Brad’s Smoldering High Risk Multiple Myeloma Story
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez

After having been diagnosed with smoldering myeloma in December 2019 and smoldering multiple myeloma at a second-opinion consultation just a few months afterwards, Brad was diagnosed with smoldering high risk multiple myeloma in October 2022–with a 50% chance of it becoming active within 2 years. Constant bone pain and worsening lab results as of April 2024 make it likely that he will need to start treatment soon.
Although the last few years of Brad’s life have been challenging, to say the least, he has taken refuge in his faith, derives strength and comfort from his relationship with his wife–a breast cancer survivor–and also possesses a can-do attitude that stands him in good stead. By sharing his story with us, he helps inspire and offers advice to others facing the same situation.
- Name: Brad H.
- Diagnosis:
- Smoldering high risk multiple myeloma
- Initial Symptoms:
- Abnormal kidney function (stage 2 kidney disease)
- Mild anemia
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
… the most important thing that you can do as a cancer patient is to live through your cancer.
Introduction
Hi, I’m Brad. I grew up in the Twin Cities area of Minneapolis.
I wear many hats. I work in the IT telecom space. I’m a professional musician. I’ve taught all my life. And I’m also a woodworker and love to golf, but I don’t do that much anymore because of my back.

I started my myeloma journey as an actual monoclonal gammopathy of undetermined significance (MGUS) person. And my current diagnosis is that of a smoldering high risk multiple myeloma.
Looking to start treatment sometime this year, according to the health professionals.
Discovery
My smoldering high-risk multiple myeloma story starts in July 2016. My primary care physician noticed that my kidney function was starting to change and that also we were starting to see my hemoglobin going down.
Now, as a type two diabetic, I’m fully aware of hemoglobin A1C, but I hadn’t really thought much about the rest. Red blood cell and hemoglobin and all of those.
So he noticed that it was getting dangerously low. So he started to say, well, why is that? And from that standpoint, we started to go through the process of a colonoscopy, let’s do an endoscopy, let’s find out if you’re bleeding somewhere. And he went through this and did the watchful waiting.
And essentially I had no abnormal feelings. I wasn’t feeling any nauseousness or dizziness. I was, you know, just kind of surprised that that was the case.
And he finally says, well, I’ve done everything I can think of. I guess we’ll send you to check with a rheumatologist. And I thought, okay, you know, having a compromised immune system, I guess that could be a possibility.
So I remember going in after the bloodwork to the rheumatologist, and the rheumatologist looked at me and said, why are you here? You have no reason to be here. You have no rheumatological issues. Okay. Thank you very much. It was one of the shorter appointments I’ve ever had in my life.
And so I reported that back to my primary care. And he says, well, you only have one more option. And so I was off to the hematologist. And in the process of the hematologist, you know, you have to go through normal blood work. Then you have to do your imaging because they wanted to do a full skeletal survey. Do all the blood work, do all those things, and then you show up for your follow up.
And so the doc says, so you have some abnormal proteins in your urine. And also we’re finding this thing called MGUS.
Diagnoses and progression
MGUS
I’m thinking, okay, what does that truly mean?
After I left, I find out that this is a non-cancerous precursor. But there’s a really bad one down the line called multiple myeloma. And your survival rate, according to those years, 2016, 2017, was not particularly good because the treatments were not strong enough to really knock it out. So that was my initial diagnosis.
Then the bone surveys show some minor lesions, lytic lesions, osteolytic lesions. And the top of my head, I remember that it was tender to the touch. But hey, you work out in the shop doing woodworking. Who knows if you hit your head doing whatever, or if you were bonked on your head by your wife while you’re asleep.

My doctor, he gets this diagnosis and he’s a little concerned because that is a step forward in your prognosis and in your diagnosis. So he goes to his buddy, another radiologist who looks at it, and they go, it really doesn’t look like anything. And I’m thinking, okay, well, this is good.
But I’ll tell you what, because your numbers keep on increasing. Maybe we should go ahead and do a bone marrow biopsy. And your kidney function is also getting a little bad because I’d been to a nephrologist, a kidney specialist, and he diagnosed me with stage two of kidney disease. Okay, let’s go have a kidney biopsy and we’ll do the bone marrow biopsy as well.
I chose to take sedation because it’s really, really painful. And you have to be sedated when you’re doing a kidney biopsy.
So December comes of 2019, and I remember taking my wife with me because I was concerned about this particular diagnosis. And we went in there and the doctor tells me that I have progressed. Now the progression percentages from MGUS to anything else is 1% a year. It’s barely been a year for me–and I’m already progressing, so I’m already over performing the wrong way.
Smoldering myeloma
And so here I was with a smoldering myeloma, which is again asymptomatic. Non-active myeloma.
Don’t worry about it. You know your chance of progression is 10% a year over five years. Okay, that sounds good. But the one important thing that everyone that has this particular stage diagnosis. I know you like your oncologist locally. But you need to get to a myeloma specialist. And being that I live about 250 miles away from Houston, I had two choices.
My wife is a breast cancer survivor, and she did her work at Cancer Treatment Centers of America up in Tulsa. So I wanted a second opinion. I wanted to make sure that we were all aligned on what my next steps are supposed to be.
Smoldering multiple myeloma Kappa
So I checked out Cancer Treatment Centers of America. I talked to MD Anderson in Houston, and I chose to go to MD Anderson because they’re a research hospital.
I happened to be scheduled with the head of the myeloma and lymphoma clinic at MD Anderson, and that was a great comfort to me. I remember making that appointment and everyone knows where this is going.
I’m now having this conversation with Anderson, and they want all my labs and they want all these other things.
So my appointment was in April of 2020, which again should remind everybody of something. So here I am waiting for all of this material to get to MD Anderson so we can go down and have a conversation. And there could be a consult. And so the date arrives and it’s toward the middle of the month. And I’d already made my reservations in Houston, and I’m driving down to Houston.
We’d already had closures, people threatening closures, and things were still relatively open so I could stop at gas stations and I could get gas if I needed to. But I came fully prepared to kind of be socked in and not have much opportunity. So I’m about 70 miles from Houston. My hotel calls–“We’re closing down.”
So I’m trying to find out where I might be able to stay. It’s a ghost town. There wasn’t anybody around. And so I put my stuff away. So the next morning I go in and meet my myeloma specialist,
You have to go through the entire intake process and they weigh you and they do all of those things. And I remember that the person, not the cancer doctor, but it was her assistant who’s also a doctor, came in and she explained what I have. And so the doctor came in, we talked about it, and she says, okay, here are your jugs. We need for you to do a 24 hour urine, and it needs you to schedule a PET scan tomorrow.
So I went through that process, did the PET scan. And so it was confirmed. She sent me a note. And so now it was watchful waiting.
Watchful waiting
So watchful waiting means that essentially, just like the words state, you are sitting here and you’re having blood work done at a regular time, and they’re looking for markers. They’re looking for changes.
Now, the thing is, nobody will tell you what those changes are. They won’t tell you what your light chains or what your ratio is or anything like that.
But watchful waiting means that you go to doctors offices 4 to 6 months, and I would choose to go every 6 months with my local doctor and every 6 months with MD Anderson. And I was able to schedule those. So every 3 months I was having some kind of bloodwork because I was not going to be the guy like on a lot of these stories. I didn’t have any idea. And all of a sudden I found myself on the floor with back problems.
It was really tough. And even going to get labs done, we decided that we would go every 6 months. So I spaced it out every 3 months. So it was 6 months local, 6 months down at MD Anderson.
So every 3 months I was having labs done. Plus I’d have my diabetic labs done. So I was doing a lot of blood work. But I decided that MD Anderson was going to be the decision maker on my care plan.
I did all of my major bloodwork and 24 hour urine collection with Anderson, because I felt that you have a nephrologist on staff. You have everybody that you need on staff.
And so MD Anderson stated that my treatment plan was going to be–come down, visit us. And during Covid we can go ahead and do virtual visits if you would like.
And so that worked out well. I would go down for my labs. And my drive for labs was to get up early in the morning, drive down to The Woodlands, which is a northern suburb of Houston. Do my labs turn around and come back. That allowed me to continue to work.
And so I could have calls while I was driving to work or driving down there and back. Managed projects, do whatever I needed to do. And then I would have a follow up with the care team and I would visit my local oncologist live.
Complications due to COVID
Covid provided unique opportunities for the United States. And it became obvious that people were supposed to be testing for Covid. They wanted you to take a shot.
I’m thinking to myself, I’m not going to take this. I’m going to take my chance. I don’t believe that this has been tested well enough with people like me. I know a lot of myeloma patients were required to take it because they had compromised immune systems. I understand that I have friends with cancer. They had to do the same thing, but they also say it was the worst decision that they ever made.
This is not a discussion about the efficacy or not of the vaccine. I’m stating that I made a personal decision and I almost paid for it with my job. Fortunately, I was able to provide a Christian reason that I don’t believe in. this particular shot and none of my doctors would give me a medical reason not to take it.
So I chose not to do it, and I was able to get dispensation.
So watchful waiting is like having an IED strapped to your body with a maniacal doctor. Standing feet from you. With a trigger ready to push the button.
I’m being hyperbolic about this, but think about what you’re looking at in those days. The potential that you will live five years was very strong. And if your genetics came back bad and they weren’t able to treat you because of those things, then you’re talking about some serious concerns.
I had two children that weren’t married. They were out of college, but I wanted to see them get married. I wanted my daughter to have grandchildren. I was hoping that my son would marry someone that wanted to have grandchildren as well.
So we come into 2022. And ’22 was pretty significant for me because I was starting to experience pain. And, you know, you tell people that you’re experiencing pain and they will always find a way to dismiss it. Gee, you’re almost 60, Brad.
Of course you’re going to have pain. And so you’re feeling really, you know, inadequate about this because you know, you don’t want to be the nervous Nelly and you don’t want to do all these things, especially someone who’s been through cancer with my wife. You know, she’s looking at you because the doctors don’t say anything.
So I found myself getting more and more concerned. I left the company that tried to fire me because of Covid, and I went to another company. The stress was immense.
I started the first portion of June, and by July I had Covid and it was difficult. But even though I have high morbidity concerns, I just took the stuff that he told me to take. It wasn’t fun, but I made it through and I was really, really tired.
And then I went for labs, and MD Anderson says if you’ve had Covid in the past three weeks, I’m not letting you in. I came down already with my 24 hour in hand, and I’m trying to find my way. I don’t want to lie to somebody when they ask me. Going through that? Yeah, it was on the 10th of July or whatever it was. Well, that hasn’t been three weeks. I’m not going home. I’m not I’m not going to do it.
So they let me in and I got my blood work done. And the numbers were a lot higher than a spike up. And so there was great concern associated with that.
Smoldering high risk multiple myeloma
Had more testing, had another bone marrow biopsy. This time I did a bone marrow biopsy without any sedation. And the doctor says, oh, you have a high pain tolerance.
And then it was time to learn about cytogenetics.
So I did my research looking at all of those things and those markers. And that’s when my doctor in November of 22 told me that I have high risk smoldering multiple myeloma. And that I have a 50% chance of being in treatment in the next two years.
I’m thinking, bring it on. Let’s just get this thing done, because I am so tired of watchfully waiting and having stress because of it.
Now in 2024, my labs continue to worsen, and the pain is now consistent–hip, pelvis, lumbar pain. You sit and you’re driving along and you feel pain in your lower back and you can feel the pressure.
Today, since my pain is now consistent, I’m sure that my smoldering high risk multiple myeloma will be there when I see my doctor next.
I am a person who prepares because that’s what I do.
I’m a risk mitigator, that’s how we handle projects.
So to mitigate my risk, I’m going to make sure that I understand what’s in front of me.
Reaction to the diagnosis
Getting cavalier
So you’re sitting there with all of these things weighing on you. Then you get cavalier.
You know, the stages of grief are that, first of all, you start to bargain and you’re saying, well, God, you know, the percentages are low, so you’re just going to keep me going here and I’m going to make it pass by 5 years and everything’s going to be great. And then, you know, the reality starts to hit as your numbers increase each time.
Each time they want to tell you again what they’re looking for. They just say that you’re stable. But when you see your numbers increase, that’s not stable to a human being, to a doctor, there is no statistical abnormality in the percentage increase because they’re looking at a number that they won’t tell you and is higher than what you have.
So emotionally it starts to drain on you. And every time, every 3 months you are going to the doctor, you get your labs done. And then you sit and you watch the labs come in and you see, oh, you have a low blood count or this is low or this is high. And so, you know, you’re doing all the things that you’re not supposed to do.
But I am a person who prepares because that’s what I do. I’m a risk mitigator, that’s how we handle projects. So to mitigate my risk, I’m going to make sure that I understand what’s in front of me.
So I had the cavalier attitude to this smoldering high risk multiple myeloma. Bring it on. I’ll do my chemo and I’ll just do this stem cell transplant. It’s going to be nothing. I am going to be cool. We’re going to have this happen.
Depression
Over time, the progression started to weigh on me more and more. Not only did I have the pressures of work, but I had this pressure and I started to go into a pretty deep depression.
I didn’t even realize I was depressed, but the depression came with such quickness and force that I found myself having trouble being able to do my job.
I almost got fired because of that.
Finding solace in prayer
So at my church, we have small groups, and I went to 1. It was the first time we were having the small group and I met some people that I didn’t know.
So I was explaining that I was getting ready to go down for some more testing and things, and I was describing that I had a smoldering high risk multiple myeloma.
And the minute I said those words, I lost it and I burst out in tears and I was inconsolable for a good five minutes as everything let out.
So those of you that have been through some type of traumatic experience, whether it’s the loss of a spouse or a child or whatever, this is the time when the acceptance happened.
And that’s the time I still get emotional. That was the time that I said, yeah, I can do this, but you know, God, you got this. And whatever your timing is for me. If this is what is to be, then I’m ready to walk this with you.
So we went around and prayed and my wife prayed for me and that was a healing thing for me.
Has God been faithful? He has been entirely faithful. Once I had that episode with my church group, it wasn’t a cavalier attitude that I had anymore. It was a peace about me. And God has nurtured that peace, despite the fact that I’ve had a lot of pain that comes.
But the problem with pain when you’re smoldering myeloma and you’re watchful waiting is your pain comes and it usually goes away about the time that it’s time to go see the doctor. Well, tell me, have you had pain? Well, yeah, about a month and a half ago. And they go, well, blah blah blah. They’re not really thinking about that because it’s not now.
… living through this diagnosis and the treatment that follows is how you get out the other side, and how you can also be part of the patient story.
Lessons Brad wants to share
So the most important thing that you can do as a cancer patient is to live through your cancer.
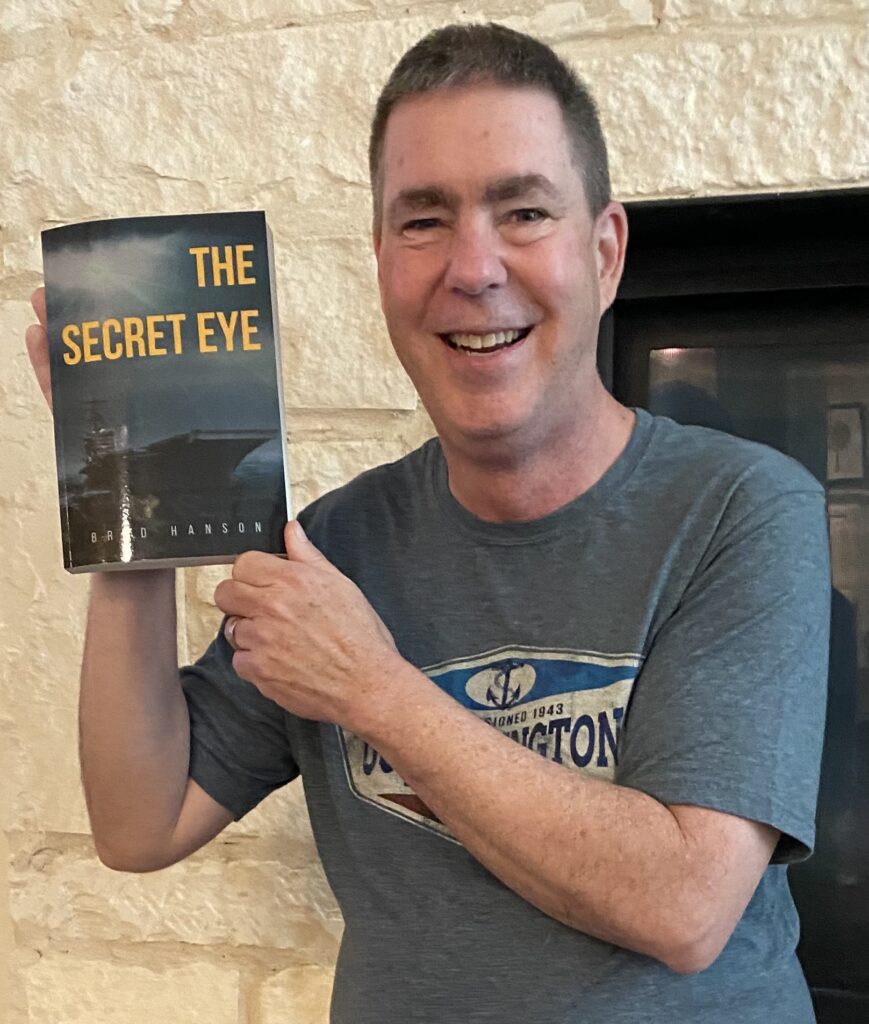
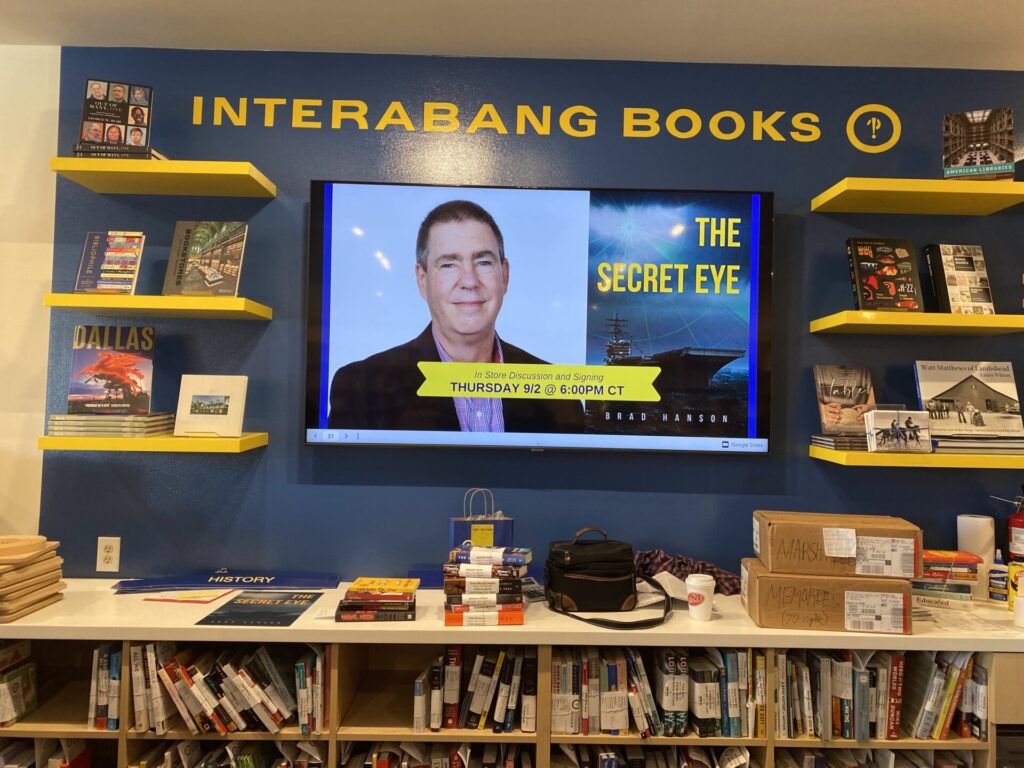
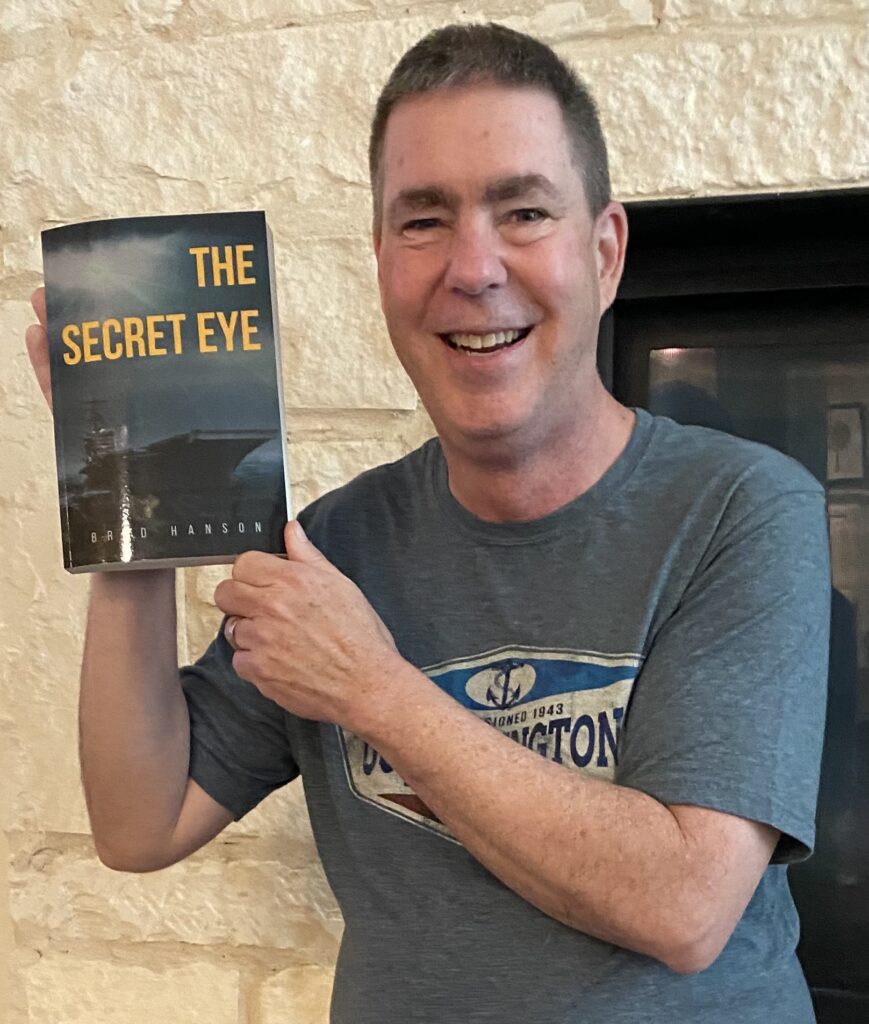
I like to write. In 2023, I started a blog called Living through Cancer and through that in 2021 I published a fiction or historical fiction book. And so I felt that writing and talking about my smoldering high risk multiple myeloma journey would be a helpful thing to others.
So you need to find a way for an outlet. You need to find people who are going to support you. And when it seems like your mind is controlling your body, telling you that you have pain that people don’t see, you need to not allow people to influence how you’re feeling. Your mind can do a perfectly fine job of making you feel a certain way when you’re really not. So you need to check yourself. You need to be aware of your body.
There are a lot of resources, good resources that are out there, on smoldering high risk multiple myeloma and other related concerns. Knowledge is power. You must have proper knowledge.
Anybody can research this information and maybe you want to do it with your spouse, one of your siblings. It’s a lot of people who need to be involved in your care. Not only your care team at your oncologist or your specialist office.
And finally, you have to make sure that if you’re in a watchful waiting or some type of a precancerous period, you need to make sure if you’re at all concerned that you don’t have the right diagnosis, get to a specialist. Your local oncologist is a great resource, but sometimes, especially with something that is as rare as blood cancer is, you need to have somebody that researches it.
And find your place and make peace with the fact that this is something that is treatable. Most cancers today are treatable. They’re not a death sentence. There are only a few that we won’t mention, but they’re treatable, and you can have a quality of life.
But living through this diagnosis and the treatment that follows is how you get out the other side, and how you can also be part of the patient story.

Inspired by Brad's story?
Share your story, too!
More Smoldering Myeloma Stories
Maui B., Smoldering Myeloma
Symptoms: Inflammatory eye disease, uterine bleeding
Treatment: Watch and wait; routine biopsies ands scans
...
Brad H., Smoldering High-Risk Multiple Myeloma
Symptoms: Abnormal kidney function (stage 2 kidney disease), mild anemia
Treatments: To be started at the time of interview
...
Yolanda B., Multiple Myeloma
Symptoms: Anemia, unusual craving for starchy food, ‘clicking’ sound produced by knees under certain circumstances (such as when walking up stairs)
Treatments: Radiation, chemotherapy, targeted therapy
...