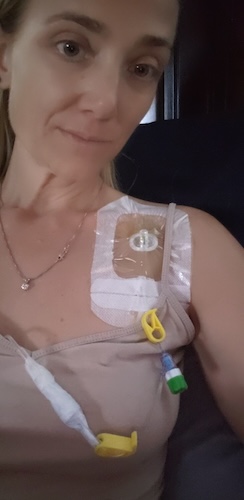
Niccole is Redefining Life After an Stage 4 Stomach Cancer
Niccole is a stage 4 stomach cancer survivor who embraced traveling the world after her diagnosed in 2021. After experiencing stomach pain, acid reflux and vomiting, she went to the doctor for testing that revealed her cancer. Ultimately, Niccole had 80% of her stomach removed, changing the way she lives each day.
Interviewed by: Nikki Murphy
Edited by: Chris Sanchez
Niccole’s tumor was blocking her stomach’s pyloric sphincter, and stomach cancer surgery meant that she might lose her stomach altogether. She initially underwent a chemotherapy regimen that worked by shrinking her tumor before surgery. Through biomarker testing, Niccole also learned that she carries the BRCA1 mutation, inherited from her mother’s side, linking her diagnosis to a known familial risk.

Niccole underwent surgery to remove her gallbladder and 80 percent of her stomach. Life afterward required a complete lifestyle change, requiring her to eat much smaller meals.
Two years later, Niccole’s cancer metastasized in her ovaries, liver, spleen, and peritoneum. She faced another uphill climb through HIPEC treatment and further surgery. Now on ongoing immunotherapy and ctDNA monitoring, she continues to live fully in the present, knowing that time is uncertain. Her story embodies acceptance, grit, and the power of patient advocacy. Through Debbie’s Dream Foundation and Hope for Stomach Cancer, Niccole mentors others navigating the unknown. She proves that life after a life-altering diagnosis can still be full of purpose.
Niccole’s story delves into:
- Small, early symptoms can signal deeper issues. Listening to your body can save your life
- Treatments may eradicate disease, but often transform how patients live afterward
- Advocacy and patient communities provide essential emotional support and empowerment
- True strength is not found in control but in embracing uncertainty with purpose
- Niccole’s transformation unfolded not just through healing, but through redefining what it means to truly live
- Name: Niccole B.
- Age at Diagnosis:
- 37
- Diagnosis:
- Stomach Cancer
- Staging:
- Stage 4
- Mutation:
- BRCA1
- Symptoms:
- Stomach pain after having alcoholic drinks
- Eating less
- Slight weight loss
- Acid reflux
- Vomiting
- Getting full fast
- Treatments:
- Chemotherapy: hyperthermic intraperitoneal chemotherapy (HIPEC), open HIPEC with cytoreductive surgery
- Surgeries: partial gastrectomy, cholecystectomy, splenectomy, partial colectomy, partial hepatectomy
- Radiation therapy: targeted radiation therapy
- Immunotherapy
- Targeted therapy: PARP inhibitor
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Niccole
- I had a quiet travel year after a cancer recurrence and HIPEC treatment
- My early symptoms, and the first signs that something was wrong
- I had worsening symptoms, including acid reflux
- My initial GI visit and missed testing opportunities
- I had an alarming ultrasound and was urged to go to the ER
- Rapid escalation: scope, CT, and oncology referral
- The phone call, my panic attack, and hearing “oncologist”
- Involving my family and getting a second opinion
- Understanding the tumor location and the possible removal of my stomach
- Facing life without a stomach, and my initial treatment plan
- Tumor disappearance, major surgery, and creating a new stomach pouch
- Completing chemo and radiation, and my first declaration of NED
- A suspicious PET scan and surprise hysterectomy findings
- HIPEC and major cytoreductive surgery
- Ongoing immunotherapy and close surveillance
- I’ve adapted to life without a stomach
- I live with the fear of recurrence, but I’ve chosen joy
- Finding strength and support through family, friends, and stomach cancer communities
My name is Niccole
I am a stage 4 stomach cancer survivor. I was diagnosed in August of 2021 at the age of 37, and I live in Arizona.
So, I am huge into travelling. Ever since my diagnosis, we have decided that we are going to travel the world because we do not know who is going to make it to what age. I am a realtor here in the Valley, and I love what I do. I do residential real estate. I work with buyers and sellers out here in the Phoenix metro area. I have two dogs. They are my pride and joy. I love them. No kids, so they are my fur babies.
Originally, the first trip that we ended up doing was on my bucket list. After I finished my chemo in 2022, we booked a cruise. We did a seven-day cruise to Alaska in May of 2022, and it was amazing. It was beautiful. We want to go back, and we want to do a land and sea cruise.
More recently, last year, we did a Mediterranean cruise. We started in Barcelona. We spent three days in Barcelona and then travelled the whole little coastal area. We went to Pisa and Florence, which were amazing. We ended in Rome, and we spent an additional three days in Rome. I think we were out there for about sixteen days. We have been to Ireland. We went to Lisbon, Portugal. We have been to the Canary Islands, so we have been all over the place. We still have a bunch of stuff to do on our bucket list, but those are some of the most recent trips.
Just getting to learn about the culture is why travel means so much to me. I really think it is important that we get outside of the United States because I really think it opens up our eyes. We really like seeing the churches and the history and just getting to understand where we came from, honestly. It is a lot of fun to see the different sights. There are so many cool things out there that are old.
Ireland was pretty cool. It was very, very wet. It rained a lot. We went in October of 2023, I think. We did a cruise. We are big into cruising, so we have done a lot of different cruises. It allows you to see multiple areas versus going to one location and then trying to figure out your travel and your stay and all that kind of stuff. The cruise line is pretty much your food and driver, and the place you lay your head.
I had a quiet travel year after a cancer recurrence and HIPEC treatment
This year has been quiet because I got busy with work, and then with the recurrence, I had surgery. We are coming up on a year in November. I had surgery in November because I did HIPEC with CRS, and that recovery was really, really rough. It was not until probably March that I was really back into—I do not even want to say normalcy, because I am still somewhat a little different—but I got more consistent with being able to do things and getting my energy back and all those types of things. So this year has been a little bit quieter on the travel front for us.
We have done a couple of things. We just got back from Holden Beach, North Carolina. But otherwise, it has been a soft travel year for us.
My early symptoms, and the first signs that something was wrong
At the beginning of 2021, none of the things that I had were really extremely “boom, in your face.” I was 37. I chalked up a lot of the things that I had going on to maybe stress with work, and just that, as we age, things happen.
We used to go and enjoy margaritas with the girlfriends. We would go out, and I would have a drink, and I would be in agonizing pain. I remember a couple of times we went out with some couples to have drinks. They were going to go out afterwards, after we did dinner and everything. They were going to go to another place, and I had to go home, because I was literally curled up in the fetal position because my gut felt so bad. So that was kind of the start of it.
I had lost a little bit of weight, but it was not significant. It was not a super extreme weight loss. I was struggling a little bit with getting full faster, and then it kind of progressed. That was probably all at the beginning of 2021, January, February time frame.
I had worsening symptoms, including acid reflux
Then things started progressing. Probably about the March-April time frame, I started to get a lot of acid reflux, and I had never experienced acid reflux before. It got to the point where I could not even lie down in my bed anymore. I would have to go sleep in our living room on the sofa, because the sofa was able to prop me up, so I was not lying down. If I lay down, I would wake up vomiting in my mouth.
I had started to take some over-the-counter medications. My family is all kind of in the medical field in one aspect or another. I had reached out to my uncle when I was having some of these problems and asked, “What can I take to calm some of this acid reflux and these intense symptoms? I am just feeling sick.” He advised me and helped me with some stuff, and I started taking some medication.
I am one of those people who reads the bottle and only takes it if I need it. That goes for pain medication and all that kind of stuff. I took it for 14 days, and it made me feel a little bit better. I thought, “Okay, this is great. I am feeling good.” The acid reflux had calmed down.
As soon as I came off of it, it got severely worse, to the point where if I ate anything by mouth, even drinking water, it made me vomit. It was making me so sick. The entire month of July 2021, I essentially spent on the sofa. I could not eat anything. We tried everything from crackers to chicken noodle soup, all of your grandmother’s secrets to help you feel better.
Of course, at the age that I was and with COVID going on, I had been healthy before all of this happened. I had no idea that I would be facing stomach cancer. So I did not have a built-up primary care physician or know where to turn. I was Googling and talking to people, and asking where I should go.
To get into anything then was insane because nobody was taking new patients. I finally got into a GI place.
My initial GI visit and missed testing opportunities
The woman I saw, her first plan for me was, “Okay, we are going to get you in for an endoscopy.” Nothing was leading up to that. We did not talk about H. pylori possibilities. We did not do a breath test. We did not do all these things.
She put me on pantoprazole. I have now learned, after the fact, that the first thing we should have done was test for these things, which I did end up coming back negative for—H. pylori and all that stuff. But I would have had to come off the pantoprazole, which was helping me with some of my acid reflux symptoms. I would have had to come off it for two weeks for them to actually even do the test.
The advice I had gotten from my family was, “Before we go to this extreme where they have to put you under to do the endoscopy, let us see what else we need to do first,” because that is a pretty extreme first step. So I ended up getting into a primary care office about a week after I went for this GI consultation, and that was even worse than my GI thing.
I had an alarming ultrasound and was urged to go to the ER
The only good thing the primary care provider did for me was to send me for an ultrasound of my stomach area. When I went in to get that done, the tech who did it asked, “When was the last time you ate?” I said, “I followed your directions. I have not eaten or drunk anything in the last 12 to however many hours. Why?” She said, “Because your stomach is full.”
She showed me the picture, and it was big and full. I was advised to go to the ER. I thought, “I am not going to go spend $1,000 at the ER when the estimate for doing this endoscopy was like seven or eight hundred bucks. I will just go back to the GI.”
It was a bit of a fight on that aspect, too, because the PCP was saying, “You need to go to the ER right now,” and was very insistent. I ended up going back and getting in with the GI. Instead of seeing one of the physician assistants, the GI actually called me to get me in almost immediately because he looked at my chart and the notes that the other provider had taken, and he got me in immediately.
Rapid escalation: scope, CT, and oncology referral
I went in, I think it was a Thursday, and met with him. The following week, he got me in for my scope. I think I went on a Wednesday for my scope. Friday, he had me in for a CT. The following Monday, he had me connected with his oncologist partner, who I still see today—my current oncologist.
I went in for my oncology consult and my surgical consult on Monday. By that following Thursday—so the same week—after my Monday consult, they had me in for a diagnostic laparoscopy and to place my port. This was all done before we even had my pathology back. We got my pathology back the same day that I met with my oncologist.
My oncologist called it without even having the pathology report back. He said, “You are either going to be a stage two or stage three, depending on what they find—how much it has gone into the stomach lining.” I ended up being a stage three when they went in and did the diagnostic laparoscopy.
The phone call, my panic attack, and hearing “oncologist”
Before I actually went in to meet with the oncologist, I received a phone call. I did not have any idea that it was going to be a cancer diagnosis. My GI doctor did not have the results yet, and he did not have the pathology. He said, “It could be cancer,” but there was no real discussion yet.
He wanted to fast-track me. I received a call from the oncologist’s office. I looked up what an oncologist was because I had no idea, and I literally almost died—or at least it felt like it. I looked it up, and, as I said, I had been struggling to eat. I had lost a bunch of weight.
I think I was at 109 pounds. I used to be about 130–135 pounds. When I started getting sick, I was about 120. By the time I actually got in and was diagnosed, I think I was at about 109 pounds, maybe 105. I cannot remember exactly now. I was not eating, and every time I ate, I was throwing up.
When I got that call, I had a panic attack. I literally had a panic attack to the point where I almost felt like I was going to black out. I could not move my hands. I was trying to text my boyfriend when I got this, and I was just really freaking out about it.
I am very blessed that I have some friends who live really close to me. Instead of me calling 911, I had a girlfriend who came over, and I had a couple of friends who came and visited with me and soothed me and calmed me down. It was a pretty freaky experience. It is not an easy diagnosis to get.
Involving my family and getting a second opinion
My second opinion was pretty much my uncle’s. When all of this started coming down the pipeline, I called him because he is essentially my dad—my dad is not in the picture.
My uncle has a medical background. He is a retired pediatrician and did a lot of education and other things, so he was my go-to for all of this.
When I found out about this, I called him immediately, and he actually flew out here to be with me for my first appointments.
Understanding the tumor location and the possible removal of my stomach
It is interesting when I talk to different people. When I talk to my significant other, he remembers things a little differently, but we both remember how intense it was.
When we went and met with the surgeon—again, this was all before having the actual pathology report back—my stomach cancer was at the base of my stomach. It was covering my pyloric sphincter. That was why nothing was going through, and it was all coming back up. Nothing could pass into my small intestine. I was not passing bowel movements or doing any of those types of things. It was all coming back up as vomit.
When I met with the surgeon, we were sitting in his office, and he was showing me this diagram. He said, “Okay, I am going to have to cut out probably at least 50, if not more, percent of your stomach. This is where your tumor is. It is at the bottom of the stomach, and down here is where everything is supposed to come through. This is all being blocked off. I am going to have to get clear margins and come up higher to wherever I get clear. I may have to take your entire stomach.”
That was freaky in and of itself. I asked, “What if the chemo works?” We were now having a conversation about both. We would start with chemotherapy and then go into surgery if chemo shrank the tumor, because essentially the plan was: start with chemo, shrink the tumor, and then go in and do the stomach removal to whatever portion he needed to — 30, 40, 50, or even 100 percent of my stomach.
Facing life without a stomach, and my initial treatment plan
My biggest question was, “How am I going to live without a stomach?” It is one of your most needed organs for processing food and nutrition and all those types of things. There are definitely ways around that, because I am still here. But it was terrifying.
We did the surgeon consult with that fear of his taking my stomach out, and then we went and met with my oncologist. The process was to do four rounds of chemotherapy and then have an endoscopy to see how much the tumor had shrunk or reduced in size. Then we would make the plan for getting me in for surgery.
I am a BRCA1-positive. I have BRCA1, which is the gene mutation that usually puts you at a predisposition for either ovarian or breast cancer. I actually do have breast cancer in my family. My mom passed away from breast cancer when I was seven years old. Her mom passed away about a year after her. I have multiple family members on either side who have had breast cancer.
Honestly, I thought that was going to be my cancer. It turned out that BRCA actually caused my stomach cancer.
Tumor disappearance, major surgery, and creating a new stomach pouch
My tumor actually shrank and was gone by the time we did my endoscopy before my surgery in November. I am coming up on four years celebrating my 80 percent removal of my stomach and my gallbladder. On November 4th of this year, it will be four years.
When we did my endoscopy before my surgery, my tumor was completely gone. I was very blessed that my response to chemotherapy was pretty much 100 percent. The surgeon went in and did an 80 percent removal of my stomach. They brought my small intestine up and attached it to my esophagus to whatever is remaining of my stomach up there. Then he created a little pouch for me. I no longer have a full stomach; I have a little pouch that they made with a hole in it that goes down into my small intestine.
He also removed my gallbladder at that time, too. There was no metastasis there, but they say that the gallbladder tends to become an issue with some of the things we have going on with this specific cancer. I am actually very grateful he took it.
Completing chemo and radiation, and my first declaration of NED
We did four rounds of chemotherapy, the surgery, and then I ended up having 25 rounds of targeted radiation. Then I had four more rounds of chemo. It was a process.
I got my first NED—no evidence of disease—in March of 2022. We continued on a PARP inhibitor that is supposed to target the mutation, my genetic mutation. We had me on that for about a year. We continued with scans to make sure nothing was showing up.
A suspicious PET scan and surprise hysterectomy findings
I had a PET scan that came back looking really weird in, I think, August or September of 2023. My oncologist was on me to get my ovaries removed because the PET scan was showing some weird stuff down by my ovarian area. They were uncertain exactly what it was or what it could be.
I finally decided to do a total hysterectomy. In April of 2024, I got scheduled and went in for my total hysterectomy. That surgery was estimated to be an hour and a half, but ended up taking four hours. He brought in a second surgeon because I had metastases to my ovaries, my tubes, and my peritoneal lining. It was on my spleen and my liver. We also found out there was some in my small bowel.
Again, I have been very blessed with my team of doctors. He could have easily said, “I am not touching this,” with the amount of metastases he found. Instead, he brought in somebody else to help, and they removed everything they could within the scope of the hysterectomy.
We proceeded to start me on chemotherapy again, just on a different drug. I asked my oncologist, because it went into my peritoneal area, if we were going to do something called HIPEC.
HIPEC and major cytoreductive surgery
We found the recurrence, and we decided to get me back on the old chemo drug. I talked to my oncologist about doing HIPEC. He referred me to my HIPEC surgeon, who was amazing. We got me qualified.
I think I had five or six treatments of that one particular chemo drug. We ended up having to take me off one of those drugs because I was having some really bad allergic reactions to it. That kind of chemotherapy is intense. It really affects your body.
I met with my HIPEC surgeon in, I think, July of last year and went in to get my PCI score done to make sure that I could qualify for HIPEC, which I did. I think I ended up with a score of 10 or 11. I qualified for HIPEC.
The first HIPEC that we scheduled was at the end of September last year. It was done laparoscopically. They did three incisions, one on either side of my abdomen and one in the middle so they could have the camera in there. Then, five weeks later, they had me come back and do open surgery. He did open HIPEC with CRS, cytoreductive surgery. He went in and removed all of the tumors that he could see or cancerous areas that were questionable.
He also did a splenectomy. They removed my spleen, two feet of my small intestine, the spot that was on my liver, and anything else they could find. That was my big surgery back in November last year.
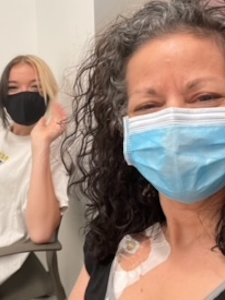
Ongoing immunotherapy and close surveillance
We have had me on immunotherapy since my recurrence in April of last year. We are also doing a ctDNA blood test called Signatera. Unfortunately, my last Signatera test just came back showing positive. We do not know if it is a false positive or not.
Right now, the plan is to have me on immunotherapy for two years, starting last April when we started it. I still have probably another 6 to 8 months, potentially more, depending on how my body holds up to it. Currently, I go every six weeks for immunotherapy.
We do all the scans. I had a PET scan done in June. We just did a CT scan. I am going for another endoscopy and colonoscopy here in the next month or so. We are on surveillance at this point, along with the immunotherapy.
They cannot really do anything with any of the positive tests until they see something again. That is kind of where we are sitting. Every three months, I am doing a scan. Unfortunately, none of my stuff shows up on my scans. A CT scan is just protocol with this, but I do not ever expect to see anything.
If my next Signatera test comes back positive, the plan would be to go in for another diagnostic lap to see if they can find what or where the potential cause of the DNA showing cancer circulating in my bloodstream is.
I’ve adapted to life without a stomach
The biggest challenge has been the lifestyle change. Losing your stomach is huge. When they first did my stomach removal, there were a lot of things I could not eat. You have to be very cautious and conscientious about what you are putting into your body, which, I mean, we all should be, but especially after this kind of surgery.
When I first had my surgery, I would go into severe dumping if I ate certain things. The first six to eight weeks after my stomach removal, I could not eat any bread products or pastas or those types of things. I could not have coffee because it would just put me in the bathroom.
Now, four years out, I have gotten used to my new way of eating and drinking. I have to have a plan. I feel like I am always continually thinking about eating because I have a very small pouch. I do not have a stomach, so I have to continually eat throughout the day. If I forget, you will know, because “hangry” is definitely a thing. My boyfriend will say, “When was the last time you ate?” and I am like, “Oh, was I that mean? I am so sorry.”
I live with the fear of recurrence, but I’ve chosen joy
It is always at the back of my mind: When is the next recurrence going to happen? I will be completely honest. I live my life, and I live my life to the fullest, but it is always going to be there.
When people ask me, and we talk about it, and I say, “Oh yeah, I have been NED since last year,” they say, “Oh, congratulations, that is great.” And it is. I will live my life to the fullest, and I will do everything every day. I tell people that we could all walk out tomorrow and get hit by a car, to be honest.
But I feel like I live my life differently because I know that I may not make it another twenty years.
Finding strength and support through family, friends, and stomach cancer communities
I am much more on Facebook than I ever was before this diagnosis, but I had the same question as a lot of people: I had no idea. Stomach cancer is not a very well-known or talked-about cancer. It was actually quite difficult for me in the beginning to find people who were like me.
My family was all very helpful. My cousin’s wife recommended that I get on Facebook and look at some of the different groups that were specific to stomach cancer. I ended up connecting with a couple of different organizations.
One that I am really involved with is called Debbie’s Dream Foundation: Curing Stomach Cancer. They are based out of Florida. We do a lot together. I do mentorship with them because they offer a mentorship program. If people want or need help and want to know about treatment and different things, I am really active with them for that, and for advocacy.
We go to Washington, D.C. every year to talk to our legislators to make sure that they continue funding stomach cancer research and allocate funds to our specific disease. Stomach cancer is one of the top five deadliest cancers, yet it receives a very minimal amount of funding for research.
We go every year for advocacy with them. I am also part of a smaller group called Hope for Stomach Cancer. They also do a lot of education—so does Debbie’s Dream—with different symposiums and things. Hope for Stomach Cancer also does the same thing.
We call each other family, to be completely honest. Next month, I am going out [to Los Angeles] because November is Stomach Cancer Awareness Month, and Hope for Stomach Cancer is doing a patient summit in LA. I am going to see some of my “family” and get some good knowledge on what is going on in the stomach cancer world.

Inspired by Niccole's story?
Share your story, too!
More Stomach Cancer Stories
Andy G., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Stomach pain, back pain, chest pain, extreme exhaustion, shortness of breath after short walks
Treatments: Chemotherapy, immunotherapy
...
Alyssa B., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...
Brittany D., Stomach Cancer, Stage T1b
Symptoms: Choking suddenly while eating and attempting to speak, neck and right shoulder pain, neck tightness, trouble swallowing certain food items
Treatments: Surgeries (subtotal gastrectomy, D1 lymphadenectomy, gastric bypass)
...
Camilla C., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Issues swallowing, swollen gland in the neck
Treatments: Palliative chemotherapy was offered but declined, nutritional changes to support her comfort and energy, meditation and mindfulness practices, self-directed healing methods
...
Emily D., Stomach Cancer (Gastric Adenocarcinoma), Stage 4 (Metastatic)
Symptoms: Persistent postpartum stomachache, early satiety, difficulty swallowing, vomiting
Treatments: Chemotherapy, immunotherapy
...
Alyssa B., Stomach Cancer, Stage 4 (Metastatic) (Hospice Update)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...