Nick’s Stage 4A Colorectal Cancer Story
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal
Nick’s symptoms began a year or two before his diagnosis, including changes in bowel habits, size, and consistency, blood in the stool, and abdominal pain, which he initially attributed to aging or irritable bowel syndrome. After experiencing fatigue and escalating pain, he went to the ER where he was diagnosed with diverticulitis and sepsis. Despite initial treatment, he required a laparoscopic washout due to a perforated colon and subsequent complications, including an abscess.
During a follow-up colonoscopy, doctors found a mass, which was later confirmed as adenocarcinoma. He underwent a sigmoid resection, removing part of his colon. While clear margins were achieved, 19 of 49 lymph nodes tested positive for cancer.
Nick began CAPOX chemotherapy, experiencing severe side effects like fatigue, neuropathy, and an acne rash due to the addition of Avastin (bevacizumab). When they noticed an elevation in his tumor marker and growth in his lymph nodes, he was switched to Keytruda (pembrolizumab), an immunotherapy, to reduce the cancer to a manageable level.
Nick emphasizes the importance of mental health support to manage anxiety. He advises listening to your body, advocating for yourself, and using support systems. He encourages seeking thorough medical evaluation for unexplained symptoms and finding strength in support groups, hobbies, and loved ones, stressing perseverance and finding reasons to keep fighting.
- Name: Nick S.
- Diagnosis:
- Colorectal Cancer
- Staging:
- Stage 4A
- Initial Symptoms:
- Change in bowel habits, size & consistency
- Blood in stool
- Abdominal pain
- Fatigue
- Treatment:
- Surgery: sigmoid colectomy
- Chemotherapy: CAPOX (capecitabine & oxaliplatin),
- Immunotherapy: bevacizumab, pembrolizumab

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
My symptoms started a year or two before diagnosis. It started with a change in bowel habits, size, consistency, some blood in the stool, and abdominal pain.
Introduction
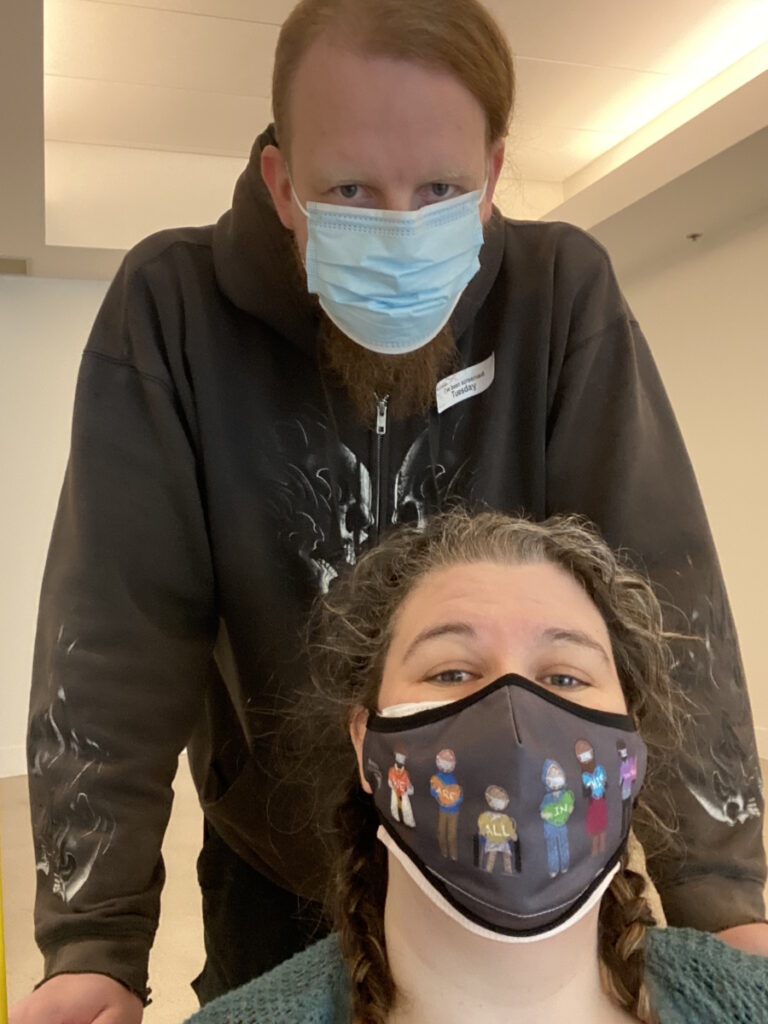
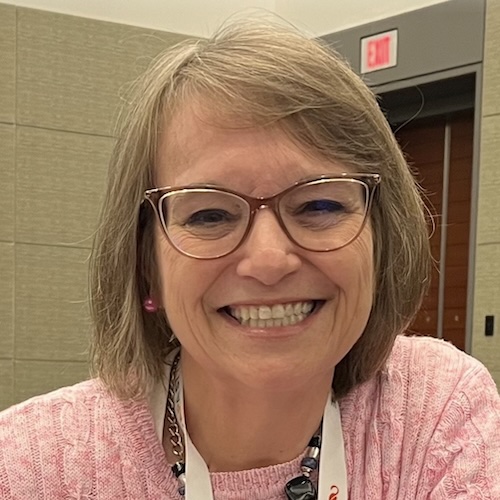
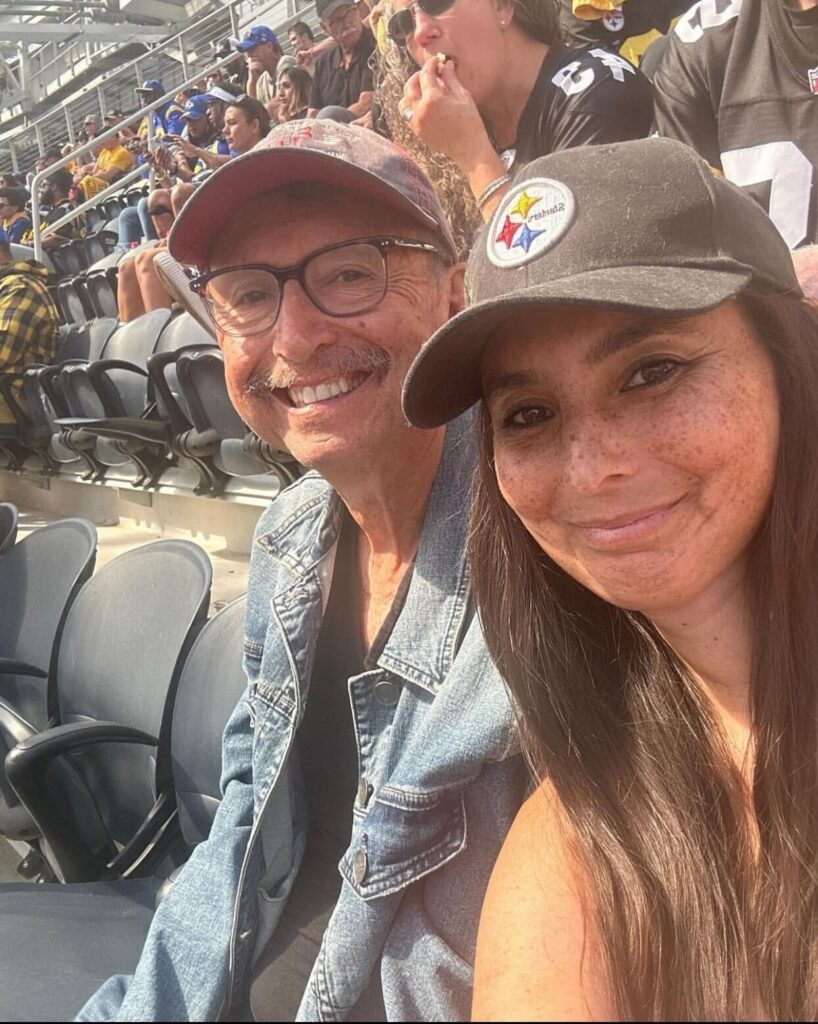
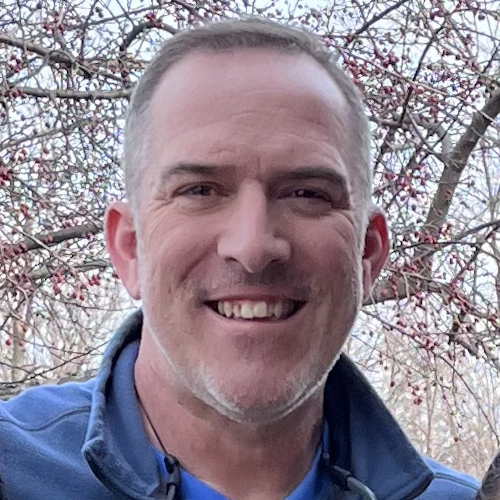
I’m a stage 4A colorectal cancer fighter. My wife and I live in Chippewa Falls, Wisconsin. We have a wonderful 28-year-old daughter.
I’m a full-time firefighter and critical care paramedic. I’ve been doing firefighting for about 16 years and paramedicine for about 13 of those 16 years.


Pre-diagnosis
Initial Symptoms
My symptoms started a year or two before diagnosis with stage 4A colorectal cancer. It started with a change in bowel habits, size, consistency, some blood in the stool, and abdominal pain. I had some acid reflux type of reactions that my wife and I chalked up to aging and not being as healthy as I could be. My wife has irritable bowel syndrome and I thought some of it was IBS because some foods would trigger some reactions in me.
I was working full-time for the department for about a decade and a couple of years later, I decided to change over to a neighboring department. For these jobs, we have to pass a physical agility test.
I have been working by myself daily. I was in pretty good shape. The test is a pretty rigorous test to be able to do what we do. I was 48. I was doing this at an older age than the 20-year-olds they were usually hiring.
I was diagnosed with diverticulitis and sepsis, so they started me on antibiotics right away.
A couple of months later, we responded to a house fire. At some point, my battalion chief pulled me off the line and said, “You look wiped out. I’m going to sit you out for a little bit to catch your breath.” I felt a little tired, but, again, I was getting a little older.
I sat out and went back in for another round. This time, the chief was on the scene and said, “Nick, take your gear off. You don’t look good. Go back to the ambulance. You’re going to be doing rehab, making sure everyone else is doing okay, but we don’t want you going back in.” I thought something was weird.
I called my wife to meet me in the ER. I didn’t know what was going on. I’ve got bad abdominal pain. I haven’t slept. I’m going to go get checked out.

Diverticulitis & Sepsis
I was diagnosed with diverticulitis and sepsis, so they started me on antibiotics right away. They weren’t sure if surgery was going to be necessary, but they transferred me to another hospital. At that point, I was stable.
When I got transferred, I met with a thoracic surgeon and started to realize that things were serious. He said, “We’re not going to go in right away. We’re going to keep an eye on you tonight. Hopefully, things will subside with some more antibiotics and some steroids, if we have to. But we’re going to keep an eye on you and evaluate you. We’d like to avoid surgery.”
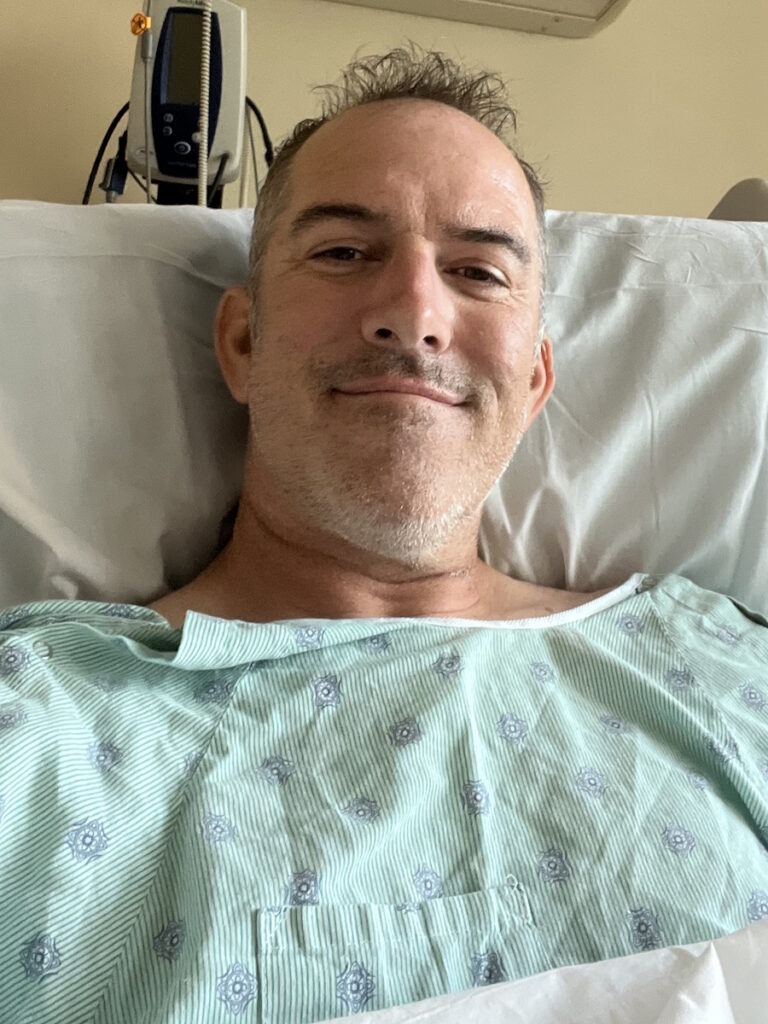
The next day, when they were getting my vitals, the nurses said, “We see you’re slated for surgery.” That turned into a laparoscopic washout. They found that I had a perforated colon in the sigmoid area, the area right before the rectum, but that had healed itself.
All of a sudden, I heard the doctors say, ‘That’s not good.’ I remember seeing a black mass on the screen.
They went in through a couple of small incisions, washed everything out to make sure there was no fecal matter, and stitched me back up. I had a couple of surgical drains. I was in the hospital for five or six days and then I was sent home to heal.
I ended up getting readmitted a couple of days later because I had some drainage coming from my drain sites. After a CT scan, they found I had an abscess. I believe E coli was one of the culprits. There was something else too, so they needed heavy-hitter antibiotics.
After another two weeks of antibiotics, the PICC line was removed. I met with the surgeon and everything was looking great. He said, “Let’s do a follow-up colonoscopy to check how the diverticulitis is.”


Colonoscopy
I wanted to sleep through it. I was joking with them and we were all relaxed when all of a sudden, I heard the doctors say, “That’s not good.” I remember seeing a black mass on the screen. He tried advancing past it and I said, “Ow,” but I didn’t feel it. I said “ow” instinctively. He said, “We can’t get past this mass. We’re going to pull out.” The tone changed. You could have heard a needle drop in that procedure room.
They wheeled me back into the recovery room where my wife was waiting. On the way there, one of the nurses handed me a polished stone that had the word “hope” stamped on it. I didn’t think that choked me up, but I carry it wherever I go. In hindsight, it meant a lot and drove home the seriousness of the situation. We didn’t know exactly what was going on, but something wasn’t right. I have enough medical training and field experience to read the room and know it wasn’t good.
The doctor eventually came back in and said they couldn’t diagnose it yet. They took a small sample to send off for testing to confirm what they thought it was. He wouldn’t say whether it was cancer or not.
The good news was they got the tumor with clear margins. They felt it hadn’t spread far…
Diagnosis
Getting the Biopsy Results
I was waiting for the results at home. When I finally got the notification on my phone, I checked it and it said adenocarcinoma. Now we know what we’re dealing with. It’s cancer of some sort. I never thought about it as a possibility.
Treatment
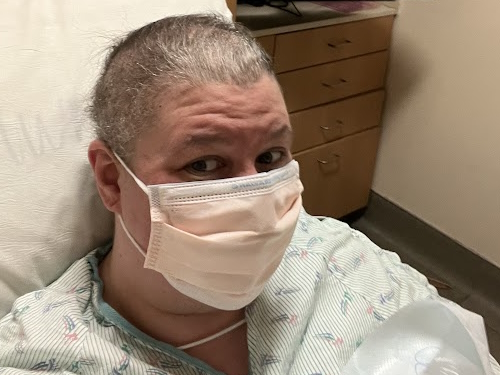
Sigmoid Colectomy
During the colonoscopy, he said we were going to have surgery because what it was had to come out. He referred me to surgery right away. Luckily, it was the same surgeon who performed my earlier surgery who I trusted with my life.
I met with him about a week later. They were going to do an exploratory surgery until they knew exactly what it was in there and then do their thing.


I remember being in the room when my mother-in-law came out too. My wife was there, of course. They wheeled me in, put in the IVs, and told me to start counting back from 100. I don’t think I hit 95. Hours later, I woke up in my hospital room with a slightly sore throat. They performed a sigmoid resection. I can’t remember how much of my colon they took out, but I didn’t require an ostomy, thankfully. They were able to resect it and reconnect it right away.
The good news was they got the tumor with clear margins. They felt it hadn’t spread far, at least in the tissue of the colon. But the surgeon sampled some lymph nodes right next to the tumor site. They took out 49 and 19 of them tested positive for cancer.
I stayed positive. The whole reason I’m in this fight is my family.
CAPOX Chemotherapy
At that point, I was referred to oncology. I met with my oncologist. His nurse was a former ER nurse who I was familiar with and seeing a familiar face went a long long way.
He explained what he planned on doing based on the CT scans. They saw some inflammation in other lymph nodes and they weren’t sure if that was post-surgical. They wanted to do another CT scan to check, but they were happy about the margins being clear. I was staged at 3C then. It metastasized a little bit past the point of origin but not very far.
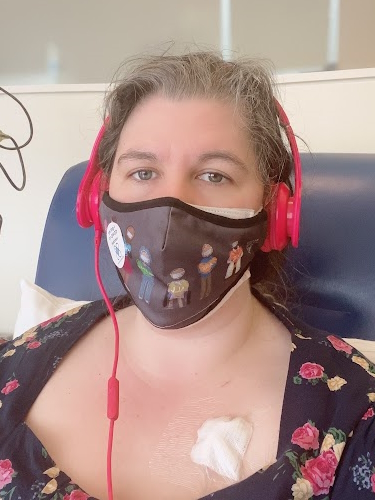
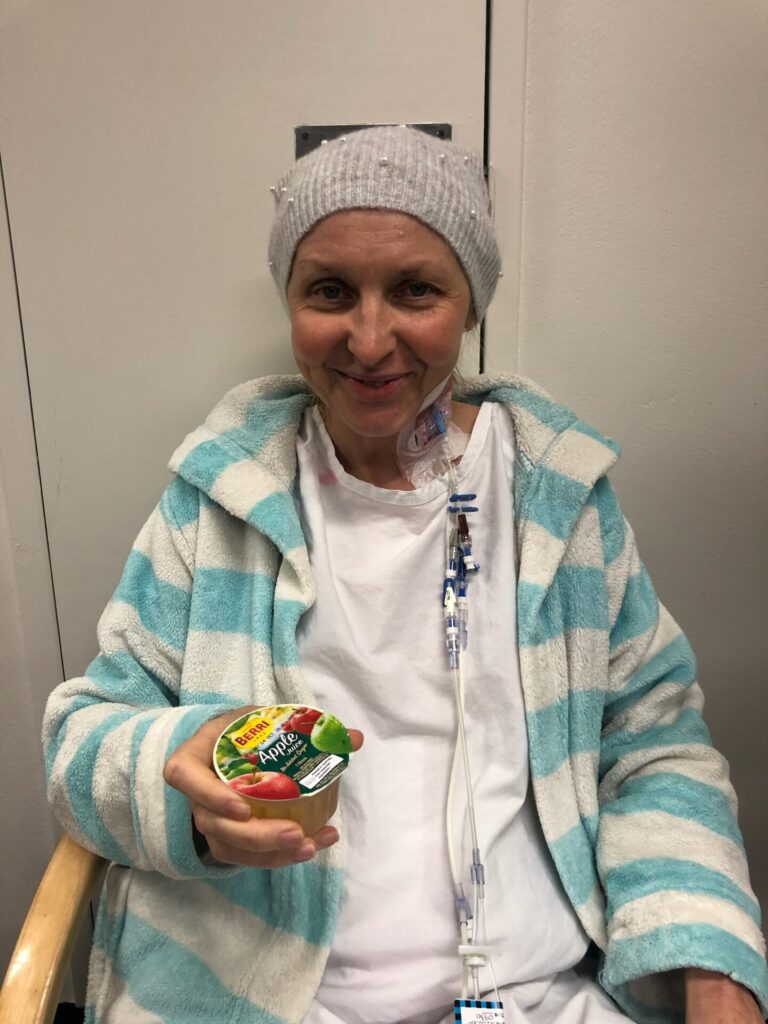
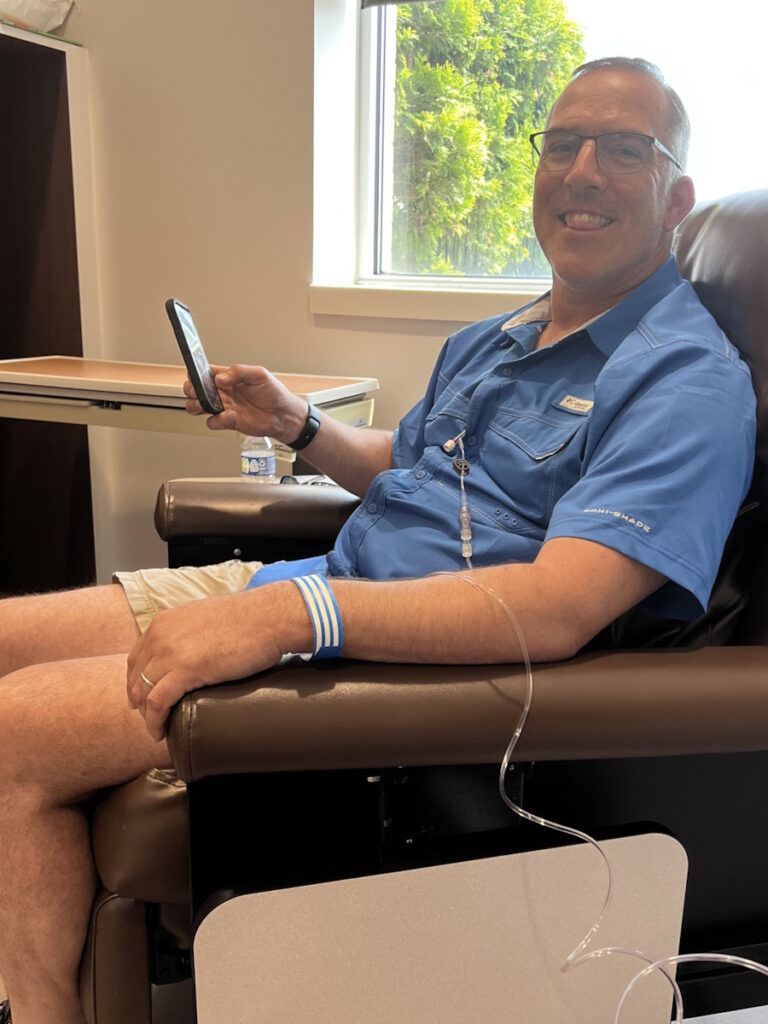
The first day of chemo was going to include labs and a CT scan to see where we were at. The plan was to do CAPOX: capecitabine, an oral medication, and oxaliplatin, an IV medication. I would do the oral chemo for two weeks and then on the third week, I would go in for the IV chemo. They would do labs on those days to make sure everything was okay.

Unfortunately, the doctor didn’t like what he saw on the CT. He wanted to get a little more defined imaging, so he set me up for a PET scan and delayed the chemo. A couple of days later, we came back to start chemo again and get the PET scan read.
The doctor confirmed that it had spread to the lymph nodes in the abdominal area, along my aorta, and up to my left shoulder. It had spread a lot further than we thought it had.
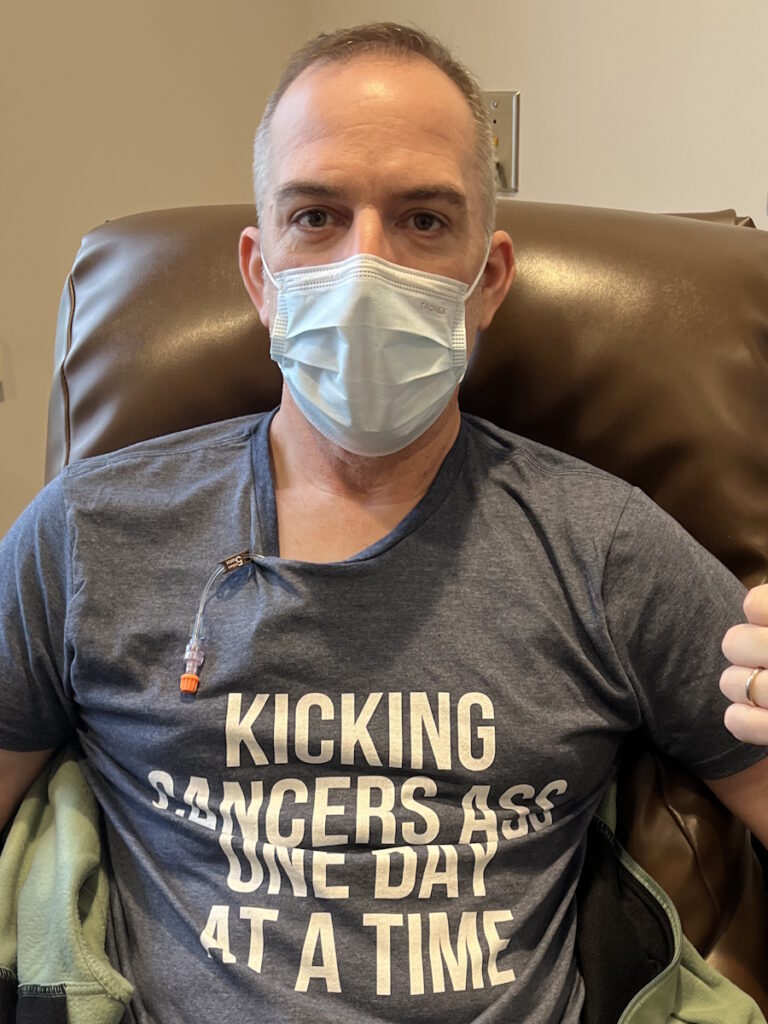
I felt like every time we made a plan to move forward, we were getting kicked back a couple of steps, but I stayed positive. The whole reason I’m in this fight is my family. I believe that someday, this cancer will get me, but I’m not going down without a fight. I’m stubborn, so it’s going to be a long fight. I won’t go down without swinging.
I have a four-day weekend so I tried to time my infusion, so I had a couple of days to recover post-infusion and feel somewhat human before returning to work.
Side Effects of CAPOX Chemotherapy
Chemo wasn’t fun. It knocks you out. I felt fatigued on the first day. For probably a week and a half, when you start getting the infusion, you can’t drink cold drinks. It felt like swallowing glass shards. A lot of fatigue and neuropathy kicked in.
I didn’t like being out in the cold and I love ice fishing. You’ll catch me outside at -20°F on a normal day, but with chemo, not a chance. I had to be bundled all the time.
My eyes were always drying out, so they hurt a lot. I had insomnia, joint pain, and muscle pain.
They added Avastin (bevacizumab), which is an immunotherapy, to my chemo routine. That caused a bad acne rash on my back from the waistline up to my neck. The doctor had never seen nor heard of it, but we can only attribute it to Avastin.


Working While in Treatment
I was able to go back to work full-time as a firefighter. I have a four-day weekend so I tried to time my infusion, so I had a couple of days to recover post-infusion and feel somewhat human before returning to work.
My work was very accommodating. We’re firefighters, so we don’t sleep all day, but the chief said if I needed to rest, I could go to the dorm, which I appreciate. I never took him up on it. I tried to stay with my brothers and sisters training or doing calls, and that worked great.
I was going to be on treatment for the rest of my life. I might get some time off if we get no evidence of disease at any point, but it will come back at some point and I’ll have to go back on treatment.
Switching to Immunotherapy
The initial plan was for six months or eight cycles of chemo and Avastin. Unfortunately, because of the restaging, I was going to be on treatment for the rest of my life. I might get some time off if we get no evidence of disease at any point, but it will come back at some point and I’ll have to go back on treatment.
My tumor marker was through the roof when this all started and it was dropping with chemo. We were seeing shrinkage in the lymph nodes. Chemo sucks, but it’s doing what it’s doing, so we stayed very positive.
When we got to cycle six, we noticed my CEA was going up a little bit. We were doing CT scans every three months and we noticed some growth in the lymph nodes. The doctor said, “We’re going to stop the chemo. It’s not working. You can only receive so much oxaliplatin before it becomes completely ineffective. This saves us a couple of cycles where if we need to go back to it, we can go back to it. We’re going to switch over to an immunotherapy called Keytruda (pembrolizumab).”

The side effects of immunotherapy are supposed to be much less than chemo and I’m all for that. I switched from chemotherapy to immunotherapy in August 2023. I still have very slight neuropathy every now and then in my toes and my fingertips. Nothing debilitating but a reminder that I was on chemo at one point and that probably won’t get any better or any worse, hopefully.
Keytruda is a half-hour infusion. Side effects are minimal. Between cycles two and three, while we were camping, I noticed that my resting heart rate was higher than it should be. I was not exercising as much and a little out of shape, but I shouldn’t have a resting heart rate of 130-140 beats a minute. I was sweating a lot without doing anything, so I couldn’t figure it out. I talked to the oncologist and they ran some thyroid tests.
One of the known side effects of Keytruda is thyroid burn. It’ll cause hyperthyroidism until the thyroid burns out and then it’ll cause hypothyroidism.
The support of my family, my work family, and my friends is what gets me through this.
Treatment Plan
We want to do Keytruda for 18 more months. It’s a two-year plan. We’ll see what it does and go from there. Hopefully, the response brings everything down to normal levels, I won’t have evidence of disease, and I can ride that out for a while.
Fingers crossed, maybe Keytruda is the cure for colon cancer, but realistically, I don’t think so. I think it’ll be a lifetime battle, but it’s going to be a long life. The support of my family, my work family, and my friends is what gets me through this.


Managing Scanxiety
As a paramedic, I’ve dealt with patients with panic attacks and anxiety. Anxiety’s a real thing. A lot of times, it doesn’t seem like it with the patients you’re dealing with, but now that I’m put in that position, it’s a real thing. I’ve dealt with it even before cancer through another set of unfortunate circumstances and luckily, I have a great support group in place.
We see a lot of things as paramedics and firefighters, so after a while, you realize things aren’t normal. I had to start paying closer attention to my mental health. I started seeing a therapist and she’s great. She taught me how to deal with stress, anxiety, and my feelings.
What we go through as cancer patients is not something most people go through nor is it something they understand.
Stay strong and recognize that the stress is real. What we go through as cancer patients is not something most people go through nor is it something they understand. Take a deep breath. Listen to what your mind and body are telling you.
Your feelings are valid. Don’t try to brush it off and try to be strong by pushing your way through it. Rely on your support team. If you have a therapist, talk to that therapist.
Most oncology teams come with a social worker. Use that resource. Rely on your family for strength. Tell your spouse what you’re feeling even when you don’t want to. Sometimes talking about it gets it out there and puts it away, as opposed to it weighing you down.
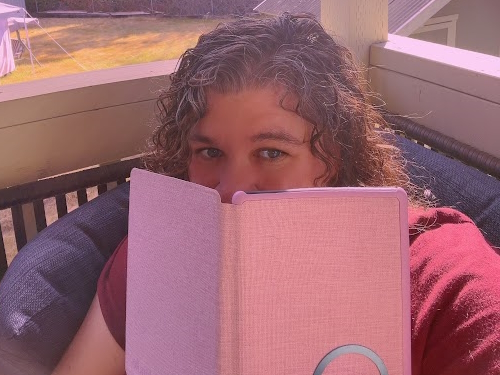
What helps me is retreating home, spending time with family, or staying busy with work. Rely on your hobbies if you have any. If you don’t, find some. I’m a big fisherman. I love fishing. You could put me on a lake and even if I couldn’t catch a fish for days, I would be in my happy place. Find something that helps you disconnect from the cancer and what you’re going through.


Words of Advice
For anyone who might be experiencing symptoms that you’re not quite sure of, listen to your body. Talk to your doctor. Advocate for yourself. If you feel something’s not right, push for tests to try and figure out what’s going on. The answer, “We don’t know what’s wrong with you,” is not acceptable. Push to find answers.
For cancer warriors who are going through this, keep going. You’re not alone. There’s support beyond your family, friends, and coworkers. There are a ton of support groups online. There are social workers available. There are platforms like The Patient Story.
(For more support options, please visit one of our many partners such as Colontown or the Colon Cancer Coalition.
You’re not in this alone. Some days, it may feel like it. Some days, I get down in the dumps, but I find something to get me back up. I find a reason to keep going. There are a million reasons to keep going and even if you find just one, that’s all it takes.
Listen to your body. Talk to your doctor. Advocate for yourself.
Inspired by Nick's story?
Share your story, too!
More Colorectal Cancer Stories
Cora V., Colorectal Cancer, Stage 4 (Metastatic)
Symptoms: Fatigue, unintentional weight loss, blood and mucus in stool
Treatments: Chemotherapy, chemoradiation, surgeries (temporary ileostomy and reversal, liver surgeries and ablation)
Monica D., Colorectal Cancer, Stage 1
Symptoms: None; caught at a routine colonoscopy
Treatment: Surgery (low anterior resection with temporary diverting ileostomy)
Edie H., Colorectal Cancer, Stage 3B
Symptom: Chronic constipation
Treatments: Chemotherapy, radiation, surgeries (lower anterior resection & temporary ileostomy)
Shayla L., Colorectal Cancer, Stage 4
Symptoms: Stomach sensitivity, food intolerances, exhaustion, blood in stool
Treatments: Chemotherapy, surgery (hepatectomy)
Tracy R., Colorectal Cancer, Stage 2B
Symptoms: Bloating and inflammation, heaviness in the rectum, intermittent rectal bleeding, fatigue
Treatments: Chemotherapy, radiation, surgery
Paula C., Colorectal Cancer, Stage 3
Symptoms: Painful gas, irregular bowel movements, blood in stool, anemia, severe pain, weight loss, fainting spells
Treatment: Surgery (tumor resection)