Tim’s Multiple Myeloma Story
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez

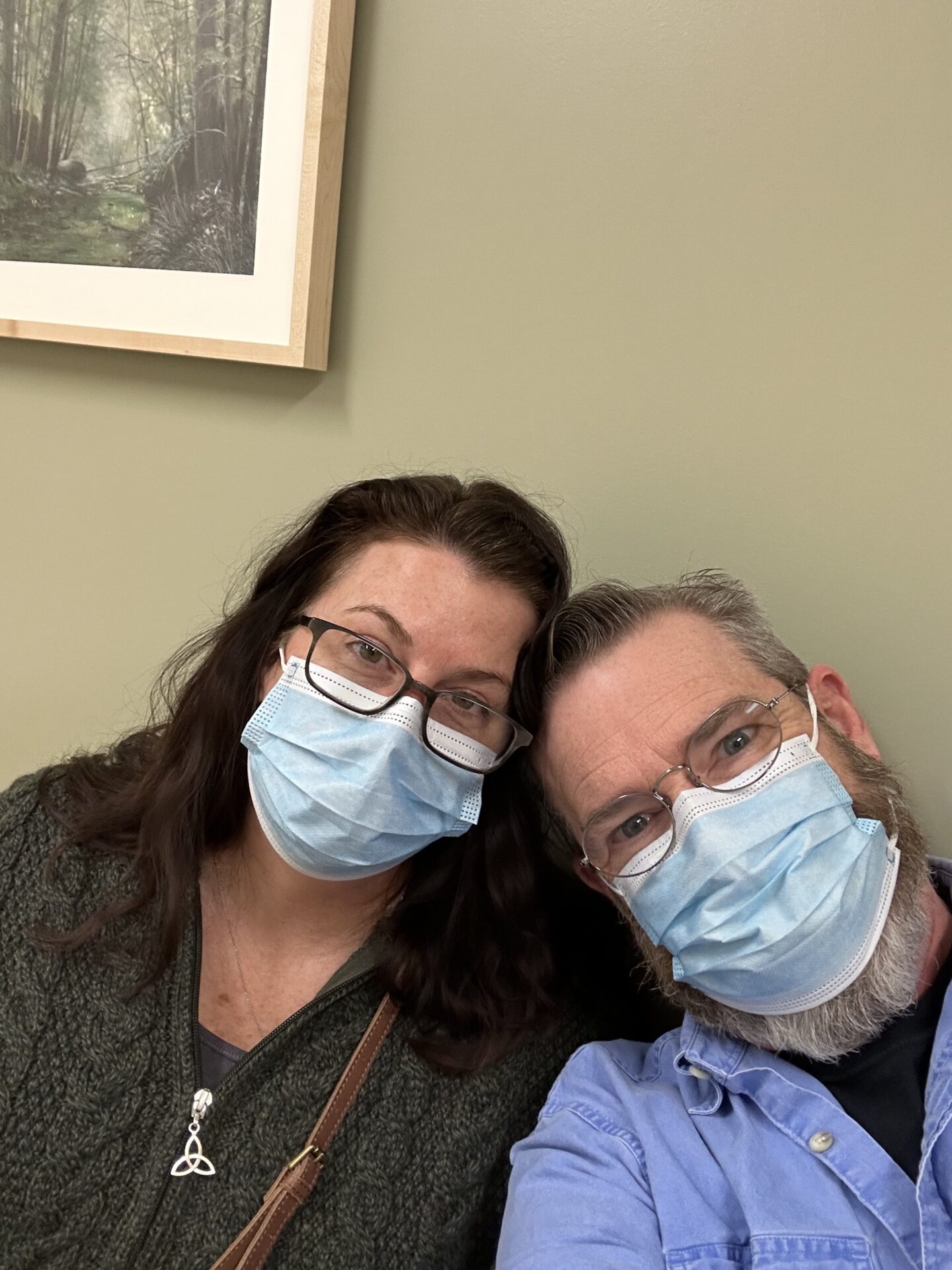
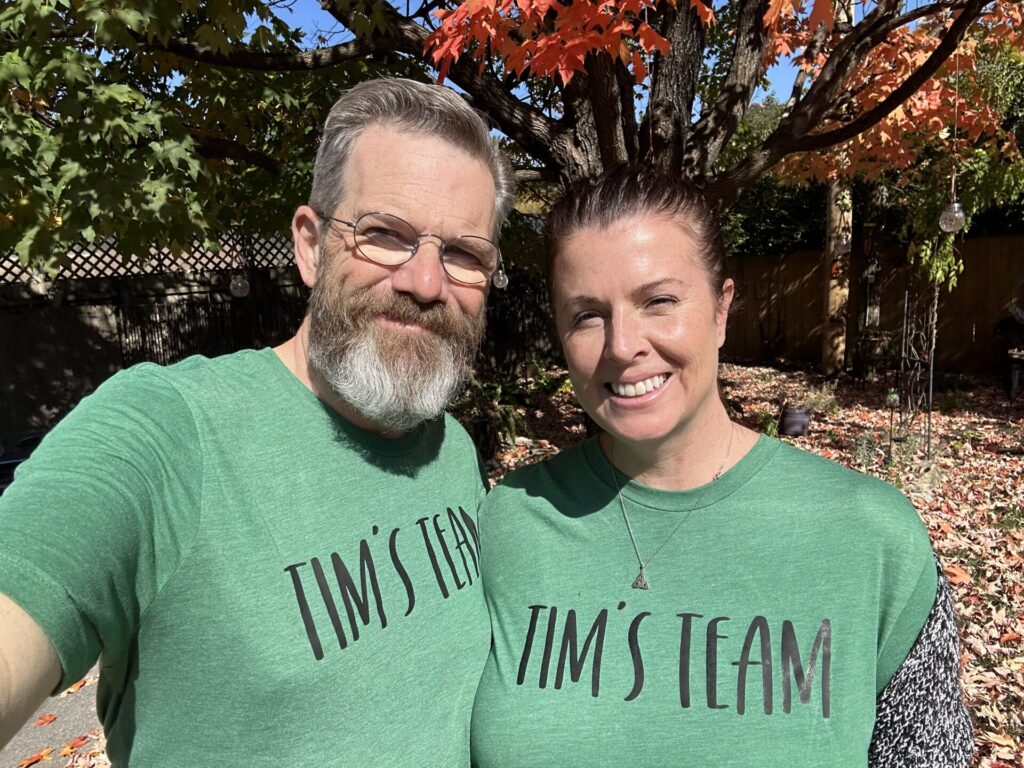
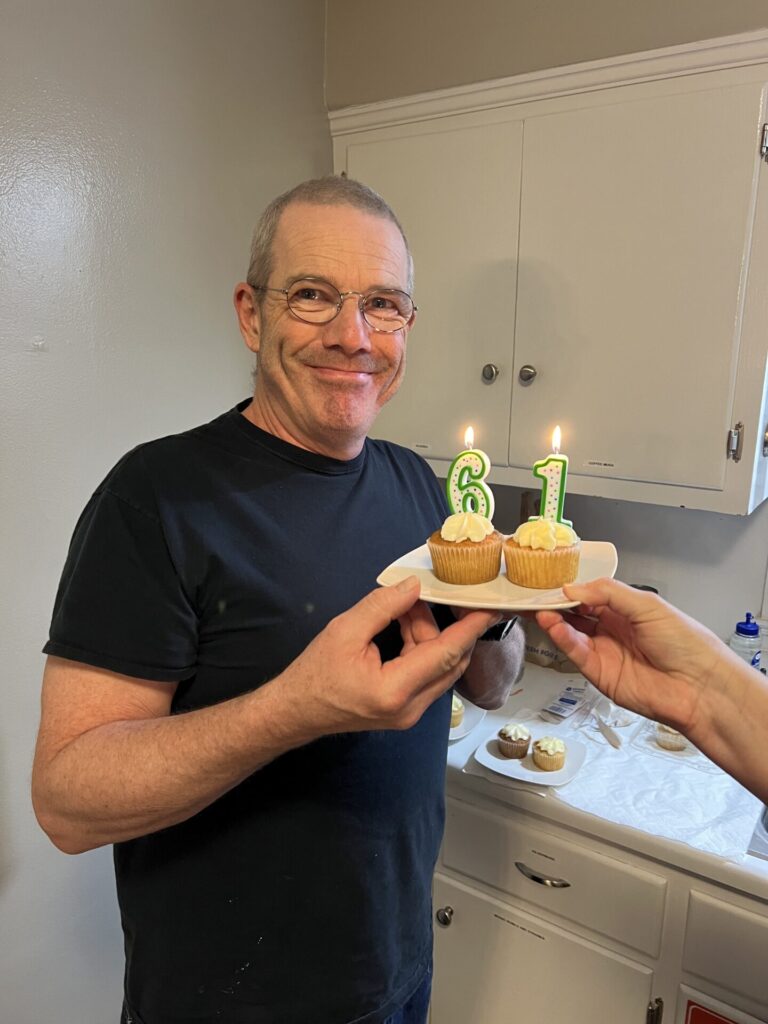
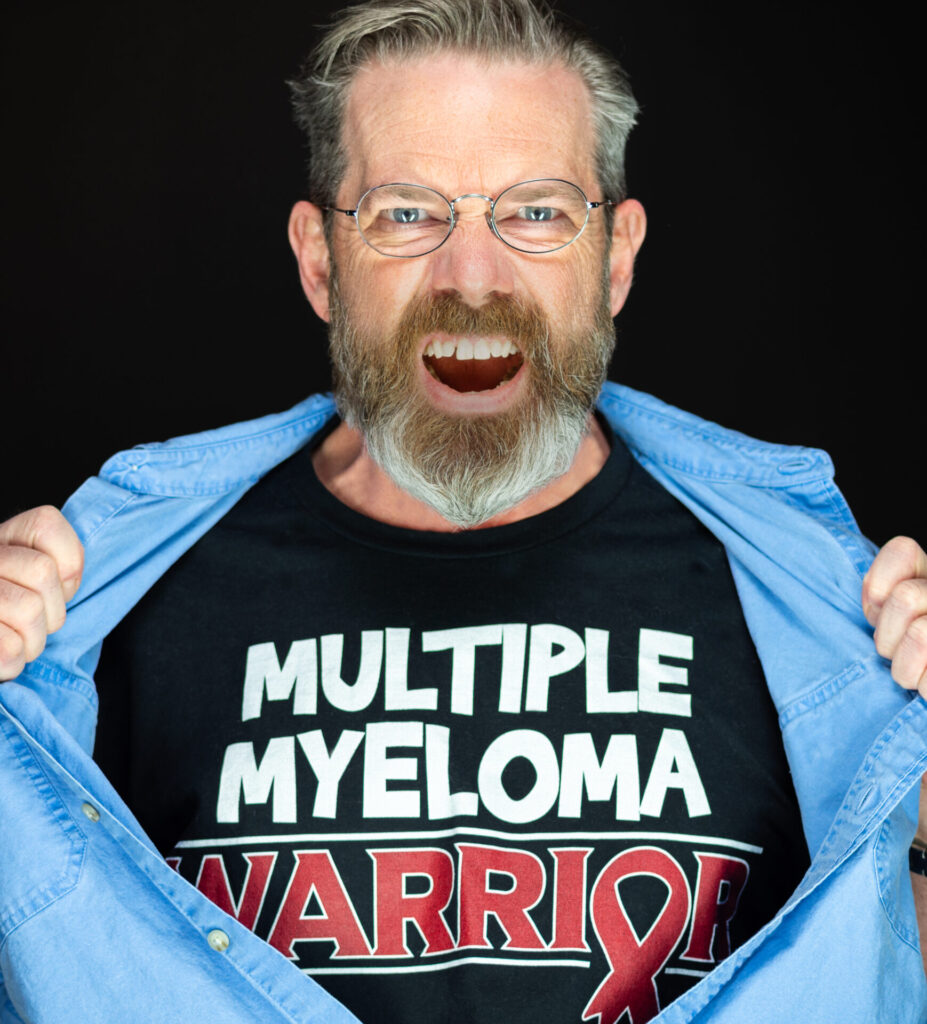
61-year-old Tim, who hails from Lexington, KY, is being treated for multiple myeloma.
An elite cyclist in his youth and still striving to be active and live healthy, Tim and his family were blindsided by his surprise diagnosis with multiple myeloma in the course of treatment for a gallbladder infection. Tim refused to succumb to depression and anger and, upon his doctors’ advice, chose to undergo chemotherapy and stem cell transplants.
Thanks to his treatments, support from his family and friends, and overall can-do attitude, Tim faces each day with positivity and hope. He shares his story with us to help others who may be facing the same situation.
In addition to Tim’s narrative, The Patient Story offers a diverse collection of stories about multiple myeloma. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Tim H.
- Diagnosis:
- Multiple myeloma
- Symptoms:
- None that could be identified; cancer found through CT scan for emergency gallbladder removal
- Treatments:
- Chemotherapy: Revlimid, Velcade, and Dexamethasone; Darzalex, Kyprolis, and Dexamethasone; Melphalan (preparatory for stem cell transplant)
- Stem cell transplant

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
You’ve got to look for hope. And you’ve got to look for help.
Introduction
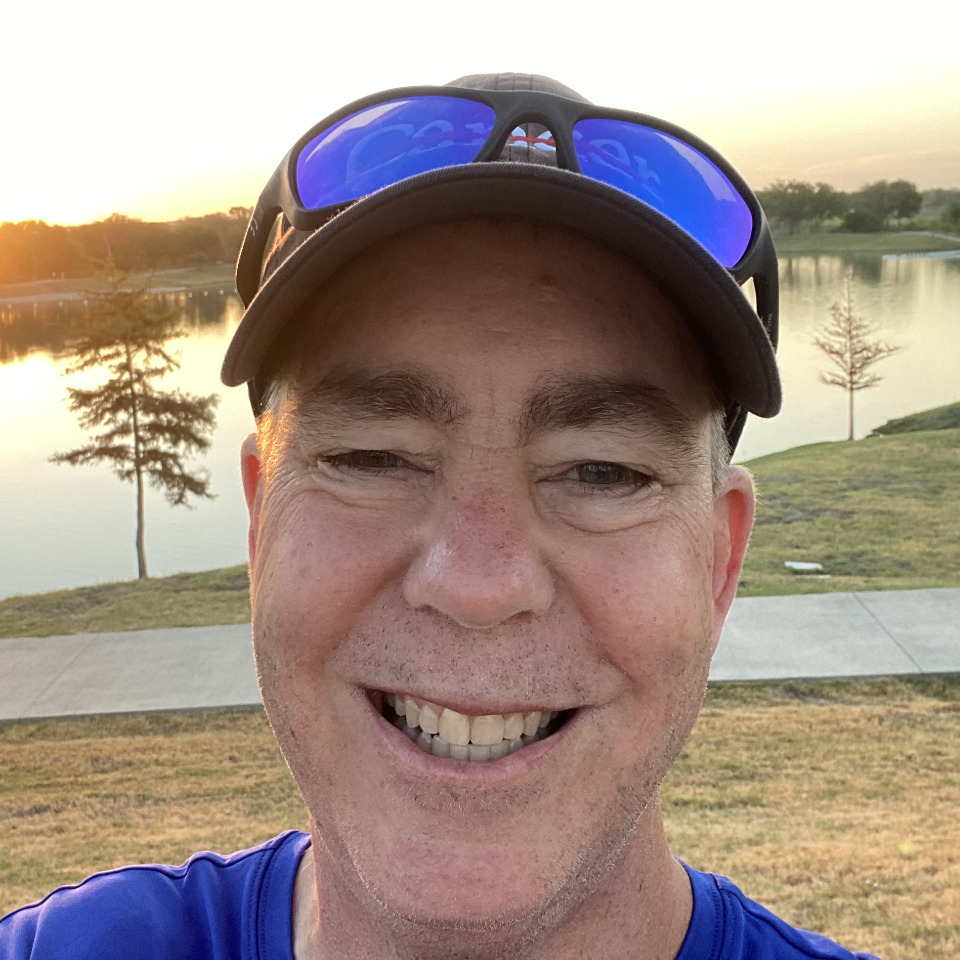
My name is Tim, and I currently live in Lexington, KY. I’m in my 60s. I’m married and we have kids.
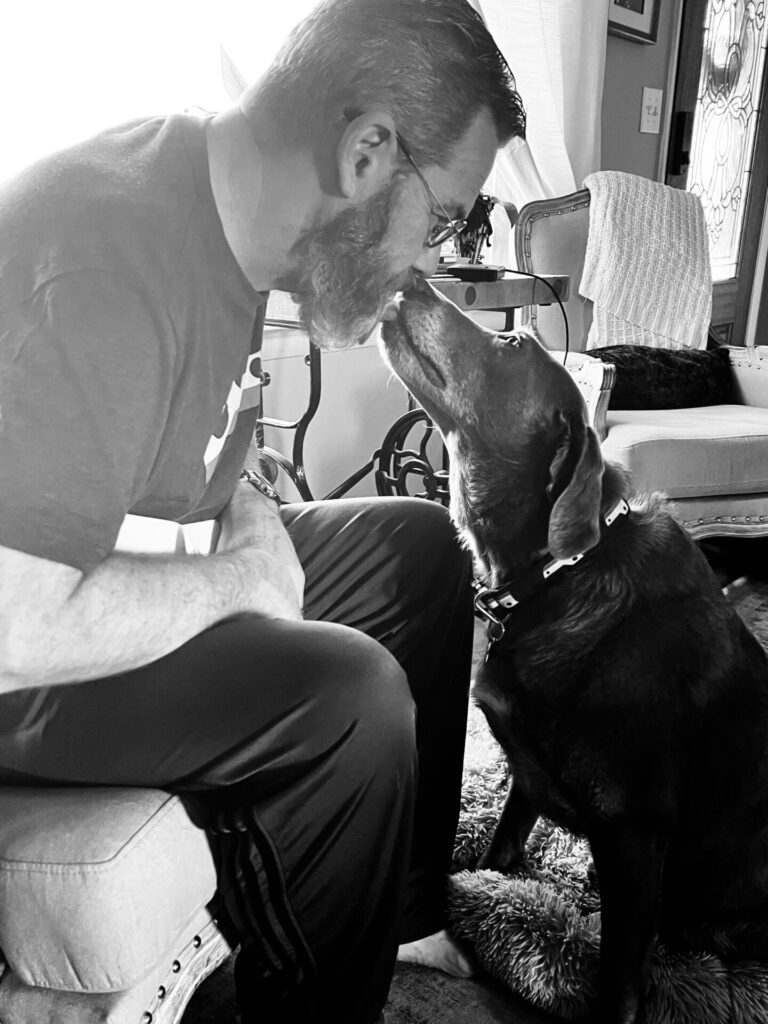
I work full time, and I also have a side business. We live on a on a small farm here in Kentucky. We have a few dogs that we like to play with. I have some old cars I like to work on. And I also try to exercise as much as possible.
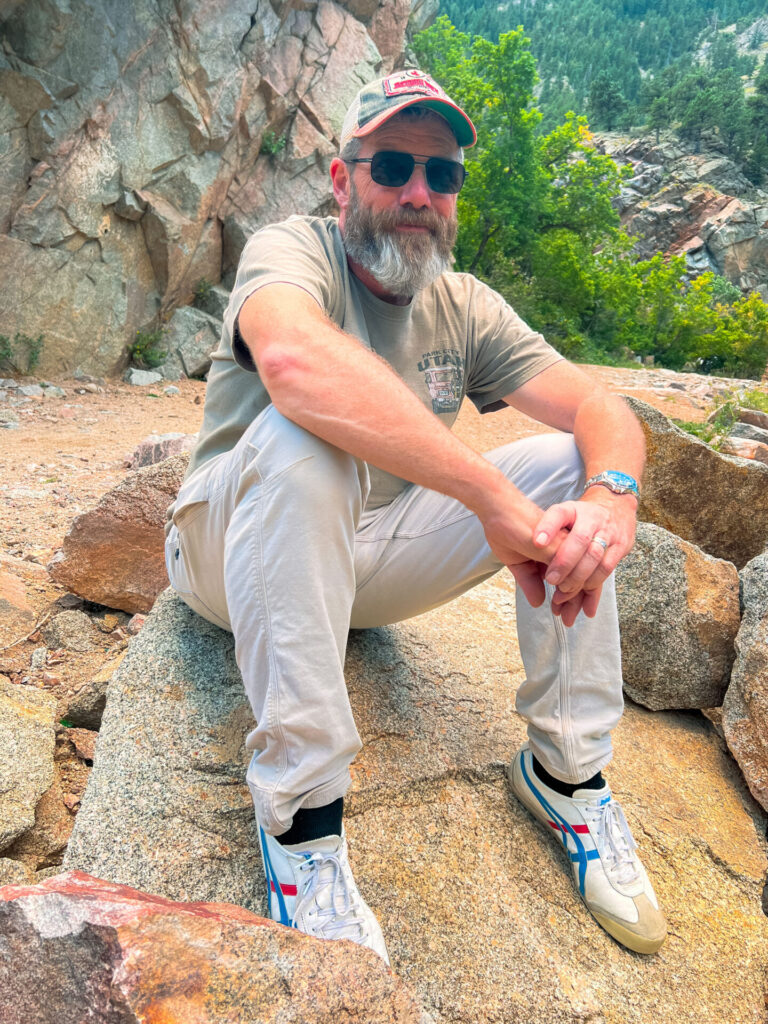
In my youth, I was an elite cyclist. I’ve continued riding throughout my life.
In the late summer of 2022, I was diagnosed with multiple myeloma. It was devastating news. But it’s almost a couple of years now and things are going quite well. My family has been very supportive and we’re trying to make the best of it.
Initial “symptoms”
I actually feel I was asymptomatic.
In the late summer of 2022, I turned 60. I had never been in a hospital for any form of stay up until that point. I broke bones and, you know, had gone for stitches and things like that. But I’ve never had a hospital stay.
For about a year prior to that I was having a lot of stomach problems, but they were not very consistent. They were sporadic and sometimes months apart. And in actuality, they had nothing to do with my multiple myeloma diagnosis.

Discovery and diagnosis

In August of 2022, my wife and I were in Colorado camping to celebrate my birthday, and I started having some severe stomach problems.
About 3:00 a.m. at the start of Labor Weekend, I was in excruciating pain. At about 5:30 a.m. or so, my wife and I drove over to the emergency room and they let me in. I got seen really quickly.
They went through the normal questions, asked where the pain was and everything and said, do you still have your gallbladder? Push comes to shove, and it ends up being a severe infection in my gallbladder.
While I’m there, they’re running all the tests. They put me on some heavy painkillers and we wait and they come back eventually after quite a number of hours and say, okay, we’ve run our tests. You know, we’ve contacted a surgeon we’ve scheduled, we’ve determined that your gallbladder is very infected, you’ve got several severely large gallstones. And tomorrow we’ll go in for surgery to have those removed.
And by the way, while we were doing your CT scan, the technician noticed some things. So we will be contacting our oncologist on call to come in and have a discussion with you. We see some lesions and we think it might potentially be a few things. One of them being multiple myeloma.
At which point I looked at my wife and I’m like, did he just say they’re going to bring an oncologist in? Completely random and out of the blue. I admit I was still doped up, so I don’t think it had quite the effect that one might expect, but it was pretty startling to hear that.
So they ended up keeping me in the hospital for five days. My infection was pretty bad, and they were waiting for it to clear, but they also were running parallel tests, protein tests and such to see what they can do.
At the end of my stay, they were pretty sure that’s what it was.
I was released and then scheduled to come back a couple of days later for a bone marrow biopsy. They did the biopsy.
And then I met with the oncologist and he said, the results show that, you know, you from what you see, you have about a 25% coverage in your bone marrow. So we’re going to start scheduling your treatments. So that was at the end of September.
Multiple myeloma really messed with my head after having a full life of good health.
But you cannot put me in a downward spiral.
Reaction
There are aches and pains in my life. You know, my back has never felt great for 15 years. I don’t think any of those things were related to my multiple myeloma diagnosis.
And so it was really out of the blue and you just get dumbfounded to begin with that somebody would say that to you.
I’m like, how can I? How can I have a multiple myeloma diagnosis? I feel other than my gallbladder problems, I feel perfectly fine. I mean, I didn’t feel tired. Really didn’t feel anything like that.
But then you start worrying, of course. Especially when, you know, you start talking to your doctor, the oncologist, and I started meeting with a secondary oncologist, so I have my primary oncologist who does my treatments. And then I have a secondary oncologist at the University of Kentucky, where they decided that it would be best to do my stem cell transplant.
So when I met with them and it’s a teaching hospital, so they’ve got fellows and students there and everything while you’re being diagnosed and, you know, they can be pretty frank about some things as well. And they didn’t really sugarcoat much.
When they talked about what we can expect from this and how my multiple myeloma was not curable. They can basically prolong things for a while, but inevitably, as the fellow put it, this is going to be end up being what causes your death eventually. Unless obviously something comes along and whatnot, you get hit by the proverbial bread truck.
Multiple myeloma really messed with my head after having a full life of good health.
But you cannot put me in a downward spiral.
Choice of treatment
My doctor gave me a choice.
At the beginning it was, listen, here’s a couple of different pathways we can take. We can do multiple myeloma treatments continuously. And then when your numbers go down, we can put you on a monthly and hopefully maintain it that way. Then you can go through a stem cell transplant. And hopefully that will add a number of years onto the end. That might not be there if we just do treatments without a transplant.
Now he really didn’t have the numbers to back that up. They’re not far enough into, I think, the collective that they can really show one way or another. But it’s again, I mean, it’s a daunting thing to think about the transplant and what that might mean. But it was the best avenue. It seemed to get the best quality and length out of what time I had.
So at the beginning of October I started my multiple myeloma treatment.
Treatment
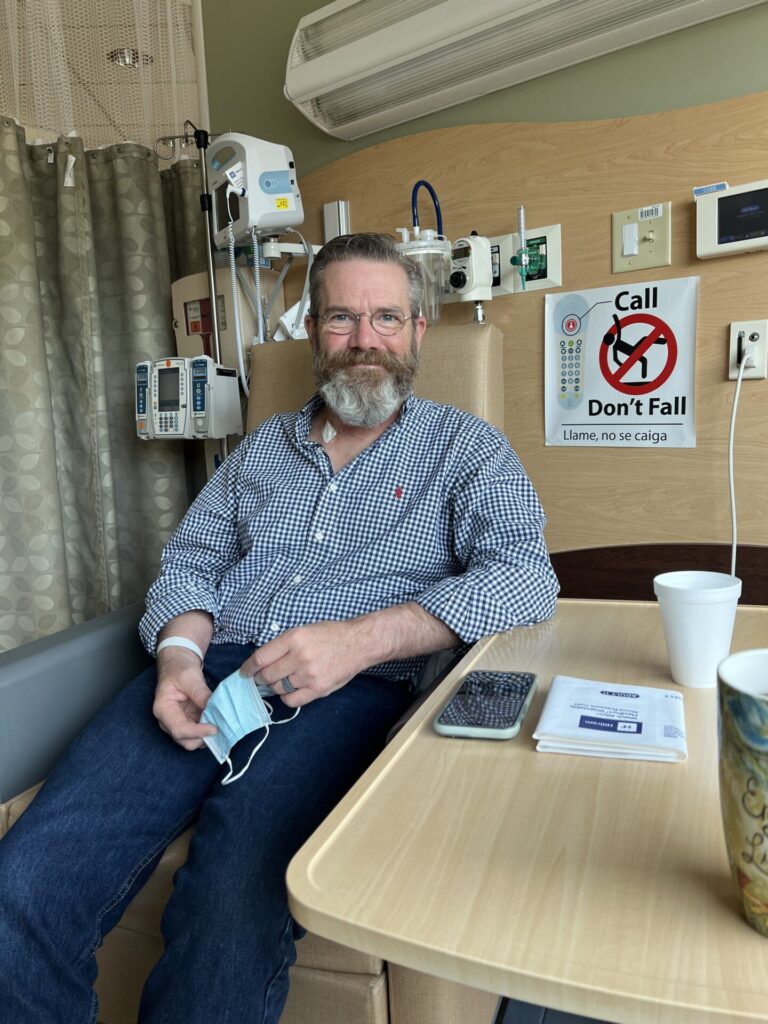
After I was diagnosed, my oncologist said, we should start treatment. We want to get you in right away.
But my wife and I asked if we could prolong a week, go away for a little bit and come back and start the treatment. It was our anniversary coming up within a couple of days. They said yes.
In the interim, they sent me the list of treatment dates and what I would be getting.
Chemotherapy: Revlimid, Velcade, and Dexamethasone; Revlimid
They started me off on the revlimid, velcade, and dexamethasone treatment.
So I was treated twice a week. Twice a week, and then revlimid 14 days on and seven off up until mid-December, when I started having a reaction to it. I ended up with a three-quarter body rash from my chest down.
I was also not reacting to it well enough. My protein levels were coming down very slowly, much slower than they really wanted to see.

Chemotherapy: Darzalex, Kyprolis, and Dexamethasone

At the beginning of the year, they moved me over to a darzalex, kyprolis, and dexamethasone treatment, which I actually liked a lot better because it was only once a week, and then you get like a week off or and whatnot.
I reacted to that much better. I came down very quickly in protein levels.
So by April, I had slotted in for the mid-May stem cell transplant. So they stopped my multiple myeloma chemotherapy at the end of April.
Pre-stem cell transplant procedures: Melphalan chemotherapy and vaccinations
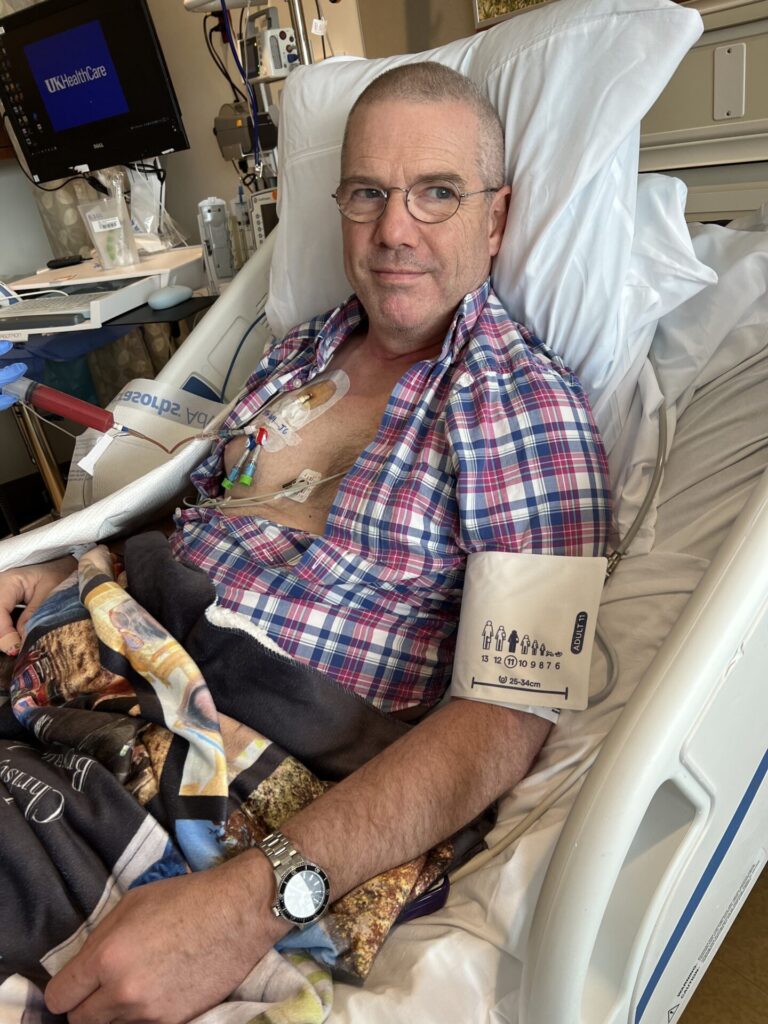
I took a couple of weeks to start getting ready for the transplant, have a chest catheter put in, and do the tests that they require to make sure you’re a valid candidate for the transplant, which I was; and then extraction of stem cells from my blood via the catheter; and then cryogenic storage of these cells.
And then I went in for chemo with melphalan to basically kill everything in my bone marrow.
After that, interestingly, I needed to get all my childhood vaccinations again.
So one of the things that the pre-stem cell transplant does is it necessitates you getting all your childhood vaccines all over again, because that protection is no longer there.
I thankfully did not have much of a reaction. I’ve heard some people tell some pretty gnarly stories about it.
I went in for my infusion and they’re like, okay, we’ll have your vaccines for you. So the nurses lined up on either side of me and then just did a countdown, and then they all just did the shots all at once.
I think they do that just to keep people’s anxiety down and such. I had some reactions of soreness and whatnot, but nothing really major.
And I had the transplant the day after that.
Stem cell transplant

The 18th of May is my rebirth day coming up. It’s going to be here in a few weeks.
Stem cell transplant sounds like a severely complicated procedure, but in reality I was amazed at how uncomplicated it can be.
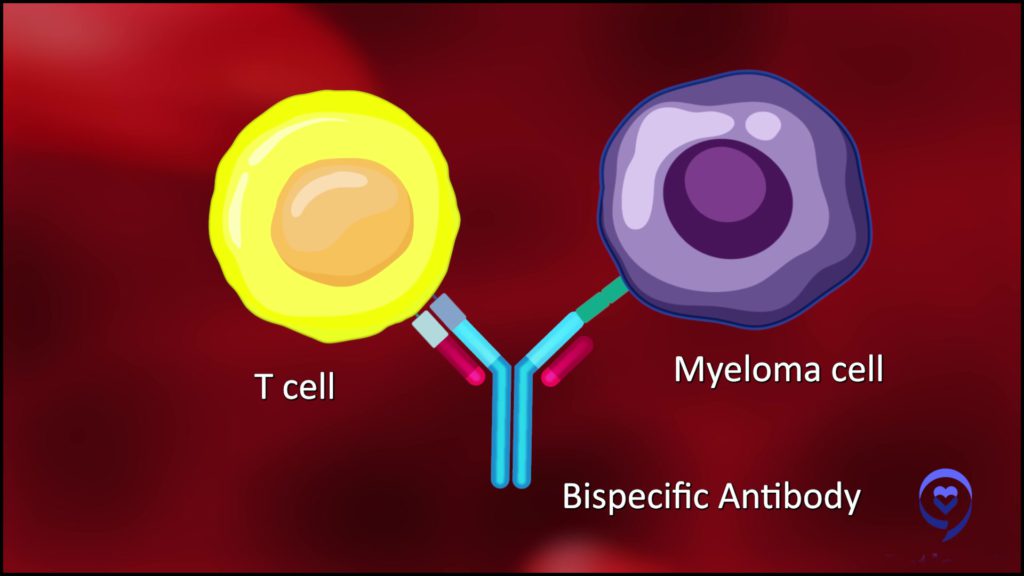
After the pre-transplant procedures I described, the day afterwards, they reintroduce your frozen stem cells into your body. And then they basically replicate or grown, you’re given some other medications to agitate them quite a bit.
So they replicate fairly quickly, and then it raises your white blood count, the blood count rate and such. The idea here is that when you’re reduced to the level that myeloma is fairly undetectable in your marrow, and then the new cells are reintroduced, it will help combat them from coming back.
I got thrown straight into things like bone marrow biopsies, things where they cycle the blood out of your body, extract the cells, put it back in, and that itself is like a five hour procedure for three days each day where you’re just lying there while it’s done. That was freaky, to put it mildly.
And then the transplant itself. So they just start reintroducing the stem cells they previously extracted back into your body through the chest catheter.
I’m not a needle guy. Like I’ve spent the last almost a year, year and a half or so of having blood taken all the time, having IVs all the time and all this stuff. And I’ve never liked that at all. But now it’s just a fact of life.
My former boss, when this first started, he was like, well, what’s the alternative? So, I just kind of learned how to deal with it.
I think if you look at it, it’s probably very disturbing to a lot of people to see things like that, but maybe it’s the disturbing things that people need to see to help them along their way, to understanding that they should not let these things go. You know, go for your colonoscopy, go when things don’t feel right.
My transplant experience wasn’t much fun, mostly from the chemotherapy. Had a lot of issues with my stomach and the general feeling that you get just from the chemotherapy itself, because it is such a high dose.
I was in the hospital for three weeks. I started off with the transplant on day one, and then they kept me in the hospital for three weeks. Felt completely and utterly lousy all the time. Just severe tiredness, nausea, that kind of stuff.
Couldn’t sleep. Had a lot of things like leg cramps and just odd muscle pains, which, they medicated me for, but you’re just lying in bed at night because you can’t sleep. And your mind is going a thousand miles an hour.
I mean, you’re trying to get sleep, but they’re running tests every x number of hours. So you’re sort of asleep and they’re coming in and drawing from you through your catheter and things. So you never really get a real full rest.
Release from hospital and recuperation at home
So I was released. Went home. Was severely fatigued for a while.
It took a while to build up, I think until about the middle of July when I started to feel better. I felt like I was cheating because I’m like, I should feel worse than I do at this point. But I had just started treatment again in the middle of July and I still feel good.
I get tired. I have neuropathy. Shins on down. That’s bothersome, but I’m perfectly capable of doing all the things I like to do. I ride all the time. I work around the house and such.
That time during the hospital stay and right after the month or so after were really rough, a lot of lot of sleep, a lot of lying on the couch. I was still working.
Other than my time in the hospital, I’ve been working full time while this is going on. I manage web operations for a firm, so it’s not physically demanding.
It was a little rough; chemo fog and things, you know, it was a little tough putting words together sometimes. But my boss knew, the heads of the company knew, they were very supportive. And the sharpness came back, thankfully. And I can talk normally again.
Maintenance chemotherapy: Darzalex, Faspro, Zometa

After the transplant, there were a couple of months where I didn’t really have anything. And then I started with my maintenance chemo for my multiple myeloma at the end of July.
So I’m on darzalex and faspro once a month, and then every third month is zometa. I’m guessing it’s going to be like that for a bit more.
I’m just at the moment getting subcutaneous shots once a month and then every third visit is a matter for bone health. So that doesn’t bother me so much, but the meds they’re giving me can leave you feeling kind of funky for a little bit.
It’s a belly shot. Nobody’s favorite thing to do, and like I said, it leaves me feeling flu-like for several days. I also get a high dose of dexamethasone on those days, so I get that lovely steroid reaction.
If you think about the fact that there are still a lot of things to experience in this life and a lot of people that want you to be around, that gives you the hope to really continue on with things that just seem really daunting.
Moving forward
My general idea here is I’ll be on maintenance for my multiple myeloma for probably another year. And then they will see where my numbers are. If my numbers are still responding, then hopefully we’ll be able to go off maintenance.
It eventually becomes something that you accept. And you learn that it’s just going to be a part of your life.
For instance, like I mentioned, I don’t mind doctors and I’ve always had blood drawn and whatnot. But it’s still a bothersome experience for me no matter how many times it’s done. But it’s just something I’m going to have to accept as part of my life from now on.
And at some point somebody’s going to say. The multiple myeloma numbers are jumping back up again, and we’re going to have to start all this all over again. And I’ve accepted that that’s going to happen sometime in my future.

Hopefully it doesn’t happen for a while because there are some things that I still want to do. But do I wish that that they had the things in place to eradicate? Sure. But I know that they don’t. And I mean, just like most other cancers, there’s really not much you can do about multiple myeloma.
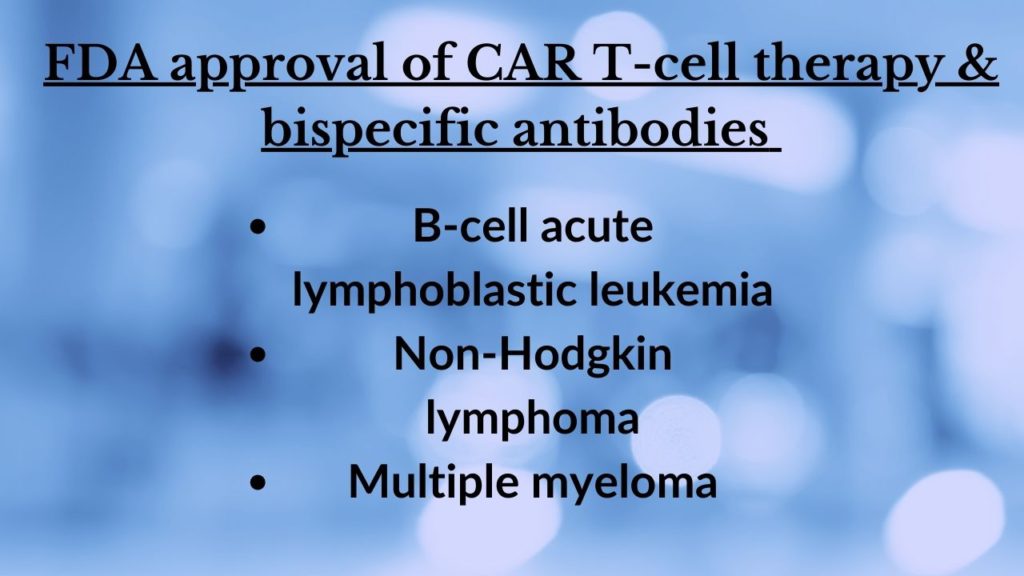
Fortunately, they’ve got enough treatments in place that as my oncologist refers to it, he says it’s just a treatable illness right now. There are others out there that are less fortunate in that respect.
So it’s kind of a two-sided sword there that you have to deal with. It does get you at the point where you start wondering, do I have everything in place that I need for my multiple myeloma treatment? You know, that was that’s part of the spiraling that I think happens right after diagnosis. My kids, my wife, all that.
What’s going to happen there? As I mentioned before, I’m very fortunate. My family is extremely supportive. My wife has been a trooper through this whole thing. I had a chest catheter in that had to be cleaned every day. She took care of that. It’s not something I could do, but she did.
She’s been with me to all the treatments. She wanted to be there in the hospital. They wouldn’t let her during my transfer. I mean, she was there during the transplant, but she couldn’t stay there.
I still have a lot of things I want to do. I’m not ready to give up on some things there. I guess it’s one aspect of my personality that has always been with me in my whole life. You know, you can have daunting things happen to you, whether they be financial or family or medical or anything like that. And you can give up. There’s that possibility that you’re just gonna throw in the towel.
And again, I don’t want to give up living life as long as I can, my multiple myeloma notwithstanding. So for me, I still plan out pretty far. And, you know, I’ll be honest, sometimes I’m thinking about things and it’s like, whoa, wait, why am I doing this? I should just be like, planning short term or something. But it’s just my personality. I just don’t want to give up. I’m not much for giving up.
So I still keep thinking long term in the future. I think that again could be personality, but it also I think is a learned thing that you don’t give up.
If you think about the fact that there are still a lot of things to experience in this life and a lot of people that want you to be around, that gives you the hope to really continue on with things that just seem really daunting.
Because I’ve been doing this for so long, I still plan out training plans for my riding, even though there’s really no end goal other than being able to do it and such. And there are days when, I have something planned, a workout or whatnot, and I wake up and I’m gung-ho. But by midday, it’s just too overwhelming. And I can just sit on the couch, you know, and that that would be perfectly fine.

I have trouble riding for a couple of days after my treatment just due to the fact that it’s an abdomen shot. They’re sometimes a little uncomfortable. So I just usually plan on not doing anything at that point in time.
But I think more than anything, it is doing something for yourself that can help you build strength both in mind and in body. That is just paramount for me.
I was riding all the way up until shortly before my stem cell transplant. I don’t ride every day, I try to get 3 or 4 times a week. Most of it is indoor training, except for the weekends. You know, if it’s nice, I try to get outside, but I have to be careful because I haven’t had a CT scan done since the originals, but I had lesions all throughout my femur, pelvis and lower spine.
And so the threat of fracture and things is extremely high. So I do have to be careful about that. I live in the country, so I don’t encounter much traffic. And I don’t go out for five hours at a time like I used to. If I get an hour and a half in, it makes me very happy.
But I find that even though you get really tired from the exercise, the end result is that you feel fatigued less from the treatments. Helps keep the weight down, helps with my blood pressure and such. It was it was pretty high from some of the treatments that I had. I was actually on blood pressure meds at the beginning of the year for a while because it seemed like I was having a little bit of a reaction. But I don’t have to do that anymore. That’s really good.
Because those have all hosted side effects as well And I just liked being out there and doing something for me. You know, I don’t have to think about work or any of those things, I can be out there just enjoying sunshine and wind and sometimes rain.
… I’m not going to hide my multiple myeloma again.
You don’t want it to be hidden if you could help somebody.
Lessons and takeaways
Once I got out of the hospital, the first couple of days, as I said, were really rough, were just spent on the couch, but I forced myself to get up and do things.
I would go for small walks around the neighborhood. It was very tiring, but being outside, being in the sun, getting air was very important.
And then continuously as I started feeling better, doing more and more. I started off just kind of shuffling around, but I worked up to half hour walks in the next couple of months and just being outside and seeing the flowers and things and just reminding yourself of what you know there is to experience in life.
I feel like also eating correctly is paramount to making sure that you recover well. My wife has celiac, and we don’t do a lot of processed food because of that. I made bread for her, all kind of things like that. Lots of vegetables. We eat a lot of beef and get a lot of protein that way. I can usually tell when I don’t think I eat well, how badly it makes me feel now.
I drink a lot of water and hydrate very well. And they were all adamant about hydrating because we’re putting all this stuff in you and you got to get it back out. The longer it stays in there, the worse you may feel. And it’s even now I have maintenance once a month. It’s still a thing to deal with. It’s mostly flu like kind of symptoms.
Another thing that I’ve found has been so important is to lean heavily on loved ones, family and such.
A lot of people, myself included, are very much, “I should be able to handle this myself. I shouldn’t have to bother other people for something that is my responsibility.” Meaning, it’s my multiple myeloma. It’s not their illness. Why do I have to bother anybody else about it? My dad, who’s still alive, he’s 92. And he’s battling his own battles with skin cancer.
At the beginning of this, I’ve been very open with everybody about my multiple myeloma . As I mentioned, I brought it to the attention of the people at work, even though, technically, I don’t have to. I think it’s very important.
And my dad was wondering, why are you telling people this? Shortly after my diagnosis, I made a post on Instagram and it got shared and some of my friends and family and whatnot reached out. “I was very surprised to hear that you did this.”
But I’m not going to hide my multiple myeloma again. You don’t want it to be hidden if you could help somebody.
Get people to realize or open their eyes that there might be something going on in themselves. Again, multiple myeloma is a disease that is usually not caught until it’s pretty far in, until the point where you can’t work, can’t walk. Or you break a bone bending over or turning over in bed or something like that, because your bones have been eaten away by the disease. At which point, it becomes so much harder just to do anything about it.
So again, if you’ve just been diagnosed with multiple myeloma, don’t be afraid to rely on those around you to help you. You know, if it hadn’t been for my wife helping me with these things, I don’t know what I would have done. You know, if she wasn’t there to help me clean the catheter or just help me when I couldn’t move. Making meals when I couldn’t get up. She put up with my massive dexamethasone treatments every week– shortness of temperament and such.
You’ve got to look for hope. And you’ve got to look for help.
You know, at this point it’s like, okay, I have this journey that I was basically documenting, but I’m like, now what do I do? I feel okay, but I’ve started thinking about it more and more.
And one of the things I’d like to do is get more involved in the cancer world and helping people. Just like we’re doing now. Learn how to answer questions. Deal with it because you’ve been through it.
Again, I’m not hiding my multiple myeloma. I’m trying to be open about it. I feel like I’ve learned a bunch of things, experienced a bunch of things.
So I have no objections to being very open about things that have gone on with me in this. It’s looking for all kinds of avenues to help wherever I can.

Inspired by Tim's story?
Share your story, too!
Related Cancer Stories
More Multiple Myeloma Stories
Tim H., Multiple Myeloma
Symptoms: None that could be identified; cancer found through CT scan for gallbladder removal
Treatments: Chemotherapy, stem cell transplant
Scott C., Refractory Multiple Myeloma, Stage 3
Symptoms: Pain in hips and ribs, night sweats, weight loss, nausea
Treatments: Clinical trial, chemo, kyphoplasty, stem cell transplant
Jude A., Multiple Myeloma, Stage 3
Symptoms: Pain in back, hips and ribs; difficulty walking
Treatments: Bilateral femoral osteotomy, reversal due to infection; chemotherapy