CBC Tests and Cancer: What Doctors Look For in Your Results
A complete blood count test (CBC) is a blood test used to help monitor your overall health. In some instances, CBC tests are also used to help diagnose and track certain forms of cancer, like leukemia and Hodgkin’s or non-Hodgkin’s lymphoma.

A complete blood count test measures:
- Red blood cell count (RBC)
- White blood cell count (WBC)
- Platelet count
- Hemoglobin (Hg or Hgb)
- Hematocrit
- Mean corpuscular volume (MCV)
In this post, we look more into a CBC test, including how it is taken, what your results mean, and how it helps diagnose and monitor different forms of cancer and treatment.
How Do I Understand My CBC Test Results?
When you receive your CBC test results, you often receive a report with a bunch of abbreviations and numbers that don’t make sense to the average person; however, once you understand what the abbreviations mean.
In a complete blood count, you’re getting a bunch of information. There are three main types of blood cells that we’re looking for.
Dr. Kamran Mirza | Read More about what doctors look for in a CBC test.
White Blood Cell Test Results
White blood cells are your body’s primary defense mechanism. They help remove foreign materials and cellular debris, destroy infectious agents and cancer cells, and help produce antibodies.
A CBC test typically provides the results of two white blood count measurements:
- White blood cell count – the measurement of the total number of white blood cells in your blood count.
- White blood cell differential – the number of each type of white blood cell in your blood sample. The five types of white blood cells are neutrophils, lymphocytes, monocytes, eosinophils, and basophils.
Red Blood Cell Test Results
Red blood cells perform the essential function of delivering oxygen from your lungs to other parts of your body, along with transporting waste like carbon dioxide out of the body.
A typical CBC test provides results for 4 different types of red blood cell measurements:
- Red blood cell count – the number of red blood cells in a blood sample.
- Hematocrit – the percentage of your blood made up of red blood cells.
- Hemoglobin – the amount of hemoglobin that is in your blood. Hemoglobin is the protein in your red blood cells that transports oxygen throughout the body.
- Mean corpuscular volume (MCV) – measures the size of your red blood cells. Irregular red blood cell sizes may be a sign that something is wrong.
Platelet Test Results
Platelets play an important part in forming blood clots to stop you from bleeding. The only measurement a CBC test provides for platelets is the total number of platelets in your blood sample.
What are the Average CBC Test Results?
Now that you know what each test measures, you may wonder, what are the average measurements for each test? When you receive your blood test results, the test usually provides the value you got, the reference range, and if your results fall within that range.
According to the National Cancer Institute, the normal CBC test results are:
| Test | Unit of Measurement | Normal Values |
| Erythrocytes (RBC) | X 1,000,000/mm3 | Male: 4.5 – 6Female: 4.3 – 5.5 |
| Hematocrit | Percentage | Male: 38 – 51%Female: 36 – 47% |
| Hemoglobin | g/dL (grams per deciliter) | Male: 14 – 17 Female: 12 – 16 |
| Platelets | X 1,000/mm3 | 200 – 500 |
| Leukocytes (WBC) | X 1,000/mm3 | 5 – 10 |
If your counts fall outside the normal range, it doesn’t necessarily mean that anything is wrong or you have cancer. However, your doctor will probably investigate further if you receive an abnormal result.

I get really cranky and crabby. Sometimes I’ll go to my primary care doctor to do a CBC just so I can see, “Okay, this is good. No surprises.” It makes me feel better, and he’s more than happy to do it.
Sheryl B | Read more about how CBC tests can help monitor cancer.
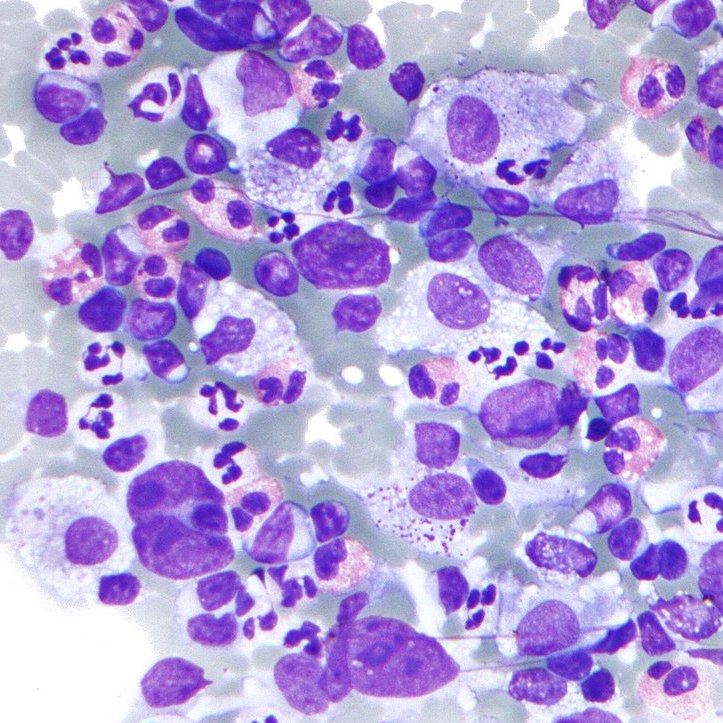
Can Cancer be Detected from a Blood Test?
Specific forms of cancers can be detected as part of a CBC result. However, it’s important to note that a CBC test is only one tool when diagnosing cancer. Just because you have abnormal CBC test results does not necessarily mean you have cancer.
The different types of cancers that a CBC test can detect include:
- Leukemia – According to the American Society of Hematology, abnormal levels of white blood cells and low levels of red blood cells may indicate leukemia.
- Hodgkin Lymphoma – An individual with anemia (low red blood cell count) and a high white blood cell count may have Hodgkin Lymphoma according to the American Cancer Society,
- Non-Hodgkin Lymphoma – Low levels of red blood cells, hemoglobin, platelets, and neutrophils may indicate a patient has non-Hodgkin lymphoma according to Lymphoma Action,
- Multiple Myeloma – Those with anemia and decreased platelet and white blood cell counts may have myeloma.
- Essential Thrombocythemia (ET) – Patients may have an abnormally high platelet count.
- Polycythemia Vera (PV) – According to the Mayo Clinic, patients with a high red blood cell count and an elevated hematocrit measurement may have PV.
- Myelofibrosis – Patients with low red blood cells and potentially increased platelet, hemoglobin, and white blood cell counts may have Myelofibrosis according to Cancer Research UK.
It’s important to remember that a CBC test is not the only diagnostic tool or blood test used to diagnose cancer. Therefore, a diagnosis cannot be made solely based on the results of a CBC test.

One of the things I didn’t know until I spoke to my doctor is that he asked me to always let him know when we did CBCs if I had exercised before or a day before. In many cases, exercise increases your white cell counts.
Jeremy S | Learn more about how CBC tests might be impacted.
Can Cancer Treatment Impact Blood Test Results?
Cancer treatment can impact your CBC test results. Some care teams may use a CBC test to track how treatment may affect you. The forms of treatment that can impact your CBC test results include:
- Chemotherapy – May lower your white blood cell, red blood cell, and platelet counts.
- Surgery – Your red blood cell count may be low following surgery.
- Radiation therapy – May lower your red blood cell and platelet counts.
While these are just the general forms of treatment that may impact your CBC test results, cancer-specific treatments and drugs may also affect your results.
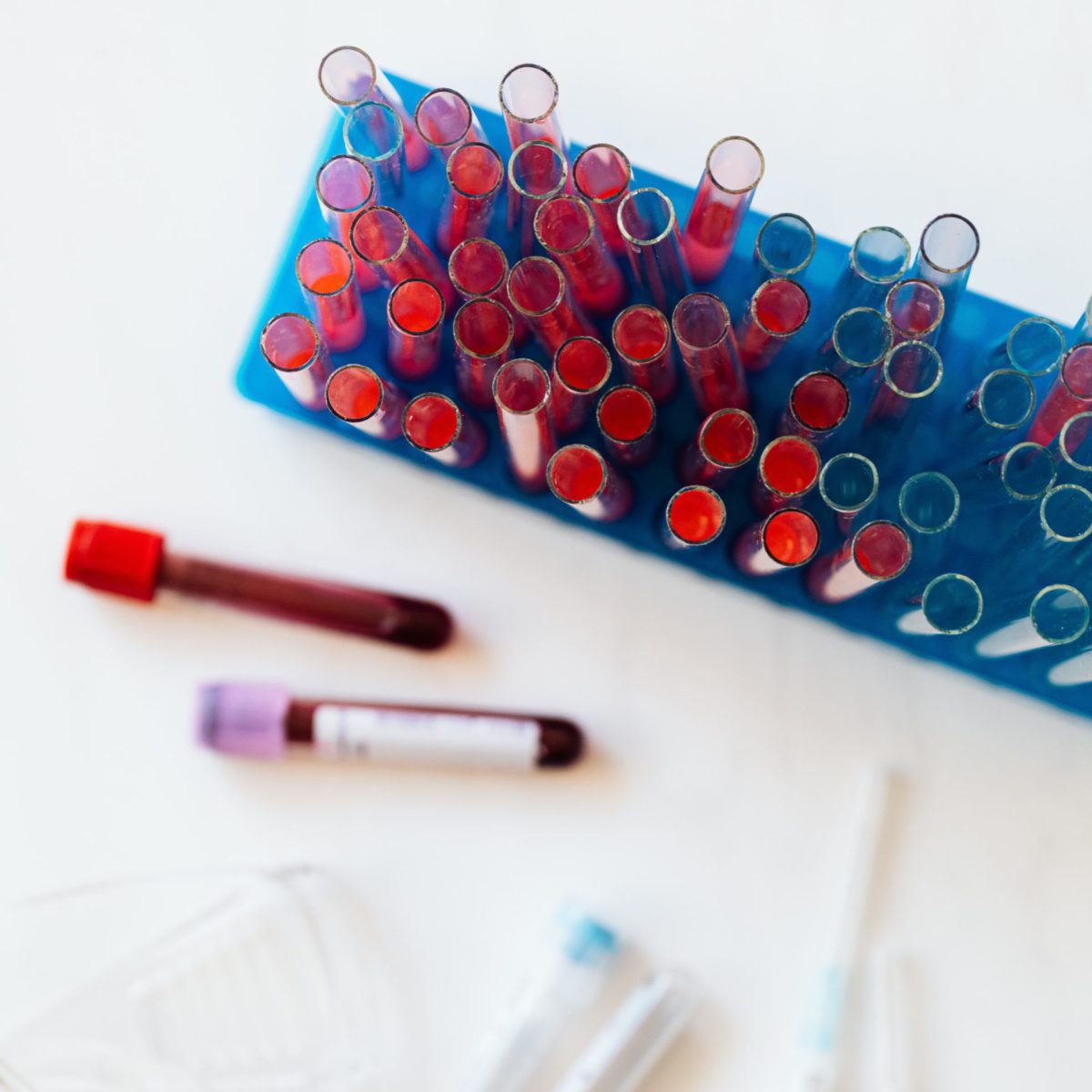
How is a CBC Test Taken?
You may not even notice, but a CBC test is typically part of the routine blood work you get for your annual physical. The test is taken by simply withdrawing a small vial of blood to be tested in a lab.
Due to its ease and accessibility, the CBC test is a great way to continuously screen for cancer.
Learn More About CBC Tests
Visit our navigating cancer page if you want to learn more about CBC tests or cancer in general. There you will find resources from dealing with a cancer diagnosis to information about the latest treatments.