Outspoken Self-Advocacy: Frank’s 2nd Opinion Found His EBV-Positive Stage 4 Stomach Cancer (Gastric Adenocarcinoma)
Frank’s experience with stage 4 stomach cancer (gastric adenocarcinoma) began with a cascade of subtle but relentless symptoms. Living in Georgia, Frank describes how unexplained weight loss, night sweats, and unusual fatigue prompted him to seek medical attention. When he developed swelling in one testicle and persistent, dull back pain, the uncertainty of his situation only deepened. Despite initial misdiagnoses of testicular cancer and lymphoma, his persistence in consulting multiple specialists eventually led to the correct identification: EBV-positive stage 4 gastric adenocarcinoma.
Interviewed by: Keshia Rice
Edited by: Chris Sanchez
His experience included the determination that his stomach cancer was associated with the Epstein-Barr virus or EBV. Frank’s self-advocacy to get second opinions and his readiness to challenge initial diagnoses proved critical. This became especially true as he navigated treatments that ranged from chemotherapy for a misdiagnosis to targeted therapies for his actual condition. He shares how grappling with disappointment over uncertain origins, coping with the side effects of chemotherapy, and finding solace in his wife, dog, and wider cancer support networks was marked by emotional highs and lows.

Frank’s outlook has been shaped not just by the disease or its treatments, but by a growing empathy and willingness to guide others. He describes the transformation from feeling isolated and overwhelmed to discovering the power of men’s cancer support groups. As he continues maintenance therapy and adapts to his “new normal,” Frank champions community, openness, and self-care, especially for men who might otherwise turn inward in the face of such challenges.
Frank’s candid reflections provide clarity on the realities of stomach cancer and underscore how seeking support and second opinions can change the course of treatment, and how connection, even in difficult times, can transform isolation into hope.
Watch Frank’s video above, and read his edited interview transcript below to delve into his story. You’ll learn how:
- Prioritizing your own intuition and seeking second opinions can significantly alter the course of a health experience
- Side effects from treatments and the disease often go beyond the physical, affecting identity, routines, and relationships
- Support networks, especially those focused on men, can be transformative and counter feelings of isolation
- Every patient’s experience is unique, and compassion toward others can deepen through health challenges
- Transformation: Frank shifted from private struggle to active, empathetic advocacy within the cancer community
- Name: Frank B.
- Diagnosis:
- Stomach Cancer (EBV-Positive Gastric Adenocarcinoma)
- Age at Diagnosis:
- 37
- Staging:
- Stage 4 (metastatic)
- Symptoms:
- Weight loss
- Night sweats
- Fatigue
- Swelling in one testicle
- Urinary tract infection
- Back pain
- Treatments:
- Chemotherapy
- Immunotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Hi. I'm Frank
- My early stomach cancer symptoms and initial concerns
- Misdiagnosis and getting a second opinion
- The correct diagnosis of EBV-positive stage 4 stomach cancer, and my emotional reaction to it
- My “New Normal:” work, fatigue, and daily life changes
- Self-advocacy and navigating the medical system
- Sources of support and maintaining perspective
- Survivorship and giving back
- Advice to others facing a similar diagnosis
- Lessons I’ve learned
- Looking forward: my hope for the future
Hi. I’m Frank
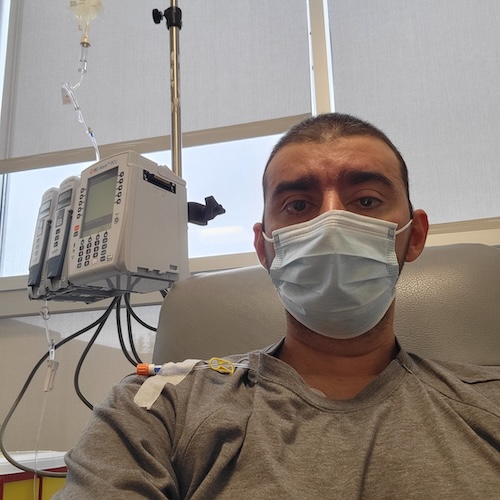
I was diagnosed with stage 4 gastric [stomach] cancer in March 2024, and I live in Georgia. I work in software development.
Generally, I have been pretty healthy. I did have one major health issue about three years ago: I had a benign brain tumor, and that was removed.
Interestingly, because of that experience, when I started having these odd symptoms, I thought it could be something serious. If I hadn’t gone through that before, I might not have thought anything of it.
My early stomach cancer symptoms and initial concerns
Before I started having some serious symptoms, I was losing weight, experiencing night sweats, and feeling very fatigued. I also had an unusual symptom: swelling in one testicle. At first, I thought it could have been an infection. I also had a urinary tract infection (UTI), which was very unusual for me as I had never had a UTI before.
So I went to a walk-in clinic. They gave me antibiotics, which cleared out the UTI. About a month later, I started having swelling again, which concerned me. I scheduled an appointment with a urologist at that point.
The swelling and back pain started around the same time. The back pain was persistent. I started experiencing it during spinning class, so at first I thought it was from the bike. I kept adjusting the height and position at the gym, but the pain wouldn’t go away. It was a dull, persistent pain, not severe enough to keep me from walking, but enough to alarm me. The combination of back pain and testicle swelling made me wonder if it could be testicular cancer. Those were the two main symptoms.
I initially had the UTI in January and went to the walk-in clinic, where I got antibiotics. I still don’t know if these symptoms were related. Then, I started having swelling and back pain in March. Between developing those symptoms and seeing a urologist was probably a few days. I was initially diagnosed with testicular cancer. The time between misdiagnosis and the correct diagnosis was about another two months.
Misdiagnosis and getting a second opinion
When I went to the urologist, he sent me for a CT scan because they noticed some enlarged lymph nodes throughout my body. There was concern that it might be lymphoma. They performed a biopsy at a community hospital and diagnosed me with testicular cancer.
After doing research, especially on social media, I was advised to get a second opinion to ensure the treatment was appropriate. So I went to a research university, where they were skeptical of the diagnosis and decided to do another biopsy at a different site. They disagreed with the original diagnosis. They identified it as metastatic carcinoma of unknown primary, meaning they didn’t know where it originated, but it was stage four.
That was frustrating because testicular cancer generally has a very high cure rate. I was told I would undergo treatment for six months and that would be it. But when diagnosed with metastatic cancer of unknown primary, I was told it was likely more about palliative care. That was a big letdown.
From then on, it was about getting more opinions to pinpoint the origin, and eventually, they determined it started in my stomach.
The correct diagnosis of EBV-positive stage 4 stomach cancer, and my emotional reaction to it
I got my diagnosis of gastric [stomach] cancer at the end of May. In between that and my testicular cancer misdiagnosis, I was put on chemotherapy for testicular cancer before the correct diagnosis was made.
To be honest, when I first received the diagnosis, I freaked out when they said it might be lymphoma; I looked up a lot about lymphoma. Then they told me it was testicular cancer, which was another shock.
After a series of tests, including next-generation sequencing, I was finally diagnosed with gastric cancer. By then, I was numb because I was tired, but also relieved to finally get a concrete diagnosis.
My wife went to all my appointments with me. We traveled from Georgia to Indiana, New York, and Tennessee; everywhere, hoping someone would offer a better answer.
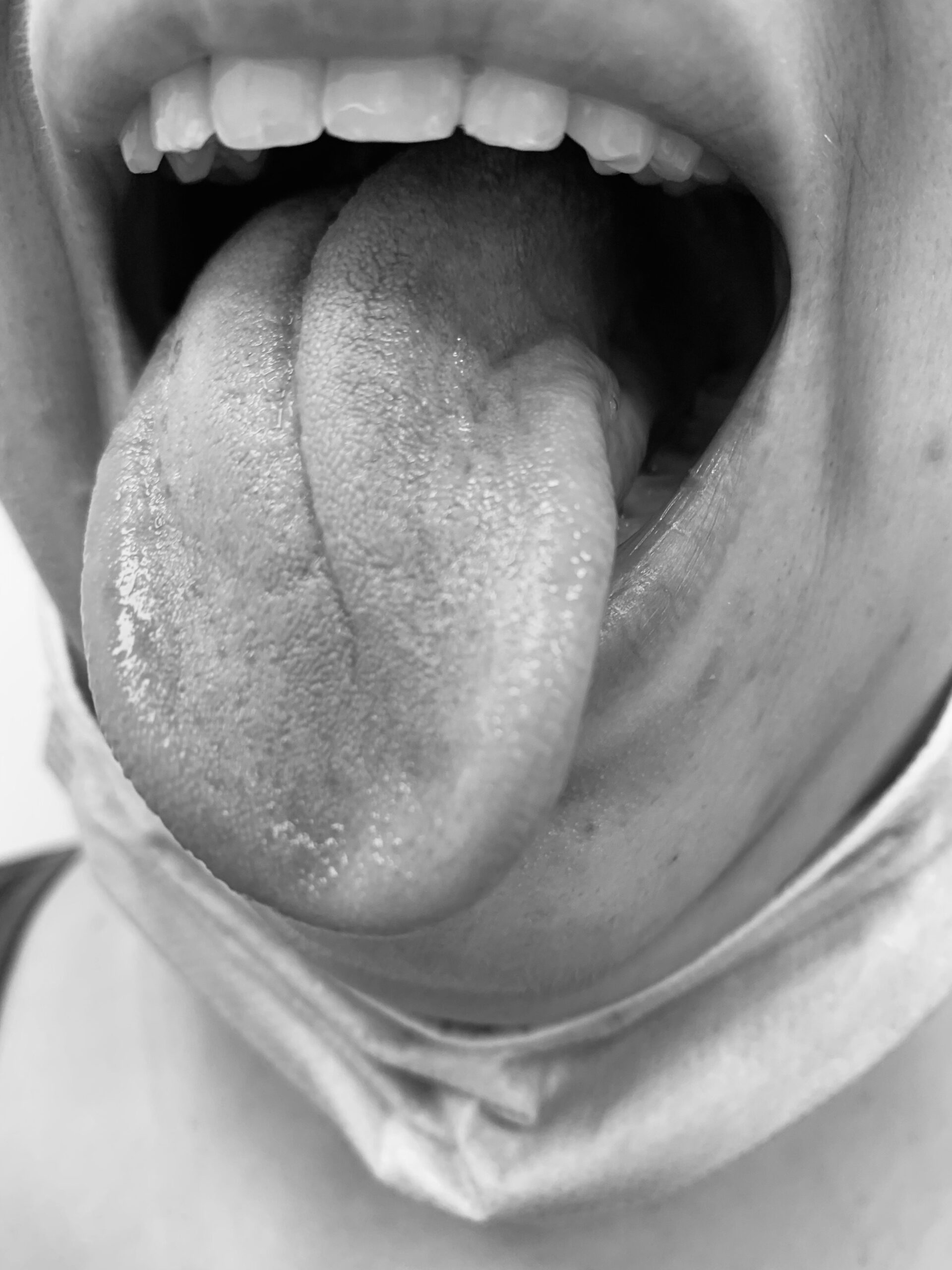
EBV, or Epstein-Barr virus, is a subset of gastric adenocarcinoma. There are maybe four subsets; mine was the one caused by Epstein-Barr, which happens in about 10% of cases. When I got the gastric cancer diagnosis, next-generation sequencing was done to see if I qualified for immunotherapy. That sequencing discovered the cancer may have been caused by a virus, prompting further tests for Epstein-Barr, which came back positive.
My “New Normal:” work, fatigue, and daily life changes
Right now, I’m on an oral chemotherapy pill that causes hand-foot syndrome, making my hands and feet very sensitive. My new normal involves using lotion and moisturizers throughout the day and sleeping with gloves on. It’s uncomfortable. Wearing gloves during the day is manageable in cold weather, but it’s uncomfortable in summer. It’s an adjustment, and I’ve become very high-maintenance.
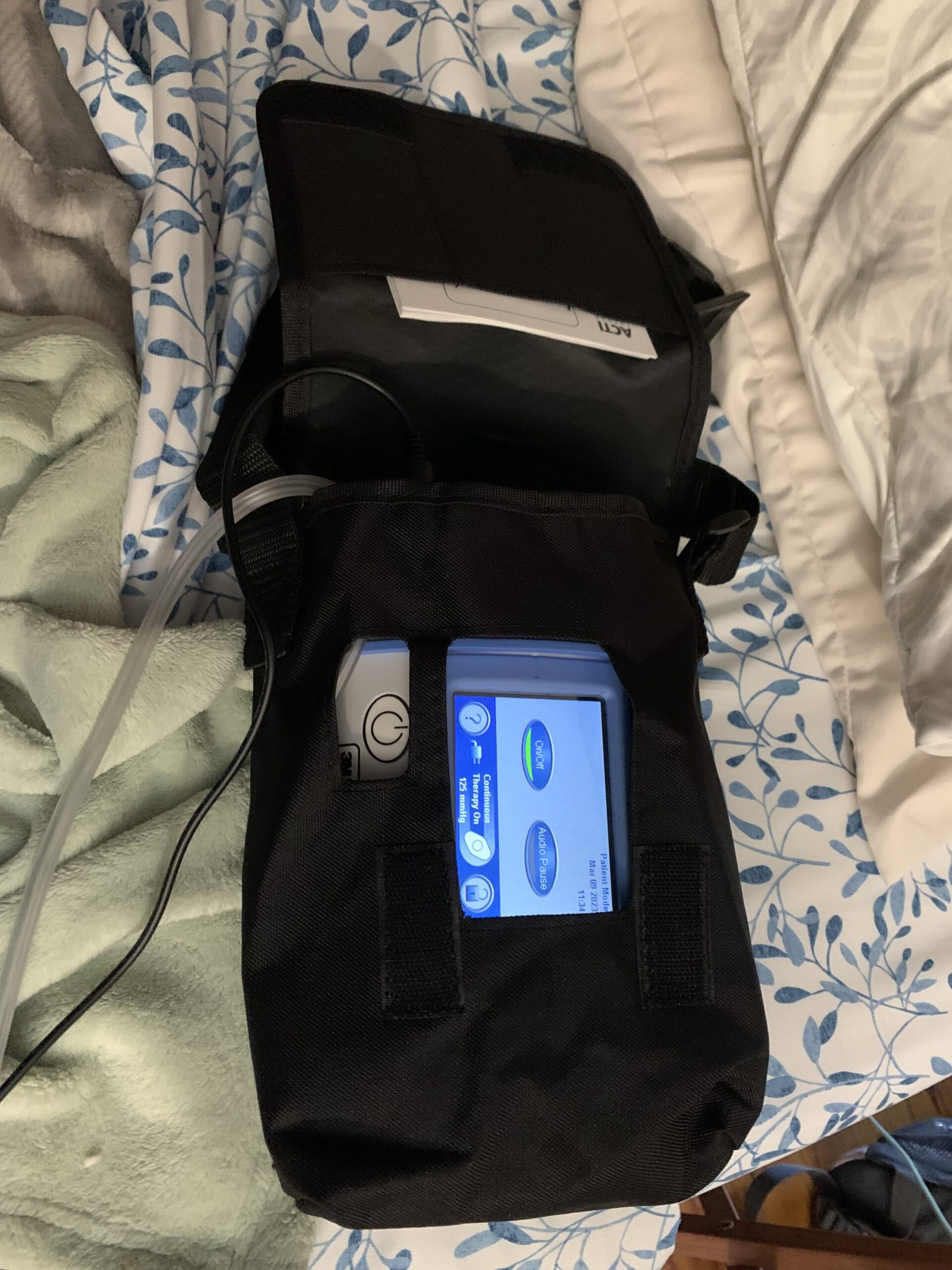
I still work as a software developer, but I don’t have the mental capacity I had before, probably due to the treatments and the resulting mental fog and fatigue. When I began treatment, it was every two weeks, then every three weeks, now monthly.
Treatments leave me tired for a few days, but I still go to work. AI tools like ChatGPT and Gemini have been helpful, especially with things I now forget.
I still go out, but less often. I used to love the gym, but now worry about getting sick, so I’m setting up a home gym to stay active without the risk. It’s a little more isolating.
Self-advocacy and navigating the medical system
Maybe it was a silver lining, but having a benign brain tumor before made me determined not to just accept a diagnosis without seeking second opinions. When I had cancer, I didn’t want to let myself just accept what I was told. If three doctors gave the same answer, that was reassuring, but if they disagreed, more opinions were helpful.
I did get some pushback. My original oncologist from the community hospital pushed back when I looked for more opinions, insisting others would say the same. It turned out they didn’t.
I believe it was worth advocating for myself; I don’t know what would have happened if I’d just gone along with the initial diagnosis and treatment.
Sources of support and maintaining perspective
What keeps me grounded are my wife and my dog.
The dog has helped a lot; I got him last year after my diagnosis to motivate me to stay active. When my feet hurt from the oral pill, the dog still wants me to walk or play with him; he doesn’t know I’m sick, which is nice. It helps not to always be seen as a patient.
My wife helps by checking in on how I’m doing, and she’s had her own health issues, so she’s compassionate and more alert to changes in me, often more than I am. It helps having someone else looking out for me because I might get used to gradual changes and not notice them anymore.
When I started losing hearing in my left ear, I didn’t think much of it, but my wife made an appointment for me. This led to the diagnosis of my brain tumor. Similarly, when I had symptoms of cancer, even after my experience with the tumor, she pushed me to go to the doctor. I didn’t resist this time because she’d been right before.
Survivorship and giving back
Honestly, I’m still figuring out what survivorship means to me.
I’m more involved with the cancer community, especially groups for men with cancer, since many men don’t talk about their experiences.
Survivorship means trying to make things a little less overwhelming for someone else going through something similar. That’s what I spend most of my time on now outside of work.
My sense of purpose has shifted. When you’re healthy, you plan for the future, vacations, and retirement. Now, being involved in the community helps me think beyond myself and helps others. Alleviating the burden, even in small ways, feels meaningful. Helping others helps me too.
Advice to others facing a similar diagnosis
I’m very involved with an organization supporting men with cancer. Women are generally more outspoken and seek support, which is why most support groups are female-oriented. Men, on the other hand, tend to isolate and bury their feelings.
My advice is not to spend too long in isolation. It’s okay to feel scared or isolated at first, but the longer you stay there, the harder it is to get out. Let other people help; people want to help, so let them.
The most common issue for men facing cancer is the cultural expectation to be strong and the provider. If they can’t work and provide for their family, it feels like their manhood is being taken away. When I lost my hair, I didn’t really care except for being cold all the time. At first, not working and having family care for me felt strange, but it’s okay to be vulnerable for a while.
Lessons I’ve learned
I wish I’d been more sympathetic to people’s invisible struggles, like cancer. The longer I’ve been involved, the more I realize how many people are affected.
Practically, I wish I’d known more about health insurance, disability, and related logistics. Before, I just picked whatever during open enrollment at work, but now I realize how important those choices can be.
I do have family and friends supporting me. I try to spend more time with them now and not postpone things. Previously, I was more career-oriented and would skip social events for work. Now, I prioritize trips or time with friends, realizing that those priorities have shifted.
One thing that’s changed: I used to get frustrated in traffic, but now it doesn’t bother me. After spending so many hours at the infusion center, waiting in the car just means I can listen to music or relax.
As for what I’d tell my past self. The main thing is about panic. Telling someone to “calm down” doesn’t work. The more I go through this, the less panic I feel. My advice to myself would be to deal with things as they come instead of trying to foresee everything that might happen in the future. Looking up survival statistics just causes anxiety, but everyone’s situation is unique. Deal with things as they come.
Looking forward: my hope for the future
What I’m looking for most is more treatment options. Stomach cancer isn’t very common in the United States, so there aren’t many options. I hope for more research and more ways to manage this as a chronic condition, something I can live with, even if it means dealing with side effects.
I’ve talked to my doctors about clinical trials. Since I’m still on my first line of treatment and it’s working, my oncologist keeps clinical trials as a backup plan for when they might be needed. I have friends who have done clinical trials, and I’ve learned a lot from their experiences.

Inspired by Frank's story?
Share your story, too!
More Stomach Cancer Stories
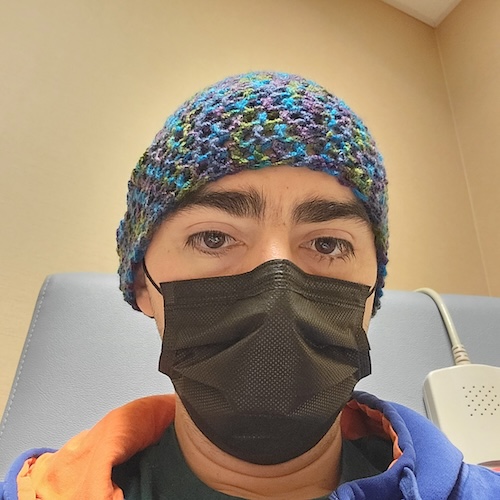
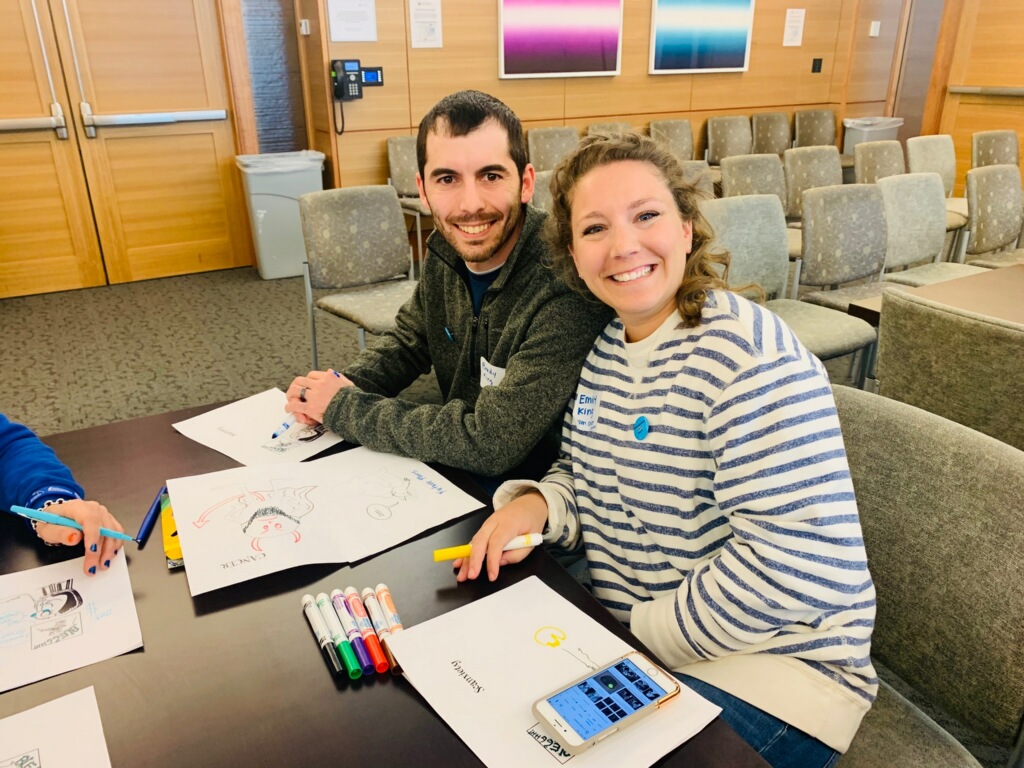
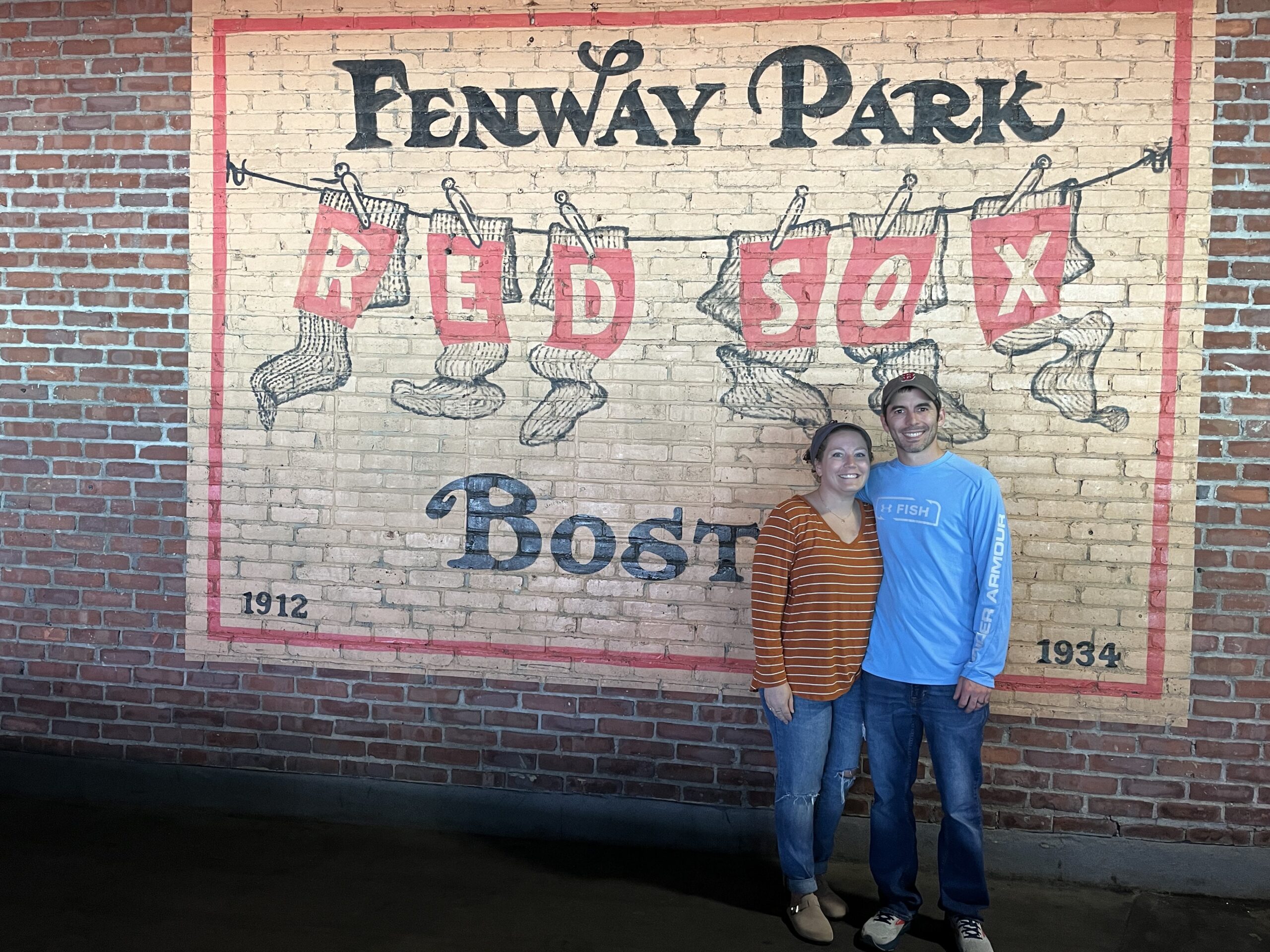
Andy G., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Stomach pain, back pain, chest pain, extreme exhaustion, shortness of breath after short walks
Treatments: Chemotherapy, immunotherapy
...
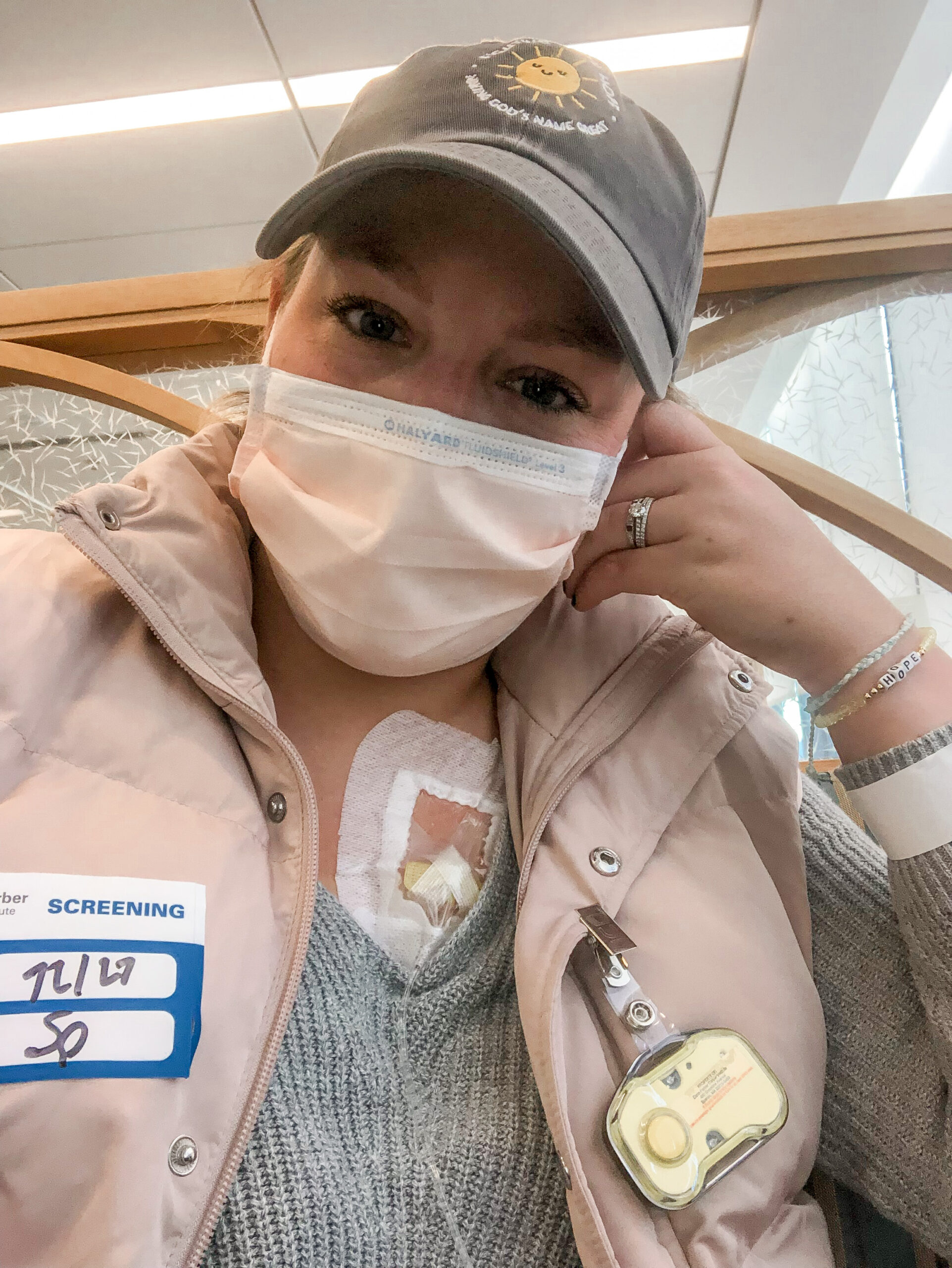
Alyssa B., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...
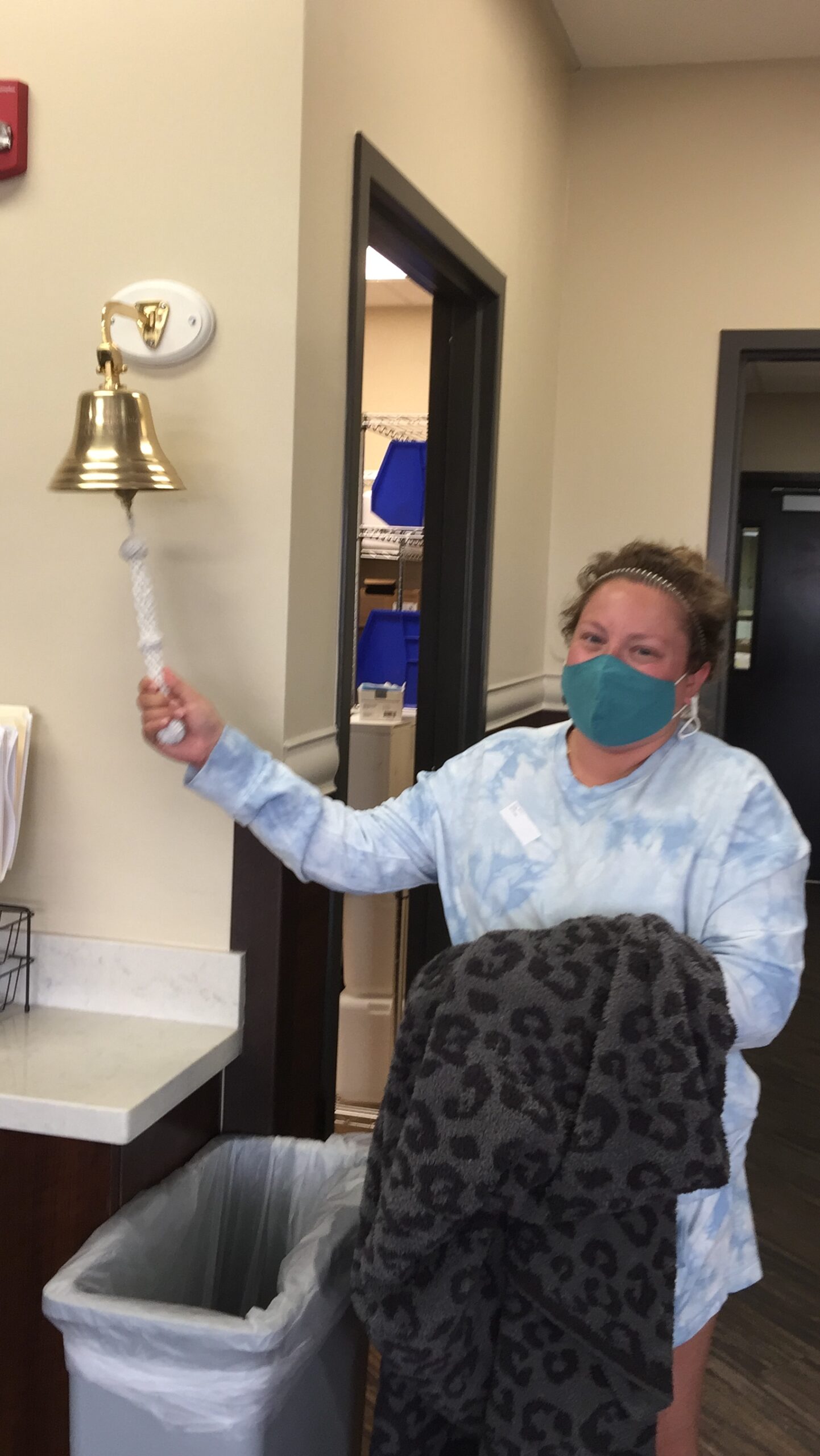
Brittany D., Stomach Cancer, Stage T1b
Symptoms: Choking suddenly while eating and attempting to speak, neck and right shoulder pain, neck tightness, trouble swallowing certain food items
Treatments: Surgeries (subtotal gastrectomy, D1 lymphadenectomy, gastric bypass)
...
Camilla C., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Issues swallowing, swollen gland in the neck
Treatments: Palliative chemotherapy was offered but declined, nutritional changes to support her comfort and energy, meditation and mindfulness practices, self-directed healing methods
...
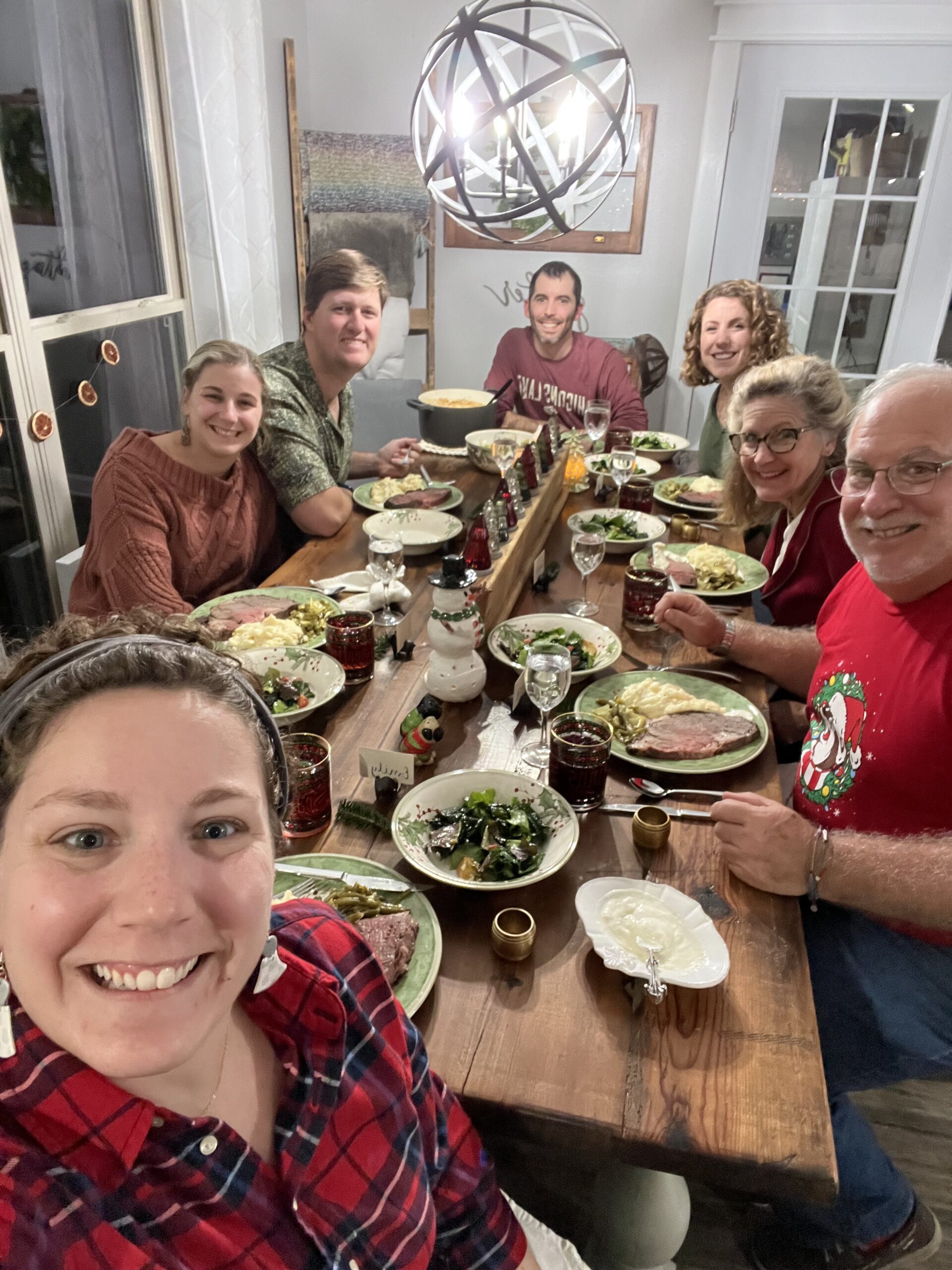
Emily D., Stomach Cancer (Gastric Adenocarcinoma), Stage 4 (Metastatic)
Symptoms: Persistent postpartum stomachache, early satiety, difficulty swallowing, vomiting
Treatments: Chemotherapy, immunotherapy
...
Alyssa B., Stomach Cancer, Stage 4 (Metastatic) (Hospice Update)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...