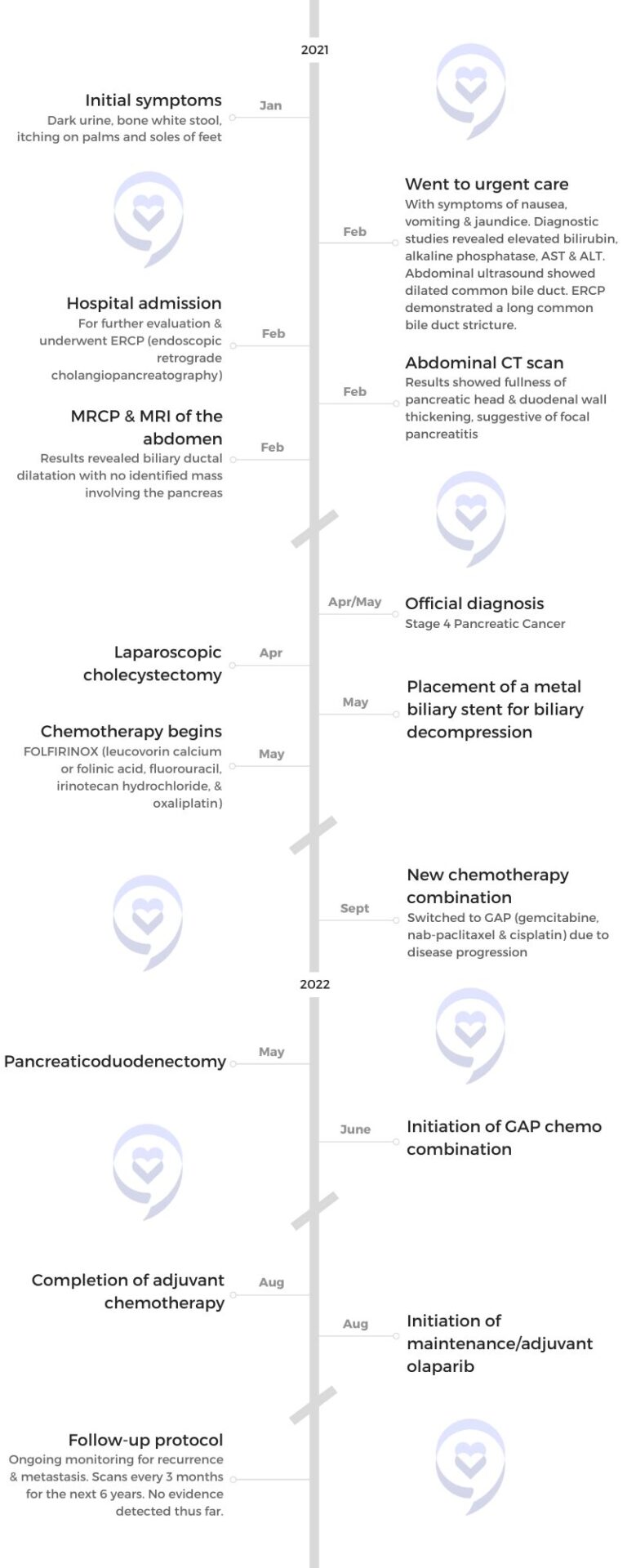
Initially misdiagnosed due to overlapping symptoms with his existing condition, Matthew experienced concerning symptoms such as dark urine, pale stool, and intense itching. Eventually diagnosed with metastatic pancreatic cancer, Matthew underwent different combination chemotherapy treatments, including FOLFIRINOX (leucovorin calcium or folinic acid, fluorouracil, irinotecan hydrochloride, and oxaliplatin) and GAP (gemcitabine, nab-paclitaxel, and cisplatin).
Despite setbacks and the grim prognosis associated with pancreatic cancer, Matthew’s tumor responded positively to the new chemotherapy regimen, leading to tumor shrinkage and the disappearance of metastases in the liver. Following a successful Whipple procedure, Matthew emphasizes the importance of not being defined by statistics and advises others facing similar challenges to live life to the fullest while also taking their health seriously.
His story highlights the unpredictable nature of cancer treatment, the importance of advocating for oneself in medical settings, and the significance of cherishing each moment, even in the face of adversity.
In addition to Matthew’s narrative, The Patient Story offers a diverse collection of cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
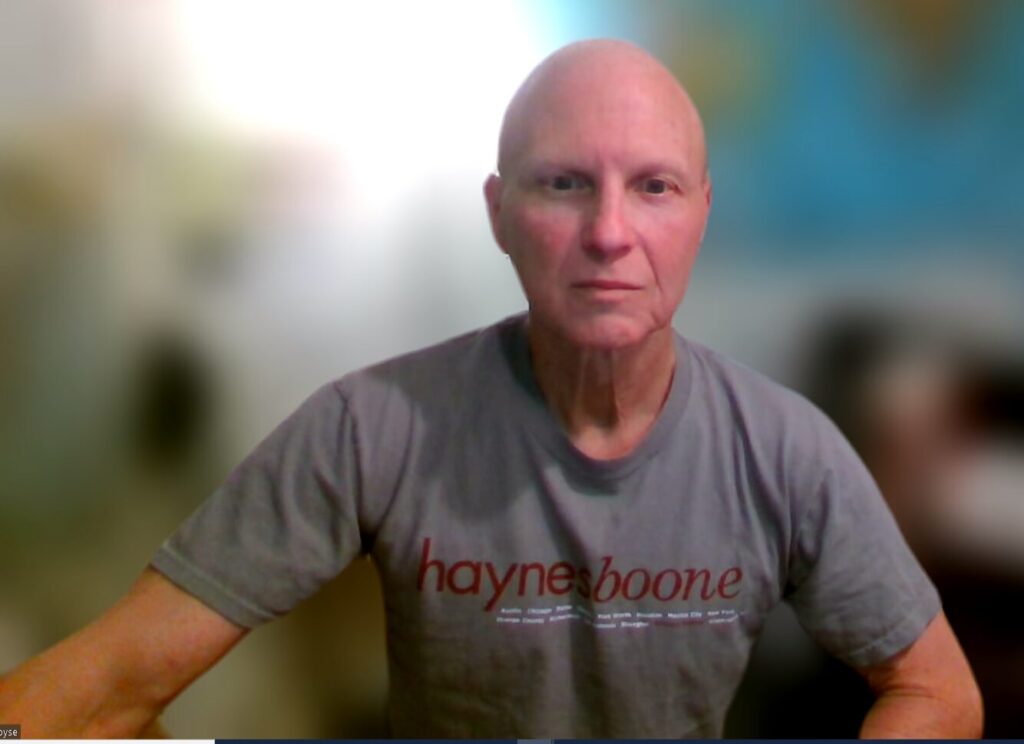
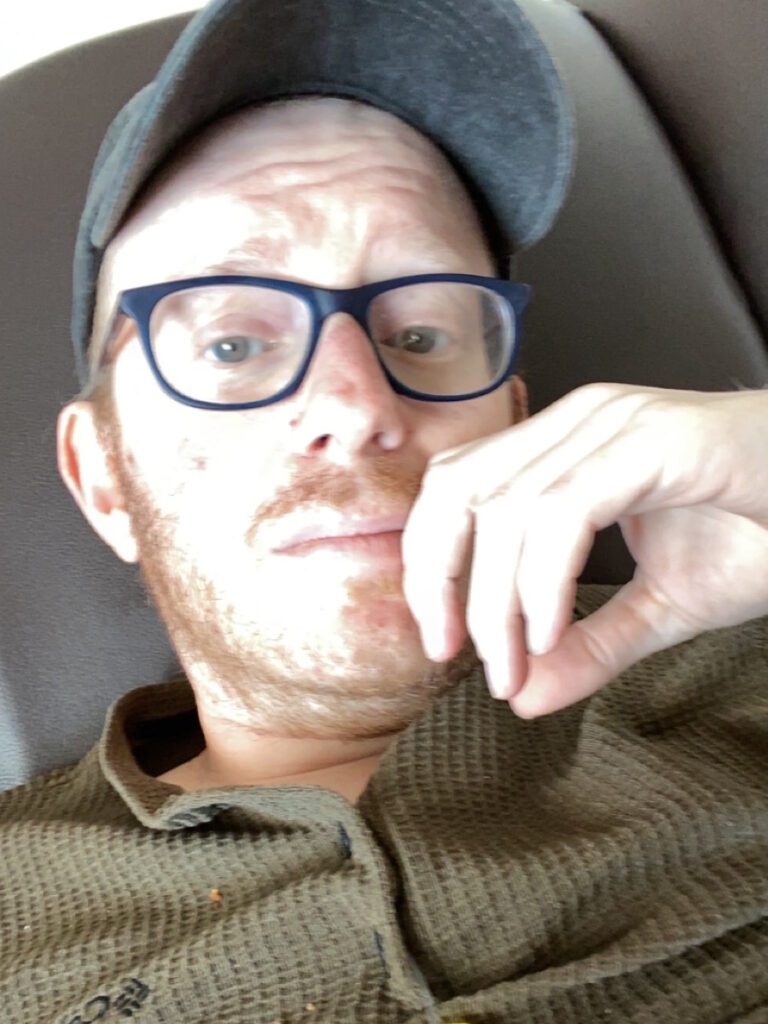
- Name: Matthew R.
- Diagnosis:
- Pancreatic cancer
- Staging:
- 4
- Initial Symptoms:
- Dark urine
- Bone white stools
- Itching on palms and soles
- Treatment:
- Chemotherapy: FOLFIRINOX, GAP
- PARP inhibitor: olaparib
- Surgeries: cholecystectomy, pancreaticoduodenectomy (Whipple procedure)

Introduction
I live in Hazel Park, Michigan, with my girlfriend Natalie and our pug Monique. Because of the nature of my illness, I haven’t had a job in three years, but in my former life, I was finishing a PhD. I was going to be an academic.


Pre-diagnosis
Initial Symptoms
The most popular narrative surrounding pancreatic cancer is that not only is it very lethal but also very difficult to diagnose. The pancreas is deep in the body. The earlier symptoms are very nuanced, can go unnoticed, and can also be misdiagnosed as a multitude of other things. By the time you’re experiencing symptoms, the cancer has spread outside of the pancreas. I don’t want to say it’s too late, but that’s what conventional wisdom is.
I was diagnosed with Crohn’s disease when I was 25. Gastrointestinal distress, which is one of the more perceptible symptoms of pancreatic cancer, was par for the course for me. I probably wouldn’t have noticed even if I didn’t have Crohn’s. I lost some weight over the months, but it wasn’t until late January 2021 that I started to experience starkly distinct symptoms.
It was the COVID pandemic. I lost my job and moved to a different city to help my friend with his business. His business closed and he moved away, so I was alone when all this started.
I had dark urine and bone-white stool. I didn’t even notice the stool color for a while. At first, I thought I was hungover. I had a few beers the night before so I drank some Gatorade and lay in bed, but the urine did not get lighter.
My skin started to itch. The bathroom symptoms were pretty jarring, seeing urine that dark and poop that pale, but the itching was probably the worst. The palms of my hands and the bottoms of my feet itch. It was worse at night. I never felt anything like it before and those are hard places to scratch.




After a whole night of itching, I put my hands and feet in the tub under hot water to numb the sensation. In retrospect, it’s jarring to think about burning my hands and feet to alleviate the pain, but the itching was that significant.
Not everyone gets the itchiness. There seems to be some controversy because not every pancreatic cancer awareness campaign includes itchiness. I experienced it and it was horrible.
When something started to happen, I sat on it for 48 hours before I finally told someone. It wasn’t the most responsible, but in retrospect, not that bad. I was in a long-distance relationship with a woman I knew from graduate school. I told her and she said, “You should go to the doctor.”
I have a lot of medical anxiety. I have never been a good patient. For someone with such anxiety about doctors and hospitals, I needed someone to tell me.
Going to Urgent Care
I had recently moved to Durham and didn’t even have health insurance, but I went to an urgent care center. My blood test results showed that my bilirubin was high. We get some more tests back. The nurse said, “You don’t have a doctor here yet and these test results are troubling. You should go to the ER.”
Going to the Emergency Room
I went home to sleep because I hadn’t slept in three nights. I was so tired that despite the itching, I passed out. Early the next morning, I went to the ER and that was the beginning of my journey.
They admitted me to the hospital and ran some more blood tests to see what was going on with my liver enzymes. They did an ultrasound and an endoscopic ultrasound.


Bile Duct Stricture
They found that there was a stricture in my bile duct. Your liver produces bile, a digestive enzyme stored in your gallbladder and then released into your small intestine to digest fats and other foods. The tube that brings the bile down goes through the head of your pancreas. That tube had a stricture, so it was closed off. When bile can’t be distributed normally, you end up depositing it in your blood and your flesh, and that causes jaundice and elevated liver enzymes.
With the endoscopic ultrasound, they were able to place a stent in my bile duct in the hope that it would stretch it out. They told me to come back in a few weeks to have another endoscopy and remove the stent.
There was no sense of urgency. I was an otherwise healthy person with a history of colitis. They didn’t think that this was anything scary.
After they removed the stent, the symptoms came back, so they decided that it was my gallbladder causing the symptoms. With pancreatic cancer, it’s very common for people to assume that it’s a gallbladder issue. They decided to take my gallbladder out. After the surgery, the symptoms return.
It was late April. I went to my gastroenterologist’s office, who was the one who did the endoscopy. She said, “I don’t know what’s happening, but you for sure don’t have cancer. We have done so many brushings and you definitely don’t have cancer. If you have cancer, I will roll over in my grave.” I left her office feeling pretty confident.


Diagnosis
Getting the Official Diagnosis
Three hours later, I got an automatic notification on my phone from MyChart. One of my cytology reports came back. It said adenocarcinoma. I didn’t know what that meant, but I knew it wasn’t good.
I sat with that for about two hours. Then the surgical oncologist who did my gallbladder surgery called me. My case got automatically referred back to him. He was out of town and called me using his personal cell phone.
I told him, “This lady told me I definitely did not have cancer and now I do so I’m freaked out,” and he apologized. My surgeon is the salt of the earth. He calmed me down. I don’t know if he remembers it this way, but I’ll never forget this conversation. He said, “If this is cancer, the tumor’s very small and I should be able to get this. I’m confident.”

The area in which they found the adenocarcinoma is called the ampulla of Vater. Everything in this part of the body is pretty small and overlapping so pancreatic cancer could be an explanation. But given my age and, let’s face it, the taboo around death, no one was talking about that.
When pressed, the doctor told me ampullary cancer, which has a higher survival rate and is still incredibly rare for someone my age but less rare than pancreatic cancer in the same age category.
Treatment
Discussing the Treatment Plan
Because of the size and the layout of this part of the body, they do the Whipple procedure, also called the pancreaticoduodenectomy. They do the same surgery for ampullary cancer as they do for pancreatic cancer.
Five days after the phone call, I was in his office and he said, “I’m going to remove part of your pancreas and part of your small intestine.” I didn’t have a gallbladder, but that also would have gone including part of my stomach.
My surgeon told me that they cut me open and, contrary to what they thought, found a tumor on the head of my pancreas that had spread outside of the pancreas. Metastatic pancreatic cancer is considered inoperable so when they saw that, they closed me up.



Because of my age and because they suspect that I’m a BRCA2 mutation carrier, the surgeon said, “We have to confirm with genetic tests, but I’m pretty sure you have this particular genetic abnormality. If that’s the case, then there are targeted therapies that might work for you.”
He said, “This is a mean cancer. But because of your particular situation, after treatment, we might be able to try the surgery again in a year.” For pancreatic cancer, surgery is the only long-term survival solution. Chemotherapy and radiation are life-extending, but they’re not curative. He was pretty confident, at least in the context of a lethal diagnosis.
Later that day, he introduced me to my oncologist. He was not as confident. When pressed, he said, “With treatment, you might have 1 to 3 good years left, but that’s it.”
FOLFIRINOX Chemotherapy
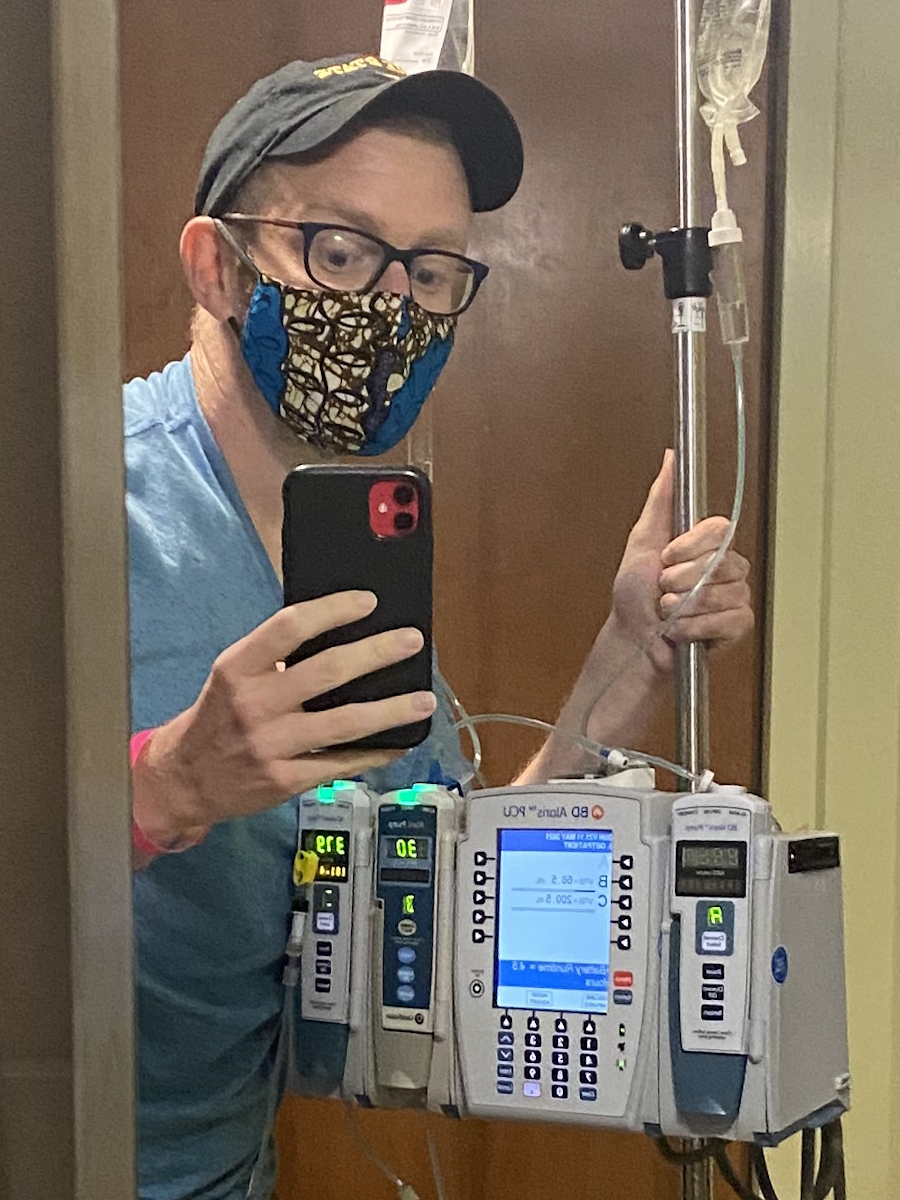
This was at the beginning of May 2021. My wound had to heal. Three weeks later, I started chemotherapy. Like a lot of other people with metastatic pancreatic cancer, I was given FOLFIRINOX, which is five different drugs. It’s awful. Chemo combinations are all awful, but FOLFIRINOX was really, really abrasive.
I had a scan after three months on FOLFIRINOX. The oncologist said, “Your tumor shrank a little bit,” but you can tell from the way he’s telling me that it could be an imaging error or a minute retreat that it’s barely perceptible.
At my next CT and MRI three months later, the tumor grew. It had metastasized to my liver so things were not looking good. At this point, I was not confident that I would be a special case or a miracle. I thought this was it.


Switching Chemotherapy Regimens
My oncologist switched me to a different chemotherapy combination. He told me there was a combination that some researchers found was promising for people in my situation. It was gemcitabine, nab-paclitaxel, and cisplatin (GAP).
I was honestly relieved because after being on FOLFIRINOX for almost six months, the neuropathy had gotten so bad that I couldn’t get out of a chair by myself. I needed someone to hoist me up. I was pretty thin at this point. It was miserable.
On the new chemotherapy regimen, my quality of life improved dramatically. By the time my first set of scans came around three months in, some of the spots on my liver had started to disappear. I did three more months of chemo and made it through.
I didn’t lose my hair. I’m six feet tall. I was 215 lbs when I was diagnosed and miraculously maintained a healthy weight so I’m very thankful for that. At this point, I thought I was still dying sooner rather than later so I was trying to have fun and it certainly made having fun a lot easier.


Post-Treatment Scans
In March 2021, he looked at my scans and, if memory serves, they could not identify cancer outside of the tumor.
Almost a year to the day, they attempted to do the Whipple and, this time, it was successful. When Dr. Allen came into my hospital room, he said all of my margins were good and the lymph nodes they tested were negative.
Before this, they couldn’t see any cancer on the CT or MRI, but that didn’t mean that my peritoneum wasn’t covered in cancer. That just meant that they wouldn’t be able to tell until they got in there. They were pleasantly surprised that things had worked.


Follow-up Protocol
The last scan was a lot smoother than the others, but they’re incredibly difficult. I get a scan every three months for the next six years, but the chances of me living out those six years are astronomically small. Pancreatic cancer has a remarkably low five-year survival rate. It’s unlikely that I will see all of that time, at least on paper.
Words of Advice
It’s important to remember that you are not a statistic. I was diagnosed with something I wasn’t supposed to have at my age. It was very unlikely. It was supposed to kill me and I didn’t die so, in a sense, I beat the odds not once, but twice.
People think that pancreatic cancer is an old person’s disease. I think that’s why no one ever looked because no one ever even thought that I could have pancreatic cancer. I’ve heard over and over again that I’m too young. Statistically speaking, they’re correct. For people under 35, it’s incredibly rare, but there is a difference between statistical analysis and what statistics are for, and encountering a patient one-on-one.
Treatment is not linear. Pancreatic cancer is often thought of in linear terms as a quick, short trajectory to death. We assume that if treatment will work, it will work immediately. You don’t take one step back and one step forward. In my experience, that’s not true. Sometimes things get worse before they get better and it’s not a reason to lose heart.
Have a drink, eat the cheeseburger, and live your life to the extent that you can. That’s how I lived. Take your health seriously but also meet yourself where you are.





Inspired by Matthew's story?
Share your story, too!
More Pancreatic Cancer Stories
Burt R.
Symptoms: None; found the cancers during CAT scans for internal bleeding due to ulcers
Treatment: Chemotherapy (capecitabine + temozolomide), surgery (distal pancreatectomy, to be scheduled)
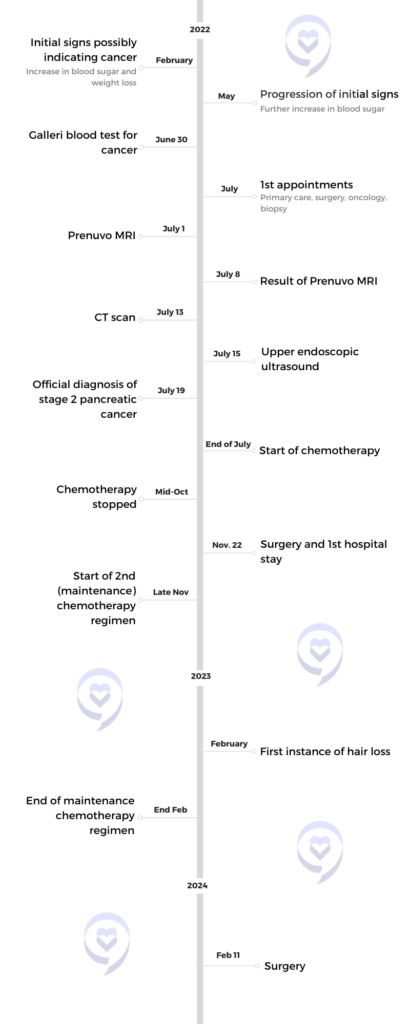
Roger R., Pancreatic Cancer, Stage 2
Cancer Details: Found after Galleri blood test and MRI
1st Symptoms: None
Treatment: 5FU (folfirinox), Gemzar, NK cell expansion therapy, Dendritic cell expansion therapy, Neoantigen peptide vaccine
Matthew R., Pancreatic Cancer, Stage 4
Symptoms: Dark urine, bone white stool, itching on palms and soles
Treatment: Chemotherapy, surgery