Finding Cancer by Chance: Cyndi’s Papillary Thyroid Cancer Story
Cyndi’s papillary thyroid cancer experience began with no warning signs. Her life revolved around motherhood, theater, and artistic expression. During a routine endocrine visit for unrelated thyroid level checks, her doctor noticed a nodule. Cyndi had always attributed the fullness in her neck to her natural features, never suspecting it could be cancer. A chief radiologist saw reason for concern, and a thorough surgeon conducted further scans and a biopsy.
Interviewed by: Carly Knowlton
Edited by: Chris Sanchez
The diagnosis of papillary thyroid carcinoma came as a shock. Genetics revealed a RAS mutation, and Cyndi also found out that her left thyroid lobe housed both cancerous and pre-cancerous nodules. Surgery, including a central neck dissection, set off a storm of emotions. She faced a difficult initial recovery, the unexpected loss of her voice, and adjusting to a new appearance.

The months after surgery challenged Cyndi’s sense of independence, body image, and leadership. She found transitioning to being a patient the hardest part. Professional support, tailored endocrinology care, and connecting with another patient who also had surgery the same day became anchors.
Today, Cyndi’s papillary thyroid cancer experience has redefined her life rhythms. She takes thyroid medication, celebrates improved energy, and has reprioritized presence for her son and students. She wants the world to know that thyroid cancer is not truly ‘the good cancer,’ as it is often known; it leaves scars both visible and invisible. She reflects, “Thyroid cancer is often seen as the ‘good cancer,’ but the experience isn’t easy.”
Watch Cyndi’s video and read the edited transcript of her interview below. You’ll delve into how:
- Advocacy and seeking a second opinion on scans can be life-saving
- There are no “easy” cancers. Thyroid cancer patients deserve validation and targeted support
- Transitions in identity, from being in control to being a patient, from health to surviving, can be the hardest challenge of all
- Support from others with similar diagnoses, rather than generic cancer groups, can be transformative
- Cyndi’s transformation from creative professional to empowered patient redefines presence and patience
- Name: Cyndi F.
- Diagnosis:
- Thyroid Cancer (Papillary Thyroid Carcinoma)
- Age at Diagnosis:
- 35
- Staging:
- Stage 1
- Mutation:
- RAS
- Symptom:
- None per se, nodules discovered during thyroid examination
- Treatments:
- Surgeries (hemithyroidectomy, isthmusectomy, mid-neck dissection, parathyroid transplant)
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Cyndi
- No red flags: my cancer was discovered incidentally
- My biopsy
- I had clear margins
- My surgery in detail
- Early days at home: my emotional adjustment
- Accepting change, my recovery timeline, and lasting effects
- The importance of support and finding the right community
- Adjusting to medication
- Thyroid cancer’s impact on me
- What I want others to know
My name is Cyndi
I was diagnosed with stage one papillary thyroid carcinoma in May 2025.
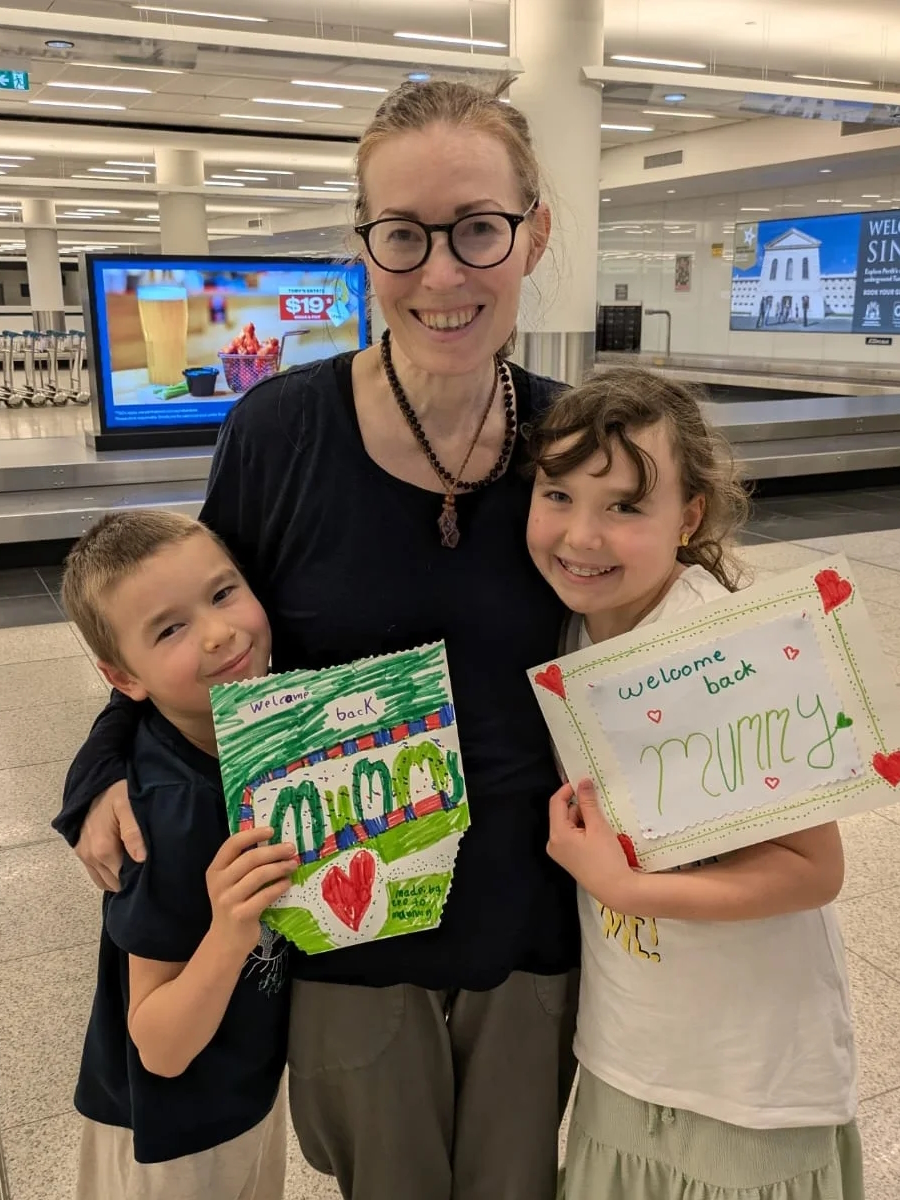
I am most passionate about my son, but I am also passionate about my work. I’m a theater director and playwright. That is what I do outside of being a mom.
For fun, I like attending theater and making theater fun.
If my friends were to describe me, they would say I’m definitely creative, original, unique, and optimistic.
No red flags: my cancer was discovered incidentally
Honestly, there were no red flags. It was totally caught incidentally.
I had gone to an endocrinologist for something I thought was unrelated. I just needed my thyroid levels checked. She checked them, but then said, “No, you have a pretty big nodule right there.” I thought that was just my face or my neck because I’d had it for such a long time. I had no idea there was anything abnormal. Looking back at photos, I realized there was a pretty big nodule there.
She had me go for an ultrasound, and the scan actually came back benign because it was read by AI. The report even said “generated by AI.” My husband works in healthcare, saw that, and suggested getting a second opinion. He showed it to his friend, the chief of radiology at a major hospital. That person said, “No, she should definitely get a second opinion and see a surgeon.” So, I saw the surgeon, and within a few minutes, he said, “Nope, you definitely need a biopsy,” and threw out the first ultrasound report. He did an ultrasound and a biopsy right in that exam room. Two weeks later, I received the pathology, which felt like a million years waiting.
My biopsy
Two weeks later, the results came back with a RAS mutation, which is usually only found in anything follicular in nature. It also came back as having nuclear changes and positive gene expression, meaning it was acting like cancer, but it was confusing. It wasn’t acting exactly like follicular, so I thought it was a follicular variant papillary. I was wrong.
My left lobe was so big it had two nodules. One was cancerous, the other was pre-cancer. Because it was so big, it was crushing my parathyroid and pressing against several lymph nodes, so they took out all the surrounding lymph nodes. I ended up with a central neck dissection and a parathyroid transplant.
I had clear margins
I waited another two weeks for the pathology to confirm that it was papillary. When I woke up, I learned there were two nodules. I actually saw it on my patient portal before I was told. I found out at 5 a.m. because I was checking the portal hourly, trying to figure out what was going on. I tapped my husband and said, “By the way, it’s papillary.” He asked what I meant, and I said, “It’s right here. I had cancer and now it’s gone.”
All the notes said my margins were clear, so I was focused on the fact that I wouldn’t need the other side taken out. I was nervous about the possibility of needing a second surgery, but my margins were clear.
My doctor called that same day. I said, “Yeah, I already know.” He said, “I have somewhat good news.” I said, “Is it that I had cancer and now I don’t?” He asked how I knew, and I said I saw it on my portal. That’s the danger of patients having instant access to their records.
My surgery in detail
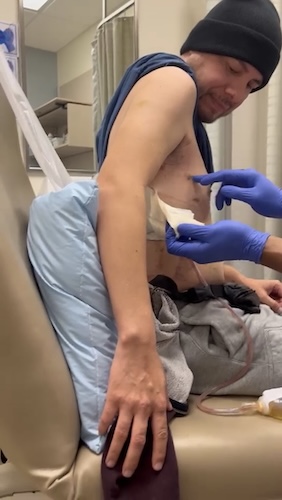
This is how my surgery went.
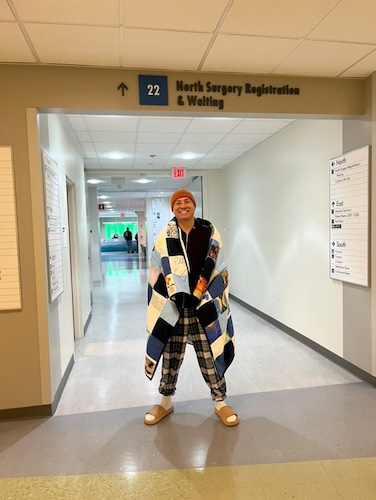
Preparing was standard, like preparing for any surgery, with all the checkups and medical tests. The surgery experience itself was not bad or traumatizing. I arrived at the hospital around 10 a.m. for a noon surgery. The staff was pleasant, and nothing about the process was negative. I walked into the operating room, greeted everyone, and joked, “Just make this part go away.” The next thing I remember, I was waking up.
When I woke up after surgery in the hospital, I wasn’t able to move. I legitimately thought I was paralyzed, but it turns out I was not. They reassured me that my head was just immobilized the way they wrapped me. I have not seen any other pictures of people being wrapped that way after surgery. I wasn’t expecting that. It felt very hard to breathe and very hard to move. My heart rate was really high when I woke up. I was very tachycardic, and I think I was more distracted by that because they kept saying, “Oh, your heart rate is high, your heart rate is high, it’s not coming down.” I was just very distracted by that as well.
When I woke up, I again thought I was paralyzed and unable to breathe, but that was not true. My doctor was calm and patient; I really lucked out with finding him. Due to my tachycardia, I wasn’t allowed out of bed, so going to the bathroom was an ordeal. Eventually, I learned to unhook myself, but I was scolded by the nurse: “You will not unhook yourself!” After that, I called for help each time I had to go. I stayed in the hospital one night, and though they offered more time, I was eager to go home.
Early days at home: my emotional adjustment
I made friends with the woman in the next bed and had a good conversation, even though my voice sounded like Minnie Mouse for a while, since my vocal cords had been moved during surgery.
They wrapped me again before I left, looking much like a mummy; something I haven’t seen in other surgery pictures. Seeing my scar for the first time at home was emotionally difficult; it was a hard day where everything hit me all at once. My heart rate was still high, and I was troubled by the loss of my voice.
Compelling Quote: “Seeing my scar for the first time at home was emotionally difficult; it was a hard day where everything hit me all at once.”
Accepting change, my recovery timeline, and lasting effects
I had to accept how I look now, and given my performance background, growing up where appearance matters, this was hard.
Recovery took about two months before I stopped noticing the scar at all, though if I lie down the wrong way, I still feel it. Swallowing is when I feel scar tissue the most.
The importance of support and finding the right community
My advice for someone going through this surgery is to find someone who really understands.
I connected through a Facebook thyroid support group with someone who had the same surgery date, and we became each other’s support through everything.
Her outcome was different. She needed a second surgery and radioactive iodine. But our connection helped us both.
It’s best to avoid general cancer support groups; thyroid cancer is in its own unique category. It’s not less traumatic just because it’s called the ‘good cancer.’ Many survivors deal with lingering health issues, and I see the world more patiently now as a result.
Adjusting to medication
I was actually thankful to go on medication because I wanted to feel like myself again.
It took several endocrinologist visits to get complete testing. Many doctors only checked my level of thyroid-stimulating hormone or TSH, and not the levels of T3 and T4, which are hormones the thyroid gland produces.
My current endocrinologist tested everything and found my T3 was off. Starting thyroid meds helped, and now I feel like myself again.
If I eat too close to taking my medication, I feel different.
Thyroid cancer’s impact on me
The experience made me more present in everything in my life, especially for my son and my students. I was always overbooked and overstimulated before. My experience forced me to reprioritize and slow down.
The initial discovery of the nodule was the hardest part for me, since it was my first medical issue and required surrendering control. I’m used to being in leadership roles and making decisions. But cancer means letting others take over, which was tough. Adjusting to being a patient was the hardest part, but I’ve now accepted that regular doctor’s visits are my new normal.
Thyroid cancer is often seen as the ‘good cancer,’ but the experience is not easy. There are no walks or marches for thyroid cancer like other cancers, and it’s often seen dismissively by others and even doctors.
Survivor’s guilt is real, and just because papillary is the most common, that doesn’t mean it can’t become serious. I’ve seen cases that spread and required lifelong oxygen or tracheostomies. I was fortunate mine was caught early, but others aren’t as lucky.
I’m now going to be monitored every three months for the first year or two, then every six months, and eventually annually. I’m a little anxious that my surgeon might retire someday since I’ve become so comfortable with him.
What I want others to know
I hope sharing my story brings more awareness and encourages others to think twice about minimizing thyroid cancer as ‘the good cancer.’

Inspired by Cyndi's story?
Share your story, too!
More Thyroid Cancer Stories
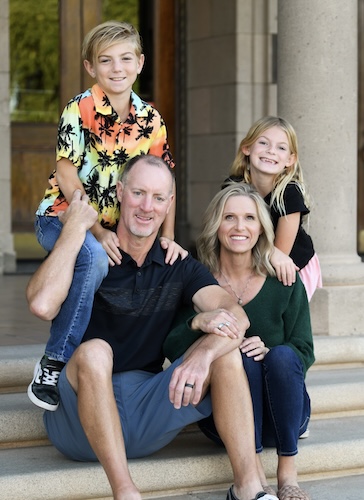
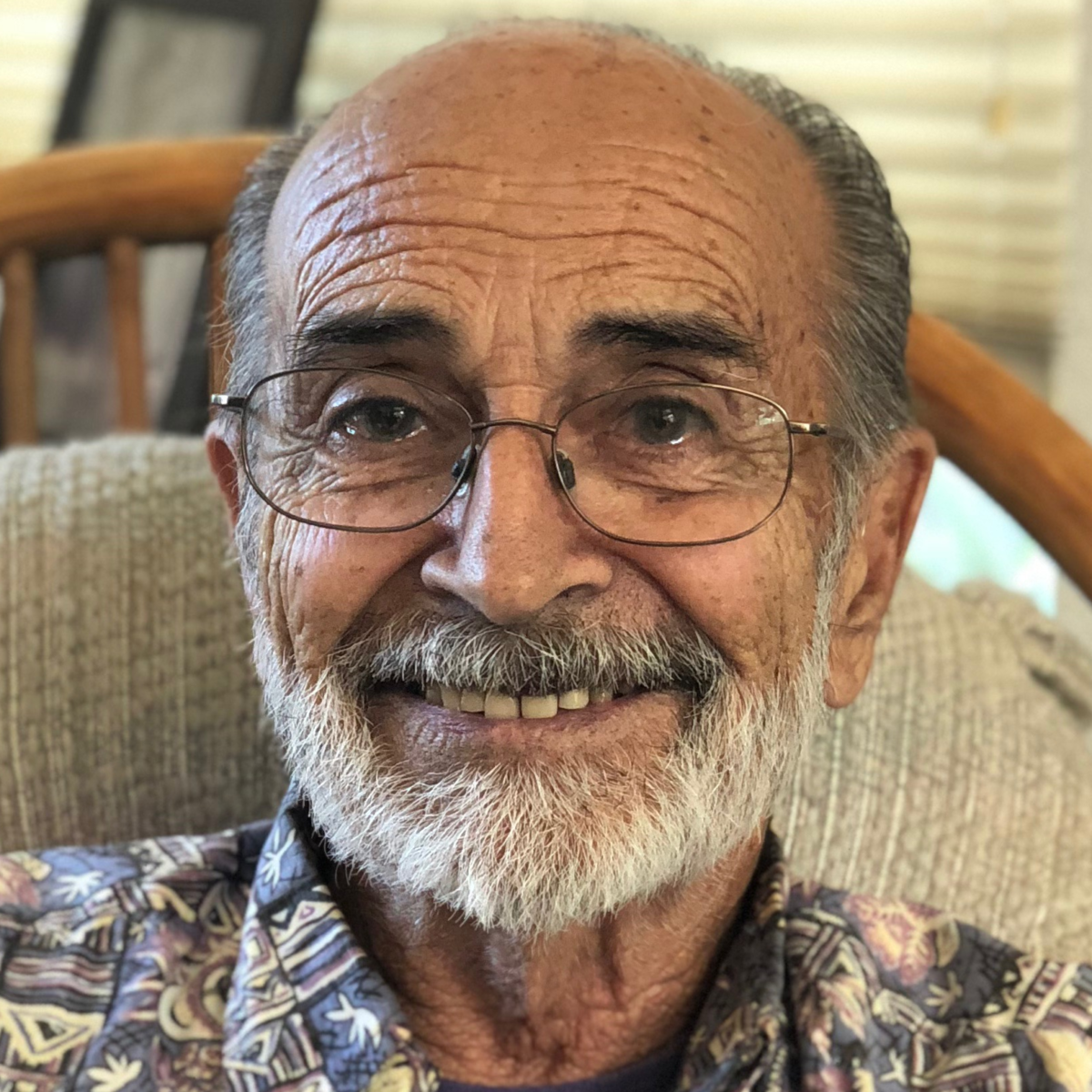
Taylor Scheib, Thyroid Cancer (Oncocytic Thyroid Cancer)
Symptom: Appearance of a visible lump on the neck
Treatments: Surgeries (hemithyroidectomy, completion thyroidectomy), radiation therapy (radioactive iodine)
...
Cyndi F., Thyroid Cancer (Papillary Thyroid Carcinoma), Stage 1
Symptoms: None per se, nodules discovered during thyroid examination
Treatments: Surgeries: hemithyroidectomy, isthmusectomy, mid-neck dissection, parathyroid transplant
...
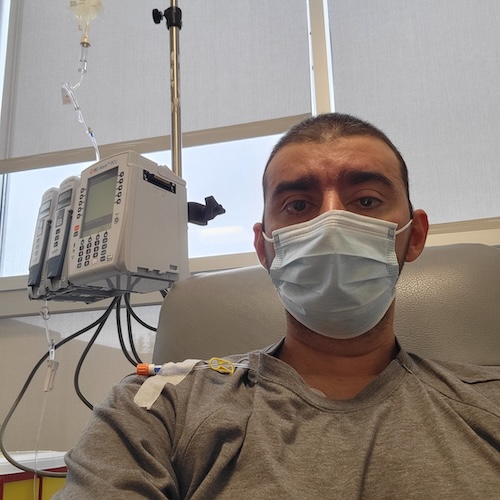
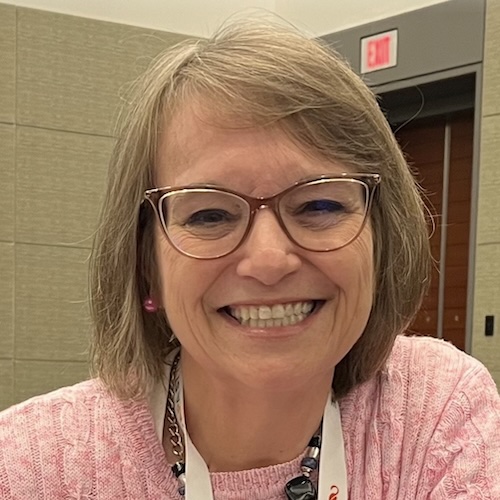
Laura C., Follicular Lymphoma, Stage 4 (Metastatic), Grade 1 to 2; Papillary Thyroid Carcinoma
Symptoms: Incidental finding after hysterectomy (follicular lymphoma), thyroid nodule detected on imaging (papillary thyroid carcinoma)
Treatments: Immunotherapy (rituximab and lenalidomide or R² regimen), surgery (thyroidectomy)
...
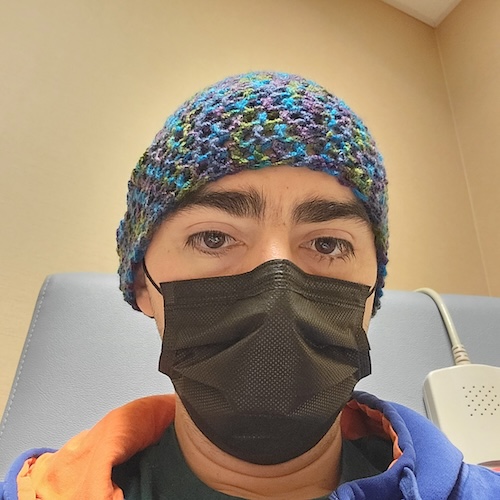
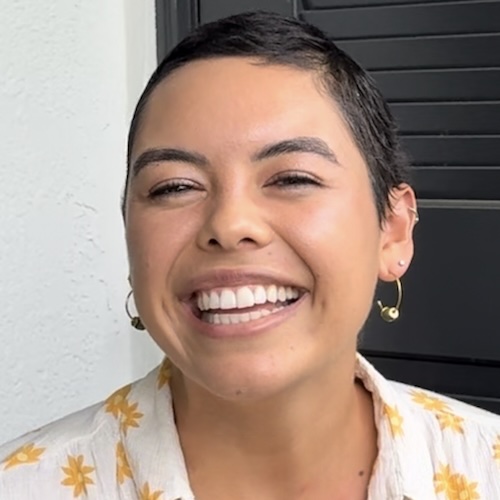
Alyse V., Thyroid Cancer (Papillary Thyroid Carcinoma, Tall Cell Variant, Metastatic)
Symptoms: None per se, lump discovered during thyroid examination
Treatments: Surgeries (neck dissection, lymphadenectomy), integrative therapies
...