Andrea’s Stage 3 Colorectal Cancer Story
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez

Andrea, a nurse practitioner from Spokane, WA, got through stage 3 colorectal cancer.
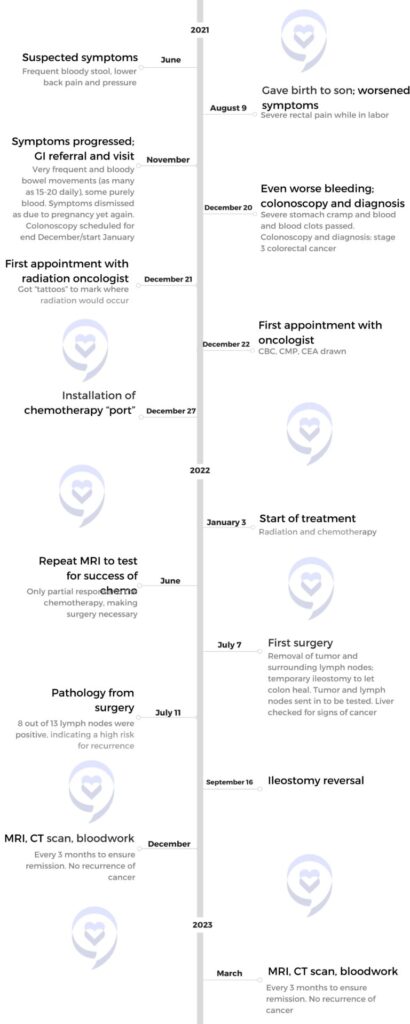
Andrea’s symptoms began when she was about 7 months pregnant with her son—bloody stool and lower back pain and pressure, progressing to more serious symptoms like rectal pain during childbirth and as many as 20 bloody bowel movements daily—but she was consistently told that they were due to her pregnancy. A colonoscopy, done after the symptoms progressed significantly and her husband was able to get some help, finally diagnosed her stage 3 colorectal cancer.
Treatment–chemotherapy, radiation and surgery–as well as a lot of support, a can-do attitude, and self-advocating, eventually helped Andrea get better. Her story isn’t without some twists and complications, though, most especially an agonizing period during which she thought her colorectal cancer might have progressed to stage 4. Thankfully, this was a false alarm: she was actually already cancer-free, and she remains so to this day.
In addition to Andrea’s narrative, The Patient Story offers a diverse collection of stories about colorectal cancer. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Andrea P.
- Diagnosis:
- Colorectal cancer
- Staging:
- Stage 3
- Initial Symptoms:
- Frequent bloody stool
- Lower back pain and pressure
- Rectal pain
- Severe stomach cramps
- Treatment:
- Chemotherapy: 5-FU
- Radiation treatment
- Surgery

This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
… I was chosen to go through this fight so I could help bring awareness to other people.
We were chosen for a reason, and we need to be strong through this fight.
Introduction

I’m Andrea, I’m from Spokane, WA. I’m 34 years old.
I am a nurse practitioner. I was a nurse for a long time, going on about ten years. And then I went to nurse practitioner school, and now I’m a nurse practitioner in the emergency department. I also was a nurse educator for some time, so I taught nursing students.
I’m married; my husband is a nurse anesthetist who works at one of the local hospitals. We have two beautiful kids: our daughter is going on 5, and our son who’ll be 3 this year.
If I’m not working, I love working out, going to one of our local gyms. We do CrossFit, and that’s like my hobby. It is like my home away from home. Working out, doing those things and spending time with my family and spending time with my friends. I have a really close group of girlfriends, and we tend to do a lot of our little girl’s nights.
I think I’ve been much more outgoing since I’ve been diagnosed and not holed up in my house; I used to be such an introvert. Like, I just want to stay home. I don’t want to go do anything. But after this I’m like, no, I want to go do all the things.
Initial symptoms
My colorectal cancer story starts when I was about 7 months pregnant with my son in June 2021. That’s when I started noticing blood in my stool.
The doctors shrugged it off. Because of my pregnancy, they said it was normal. You can have hemorrhoids, they said. So I didn’t think anything of it.
But it just kept getting worse. I started to have a lot of lower back pain, as well as this feeling of back pressure. I always felt like I needed to go to the bathroom.
Even then, I was told that it was because my baby was sitting really low. He’s sitting posterior, they shrugged. Just pregnancy stuff.

I gave birth to my son on August 9. While I was in labor, I was having an incredible amount of rectal pain. I remember telling my husband, gosh, this hurts so bad—there’s no way this is just a hemorrhoid. I was having contractions back to back, but they paled in comparison to the pain.
Give me the epidural to take the pain away, I said to my husband. Again I was told that it was because the baby’s just sitting very low. But I had had a daughter before, and I knew that this was completely different.
Come October and November, I started to have even worse symptoms. Each and every bowel movement was bloody—worse, sometimes all I would be excreting would be blood. I was having 15, 20 bowel movements a day that were just blood.
I asked my OB to refer me to a GI doctor in Spokane. While they did get me in relatively quickly, in November, once again, my symptoms were only chalked up to pregnancy.
I was told: you’re way too young. You just had a baby. You have a bunch of hormones going through you. You’ve had hemorrhoids. Basically just dismissing my concerns. But at least I did get them to commit to a colonoscopy at the end of December or the start of January.
But something happened in December that sped things up. I was at my cousin’s basketball game, and I had a sudden really severe stomach cramp. And I went to the bathroom and it was all blood clots, the worst one I’ve had. It was just bright red blood with dark red clots.
My husband contacted one of the GI docs that he works with and was like, listen, no one’s taking my wife seriously. Can we please get her in? And the GI doctor went, bring her in next week. I’ll scope her right away.
And December 20th is when I got my colonoscopy and colorectal cancer diagnosis.
Diagnosis and Reaction

I was 32 years old when I was diagnosed with stage 3 colorectal cancer.
Going into the colonoscopy, I knew it would be cancer deep down. But my husband was so reassuring and supportive; he told me I shouldn’t think like that. So when I went in for the colonoscopy, I actually wasn’t terrified or even anxious.
But when I woke up from the anesthesia, the doctor came over to me. He said: there’s a really big mass there. I’m so sorry.
And I think in that moment, I was like: there’s no way this is my real life. You think it will never happen to you, but it does. The thought in my head was: is it everywhere?
My son was 4 months old at that point in time. My daughter was about to be 3 or 4 years old. I was like, am I even going to see my son turn 1? I was in the middle of nurse practitioner school. Why even finish school? Shouldn’t I just spend as much time as I can with my kids?
I remember the first thing we did was call my mom, who was watching my kids, and I couldn’t even tell her. My husband had to tell her. I got on the phone to my best friend, and I told her. And then I had to FaceTime four of my best friends who knew that I was going in for the colonoscopy.
I could die next month, I remember thinking. It is the most terrifying, sickening feeling. The diagnosis really put things in perspective.
I’m thankful that when my diagnosis came out, my doctor really took charge. The doctor came over and said, we’re getting this looked at today. I’ve already scheduled you for an MRI. I’m getting you a CT scan today. I’ve already talked to an oncologist, a surgeon, a radiation oncologist. I’m not letting you leave until we have a plan for you today.
It was a really long day that day because my colonoscopy was in the morning, and then I had to go through the CT, go through the MRI. Luckily, the doctor fixed it up so that the radiologist would read those scans when I was there.
So I was able to find out quickly via my CT scan that there were no other masses anywhere at that point. The MRI did show the tumor and some lymph nodes, but it didn’t show any masses anywhere else. So I felt some relief that, okay, so far it hasn’t spread.
I went home and all I wanted to do was be around my kids, but at the same time, I didn’t want them to see how upset I was. My mom was trying to hold it together and she was having a hard time.
I tried to be normal, but I hadn’t eaten or drank in that day, so I ended up getting so sick that I ended up having to go to the ER for fluids because I couldn’t keep anything down and kept vomiting profusely. I also think I cried every ounce of water that I had in my body out.
So I ended up calling one of the girls I worked with, and she actually snuck me into the E.R. One of the doctors who is a good friend also knew, as well as the provider who took care of me. That level of support was really nice.
Treatment
Chemotherapy and radiation
My colorectal cancer treatment was a whirlwind of “let’s get your appointments going”.
So I actually got called by the radiation oncologist the very next day and they were like, we want to get you in today. We’re going to map everything out for your radiation.
And then I got called from the oncology office and they said, we want to see you today to go over what your plan is going to look like. And so I ended up going to the oncologist that next day, and, he mapped everything out for me.
He said, we’re going to start with radiation, where you’re going to go under 28 treatments of radiation. And while you’re going radiation, you’re going to have a chemo pump. So you’re going to have continuous chemotherapy infusing. And then once you complete those treatments, then you take a week break from the chemo.

Then you do eight intensive treatments of chemotherapy where you come in and get the four hour infusions. After that, you have surgery.
And after your chemo, we rescan you, we remap and see what your tumor is doing. There is a possibility that if your tumor is gone, you don’t have to have surgery.
But I was like, absolutely not. You’re taking that thing out. We’re not watching and waiting for anything. I had already made my mind up that I was going to have surgery.
So I went to the radiation oncologist later that day and got mapped. So he tattooed my back, my abdomen, mapped where they were going to do the radiation treatments. And then I think the day or two after Christmas, I went and got a port placed for all of my treatment.
And I started treatment January 3rd. So really very quickly, I started my first radiation treatment, and then they hooked me up to the pump that I had to wear 24 -7.
Initially the GI doc said, surgery first. But then when I talked to the oncologist he said, typically if it’s stage one, if it’s just this isolated tumor that hasn’t gone into the lymph nodes, we would do surgery where we cut the tumor out and then we do like a clean up chemo. But mine was very eroded. If I would have waited a couple more months, I probably would have had a perforated colon, that’s how bad it was.
And because I had lymph node involvement, we needed to get the chemo in there and kill what we can. The radiation was to kill the tumor, and the chemo was to stop the tumor cells that were floating around from duplicating and so on. That’s why I had to do the chemo and radiation before the surgery.
Surgery

I underwent a pretty major surgical procedure. They basically went in and dissected the entire tumor, plus did a few things on one side of the tumor and then the other side to make sure that it gets all taken out.
Then they did a temporary ileostomy, where they basically take my colon and bring it out through my stomach to let my surgery site heal. I had to have that for 8 to 10 weeks.
I had to be in the hospital for a couple days, just to make sure that everything was working, and that was the first surgery. And then I had that ileostomy for about 8 to 10 weeks, and then I had to go in and have it reversed.
So they go in and they just basically put my colon back together without that tumor in it. And that surgery was actually a little bit more intense. It was much more painful, even though it was a shorter surgery, and I was in the hospital for about two nights with that one too.
When I got told about the ileostomy, you know, my initial thoughts were like, I don’t care. Do it. I just was in that mindset. Do what you need to do to get me better, I don’t care.
But when I actually came home with the ileostomy, it was a very big mental block for me. I felt like I didn’t want to go out in public since I found it disgusting. I never minded taking care of them on other people, but I never thought that I would have to have one.
And I remember the first day that the home health nurse came over to help me figure out how to change the bag and stuff. I couldn’t do it. My husband had to do it because I was so emotionally distraught from it. And my husband actually just said, you don’t ever have to look at this. I will take care of it for as long as you have it. It took me a couple of weeks to finally get used to it.
And actually one of my preceptors for school has an ileostomy and he and I actually became really good friends. And I remember when I found out I was going to have one, he was like, hey, I got your back. I’m going to walk you through this whole thing. I’ve had mine for years. And he was such a big supporter.
He would talk me through it. He’s like, this is just part of our lives now. He was a big reason why I think I did so well with it, because I had him just there, supporting me through it.
And he knew what it was like to have one knowing that it wasn’t permanent. There is an end in sight.
And when I got it reversed, I just remember the doctor being like, okay, it’s getting reversed, but I’m just telling you right now, it’s not going to be a walk in the park. We have removed a lot of your nerve endings, your colon has basically been asleep for weeks. Basically, you might have to potty train yourself again. And I was like, maybe I don’t want it reversed, maybe I just want to keep it.
And so when I had the second surgery, I remember I was in so much pain, I can’t even remember being like, oh, it’s gone. I just was like, get this pain taken care of. Definitely having it reversed was worse than having it placed. And that took a mental toll on me for sure.
Side effects
So the side effects of the radiation, I didn’t have too many. The most significant was fatigue from the radiation, which was insane. More fatigue than I had when I was pregnant with my son, when I was 12 weeks pregnant and I got Covid. The fatigue from the radiation felt maybe 20 times more than that.
I also had a lot of back pain, aches in my pelvis.
They also had said that we’re radiating your uterus, your ovaries, you’re not going to be able to have any more children. They did give me a chance: we can do what’s called an ovarian transposition, where they pull the ovaries out of the radiation field to try and salvage if you want to have kids. And I was like, listen, I have two healthy babies. I need to be there for them. I can’t delay this any longer.
As for side effects from the initial chemo pump, I didn’t have any other than my fingertips turned different colors, like I dipped my fingertips in self-tanner. And everyone would be like, whoa, your fingertips are brown. My oncologist said that the chemo regimen I had to do was called 5-FU, and he was like, oh, it’s the 5-FU fingers. It’s totally normal to have that.

But later on, the side effects from the chemotherapy got way more intense. I went into the first treatment and after the treatment, I felt fine, just a little tired. I was told, though, that the side effects would really hit me—and they did.
Tuesday night after my very first infusion, I ended up so violently ill that I passed out. I got rushed to the emergency room at one in the morning because I was so sick.
When I got to the E.R., my blood pressure was in the 70s. My heart rate was super high. They were like, she is so severely dehydrated, we might need to admit her to the hospital. I can’t even tell you how many liters of fluids they gave me. Every antiemetic possible. I was still so sick.
They called my oncologist. They were like, what do we need to give her? And he was like, you need to give her this specific type of antiemetic. That’s for chemo. That’s really expensive. And hospitals don’t usually carry it. But he’s like, that’s what’s going to keep her out of the hospital.
So after that I went to my follow up appointment. He’s like, we need to do pre-meds on you because that obviously can’t happen again.
And I remember after when I was laying in the hospital after my first treatment, I said, I will not do this anymore. I’m done. I’m done with chemo. I can’t do this for seven more times.
And my mom’s like, you don’t have a choice. You have two children at home. You’re doing this. So we need to figure out what we need to do to make it so you can do this.
So I would pre-medicate, I would get this infusion of this antiemetic that was supposedly only for like chemo patients, before I got my chemo. And then on Wednesday when I got my pump disconnected, I would get fluids and that I did pretty well with that. I really didn’t have any other side effects from the chemo from that point on other than fatigue.
Aside from that, I would usually have to take a nap. I got a little bit of neuropathy towards the end where my feet were really numb and it felt like my feet were asleep, just chronically asleep. Which was pretty common for this type of chemo.
I didn’t lose my hair.
I had so much support and I will always be grateful for it.
Support
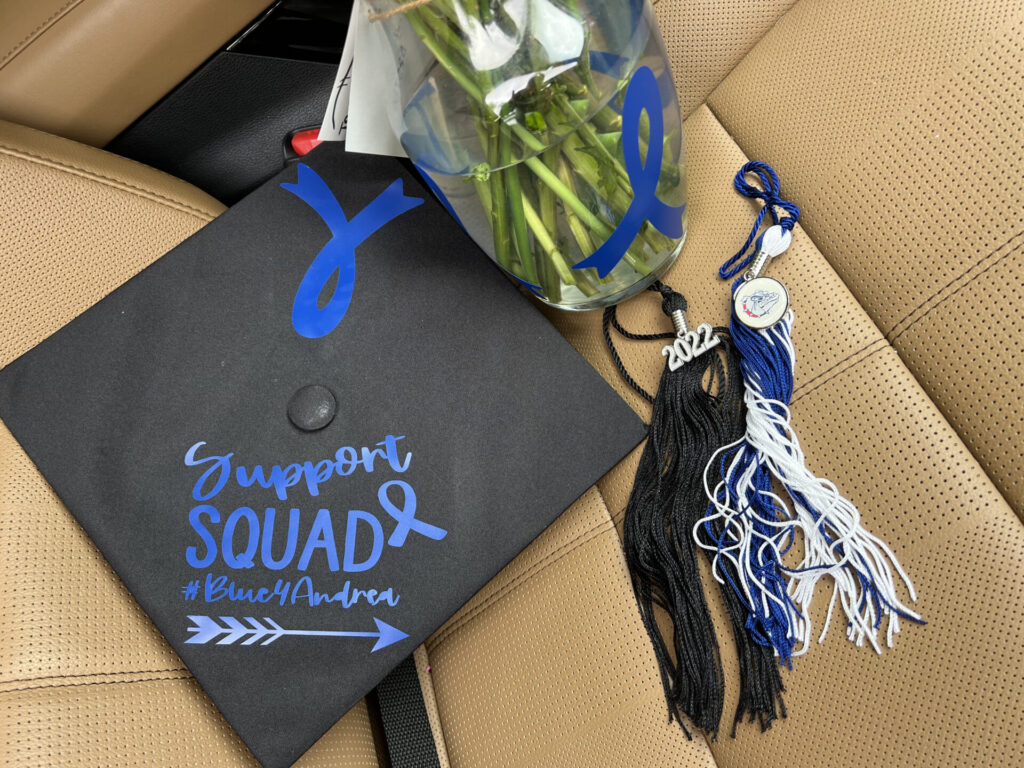
I had so much support and I will always be grateful for it.
I’m originally from Portland, Oregon. I have a really close friend group in Portland. I have a really good friend who contacted all my friends in Portland when she heard about my colorectal cancer.
She contacted all my family, all my friends in Spokane, like friends that I have in Arizona. She just went above and beyond, and she basically had them send her a letter of everything they love about me and basically wishes for me and then send pictures. And she put together this book. And so each page was like a friend who wrote a letter to me. I took that with me to my treatments because it was just like seeing how much love and support I had.
My best friend put together a bunch of stickers that said Support Squad Blue for Andrea, and people throughout the hospital were putting them on their water bottles, people I didn’t even know, but worked with her on in her unit and knew how much I meant to her were like wearing, buying these stickers to support me. And so just seeing that was like, so helpful.
I think when you’re literally fighting for your life, I didn’t hold grudges; didn’t get upset or anxious over really little things. I actually had a way better outlook on life when I was going through that because I was like, hey, I don’t know what next week looks like. I’m just going to enjoy everything I can right now, like my children and school.
Keeping Busy
My oncologist was like, you can’t work. You need to just rest. And I’m like, I’m not just going to sit at home and sulk.
So I actually completed my last semester of nurse practitioner school while I was in chemo. And I used my colorectal cancer treatments as my study time away from my kids. So, keeping myself busy and just continuing to push through, really helped me.
But I had days like there there were absolutely times where it would hit me like, I cannot believe that I have colorectal cancer and that this is what I’m going through.

And I would have to go upstairs. I’d lock myself in my room so my kids didn’t see me, and I would completely break down and just have a moment of hysterically crying, like ugly crying. Why? Why is this happening to me? Like, what did I do? And then I’d pop right out of it.
One of my good friends, she’s always like, okay, have your moment in Pity City and then get yourself out of it and let’s go. So I’d always just tell myself that, get out of Pity City. We had our moment, time to get back.
Stage 4 Scare

I had a bit of a scare during which I thought my colorectal cancer might be stage 4, but it hadn’t after all.
I was just starting my job as a nurse practitioner. Right after I completed treatment. Right before I had my first surgery. They wanted to rescan me and see just how much the tumor had shrunk. So I ended up having another CT and an MRI, and I remember being at my very first day of work at my new job, I was training, and I got the MyChart result.
So I opened it up and the first thing I saw was a new lesion on the liver, and my heart dropped. I remember I got through another hour of work, and then I finally just told my preceptor, I need to go. I’ll be back tomorrow.
And I called my husband, and I’m like, I’m stage four. He’s like, what are you talking about? And I’m like, there’s a lesion on my liver.
That day was the worst. Way worse than the day I got diagnosed. One of the most defeating days ever.
I came home and said, we need to plan my funeral, we need to get our things in order. And my husband, at that point, he’s always tried to be so positive. And at that point he literally goes, I don’t really know what else to say other than, we need to get things in order for you. Because he knew, this isn’t good. That day gives me more anxiety and just makes me cringe more than the day I got diagnosed. Because it felt like I had gone through so much for it just to not work.
The next day I remember messaging my oncology team and I was like, can I please can I have a phone call with my oncologist so we can talk about my CT scan? And she goes, yeah, he’ll like, do a telephone call with you or tell a zoom video. I was like, okay. So I went out to my car. I was again at work.
I went out to my car and got on the call, and he had my CT scan pulled up and he was there. And so I was sitting there and I was just waiting for him to tell me. And he goes, you know, the spot on your liver. He’s like, I am 99% sure it’s not cancer. I actually have a call out to the liver specialist to just look at it.
He said, you know, the chemo you have can really damage your liver. And I had actually had on my last chemo, I had labs done in my liver. Enzymes were elevated. And he said, I think this is a piece of your liver that just died from the chemo and is just trying to regenerate. Doc’s calling me right now. She’s reviewing all your images.
So he talked to her and then he got back on. He’s like, yeah, she is pretty confident.
This is nothing to be worried about. So at that moment I was like, oh my gosh. He said, you know, your tumor is actually shrunk significantly. It’s still there. We still need to do the surgery. But yeah, this spot on your liver, I’m just really not concerned about.
Remission
So technically, my colorectal cancer was in remission on the day of my surgery when they pulled the whole tumor out. June of 2022. And I guess at that point, I didn’t necessarily think I was in remission because I was like, well, they still need to scan to make sure they got everything.
They took the tumor out and they take the test, the margins to make sure there was no tumor cells. And I had negative margins, which they said is really good.
But unfortunately I had like eight lymph nodes that had live cells in it. And that puts you at such a high risk for recurrence.
I remember my oncologist being like, you have a 40% chance of going to stage four even with all of this out. And still it’s like a 60% chance of it not happening. Yeah, but 40% is pretty high. Because of that, they were like, we’re going to have you on a really close scan bloodwork every three months for five years.

So it wasn’t until probably my three month scan after that where they didn’t see anything that I was like, okay, I’m officially in remission. I don’t have the colorectal cancer in me anymore.
To this day, I still don’t think I’ve ever gotten to the point where I don’t feel that I have colorectal cancer. It’s just, I think a part of me feels that someday it probably will come back. And I don’t know how to get out of the mindset that it won’t.
Like, even though, my blood work, I get a CT scan, an MRI every three months, and then I get a tumor DNA test where they actually extract DNA from my tumor, and then they draw my blood every three months, and they compare those so they can actually pick up if there’s like, tumor cells floating. Every single one’s been negative since June of 2022.
But I can’t get in the mindset that it’s gone. I just I think that’s just part of it. I just can’t no matter what, I’m like, okay, well, another month where it hasn’t popped up again, but we’ll just wait till the next month like so.
And I think that’s just part of the process of this. Like you just once have once you have colorectal cancer, you’re never going to feel like you’re fully out of it.
Going during the treatment and everything, I felt less anxiety because I think when you’re going through treatment, you feel like you’re actively doing something to get rid of the cancer. When you’re in remission, you feel like a sitting duck, like you’re not doing anything to actively get rid of it, even though it’s technically gone.
So that has been really hard because when I was in treatment, I’m like, oh, every day I’m going in that’s killing more of those cells, and it’s getting rid of it, and you feel like you’re actively taking care of it. And then sitting in remission for the past two years, I think, okay, is this next scan, the one that’s going to pick something up, is this next bloodwork, the one that’s going to pick something up.
You just kind of feel it’s just like a waiting game. I think it’s because, you know, they say you can’t say you’re cancer-free until five years out.
So statistics show that I was 71% at stage three B, which I was I have a 71% five year survival rate. In hindsight 71% is great, but there’s also that 29% rate, that’s not. And so, I also get to the point where like, okay, yeah, I’m two years out from this. Does that mean I only get three years left? So I just get into a negative headspace and you just have to take a lot to get yourself out of it.
There are going to be dark days. There are going to be days where you feel like you cannot go on any longer. I had plenty of those days where I felt like, I cannot, I don’t want to wake up tomorrow. I cannot move on from this.
Just know that we can. There is a light at the end of the tunnel.
There is a bright side, even though you don’t feel like there is.
Lessons and Learnings

I am a huge advocate now for self-advocating.
I’ve had people reach out to me, on Facebook, on Instagram who’ve seen my story and they’re like, hey, I started to have these symptoms. I went to my doctor and my doctor was like, oh, you know, we’ll just follow up in a couple of months.
Absolutely not. You find yourself a new doctor, you go to an urgent care, you go to an ER and you say, this is what I need, this is what I want. You have to push for it. And, you know, I have told people: exaggerate your symptoms a little bit, like if you had one bloody bowel movement, go and you say I’m having multiple bloody bowel movements.
You get the colonoscopy because right now the colonoscopy age is 45, which is so crazy to me. With the rates of colon cancer showing up in people 18 to 35. I read an article that showed rectal cancer is supposed to increase by 112% in patients 18 to 35 by like 20, 35 or something crazy like that. And then colon cancer is supposed to increase by like 114%, just some outrageous number. Then it’s supposed to be the leading cause of cancer death in people 18 to 35.
And yet the colonoscopy age in the United States is 45. I’ve been in ER medicine for ten years now, but I’m a new provider and I’ve actually had a couple young patients come in who have had similar symptoms and they’re like, yeah, my primary doesn’t take me seriously.
And I’m like, we’re gonna call GI here in the ER today. We are going to try and get this figured out. We need to lower the age. But I also understand that with the increased amount of cancer cases and people needing scopes, they’re overwhelmed too. There isn’t enough providers.
I just think that we need to stop making it an age thing like it is. Colorectal cancer is not a 50 year old man’s disease. Someone who is 19 can get it, someone who is 20. And you can do all the right things and still get it.
I have never smoked a cigarette a day in my life; I do not do drugs; I hardly drink alcohol. I work out and I eat relatively healthy. And I still ended up here. And I had genetic testing. I have no genetic risk factors. I have no family history. So it can happen to anyone, it can literally happen to anybody.
Advice that I’d have for anyone in this situation is that there is a reason for everything. There is a reason that we were chosen to go through this fight.
I look at it as like I was chosen to go through this fight so I could help bring awareness to other people. We were chosen for a reason, and we need to be strong through this fight. We need to be there for our friends.
There are going to be dark days. There are going to be days where you feel like you cannot go on any longer. I had plenty of those days where I felt like, I cannot, I don’t want to wake up tomorrow. I cannot move on from this.
Just know that we can. There is a light at the end of the tunnel. There is a bright side, even though you don’t feel like there is. And know that your feelings are validated.
I had people be like, look at you, you’re still here. It’s like, no, you don’t know. You have no idea how this is feeling. And we are the only ones that will know truly how this feels. Know your feelings are validated, but know that you can get through this. I’m always here to talk to anybody who’s going through that.
My other thing is, stay off of the internet. I was in that support group for a little bit, but then it got to the point where I was seeing so many just negative things, stuff that started to bring me down, and I’m like, I had to remove myself from it. Stay off the internet, stay off of social media, stay off of any of that. That is the best advice I can give, because you will go down a rabbit hole of so many things, and that’s not what your body needs.
And your fight is your own fight, like my colorectal cancer fight isn’t somebody else’s. Like we’re all going to be different. Try not to compare it to other cases. Just know that, like your fight’s your own and you’re going to be different.

Inspired by Andrea's story?
Share your story, too!
Related Cancer Stories
More Colorectal Cancer Stories
Allison R., Colorectal Cancer, Stage 2C
Age at Diagnosis: 32
1st Symptoms: Extreme fatigue, unexplained weight loss, blood in stool, "blockage" feeling after eating
Treatment: Concurrent adjuvant (oral) chemotherapy + radiation, colectomy, oral chemotherapy
Michelle C.
Symptoms: Felt like either a UTI or yeast infection
Treatment: Chemotherapy (carboplatin and paclitaxel), surgery (hysterectomy), and radiation
Jason R., Colorectal Cancer, Stage 4
Symptoms: Blood in stool, diarrhea, tenesmus, feeling run down
Treatment: Chemotherapy, radiation, HAI pump
Raquel A., Colorectal Cancer, Stage 4
Symptoms: Frequent bowel movements, pin-thin stools, mild red blood in stool
Treatment: Chemotherapy (oxaliplatin, 5-fluorouracil, and irinotecan)