Common Chronic Lymphocytic Leukemia (CLL) Symptoms, Described by Real Patients

Many people who are diagnosed with Chronic Lymphocytic Leukemia (CLL) are surprised to discover they have the disease because they often don’t have symptoms. In fact, most cases of CLL are diagnosed following a routine CBC blood test.
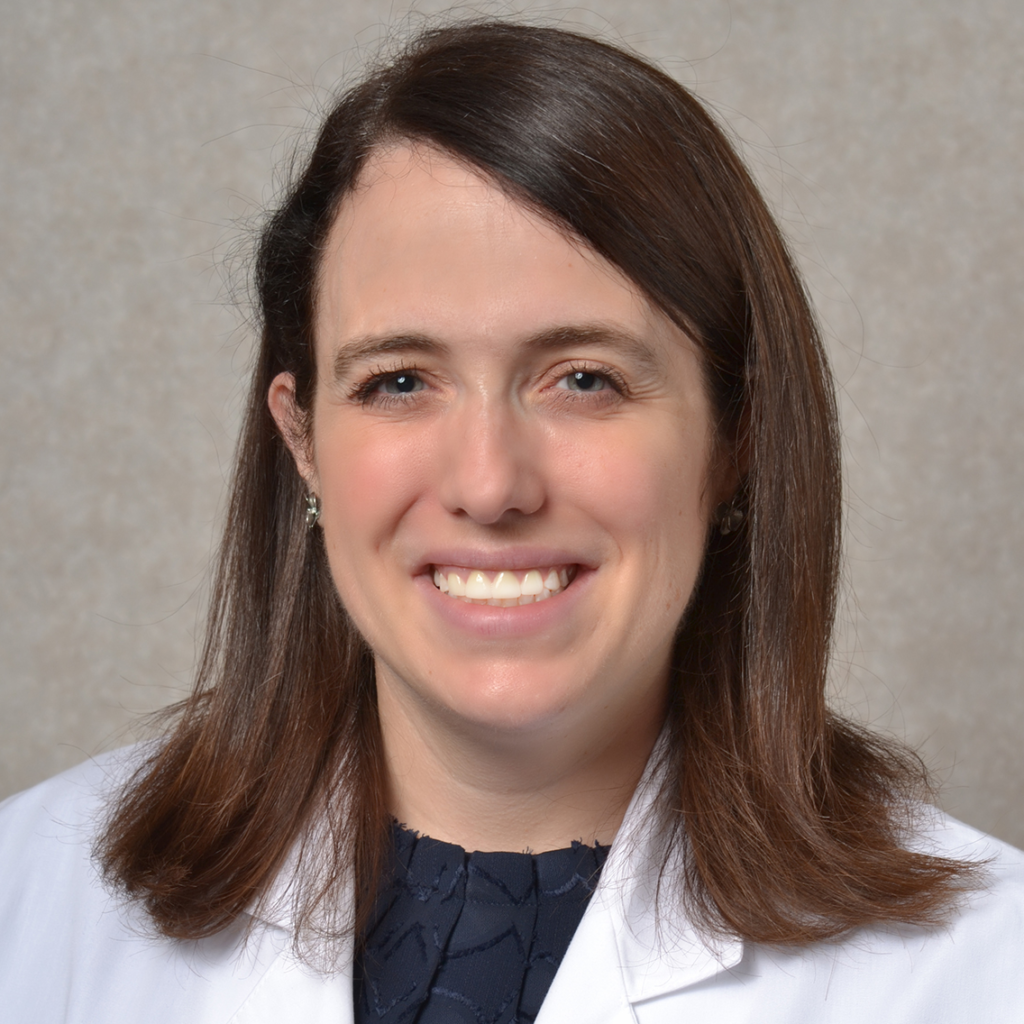
Patients often describe flu-like symptoms, including fatigue and fever, before being diagnosed with CLL.
In this post, we look at some of the symptoms of Chronic Lymphocytic Leukemia and how real-life patients first experienced those symptoms.
First signs and symptoms of CLL
- Weakness
- Swollen lymph nodes
- Enlarged spleen or liver
- Extreme fatigue
- Unexplained weight loss
- Chills
- Fever
- Abnormal Range of Red Blood Cells, White Blood Cells, and Platelets
- Night sweats
- Bleeding or bruising
- Lingering or recurrent infections
Swollen Lymph Nodes
Patients with CLL often experience swollen lymph nodes in their neck or underarms. This is caused by the multiplication of abnormal lymphocytes that collect in the lymph nodes.
I was feeling the back of my neck and noticed a lump. I went to the walk-in center and they said, “You must be fighting a virus. A lot of people get swollen lymph nodes. It’s really nothing.”
Susan K.
I felt a lump in the back of my neck. I thought this was a muscle knot and kept trying to rub it out. It got bigger.
Tony D.
Enlarged Spleen or Liver
Many CLL patients experience stomach pain or tenderness due to a swollen spleen. The role of the spleen is to filter blood by breaking down worn-out red blood cells. With CLL, your spleen may become so clogged with abnormal cells that it swells. Similarly, an enlarged lymphocyte count may result in a patient’s liver swelling.
I was frankly puzzled by this shoulder [pain]. Much later, when I finally connected with the doctor at UT Southwestern, he said, “Oh, well, I’ll tell you what that was. It was your spleen. The nerve pathways from the spleen and your shoulder travel together. We call it referred pain. Your spleen is really in an uproar, but it’s not going to hurt down there. It hurts up here. I have other patients with the same problem.”
Bill M.
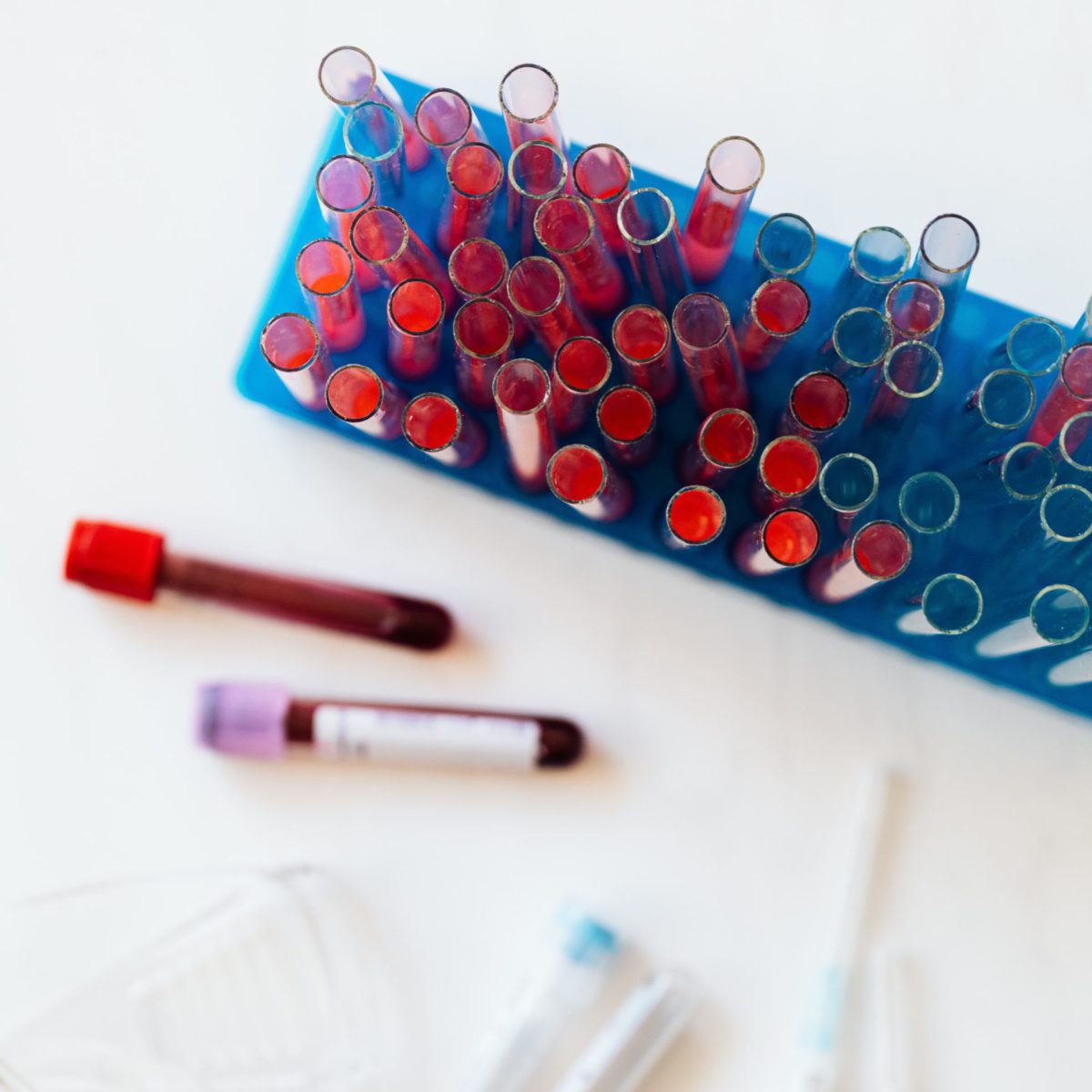
Abnormal Range of Red Blood Cells, White Blood Cells, and Platelets
As CLL continues to advance, it replaces the bone marrow’s normal blood-making cells with abnormal leukemia cells. As a result, your blood cell count may be thrown off in a number of ways. These include:
- Anemia – a shortage of red blood cells resulting in tiredness or shortness of breath
- Leukopenia – a shortage of white blood cells that may result in
- Lymphocytosis – an extremely high number of white blood cells that don’t function properly.
- Thrombocytopenia – a shortage of blood platelets that can lead to bruising, bleeding, or frequent nose bleeds.
The number of blood cells and platelets is determined through a simple blood test. Your doctor will want to get an initial read on these numbers upon diagnosis and during CLL treatment.
I had seen my general practitioner (GP), and she informed me that I had a high white blood cell count. My response was, “Well, I don’t remember a time where a doctor hasn’t said that to me, and they always followed it up with, ‘Look, it’s nothing. You probably have a little infection getting started, or maybe you’re nervous about being here.’”
Hannah D.
We were tracking my white blood cell count and fatigue primarily. In 2014, my white blood cell count had doubled within a 6-month period.
Lacey B.
Extreme Fatigue
Many patients with CLL experience extreme fatigue when they have the disease. This fatigue is the result of either increased inflammation or a lack of red blood cells to carry oxygen throughout the body.
I can usually stick it out, have an extra cup of coffee, maybe throw down a chocolate bar or something like that, and get everything done that I needed to get done. Now, sometimes I go, ‘This is going to have to wait because I don’t have enough gas in the tank”
Jeff F.
So when I talked to doctors and describe the fatigue, they asked me what my lifestyle is. And they said, “Well, you just went out for a hundred-mile bike ride. You’re going to feel a little fatigued.”
Stephen B.
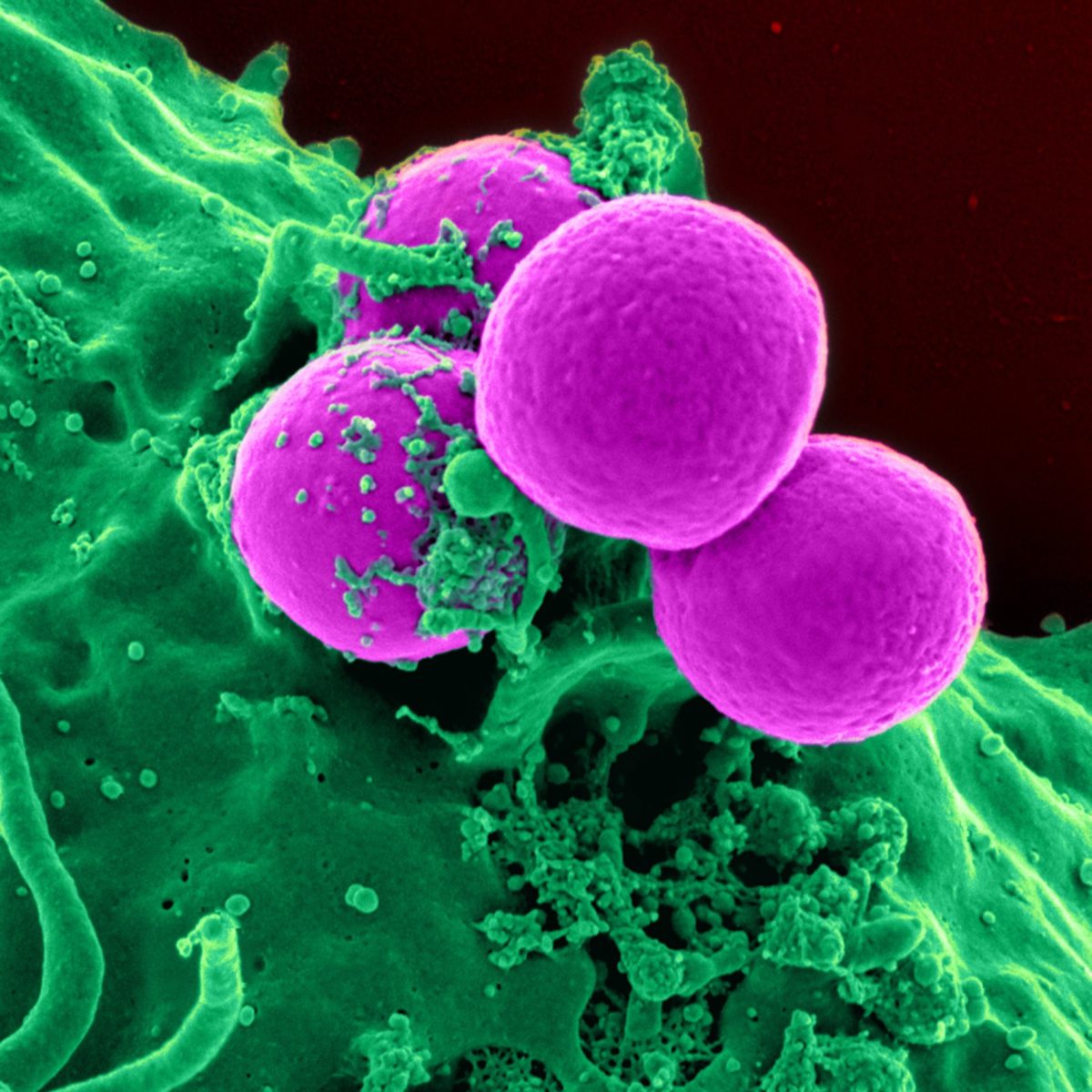
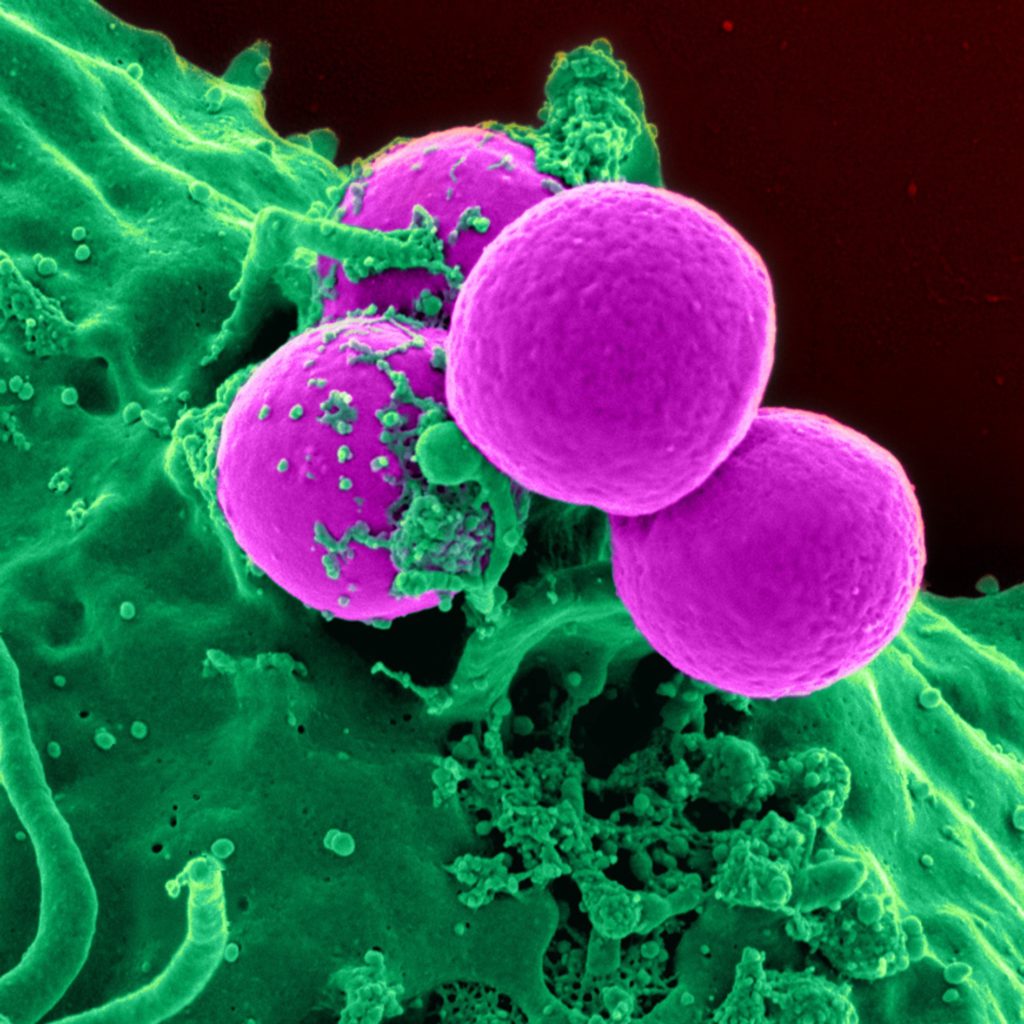
Lingering or Recurrent Infections
Patients with CLL have a compromised immune system, making them more susceptible to getting infections. In addition, people with CLL have a more difficult time fighting infections once they get them.
This susceptibility is caused by CLL’s impact on B-lymphocytes. Since the b-lymphocytes are abnormal, the body is unable to create antibodies.

I just kept getting sick. I would catch a cold, and it wouldn’t go away. I would get a flu or sinus infection. It just lasted forever. These are all really common things now that I know about CLL. These are really common things and signs for someone to look at and put all together that you have something.
Michele N.
Night Sweats
Experiencing night sweats is another common symptom of CLL. Night sweats are a sign that your body is attempting to fight the disease by raising your internal temperature to rid the body of the disease.

I just kept getting sick. I would catch a cold, and it wouldn’t go away. I would get a flu or sinus infection. It just lasted forever. These are all really common things now that I know about CLL. These are really common things and signs for someone to look at and put all together that you have something.
Jeff F.
Bleeding or Bruising
The final frequent symptom of CLL is frequent or excessive bleeding and easy bruising. Bleeding may come in the form of frequent nose bleeds or scrapes.
Bleeding and bruising in CLL patients are the result of not having enough platelets to clot your blood and stop you from bleeding. The lack of platelets may be a direct result of the disease or not having enough room in your bloodstream due to an increase in white blood cells.
I started bruising very easily in my early 40s. When my husband first met me, he said, “You’re like a banana,” because I always had maybe about 20 bruises on my legs at any given time. I had to hold my shopping bags out to the side because if they touched my leg, I would bruise.
Leesa T.
What to Do If You’re Experiencing CLL Symptoms?
If you’re experiencing any of the above symptoms with regularity, it’s best to consult your doctor. While these symptoms may be signs of other illnesses it’s best to do a blood test to monitor for any issues. Catching any type of cancer as early as possible is key to effectively managing and treating the disease.
CLL Patient Stories
Lynn S., Chronic Lymphocytic Leukemia (CLL)
Symptom: Elevated white blood cell count
Treatments: Chemotherapy, targeted therapy (BTK inhibitor)
Serena V., Chronic Lymphocytic Leukemia (CLL)
Symptoms: Night sweats, extreme fatigue, severe leg cramps, ovarian cramps, appearance of knots on body, hormonal acne
Treatment: Surgery (lymphadenectomy)
Margie H., Chronic Lymphocytic Leukemia
Symptoms: Large lymph node in her neck, fatigue as the disease progressed
Treatment: Targeted therapy
Nicole B., Chronic Lymphocytic Leukemia
Symptoms: Extreme fatigue, night sweats, lumps on neck, rash, shortness of breath
Treatments: BCL-2 inhibitor, monoclonal antibody
References
American Cancer Society. Signs and Symptoms of Chronic Lymphocytic Leukemia. Accessed at https://www.cancer.org/cancer/types/chronic-lymphocytic-leukemia/detection-diagnosis-staging/signs-symptoms.html on November 22, 2023.
Goldman D. Chronic lymphocytic leukemia and its impact on the immune system. Clin J Oncol Nurs. 2000 Sep-Oct;4(5):233-4, 236. PMID: 11111455.
Leukemia & Lymphoma Society. CLL Signs & Symptom. Accessed at https://www.lls.org/leukemia/chronic-lymphocytic-leukemia/signs-and-symptoms on November 21, 2023.